Abstract
This study was to investigate the role of complementary and alternative medicine in the prevention and treatment of benign prostatic hyperplasia. For this purpose, a randomized, double-blind, placebo-controlled trial was performed over 12 months on 47 benign prostatic hyperplasia patients with average age of 53.3 years and international prostate symptom score over 8. Subjects received either sweet potato starch (group A, placebo, 320 mg/day), pumpkin seed oil (group B, 320 mg/day), saw palmetto oil (group C, 320 mg/day) or pumpkin seed oil plus saw palmetto oil (group D, each 320 mg/day). International prostate symptom score, quality of life, serum prostate specific antigen, prostate volume and maximal urinary flow rate were measured. In groups B, C and D, the international prostate symptom score were reduced by 3 months. Quality of life score was improved after 6 months in group D, while those of groups B and C were improved after 3 months, compared to the baseline value. Serum prostate specific antigen was reduced only in group D after 3 months, but no difference was observed in prostate volume in all treatment groups. Maximal urinary flow rate were gradually improved in groups B and C, with statistical significance after 6 months in group B and after 12 months in group C. None of the parameters were significantly improved by combined treatment with pumpkin seed oil and saw palmetto oil. From these results, it is suggested that administrations of pumpkin seed oil and saw palmetto oil are clinically safe and may be effective as complementary and alternative medicine treatments for benign prostatic hyperplasia.
Keywords: Symptomatic benign prostatic hyperplasia, pumpkin seed oil, saw palmetto oil, International prostate symptom score
Introduction
Benign prostatic hyperplasia (BPH) is a pathological symptom frequently found in the elderly population. Treatment options for men with symptomatic BPH include active monitoring, phytochemical treatment, medical therapy with α-blockers or 5-α-reductase inhibitors, and surgery (Barry et al., 1997; Watson et al., 2004). The use of complementary and alternative medicine (CAM) for the treatment of BPH patients has a long history, especially in European countries (Ortiz, 1998; Pathak et al., 2003). Nevertheless, there is still a considerable degree of skepticism from the urologic community about the efficiency and safety of these CAM products. This is mainly due to the lack of an established mechanism of action for CAM (Melo et al., 2002; Wilt et al., 1999) materials. The CAM used in this trial was pumpkin seed oil, saw palmetto oil and a combination of pumpkin seed oil and saw palmetto oil (Ernst, 2002; Hirsch, 2000). For these materials, the mechanisms of action may include alteration of cholesterol metabolism, anti-androgenic activity (including 5-α-reductase inhibitor activity), anti-inflammatory effects, and a decrease in available sex hormone binding globulin (Cristoni et al., 2000). Although the mechanisms of action of these materials have been investigated in many in vitro and indirect in vivo studies, they have yet to be clearly defined (Shoskes, 2002; Wilt et al., 2000). Nevertheless, many BPH patients are currently taking these CAM materials everyday without apparent adverse effects (Vickers, 2000). Yet, long-term treatment of BPH patients with CAM is necessary in order to assess the occurrence of side effects. Therefore, the objective of this study was to carry out a long-term study to determine the effectiveness and the potential side effects of pumpkin seed oil and/or saw palmetto oil in the treatment of Korean men with symptomatic BPH.
Materials and Methods
Study design
BPH patients with an international prostate symptom score (IPSS) of 8 or more participated in a randomized, double-blind, placebo-controlled trial of pumpkin seed oil and saw palmetto oil for a 12-month period. Volunteers were requested to sign the documents of clinical examinations agreement after careful review of the instructions. Clinical examinations were conducted for 18 months at Chung-Ang University Medical Center, Department of Urology.
By baseline checkup of general health, patients with any major diseases except BPH or patients who had BPH related treatment such as 5-α-reductase inhibitor, α-receptor blocker, urogenital surgery or any other alternative therapy for BPH were excluded. Any other medication or surgery related to BPH was not allowed during the trial.
