Abstract
OBJECTIVE
Obesity is associated with monocyte-macrophage accumulation in adipose tissue. Previously, we showed that glucose-stimulated production by adipocytes of serum amyloid A (SAA), monocyte chemoattractant protein (MCP)-1, and hyaluronan (HA) facilitated monocyte accumulation. The current objective was to determine how the other major nutrient, free fatty acids (FFAs), affects these molecules and monocyte recruitment by adipocytes.
RESEARCH DESIGN AND METHODS
Differentiated 3T3-L1, Simpson-Golabi-Behmel syndrome adipocytes, and mouse embryonic fibroblasts were exposed to various FFAs (250 μmol/l) in either 5 or 25 mmol/l (high) glucose for evaluation of SAA, MCP-1, and HA regulation in vitro.
RESULTS
Saturated fatty acids (SFAs) such as laurate, myristate, and palmitate increased cellular triglyceride accumulation, SAA, and MCP-1 expression; generated reactive oxygen species (ROS); and increased nuclear factor (NF) κB translocation in both 5 and 25 mmol/l glucose. Conversely, polyunsaturated fatty acids (PUFAs) such as arachidonate, eicosapentaenate, and docosahexaenate (DHA) decreased these events. Gene expression could be dissociated from triglyceride accumulation. Although excess glucose increased HA content, SFAs, oleate, and linoleate did not. Antioxidant treatment repressed glucose- and palmitate-stimulated ROS generation and NFκB translocation and decreased SAA and MCP-1 expression and monocyte chemotaxis. Silencing toll-like receptor-4 (TLR4) markedly reduced SAA and MCP-1 expression in response to palmitate but not glucose. DHA suppressed NFκB translocation stimulated by both excess glucose and palmitate via a peroxisome prolifterator–activated receptor (PPAR) γ–dependent pathway.
CONCLUSIONS
Excess glucose and SFAs regulate chemotactic factor expression by a mechanism that involves ROS generation, NFκB, and PPARγ, and which is repressed by PUFAs. Certain SFAs, but not excess glucose, trigger chemotactic factor expression via a TLR4-dependent pathway.
Macrophage accumulation in adipose tissue is a hallmark of obesity (1–3). Adipose tissue macrophages have been implicated in the pathogenesis of insulin resistance and systemic inflammation (4–6). However, the mechanism by which monocytes are recruited into adipose tissue to become macrophages remains elusive. While monocyte chemoattractant protein (MCP)-1 has been proposed as a key monocyte chemoattractant (2,7,8), recent studies have found that neither MCP-1 (9) nor its receptor C-C motif chemokine receptor 2 (10) are required for adipose tissue macrophage accumulation. Therefore, other mechanisms must exist. We recently described another monocyte recruitment pathway responsible for macrophage accumulation in adipose tissue (i.e., a complex containing both an extrahepatic serum amyloid A [SAA] isoform, SAA3, and hyaluronan [HA]). SAA3 is chemotactic for monocytes, whereas HA acts as a scaffold to which both monocytes and SAA3 adhere (11).
Previously, we showed that glucose-induced adipocyte hypertrophy increased expression of SAA3, MCP-1, and hyaluronan synthase (HAS) 2, the enzyme responsible for HA synthesis in adipocytes, via a nuclear factor (NF) κB and peroxisome prolifterator–activated receptor (PPAR) γ–dependent mechanism (11). We also demonstrated that this pathway increases in susceptible mice fed diets rich in saturated fatty acids (SFAs) and refined sugar (11). Moreover, others have shown that obesity resulting from excess SFA consumption leads to insulin resistance via a toll-like receptor-4 (TLR4)-dependent pathway (12,13). Obesity occurs when excess nutrients derived from glucose and/or fatty acids accumulate in adipose tissue. However, little is known about the effects of different classes of long-chain FFAs on SAA, MCP-1, and HAS2 expression in adipocytes.
By exposing differentiated adipocytes to various long-chain FFAs, we have shown that specific SFAs stimulate monocyte chemotaxis, whereas specific polyunsaturated fatty acids (PUFAs) inhibit these monocyte recruitment pathways. Moreover, glucose and specific SFAs appear to share a common pathway for macrophage accumulation in adipose tissue.
