Abstract
OBJECTIVE
Several studies have suggested an association between specific diabetes treatment and cancer mortality. We studied the association between metformin use and cancer mortality in a prospectively followed cohort.
RESEARCH DESIGN AND METHODS
In 1998 and 1999, 1,353 patients with type 2 diabetes were enrolled in the Zwolle Outpatient Diabetes project Integrating Available Care (ZODIAC) study in the Netherlands. Vital status was assessed in January 2009. Cancer mortality rate was evaluated using standardized mortality ratios (SMRs), and the association between metformin use and cancer mortality was evaluated with a Cox proportional hazards model, taking possible confounders into account.
RESULTS
Median follow-up time was 9.6 years, average age at baseline was 68 years, and average A1C was 7.5%. Of the patients, 570 died, of which 122 died of malignancies. The SMR for cancer mortality was 1.47 (95% CI 1.22–1.76). In patients taking metformin compared with patients not taking metformin at baseline, the adjusted hazard ratio (HR) for cancer mortality was 0.43 (95% CI 0.23–0.80), and the HR with every increase of 1 g of metformin was 0.58 (95% CI 0.36–0.93).
CONCLUSIONS
In general, patients with type 2 diabetes are at increased risk for cancer mortality. In our group, metformin use was associated with lower cancer mortality compared with nonuse of metformin. Although the design cannot provide a conclusion about causality, our results suggest a protective effect of metformin on cancer mortality.
Much debate has arisen recently after an online publication stated that insulin glargine might be associated with an increased cancer risk (1). Soon after this publication, the European Medicines Agency issued a statement that changes to the prescribing advice were not necessary. This initially disturbing news overshadowed positive news regarding the relation between metformin and cancer risk (2). If metformin indeed decreases cancer mortality risk, it would further strengthen the position of metformin as the preferred initial treatment in patients with type 2 diabetes.
In general, there is evidence that type 2 diabetes alters the risk of developing a variety of cancers (3–7) and that cancer mortality is increased (8). Glucose-lowering therapy itself could also be associated with cancer risk. For example, the risk for colon cancer seemed to be increased in patients using insulin (9). However, the quality and validity of that study are questionable.
Insulin is a growth-promoting hormone with mitogenic effects, and it has been suggested that hyperinsulinemia promotes carcinogenesis (10). Conversely, metformin may have protective effects on cancer development. Metformin targets AMP-activated protein kinase, which induces glucose uptake in muscles. Activation of AMP-activated protein kinase requires LKB1, a well-known tumor suppressor. The relationship between metformin and LKB1 could therefore be an explanation for the potential beneficial effects of metformin on cancer development (11).
Two previous studies showed that cancer risk was lower in patients exposed to metformin than in unexposed patients (12,13). Metformin has also been shown to be potentially beneficial in patients with specific types of cancer. For example, type 2 diabetic patients receiving neoadjuvant chemotherapy for breast cancer as well as metformin were more likely to have a complete remission than patients not receiving metformin (14). Furthermore, patients receiving metformin seem to have a lower incidence of prostate and pancreatic cancer (15,16).
In the only study designed to evaluate cancer mortality, treatment with a sulfonylurea drug and insulin was associated with an increased risk of cancer-related mortality compared with treatment with metformin (17). These results are somewhat questionable, because in this study a limited set of confounders was used in the multivariate analyses. For instance, the BMI of the patients was not taken into account. Furthermore, the design of this trial was retrospective. We aimed to study the effect of metformin on cancer mortality in a prospectively designed cohort of type 2 diabetic patients in primary care.
RESEARCH DESIGN AND METHODS
The present study is part of the Zwolle Outpatient Diabetes project Integrating Available Care (ZODIAC) study (18), which started in 1998 and is part of a diabetes shared care project. In this project, general practitioners are assisted in their care of type 2 diabetic patients by hospital-based diabetes specialist nurses. At baseline, patients with a very short life expectancy (including patients with active cancer) or insufficient cognitive abilities were excluded from this study. Therefore, general practitioners excluded 5% of patients treated in primary care from participating in the study. Nearly 90% (n = 1,357) of the remaining patients agreed to participate, but 4 patients were also excluded because of insufficient baseline data. The ZODIAC study was approved by the medical ethics committee of the Isala Clinics in Zwolle, the Netherlands.