Sixty-two patients were distributed into 4 separate groups according to their time sequence of participation; group A (placebo, control, sweet potato starch, 320 mg/day), group B (pumpkin seed oil, 320 mg/day), group C (saw palmetto oil, 320 mg/day) and group D (the combination of pumpkin seed oil, 320 mg/day and saw palmetto oil, 320 mg/day). Sweet potato starch (Bum-Ah, Seoul, Korea), standardized pumpkin seed oil and saw palmetto oil (RIA International, New Jersey, USA) were prepared in hard capsules. Patients took 2 capsules per day in the morning and the evening after a meal, over a 12-month period. After the baseline assessment of general health, each participant visited the hospital every 3 months to measure BPH parameters such as IPSS, quality of Life score (QoL), serum prostate specific antigen (PSA), prostate volume (PV) and maximal urinary flow rate (MFR). Fifteen patients (24%) were dropped during the trial due to aggravation of symptoms (n=13), movement (n=2) and initiation of BPH medication (n=1).
Finally, 47 patients were completely participated in our study. They have been checked on overall functioning, difficulties with intervention adherence and adverse symptoms weekly by phone, and visited hospital every 3 months.
Measurements
IPSS and QoL were assessed using standard questionnaire forms (2003 American Urology Association Guideline on the Management of BPH: Diagnosis and Treatment Recommendations) (Zhang et al., 2008). The questionnaire for IPSS is composed with seven questions and each measured on a 5 point scale. For the assessment, the patients responded on a scale of 0 (delighted) to 6 (terrible) to the question, "If you were to spend the rest of your life with your urinary condition just the way it is now, how would you feel about this?" The serum PSA was measured using an electrochemiluminescence method (Cho et al., 2005) (Elecsys systems modular E-170, Roche diagnostics GmbH, Germany). PV was measured using transrectal ultrasonography (Cho et al., 2005) (Voluson 730 proV GE Healthcare, Austria), and MFR was done using an uroflowmeter (Willetts et al., 2003) (Medtronic Urodyn 1000, High Med, Denmark). PV and MFR measurements started after 6 months because the urologists advised that there would not be a significant change over a short period such as the first 3 months of treatment. All patients were measured for body weight, height and body mass index (BMI) (Fanics Co. Ltd, HM-170, Korea) at the beginning of the experiment.
Statistical analysis
The differences among groups and experimental periods of each group were analyzed by Tukey's studentized range test for BPH parameters. BPH parameters for IPSS, QoL, serum PSA, PV and MFR were expressed as the mean ± standard error, and were age adjusted against group A (control), in which acquired by analysis of covariance (ANCOVA) with least square mean (LSMEAN). Also Pearson correlation was compared between parameters. SAS 9.01 (SAS Institute Inc., Cary, NC, USA) was used for statistical analysis.
Results
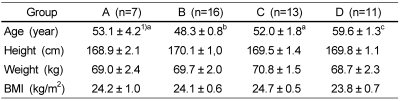
General characteristics for the patients are shown in Table 1. The average age of patients who completed the 1 year trial was 53.3 years, and the average age of group D was significantly higher than those of groups B and C (Table 1). The average height, weight and BMI of patients were not significantly different among groups, and the average BMIs of all groups were within an overweight range based on Korean obesity evaluation criteria (Lee et al., 2006).
Table 1.
General characteristics of patients (n=47)
1)Mean ± SE
Different superscripts within the same row are significantly different at α=0.05 by Tukey's studentized range test.
BMI: Body mass index (body weight/height2 = kg/m2)
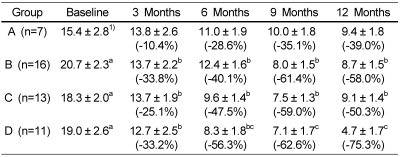
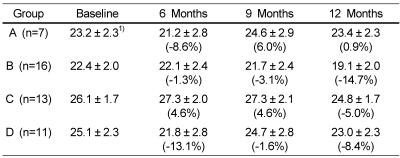
IPSSs in groups B, C and D were significantly reduced (P < 0.05) after 3 months of treatment (Table 2). IPSS of group B was decreased by 12.0 points (58.0% change), from 20.7 to 8.7 after 12-month treatment. IPSS of group C was also decreased by 9.2 points (50.3% change), from 18.2 to 9.1. The average IPSS of group D showed a constant decline from the beginning (19.0) to the end of the 12-month treatment (4.7) by 14.3 points, indicating 75.3% improvement in voiding symptoms. In particular, BPH status of group D was improved from moderate (8~19) to mild (≤7) according to IPSS. The reduction of IPSS after 12 month treatment was highest in group D, however, there was no significant difference among the groups.