RESEARCH DESIGN AND METHODS
Reagents and detailed methods are described in an online appendix, which can be found at http://diabetes.diabetesjournals.org/cgi/content/full/db09-0925/DC1.
Cell culture.
3T3-L1 murine preadipocytes, obtained from American Type Tissue Culture Collection, and mouse embryonic fibroblasts (MEFs), isolated from embryos of C57BL/6 mice at 13.5 days postcoitum (a gift from Dr. Carol B. Ware, University of Washington), were propagated and differentiated according to standard protocol procedures (14), with the exception that media containing either 5 or 25 mmol/l glucose with or without 250 μmol/l FFAs were replenished daily. Human preadipocytes from Simpson-Golabi-Behmel syndrome (SGBS) were grown and differentiated, as described previously (15), with daily replenishment of media containing either 5 or 25 mmol/l glucose with or without 250 μmol/l FFAs. U937 and THP-1 monocytic cell lines were cultured in RPMI-1640 medium for use in the monocyte adhesion and chemotaxis assays, respectively.
In vitro TLR4 gene silencing.
To test the role of TLR4-mediated SAA3 and MCP-1 expression, 3T3-L1 adipocytes were transiently transfected (2 days after completion of the differentiation protocol) with small-interfering RNA (siRNA) duplexes for TLR4 synthesized and purified by Ambion using the DeliverX system (Panomics), as described previously (11,16).
Reactive oxygen species quantification.
Reactive oxygen species (ROS) generation was assessed as CM-H2DCFDA (Molecular Probes) fluorescence, which was monitored by fluorescence-activated cell sorting (FACS) (FACScan, Becton Dickinson), as described previously (17).
Multiplex real-time quantitative reverse-transcription PCR.
Real-time reverse-transcription PCR (RT-PCR) was performed using the TaqMan Master kit (Applied Biosystems) in the Stratagene MX3000P system (16) (online appendix).
Western blot analysis.
Differentiated mouse 3T3-L1 and human SGBS adipocytes were cultured in medium containing 5 or 25 mmol/l glucose with or without 250 μmol/l FFAs. After incubation, culture media were collected and proteins separated in 10–20% gradient SDS-PAGE for Western blot analysis using an anti-mouse SAA3 antibody (a generous gift from Dr. Philipp E. Scherer, University of Texas, Southwestern) (11) for the 3T3-L1 cells or an anti-human SAA1 antibody (Anogen, Ontario, Canada) for the SGBS cells.
Monocyte adhesion assay.
Monocyte adhesion to 3T3-L1 adipocytes was assessed using U937 cells, as described previously (18) (online appendix).
Monocyte chemotaxis assay.
The chemotactic activity of conditioned media from 3T3-L1 adipocytes grown in 5 or 25 mmol/l glucose with or without 250 μmol/l FFAs was studied in a 96-well microchamber (ChemoTx; Neuro Probe), as described previously (19) (online appendix).
FACS analysis for cell death.
Since specific FFAs can elicit apoptosis (20), we also measured cell death in adipocytes cultured in 5 or 25 mmol/l glucose with or without FFAs by FACS (online appendix).
Statistical analysis.
Statistical significance was determined by Student's t tests. Data are reported as means ± SD of two or three independent experiments performed in triplicate. P < 0.05 was considered significant.
RESULTS
Adipocyte hypertrophy after exposure of differentiated 3T3-L1 cells to excess glucose and FFAs.