Data collection
Baseline data were collected in 1998 and 1999 and consisted of a medical history, including macrovascular complications, diabetes duration, medication use, and tobacco consumption. Laboratory and physical assessment data were collected annually and included the following variables: A1C, nonfasting lipid profile, serum creatinine, urinary albumin-to-creatinine ratio, blood pressure, weight, and height. At the beginning of 2009, life status and cause of death were retrieved from records maintained by the hospital and general practitioners. Thirteen baseline variables were selected for their possible confounding effects in the relationship between metformin use and cancer mortality: smoking (yes or no), age, sex, diabetes duration, A1C, serum creatinine, BMI, blood pressure, total cholesterol–to–HDL ratio, albuminuria, insulin use, sulfonylurea use, and macrovascular complications (yes or no).
Statistical analysis
To study the incidence of cancer mortality, standardized mortality ratios (SMRs) were calculated for total mortality and cardiovascular and cancer mortality using general mortality reference rates from the Netherlands (http://statline.cbs.nl/StatWeb/). SMRs were also calculated for metformin users and nonusers. We used a Cox proportional hazards model to investigate the association between metformin use and cancer mortality with and without adjustment of the selected confounders. We used two different models. In model 1, the 13 earlier mentioned baseline variables were taken into account as possible confounders. This model thus included factors associated with both cardiovascular mortality and cancer mortality. Model 2 included factors directly related to cancer mortality: age, sex, BMI, insulin use, and sulfonylurea use.
To evaluate the relationship with dose of metformin, we repeated the analyses and included the dose of metformin per day as a continuous variable. Adjustments were made for all covariates.
We also investigated which variable was an actual confounder in the relation between metformin and cancer mortality. Confounding was defined as a 10% change in the β coefficient of the hazard ratio (HR). We created interaction terms for all variables with metformin. The proportional hazards assumption was examined using log (−log) survival plots. The parallel lines in the plots indicate that the assumption was met. All tests were two-sided, and analyses were performed with SPSS (version 15.0.1; SPSS, Chicago, IL).
RESULTS
The baseline characteristics of the study population are shown in Table 1. After a median follow-up time of 9.6 years, a total of 570 (42%) patients had died. There were 122 (21%) cancer deaths, of which 26 (21%) related to lung cancer and 21 (17%) to abdominal cancer. A total of 238 (41%) patients had died of cardiovascular disease.
Table 1.
Baseline characteristics
| Characteristics | Total | Metformin users | No metformin use |
|---|---|---|---|
| n | 1,353 | 289 | 1,064 |
| Age (years) | 67.8 ± 11.7 | 67.3 ± 10.6 | 68.0 ± 12.0 |
| Female sex (%) | 57.6 | 61.2 | 56.5 |
| Diabetes duration (years) | 6.0 (3–11) | 4.9 (3–11) | 7.1 (4–12) |
| Smoking (%) | 18.6 | 19.2 | 18.4 |
| BMI (kg/m2) | 28.9 ± 4.8 | 29.6 ± 5.1 | 28.8 ± 4.6* |
| Systolic blood pressure (mmHg) | 153.0 ± 25.2 | 154.3 ± 24.9 | 153.6 ± 25.3 |
| A1C (%) | 7.5 ± 1.2 | 7.7 ± 1.1 | 7.4 ± 1.3* |
| eGFR (ml/min per 1.73 m2) | 73.9 ± 28.1 | 76.9 ± 30.0 | 73.0 ± 27.6† |
| Total cholesterol–to–HDL ratio | 5.2 ± 1.6 | 5.3 ± 1.6 | 5.1 ± 1.5 |
| Albumin-to-creatinine ratio | 2.2 (1.0–7.2) | 2.6 (1.1–9.4) | 2.1 (1.0–6.8) |
| Macrovascular complications (%) | 32.7 | 35.3 | 32.1 |
| Insulin use (%) | 16.5 | 5.9 | 19.3‡ |
| Sulfonylurea use (%) | 55.0 | 15.9 | 65.8‡ |
| Diet only (%) | 13.0 |
Data are means ± SD, median (interquartile range) for nonnormally distributed data, or %.
*P < 0.01;
†P < 0.05;
‡P < 0.001, two-sided parametric test (Student t) and nonparametric test (Mann-Whitney U) as appropriate. eGFR, estimated glomerular filtration rate.