Table 2.
International prostate symptom scores
1)Mean ± SE (adjusted for age)
Different superscripts within the same row are significantly different at α=0.05 by Tukey's range test with age adjusted.
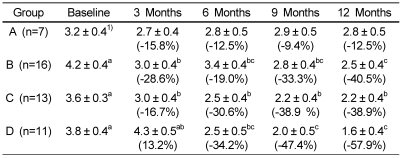
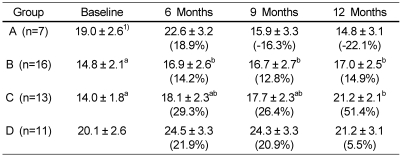
The QoL were significantly improved in groups B and C after 3 months, and in group D after 6 months (P < 0.05) (Table 3). The QoL score of group A (placebo) was not changed, but those of group B and group C were reduced by 1.7 points (40.5% change) and 1.4 points (38.9% change) after 12-month treatment, respectively. The QoL score of group D was reduced by 2.2 points (57.9% change) after 12-month treatment.
Table 3.
Quality of life scores
1)Mean ± SE (adjusted for age)
Different superscripts within the same row are significantly different at α=0.05 by Tukey's range test with age adjusted.
Serum PSA levels are shown in Table 4. The serum PSA levels of groups A, B and C remained unchanged during the 12 month trial. The serum PSA levels of group D showed a constant decline from the beginning (1.2 ng/ml) to the end of the 12-month treatment (0.7 ng/ml), indicating 41.7% reduction.
Table 4.
Serum prostate specific antigen (ng/ml)
1)Mean ± SE (adjusted for age)
Different superscripts within the same row are significantly different at α=0.05 by Tukey's range test with age adjusted.
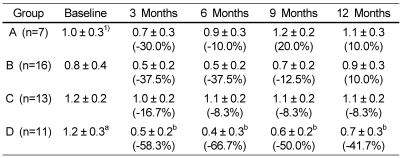
The PV of groups B, C and D showed a gradual decline over the experimental period, but these changes were not statistically significant (Table 5). The PV of group A remained unchanged over the experimental period.
Table 5.
Prostate volume (ml)
1)Mean ± SE (adjusted for age)
As shown in Table 6, the MFR of group A was gradually decreased over the experimental period with a worsening in urinary symptoms. The MFR of group B was significantly increased after 6 months and that of group C was significantly increased at 12 months (P < 0.05). The MFR of group B was increased from 14.8 ml/second at the initiation of the study to 17.0 ml/second at the end, for an improvement of 14.9%. The MFR of group C was increased from 14.0 to 21.2 ml/second after 12-month treatment, which was an improvement of 51.4%. The MFR score of group D, however, was not changed significantly during the treatment period.
Table 6.
Maximal urinary flow rate (ml/second)
1)Mean ± SE (adjusted for age)
Different superscripts within the same row are significantly different at α=0.05 by Tukey's range test with age adjusted.
Correlation between parameters existed; IPSS vs QoL (Correlation coefficient = 0.635, P < 0.05), IPSS vs MFR (Correlation coefficient = -0.375, P < 0.05), QoL vs MFR (Correlation coefficient = -0.255, P < 0.05), and prostate volume vs serum PSA (Correlation coefficient = 0.323, P < 0.05).
In the meanwhile, there were no statistically significant differences in all BPH parameters among groups at every treatment time.
Discussion
The use of phytochemicals (phytosterols) as an alternative therapy for the relief of lower urinary tract symptoms due to a prostatic disease seems to be growing quickly all over the world, including the Republic of Korea (Buck, 2004). A phytochemical based therapy is widely given to men with symptomatic BPH in Western Europe, where physicians prescribe phytochemical products in the same manner as they prescribe drugs (Marks et al., 2000).