To mimic the metabolic milieu that promotes obesity, a condition of chronic energy excess, we exposed differentiated 3T3-L1 and SGBS adipocytes and adipocytes differentiated from MEFs to high glucose concentrations and/or FFAs. We have shown previously that 3T3-L1 adipocytes exhibit increased hypertrophy following exposure to 25 mmol/l (11). In this study, daily replenishment of medium for 7 days with the SFAs, laurate (12:0), myristate (14:0), palmitate (16:0), and stearate (18:0), and the monounsaturated fatty acid, oleate (18:1), all induced adipocyte hypertrophy in both 5 and 25 mmol/l glucose. However, the n-6 PUFAs, linoleate (18:2) and arachidonate (C20:4), and the n-3 PUFAs, eicosapentaenoate (EPA; 20:5) and docosahexaenoate (DHA; 22:6), decreased lipid droplet size induced by 25 mmol/l glucose (supplemental Fig. 1). These findings are similar to the reduction of glucose-induced adipocyte hypertrophy by the PPARγ agonist, rosiglitazone (11). Triglyceride content was increased by 25 mmol/l glucose, each of the SFAs, and oleic acid. Triglycerides increased in an additive fashion with a combination of 25 mmol/l glucose and either SFAs or oleic acid. In contrast, n-3 and n-6 PUFAs decreased triglyceride content, even in the presence of 25 mmol/l glucose (supplemental Fig. 1). Thus, the FFAs studied have divergent effects on adipocyte hypertrophy. As with 3T3-L1 adipocytes, laurate, palmitate, stearate, and oleate induced, while DHA decreased, adipocyte hypertrophy in human SGBS adipocytes (supplemental Fig. 1) and adipocytes differentiated from MEFs (data not shown).
SAA and MCP-1 expression.
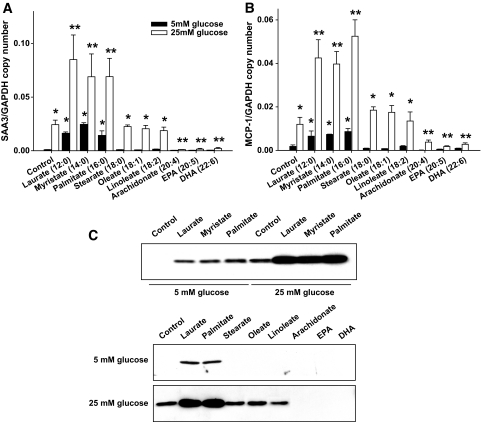
Previously we have shown that 25 mmol/l, but not 5 mmol/l, glucose upregulated SAA3 and MCP-1 mRNA expression in differentiated 3T3-L1 cells time dependently (11). We now exposed differentiated 3T3-L1 adipocytes to various FFAs for 7 days in both 5 and 25 mmol/l glucose with daily media replenishment. The SFAs, laurate, myristate, and palmitate, all increased SAA3 and MCP-1 mRNA levels in both 5 and 25 mmol/l glucose (Fig. 1A and B). SAA3 mRNA was increased in a dose- and time-dependent manner by exposure to palmitate, with increased expression observed by 24 h (data not shown). Linoleate neither stimulated gene expression nor caused cellular hypertrophy. Despite inducing adipocyte hypertrophy, neither stearate nor oleate altered SAA3 and MCP-1 gene expression (Fig. 1A and B). Thus, chemotactic factor gene stimulation and adipocyte hypertrophy can be dissociated. Arachidonate, EPA, and DHA decreased glucose-induced expression of SAA3 and MCP-1 (Fig. 1A and B), similar to results observed with rosiglitazone (11).
FIG. 1.
SAA3 and MCP-1 expression is stimulated by specific SFAs and inhibited by specific PUFAs. 3T3–L1 adipocytes were differentiated in 5 or 25 mmol/l glucose and cultured for 7 days in the same medium with various FFAs (250 μmol/l). Total RNA was isolated and analyzed by multiplex real-time RT-PCR using SAA3-specific (A) or MCP-1–specific (B) primers and probes and normalized to GAPDH. C: Conditioned media were analyzed by immunoblot using anti-SAA3 antibody. *P < 0.001 vs. 5 mmol/l glucose control. **P < 0.001 vs. 25 mmol/l glucose control.
As for mRNA expression, SAA3 protein levels by immunoblot increased after exposure to 25 mmol/l glucose, laurate, myristate, and palmitate and decreased after exposure to arachidonate, EPA, and DHA (Fig. 1C). No changes in SAA protein were observed with stearate, oleate, and linoleate. Thus, effects on gene expression also were seen at the level of protein expression.