The cause of death was known for 541 (94%) patients. Life status of 20 patients (1.5%) could not be obtained. Data on medication use were complete for 1,350 patients (>99%).
SMRs
The SMR for total mortality was 2.22 (95% CI 2.03–2.42), for cardiovascular mortality was 2.45 (2.15–2.79), and for cancer mortality was 1.47 (1.22–1.76). The SMR for cancer mortality in the nonmetformin group was 1.62 (1.32–1.96). The SMR for cancer mortality in the metformin group was 0.88 (0.51–1.44).
Cancer mortality
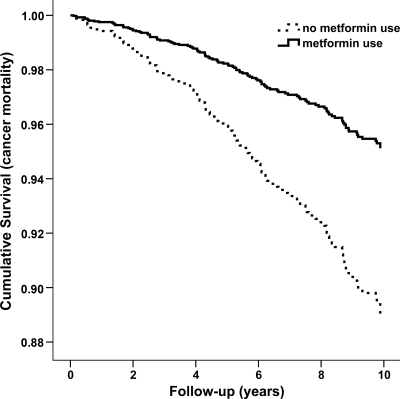
The unadjusted HR of metformin use for cancer mortality was 0.54 (95% CI 0.32–0.91). For model 1, taking all 13 possible variables into account, the adjusted HR of metformin use for cancer mortality was 0.43 (0.23–0.80) (Fig. 1). The adjusted HR for model 2 was 0.46 (0.26–0.83). There were no significant interaction terms between metformin and cancer mortality. Furthermore, only sulfonylurea use and macrovascular complications were confounders in the relationship between metformin use and cancer mortality. With adjustment only for macrovascular complications and sulfonylurea, the outcome did not change. Furthermore, after exclusion of mortality in the first 3 years after baseline, the results remained similar (HR 0.38 [95% CI 0.18–0.81]). Sulfonylurea use was not significantly associated with cancer mortality (0.69 [0.36–1.34]) nor was insulin use (0.70 [0.36–1.34]).
Figure 1.
Cumulative survival curve for cancer mortality.
Dose-response analysis
The HR of metformin as a continuous variable for cancer mortality was 0.58 (95% CI 0.36–0.93). The hazard for cancer mortality decreased by 42% for every 1-g increase in the metformin dose.
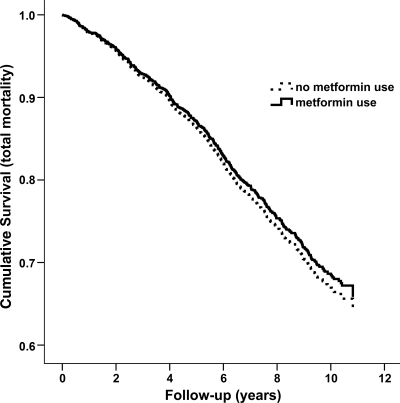
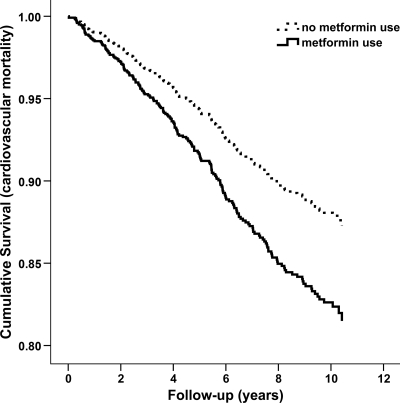
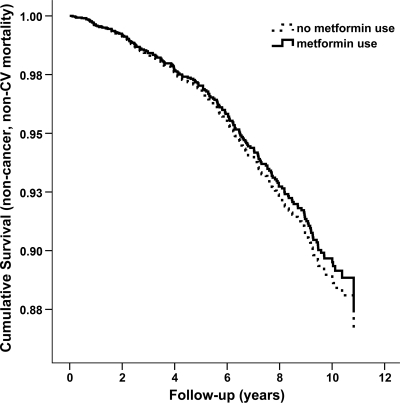
All-cause and cardiovascular mortality
After adjustment for all covariates, the HRs for total and cardiovascular mortality among metformin users were 0.94 (95% CI 0.73–1.22) and 2.27 (1.36–3.78), respectively (Figs. 2 and 3). The HR for all other causes of death was 0.97 (0.72–1.30) (Fig. 4). A significant interaction between metformin and sulfonylurea use was observed in the cardiovascular mortality analysis and an interaction term was added to the model. The proportional hazard assumptions were met for all analyses.