The results of this study show that the symptoms of BPH for all patients receiving treatment with pumpkin seed oil, saw palmetto oil, or a combination of pumpkin seed oil plus saw palmetto oil were improved over 12 months, in comparison with placebo. But therapeutic efficiency was not improved by combination of these two compounds. During the experimental period, no side effects were reported; this was in contrast with Singh et al. (2007) in similar trials.
According to Braeckman's study (1994), oral doses of saw palmetto oil 160 mg twice daily for 3 months improved IPSS about 22% after 45 days and 35% at 90 days. This was comparable with our result in which group B (33.8%) and group C (33.2%) showed similar improvement after 3 months. In the study by Bach (2000), 12-month pumpkin seed treatment improved the IPSS at least 5 points and overall improvement of 64.8%. In a double-blind randomized trial that compared the effects of saw palmetto (320 mg/day) with 5-α-reductase inhibitor (5 mg/day), the IPSS was declined by 37% and 39%, respectively (Carraro et al., 1996) after 6 months of treatment. Hisashi et al. (2005) reported a significant linear relationship between IPSS and QoL score, a finding in agreement with our own, in which IPSS was correlated exactly with QoL score. Both IPSS and QoL score tended to decline significantly at the 3rd month of treatment in our study, a finding similar to that of other researchers (Nickel, 1998; Willetts et al., 2003).
There have been recent reports suggesting that the serum PSA value may not be the best marker for prostate cancer detection, but it still remains one of the simplest means of early diagnosis and follow-ups for this disease. Serum PSA is also increased in other conditions such as BPH, prostatitis and others (Lee et al., 2005; Mehrabi et al., 2005). Debruyne et al. (2002) showed saw palmetto does not affect serum PSA level within 12 months of treatment. In our study, only a minimal change of PSA was observed within the normal range (0.0~4.0 ng/ml), although a synergistic combination of pumpkin seed oil and saw palmetto oil may have contributed to the decrease of serum PSA level observed in our study.
Braeckman (1994) showed that prostate volume was significantly decreased by 9% after 45 days and 10% after 90 days of treatment with saw palmetto oil. But several of reports demonstrated only a minimal change of prostate volume within 1 year (Marks et al., 2000; Wilt et al., 1998). We also could not detect any significant decrease of the prostate volume even within 12 months.
In a randomized trial of natural products by Preuss et al. (2001), the IPSS was decreased significantly after 90 days, but serum PSA, MFR and PV were not changed. This is in contrast to the present study in which the serum PSA of patients fed the combination of pumpkin seed oil and saw palmetto oil was decreased, and MFR in the pumpkin seed oil group was increased, significantly after 6 months.
In a study by Moon et al. (1990), urinary flow rate of BPH patients supplemented with Sitosterol was increased from a baseline MFR of 9.3 ml/s to 12.2 ml/s after 4 weeks of treatment, and continued to increase consistently for 12 weeks. Kondas et al. (1996) reported that the average MFR was increased from 10.36 ml/s to 14.44 ml/s without any adverse effects after 12 months of treatment with saw palmetto oil . In addition, this treatment did not influence the effectiveness of drugs taken for other chronic diseases by these patients. Carbin et al. (1990) studied the combination of saw palmetto with pumpkin seed oil and reported a significant increase in MFR value in BPH patients after 3 months of treatment. Our study showed a similar effectiveness on MFR in the pumpkin seed oil group and the saw palmetto oil group, but the combination of pumpkin seed oil with saw palmetto oil group did not significantly affect MFR.