To extend the observation in 3T3-L1 adipocytes to other adipocyte-like cells, differentiated human SGBS adipocytes and MEFs also were studied. Since the isoform of SAA produced by human adipocytes is SAA1 rather than SAA3 (21), SAA1 mRNA and protein were measured in human SGBS adipocytes. As with 3T3-L1 adipocytes, the SFAs, laurate and palmitate, increased SAA and MCP-1 mRNA levels, while stearate and oleate had no effect despite inducing adipocyte hypertrophy (supplemental Fig. 2). However, DHA also decreased glucose-induced expression of SAA and MCP-1 in these cell lines (supplemental Fig. 2). Consistent with mRNA expression, SAA1 protein levels in SGBS adipocytes increased after exposure to 25 mmol/l glucose, laurate, and palmitate and decreased after treatment with DHA (supplemental Fig. 2). As with 3T3-L1 cells, stearate and oleate did not change SAA1 protein in SGBS cells.
To confirm that the protein expression results were not due to glucose- or FFA-induced apoptosis (20), cell death was assessed using propidium iodide and annexin V staining. Exposure of cells to 25 mmol/l glucose, with or without palmitate or stearate, failed to induce apoptosis in differentiated 3T3-L1 adipocytes (supplemental Fig. 3).
Effect of glucose and FFAs on HA content and hyaluronan synthase expression.
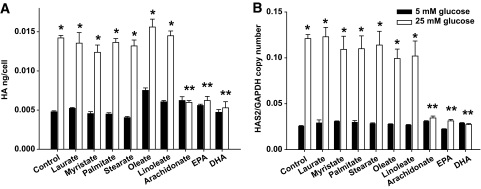
We have shown previously that HA production and expression of the enzyme responsible for its synthesis in adipose tissue, HAS2, are increased during glucose-induced adipocyte hypertrophy in vitro and by diet-induced obesity in mice (11). Therefore, we evaluated the effects of various FFAs on HAS2 expression and HA content in differentiated 3T3-L1, human SGBS adipocytes, and MEFs. Although HA content and HAS2 expression increased after exposure to high glucose, they were not altered by SFAs, the monounsaturated fatty acid, oleate, or the n-6 PUFA, linoleate. Interestingly, another n-6 PUFA, arachidonate, and the n-3 PUFAs, EPA and DHA, markedly attenuated glucose-stimulated HA content and HAS2 expression (Fig. 2A and B, supplemental Fig. 2), an effect similar to that observed previously with rosiglitazone (11). Thus, the effect of FFAs on HA differs from that of glucose excess.
FIG. 2.
HA content and HAS2 gene expression are increased by high glucose conditions but not SFAs and attenuated by arachidonate, EPA, and DHA. 3T3–L1 adipocytes differentiated in 5 or 25 mmol/l glucose were cultured for 7 days in the same media with or without various FFAs (250 μmol/l). A: Cell lysates that included cell-associated extracellular matrix were harvested and analyzed for HA content by ELISA. B: Total RNA was isolated and analyzed by multiplex real-time RT-PCR using HAS2 specific primers and probes and normalized to GAPDH. *P < 0.001 vs. 5 mmol/l glucose control. **P < 0.001 vs. 25 mmol/l glucose control.
Glucose excess and certain SFAs have proinflammatory effects, whereas arachidonate and the n-3 PUFAs, EPA and DHA, have anti-inflammatory properties. We therefore evaluated the effect of glucose excess and FFAs on adiponectin, an anti-inflammatory molecule expressed during adipocyte differentiation. Exposure of 3T3-L1–differentiated adipocytes to 25 mmol/l glucose, SFAs, oleate, and linoleate had no effect on adiponectin mRNA levels. However, adiponectin mRNA was further increased by exposure to arachidonate, EPA, and DHA (supplemental Fig. 4).