Figure 2.
Cumulative survival curve for total mortality.
Figure 3.
Cumulative survival for cardiovascular mortality.
Figure 4.
Cumulative survival for non-cancer and non-cardiovascular (CV) (all other causes) mortality.
CONCLUSIONS
For the first time in a prospective study, we found (after a median follow-up time of 9.6 years) that metformin use at baseline was associated with less cancer-related mortality and that this association appeared to be dose-dependent. Patients with type 2 diabetes who were not taking metformin showed an increased cancer mortality ratio compared with that for the general population. The mortality of patients taking metformin was comparable with that for the general population.
A study by Currie et al. (2) suggested an increased cancer risk for patients taking insulin and with metformin a decrease in this risk to a level as observed in the general population. Another study, in which population-based sampling was used, showed a reduced cancer risk for patients taking metformin compared with patients taking a sulfonylurea drug (12). The researchers suggested a dose-response relation: the greater the metformin exposure, the stronger the risk reduction. It is not clear whether the researchers excluded or adjusted for the use of insulin in this study. A third study, a large administrative database study, showed that patients exposed to a sulfonylurea drug and insulin were more likely to have a cancer-related death than patients using metformin (17). The researchers of this retrospective study had no data about cardiovascular mortality and did not adjust for some essential confounders such as BMI and smoking.
Our study has some notable strengths. First, our study is the first observational study with a prospective design investigating the relation between metformin and cancer (mortality). Second, we adjusted for more potential confounders than the researchers in the previous study (17). Third, we were able to present data on non–cancer-related mortality and compared our results with those for the general population in the Netherlands. Fourth, the number of deaths in the 10-year follow-up period was sufficient to make reliable estimates regarding associations with mortality. If there is an association between cancer mortality and metformin use, a long-term follow-up is needed, because cancer takes a long time to develop, and it takes time before patients die of cancer.
There are, of course, also limitations to our study. Cancer mortality depends on the type and aggressiveness of the cancer and the effectiveness of the cancer treatment. Unfortunately, data concerning nonfatal cancer incidence are lacking in the ZODIAC study. Diabetes or diabetes treatment may have an effect on the intensity of the cancer treatment or on the choice of a specific cancer treatment regimen. Furthermore, no adjustment could be made for a history of cancer in our analyses because these data were imprecise. However, after excluding the first 3 years of follow-up from the analysis, the relationship remained highly significant. Excluding the first 3 years of follow-up could correct for undiagnosed cancer at the start of the study, which could influence outcome. Furthermore, we were not able to perform analyses for site-specific cancers, because our analyses were based on only 122 cancer deaths. Finally, the study started in 1998. At that time, metformin was not a first-choice treatment, a fact that is also confirmed by the relatively small group of patients using metformin at baseline.
Patients who were taking metformin at the beginning of this study (in 1998) might also be different from patients taking metformin at this time. Patients taking metformin had an increased risk for cardiovascular mortality after 10 years. A possible explanation is that their cardiovascular disease risk was higher at baseline. For example, metformin users had a higher BMI compared with nonusers.
Our study confirms that the cancer mortality risk for metformin users is lower compared with that of nonusers. In our opinion, this finding further strengthens the position of metformin as the treatment of first choice in patients with type 2 diabetes. Further research is needed to establish whether metformin is a definite beneficial causal factor in lowering the risk of cancer mortality.