The action mechanism of pumpkin seed oil is well known by its inhibition on 5-α-reductase which converts testosterone into DHT (dihydrotestosterone) (Gossell-Williams et al., 2006; Tsai et al., 2006). Meanwhile various action mechanisms are suggested for saw palmetto oil, including nuclear estrogen receptor inhibitor (Di Silverio et al., 1992), inhibition of cyclooxygenase and 5-lipoxygenase pathway (Breu et al., 1992) as well as 5-α-reductase inhibition (Weisser et al., 1996). Recently, epithelial contraction in the prostate transition zone was demonstrated by Marks et al. (2000). According to the difference in action mechanisms, a synergistic effect on BPH was expected from combination treatment of pumpkin seed oil and saw palmetto oil. In our study, combination treatment of pumpkin seed oil and saw palmetto oil induced a higher symptomatic improvement, though not statistically significant, in IPSS, QoL and PSA than a single treatment. A better result is expected by increasing subject numbers and longer observation period as well as in vitro mechanism studies.
Based on the results of this study, it could be suggested that pumpkin seed oil and saw palmetto oil are clinically safe and may be effective complementary and alternative medicine for BPH.
References
- 1.Bach D. Placebo-controlled, long-term therapeutic study of a pumpkin seed extract product in patients with micturition complaints from benign prostatic hyperplasia. Urologe B. 2000;40:437–443. [Google Scholar]
- 2.Barry MJ, Fowler FJ, Jr, Bin L, Pitts JC, 3rd, Harris CJ, Mulley AG., Jr The natural history of patients with benign prostatic hyperplasia as diagnosed by North American urologists. J Urol. 1997;157:10–14. [PubMed] [Google Scholar]
- 3.Braeckman J. The extract of serenoa repens in the treatment of benign prostatic hyperplasia: A multicenter open study. Curr Ther Res. 1994;55:776–785. [Google Scholar]
- 4.Breu W, Hagenlocher M, Redl K, Tittel G, Stadler F, Wagner H. Anti-inflammatory activity of sabal fruit extracts prepared with supercritical carbon dioxide. In vitro antagonists of cyclooxygenase and 5-lipoxygenase metabolism. Arzneimittelforschung. 1992;42:547–551. [PubMed] [Google Scholar]
- 5.Buck AC. Is there a scientific basis for the therapeutic effects of serenoa repens in benign prostatic hyperplasia? Mechanisms of action. J Urol. 2004;172:1792–1799. doi: 10.1097/01.ju.0000140503.11467.8e. [DOI] [PubMed] [Google Scholar]
- 6.Carbin BE, Larsson B, Lindahl O. Treatment of benign prostatic hyperplasia with phytosterols. Br J Urol. 1990;66:639–641. doi: 10.1111/j.1464-410x.1990.tb07199.x. [DOI] [PubMed] [Google Scholar]
- 7.Carraro JC, Raynaud JP, Koch G, Chisholm GD, Di Silverio F, Teillac P, Da Silva FC, Cauquil J, Chopin DK, Hamdy FC, Hanus M, Hauri D, Kalinteris A, Marencak J, Perier A, Perrin P. Comparison of phytotherapy (Permixon) with finasteride in the treatment of benign prostate hyperplasia: a randomized international study of 1,098 patients. Prostate. 1996;29:231–240. doi: 10.1002/(SICI)1097-0045(199610)29:4<231::AID-PROS4>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 8.Cho JS, Kim CI, Seong DH, Kim HS, Kim YS, Kim SJ. Relationship between serum prostate specific antigen and prostate volume in men with benign prostatic hyperplasia from multicenter study. Korean Journal of Urology. 2005;46:792–798. [Google Scholar]