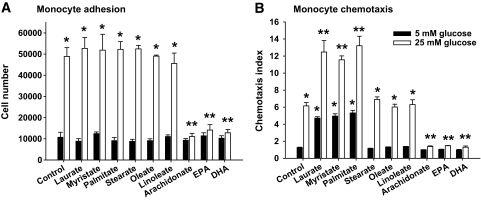
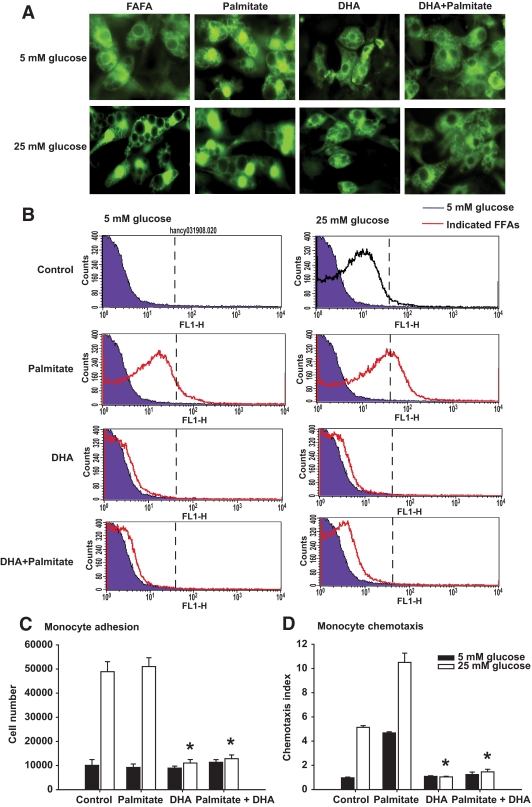
Monocyte adhesion and chemotaxis.
To investigate the potential of excess glucose and FFAs to recruit monocytes, monocyte adhesion and chemotaxis assays were performed with 3T3-L1 adipocytes grown in 5 or 25 mmol/l glucose with various FFAs. Adhesion of monocytes, an HA-dependent process (11), was increased only in adipocytes exposed to excess glucose. SFAs, oleate, and linoleate had no effect on monocyte adhesion, while glucose-stimulated HA-dependent cell adhesion was decreased in cells exposed to arachidonate, EPA, and DHA (Fig. 3A), consistent with the effect of these FFAs on HA content and HAS2 expression.
FIG. 3.
Monocyte adhesion and chemotaxis are increased by growth of adipocytes in the presence of excess glucose and certain SFAs. 3T3–L1 preadipocytes were differentiated into adipocytes and cultured for 7 days in 5 or 25 mmol/l glucose-containing media with various FFAs (250 μmol/l) with daily medium changes. U937 monocytes, prelabeled with calcein-AM, were then added and allowed to adhere for 90 min at 4°C. The cells were then washed three times and adherent cells measured in a multiwell fluorescent plate reader. A: Results are expressed as the number of adherent U937 cells per dish. In separate experiments, THP-1 monocytes, prelabeled with calcein-AM, were placed into the top chambers of a 96-well Boyden chemotaxis and conditioned media from adipocytes were placed in the bottom chambers. B: After incubation for 90 min, migrated monocytes were counted with a multiwell fluorescent plate reader. *P < 0.001 vs. 5 mmol/l glucose control. **P < 0.001 vs. 25 mmol/l glucose control.
We next compared the chemotactic potency of factors secreted by adipocytes cultured in 25 mmol/l glucose and various FFAs. Only conditioned medium from adipocytes cultured in excess glucose, laurate, myristate, and palmitate increased monocyte chemotaxis. The effects of glucose and these SFAs were additive (Fig. 3B). Conditioned media from adipocytes cultured in arachidonate, EPA, and DHA decreased monocyte chemotaxis induced by excess glucose. In contrast to the effect of FFAs on monocyte adhesion, the effect of FFAs on chemotaxis mirrored their effects on SAA3 and MCP-1 expression.