Acknowledgments
No potential conflicts of interest relevant to this article were reported.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1.Hemkens LG, Grouven U, Bender R, Günster C, Gutschmidt S, Selke GW, Sawicki PT. Risk of malignancies in patients with diabetes treated with human insulin or insulin analogues: a cohort study. Diabetologia 2009; 52: 1732– 1744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Currie CJ, Poole CD, Gale EA. The influence of glucose-lowering therapies on cancer risk in type 2 diabetes. Diabetologia 2009; 52: 1766– 1777 [DOI] [PubMed] [Google Scholar]
- 3.Calle EE, Murphy TK, Rodriguez C, Thun MJ, Heath CW., Jr Diabetes mellitus and pancreatic cancer mortality in a prospective cohort of United States adults. Cancer Causes Control 1998; 9: 403– 410 [DOI] [PubMed] [Google Scholar]
- 4.Will JC, Vinicor F, Calle EE. Is diabetes mellitus associated with prostate cancer incidence and survival? Epidemiology 1999; 10: 313– 318 [PubMed] [Google Scholar]
- 5.Chow WH, Gridley G, Nyrén O, Linet MS, Ekbom A, Fraumeni JF, Jr, Adami HO. Risk of pancreatic cancer following diabetes mellitus: a nationwide cohort study in Sweden. J Natl Cancer Inst 1995; 87: 930– 931 [DOI] [PubMed] [Google Scholar]
- 6.Hu FB, Manson JE, Liu S, Hunter D, Colditz GA, Michels KB, Speizer FE, Giovannucci E. Prospective study of adult onset diabetes mellitus (type 2) and risk of colorectal cancer in women. J Natl Cancer Inst 1999; 91: 542– 547 [DOI] [PubMed] [Google Scholar]
- 7.Adami HO, Chow WH, Nyrén O, Berne C, Linet MS, Ekbom A, Wolk A, McLaughlin JK, Fraumeni JF., Jr Excess risk of primary liver cancer in patients with diabetes mellitus. J Natl Cancer Inst 1996; 88: 1472– 1477 [DOI] [PubMed] [Google Scholar]
- 8.Coughlin SS, Calle EE, Teras LR, Petrelli J, Thun MJ. Diabetes mellitus as a predictor of cancer mortality in a large cohort of US adults. Am J Epidemiol 2004; 159: 1160– 1167 [DOI] [PubMed] [Google Scholar]
- 9.Yang YX, Hennessy S, Lewis JD. Insulin therapy and colorectal cancer risk among type 2 diabetes mellitus patients. Gastroenterology 2004; 127: 1044– 1050 [DOI] [PubMed] [Google Scholar]
- 10.van der Burg B, Rutteman GR, Blankenstein MA, de Laat SW, van Zoelen EJ. Mitogenic stimulation of human breast cancer cells in a growth factor–defined medium: synergistic action of insulin and estrogen. J Cell Physiol 1988; 134: 101– 108 [DOI] [PubMed] [Google Scholar]
- 11.Ben Sahra I, Laurent K, Loubat A, Giorgetti-Peraldi S, Colosetti P, Auberger P, Tanti JF, Le Marchand-Brustel Y, Bost F. The antidiabetic drug metformin exerts an antitumoral effect in vitro and in vivo through a decrease of cyclin D1 level. Oncogene 2008; 27: 3576– 3586 [DOI] [PubMed] [Google Scholar]
- 12.Evans JM, Donnelly LA, Emslie-Smith AM, Alessi DR, Morris AD. Metformin and reduced risk of cancer in diabetic patients. BMJ 2005; 330: 1304– 1305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Libby G, Donnelly LA, Donnan PT, Alessi DR, Morris AD, Evans JM. New users of metformin are at low risk of incident cancer: a cohort study among people with type 2 diabetes. Diabetes Care 2009; 32: 1620– 1625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jiralerspong S, Palla SL, Giordano SH, Meric-Bernstam F, Liedtke C, Barnett CM, Hsu L, Hung MC, Hortobagyi GN, Gonzalez-Angulo AM. Metformin and pathologic complete responses to neoadjuvant chemotherapy in diabetic patients with breast cancer. J Clin Oncol 2009; 27: 3297– 3302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wright JL, Stanford JL. Metformin use and prostate cancer in Caucasian men: results from a population-based case-control study. Cancer Causes Control 2009; 20: 1617– 1622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li D, Yeung SC, Hassan MM, Konopleva M, Abbruzzese JL. Antidiabetic therapies affect risk of pancreatic cancer. Gastroenterology 2009; 137: 482– 488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bowker SL, Majumdar SR, Veugelers P, Johnson JA. Increased cancer-related mortality for patients with type 2 diabetes who use sulfonylureas or insulin. Diabetes Care 2006; 29: 254– 258 [DOI] [PubMed] [Google Scholar]
- 18.Ubink-Veltmaat LJ, Bilo HJ, Groenier KH, Rischen RO, Meyboom-de Jong B. Shared care with task delegation to nurses for type 2 diabetes: prospective observational study. Neth J Med 2005; 63: 103– 110 [PubMed] [Google Scholar]