- 9.Cristoni A, Di Pierro F, Bombardelli E. Botanical derivatives for the prostate. Fitoterapia. 2000;71:S21–S28. doi: 10.1016/s0367-326x(00)00174-x. [DOI] [PubMed] [Google Scholar]
- 10.Debruyne F, Koch G, Boyle P, Da Silva FC, Gillenwater JG, Hamdy FC, Perrin P, Teillac P, Vela-Navarrete R, Raynaud JP. Comparison of a phytotherapeutic agent (Permixon) with an alpha-blocker (Tamsulosin) in the treatment of benign prostatic hyperplasia: a 1-year randomized international study. Eur Urol. 2002;41:497–506. [PubMed] [Google Scholar]
- 11.Di Silverio F, D'Eramo G, Lubrano C, Flammia GP, Sciarra A, Palma E, Caponera M, Sciarra F. Evidence that Serenoa repens extract displays an antiestrogenic activity in prostatic tissue of benign prostatic hypertrophy patients. Eur Urol. 1992;21:309–314. doi: 10.1159/000474863. [DOI] [PubMed] [Google Scholar]
- 12.Ernst E. The risk-benefit profile of commonly used herbal therapies: Ginkgo, St. John's Wort, Ginseng, Echinacea, Saw Palmetto, and Kava. Ann Intern Med. 2002;136:42–53. doi: 10.7326/0003-4819-136-1-200201010-00010. [DOI] [PubMed] [Google Scholar]
- 13.Gossell-Williams M, Davis A, O'Connor N. Inhibition of testosterone-induced hyperplasia of the prostate of sprague-dawley rats by pumpkin seed oil. J Med Food. 2006;9:284–286. doi: 10.1089/jmf.2006.9.284. [DOI] [PubMed] [Google Scholar]
- 14.Hirsch IH. Integrative urology: a spectrum of complementary and alternative therapy. Urology. 2000;56:185–189. doi: 10.1016/s0090-4295(00)00610-5. [DOI] [PubMed] [Google Scholar]
- 15.Hisashi H, Masahiro N, Yoshifumi S, Kenichi T, Hiroshi K, Tsuneharu M. Prevalence of lower urinary tract symptoms and seeking acupuncture treatment in men and women aged years or older: A community-based epidemiological study in Japan. Japanese Acupuncture and Moxibustion. 2005;1:27–35. [Google Scholar]
- 16.Kondas J, Philipp V, Dioszeghy G. Sabal serrulata extract (Strogen forte) in the treatment of symptomatic benign prostatic hyperplasia. Int Urol Nephrol. 1996;28:767–772. doi: 10.1007/BF02550725. [DOI] [PubMed] [Google Scholar]
- 17.Lee DH, Yang WJ, Chung BH, Kim SI, Kim SJ, Kim HS. A multicenter study of the detection rate for prostate cancer according to the serum prostate specific antigen level in Korean men. Korean Journal of Urology. 2005;46:433–437. [Google Scholar]
- 18.Lee S, Min HG, Choi SH, Kim YJ, Oh SW, Park Y, Kim SS. Central obesity as a risk factor for prostatic hyperplasia. Obesity (Silver Spring) 2006;14:172–179. doi: 10.1038/oby.2006.21. [DOI] [PubMed] [Google Scholar]
- 19.Marks LS, Partin AW, Epstein JI, Tyler VE, Simon I, Macairan ML, Chan TL, Dorey FJ, Garris JB, Veltri RW, Santos PB, Stonebrook KA, deKernion JB. Effects of a saw palmetto herbal blend in men with symptomatic benign prostatic hyperplasia. J Urol. 2000;163:1451–1456. [PubMed] [Google Scholar]
- 20.Mehrabi S, Shirazi HG, Rastim M, Bayat B. Analysis of serum prostate-specific antigen levels in men aged 40 years and older in yasuj, Iran. Urol J. 2005;2:189–192. [PubMed] [Google Scholar]
- 21.Melo EA, Bertero EB, Rios LA, Mattos D., Jr Evaluating the efficiency of a combination of Pygeum africanum and stinging nettle (Urtica dioica) extracts in treating benign prostatic hyperplasia (BPH): double-blind, randomized, placebo controlled trial. Int Braz J Urol. 2002;28:418–425. [PubMed] [Google Scholar]
- 22.Moon YT, Oh CH, Kim SC. Clinical effect of Sitosterol (PronalR) on the treatment of benign prostatic hypertrophy. Korean Journal of Andrology. 1990;8:23–29. [Google Scholar]