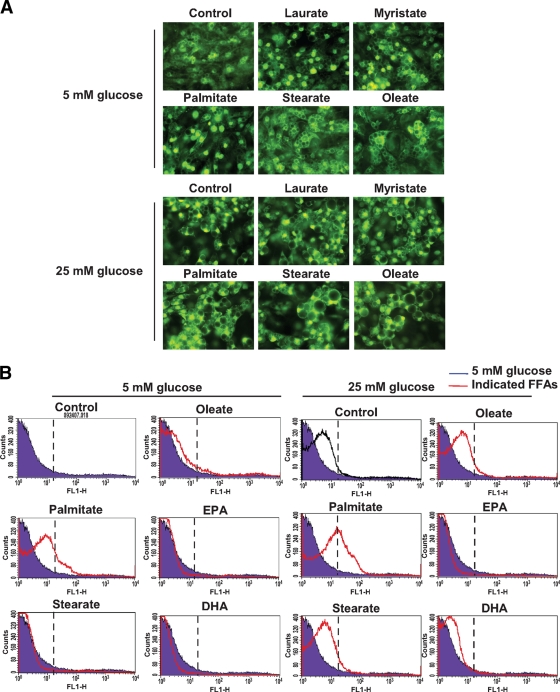
Effect of glucose and FFAs on NFκB transactivation and ROS generation.
Previously, we showed that NFκB transactivation increased while PPARγ transactivation decreased in differentiated 3T3-L1 cells exposed to high glucose (11). Since NFκB transactivation regulates transcription of a wide range of proinflammatory mediators (22–25), whereas PPARγ activation has anti-inflammatory properties (26,27), we examined the effects of various FFAs on NFκB transactivation. Laurate, myristate, and palmitate increased transactivation of NFκB in both 5 and 25 mmol/l glucose, suggesting that these SFAs are proinflammatory, whereas oleate and stearate had no effect (Fig. 4A).
FIG. 4.
FFAs have differential effects on NFκB translocation and ROS generation. 3T3–L1 adipocytes differentiated in 5 or 25 mmol/l glucose were cultured on glass for 7 days in the same medium with various FFAs (250 μmol/l) as indicated. A: Adipocytes were fixed and stained using an anti-p65 NFκB antibody, followed by the addition of a fluorescein isothiocyanate secondary antibody (original magnification ×400). B: Cells were subjected to FACS analysis using CM-H2DCFDA. Results are plotted as counts (number of cells) on the vertical axis versus CM-DCF fluorescence intensity on the horizontal axis. Cells exposed to 5 mmol/l glucose are shown in the blue color and are used as the negative control. The dashed lines, which indicate the peak of CM-DCF fluorescence of cells exposed to 250 μmol/l palmitate in the presence of 25 mmol/l glucose, are used as the high reference. These two conditions are used as low and high standards to compare ROS generation by the different FFAs, which are shown in red. Cells exposed to 25 mmol/l glucose alone are shown in black. (A high-quality digital representation of this figure is available in the online issue.)
To test potential intermediates by which excess glucose and certain SFAs might activate NFκB in 3T3-L1 adipocytes, ROS generation was measured using CM-H2DCFDA (Molecular Probes), a membrane-permeable dye that is oxidized by intracellular ROS to the fluorescent product CM-DCF (28). Daily exposure for 7 days of cells to 25 mmol/l glucose and/or palmitate (Fig. 4B), laurate, or myristate (not shown) increased intracellular CM-DCF fluorescence. When incubated with palmitate and 25 mmol/l glucose, ROS generation was additive (Fig. 4B). Stearate, oleate (Fig. 4B), and linoleate (not shown) had no effect on ROS in either 5 or 25 mmol/l glucose. Conversely, arachidonate (not shown), EPA, and DHA blunted the effect of 25 mmol/l glucose (Fig. 4B). These results raise the question of whether ROS generated by high glucose and/or palmitate may be involved in NFκB activation in 3T3-L1 adipocytes.
Effect of antioxidants on NFκB translocation, ROS generation, and monocyte adhesion and chemotactic factors.
To further evaluate this possibility, several antioxidants were added to adipocytes together with 25 mmol/l glucose and/or 250 μmol/l palmitate. Although CM-DCF fluorescence was observed with several FFAs, for these and many subsequent experiments we have used palmitate, since this fatty acid is common in the diet and constitutes a large proportion of circulating FFAs. N-acetyl cysteine (NAC), catalase, and superoxide dismutase (SOD) all inhibited CM-DCF fluorescence induced by excess glucose and palmitate (data not shown) and NFκB translocation (supplemental Fig. 5A). All these antioxidants also suppressed SAA3 and MCP-1 gene expression, SAA3 protein secretion, and monocyte chemotaxis induced by 25 mmol/l glucose and palmitate (supplemental Fig. 5). They also inhibited glucose-induced HA content. Thus, ROS might be important intermediates that affect the production of SAA3, MCP-1, and HA in 3T3-L1 adipocytes.
TLR4 inhibition of palmitate-induced gene expression.
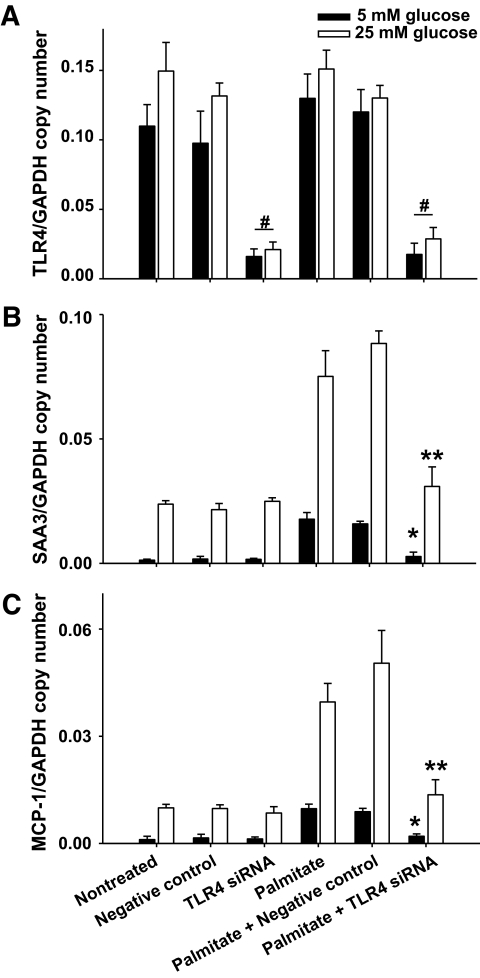
Since SFAs such as laurate and palmitate can activate TLR4-mediated pathways, we evaluated the role of TLR4 on the expression of SAA3 and MCP-1 induced by SFAs. Transfection of differentiated 3T3-L1 cells with a TLR4-specific siRNA markedly silenced TLR4 expression compared with transfection of scrambled constructs and to untreated cells (Fig. 5A). SAA3 and MCP-1 expression levels were markedly decreased in response to palmitate exposure in both 5 and 25 mmol/l glucose in TLR4 siRNA-transfected cells, whereas TLR-4 silencing had no effect on glucose-mediated stimulation of gene expression (Fig. 5B and C). These results imply that palmitate increases SAA3 and MCP-1 expression via a TLR4-dependent mechanism.
FIG. 5.
Inhibition of palmitate-induced expression of SAA3 and MCP-1 by silencing TLR4. 3T3–L1 adipocytes were transfected with a siRNA specific for TLR4 or a scrambled siRNA (negative control). Twenty-four hours later, the cells were exposed to palmitate (250 μmol/l) in 5 and 25 mmol/l glucose for 7 days with daily medium changes. Total RNA was isolated and analyzed by multiplex real-time RT-PCR using primers specific for TLR4 (A), SAA3 (B), or MCP-1 (C) and normalized to GAPDH. *P < 0.001 vs. negative control plus palmitate in 5 mmol/l glucose. **P < 0.001 vs. negative control plus palmitate in 25 mmol/l glucose. #P < 0.001 vs. negative control.
DHA inhibition of palmitate-induced expression of SAA3 and MCP-1.