- 23.Nickel JC Canadian PROSPECT Study Group. Placebo therapy of benign prostatic hyperplasia: a 25-month study. Br J Urol. 1998;81:383–387. doi: 10.1046/j.1464-410x.1998.00554.x. [DOI] [PubMed] [Google Scholar]
- 24.Ortiz MV. Alternative medicine: Incorporation into therapeutics topics. Am J Pharm Educ. 1998;62:208–212. [Google Scholar]
- 25.Pathak SK, Sharma RA, Mellon JK. Chemoprevention of prostate cancer by diet-derived antioxidant agents and hormonal manipulation (Review) Int J Oncol. 2003;22:5–13. [PubMed] [Google Scholar]
- 26.Preuss HG, Marcusen C, Regan J, Klimberg IW, Welebir TA, Jones WA. Randomized trial of a combination of natural products (cernitin, saw palmetto, B-sitosterol, vitamin E) on symptoms of benign prostatic hyperplasia (BPH) Int Urol Nephrol. 2001;33:217–225. doi: 10.1023/a:1015227604041. [DOI] [PubMed] [Google Scholar]
- 27.Shoskes DA. Phytotherapy in chronic prostatitis. Urology. 2002;60:35–37. doi: 10.1016/s0090-4295(02)02383-x. [DOI] [PubMed] [Google Scholar]
- 28.Singh YN, Devkota AK, Sneeden DC, Singh KK, Halaweish F. Hepatotoxicity potential of saw palmetto (Serenoa repens) in rats. Phytomedicine. 2007;14:204–208. doi: 10.1016/j.phymed.2006.03.024. [DOI] [PubMed] [Google Scholar]
- 29.Tsai YS, Tong YC, Cheng JT, Lee CH, Yang FS, Lee HY. Pumpkin seed oil and phytosterol-F can block testosterone/prazosin-induced prostate growth in rats. Urol Int. 2006;77:269–274. doi: 10.1159/000094821. [DOI] [PubMed] [Google Scholar]
- 30.Vickers A. Recent advances: complementary medicine. BMJ. 2000;321:683–686. doi: 10.1136/bmj.321.7262.683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Watson V, Ryan M, Brown CT, Barnett G, Ellis BW, Emberton M. Eliciting preferences for drug treatment of lower urinary tract symptoms associated with benign prostatic hyperplasia. J Urol. 2004;172:2321–2325. doi: 10.1097/01.ju.0000140957.31325.7f. [DOI] [PubMed] [Google Scholar]
- 32.Weisser H, Tunn S, Behnke B, Krieg M. Effects of the Sabal serrulata extract IDS 89 and its subfraction on 5 alpha-reductase activity in human benign prostatic hyperplasia. Prostate. 1996;28:300–306. doi: 10.1002/(SICI)1097-0045(199605)28:5<300::AID-PROS5>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 33.Willetts KE, Clements MS, Champion S, Ehsman S, Eden JA. Serenoa repens extract for benign prostate hyperplasia: a randomized controlled trial. BJU Int. 2003;92:267–270. doi: 10.1046/j.1464-410x.2003.04316.x. [DOI] [PubMed] [Google Scholar]
- 34.Wilt TJ, Ishani A, Rutks I, MacDonald R. Phytotherapy for benign prostatic hyperplasia. Public Health Nutr. 2000;3:459–472. doi: 10.1017/s1368980000000549. [DOI] [PubMed] [Google Scholar]
- 35.Wilt TJ, Ishani A, Stark G, MacDonald R, Lau J, Mulrow C. Saw Palmetto extracts for treatment of benign prostatic hyperplasia. JAMA. 1998;280:1604–1609. doi: 10.1001/jama.280.18.1604. [DOI] [PubMed] [Google Scholar]
- 36.Wilt TJ, MacDonald R, Ishani A. beta-sitosterol for the treatment of benign prostatic hyperplasia: a systematic review. BJU Int. 1999;83:976–983. doi: 10.1046/j.1464-410x.1999.00026.x. [DOI] [PubMed] [Google Scholar]
- 37.Zhang W, Wang X, Liu Y, Tian H, Flickinger B, Empie MW, Sun SZ. Effects of dietary flaxseed lignan extract on symptoms of benign prostatic hyperplasia. J Med Food. 2008;11:207–214. doi: 10.1089/jmf.2007.602. [DOI] [PubMed] [Google Scholar]