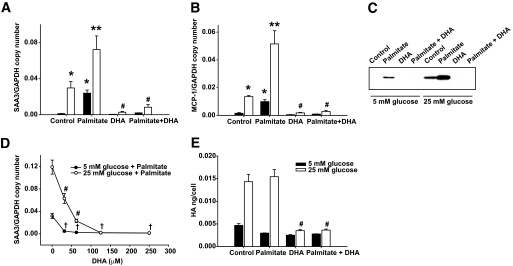
Since n-3 fatty acids have anti-inflammatory properties (29,30), we examined the effect of DHA on SAA3 and MCP-1 expression induced by excess glucose and palmitate. Exposure to DHA for 7 days reduced the increase in lipid droplet size induced by high glucose and/or palmitate (data not shown), inhibited SAA3 and MCP-1 gene expression induced by high glucose and/or palmitate (Fig. 6A and B), and reduced secreted SAA protein (Fig. 6C). DHA inhibited palmitate-induced expression of SAA3 in either 5 or 25 mmol/l glucose in a dose-dependent manner and at relatively low concentration (Fig. 6D). DHA also suppressed HA content induced by exposure of cells to both high glucose and palmitate (Fig. 6E). These effects of DHA were not an artifact due to apoptosis (supplemental Fig. 3).
FIG. 6.
DHA suppresses SAA3, MCP-1 gene expression, and HA content. 3T3–L1 adipocytes differentiated in 5 and 25 mmol/l glucose were cultured for 7 days with and without palmitate (250 μmol/l) and/or DHA (250 μmol/l). Total RNA was collected for analysis of SAA3 and MCP-1 mRNA expression by real-time RT-PCR using SAA3- and MCP-1–specific primers and probes and normalized to GAPDH (A and B), and conditioned media were analyzed by immunoblot using a SAA3 antibody (C). E: Cell lysates were also harvested for analysis of HA content by ELISA. D: To determine the concentration dependence of DHA, differentiated 3T3–L1 adipocytes were cultured in 5 and 25 mmol/l glucose with and without palmitate (250 μmol/l) plus the concentrations of DHA indicated. *P < 0.001 vs. 5 mmol/l glucose control. **P < 0.001 vs. 25 mmol/l glucose control. #P < 0.001 vs. 25 mmol/l glucose with palmitate. †P < 0.01 vs. 5 mmol/l glucose with palmitate.
We also examined whether DHA could inhibit the translocation of NFκB and ROS generation induced by high glucose and/or palmitate. DHA inhibited NFκB translocation, CM-DCF fluorescence (Fig. 7A and B), and monocyte chemotaxis (Fig. 7D) stimulated by both high glucose and/or palmitate, consistent with its effect on chemotactic factor expression (Fig. 6A and B). Moreover, DHA inhibited monocyte adhesion stimulated by high glucose, consistent with its effect on HA synthesis (Fig. 7C).
FIG. 7.
DHA suppresses the translocation of NFκB and ROS generation stimulated by excess glucose and palmitate. 3T3–L1 adipocytes were cultured in 5 or 25 mmol/l glucose with or without palmitate or DHA (250 μmol/l) for 7 days as indicated. Nuclear translocation of NFκB was analyzed using an anti-p65 NFκB antibody followed by a fluorescein isothiocyanate–labeled secondary antibody (A, original magnification ×600). B: Cells were also subjected to FACS analysis using CM-H2DCFDA. Results are plotted as counts (number of cells) on the vertical axis versus CM-DCF fluorescence intensity on the horizontal axis. Cells exposed to 5 mmol/l glucose are shown in blue and cells exposed to 250 μmol/l palmitate in the presence of 25 mmol/l glucose as dashed lines. These two conditions are used as low and high standards, respectively, to compare ROS generation by the different FFAs, which are shown in red. Cells exposed to 25 mmol/l glucose alone are shown in black. Cells and conditioned media were subjected to the monocyte adhesion (C) or chemotaxis (D) assays described in the legend to Fig. 3. *P < 0.001 vs. 25 mmol/l glucose with palmitate. (A high-quality digital representation of this figure is available in the online issue.)
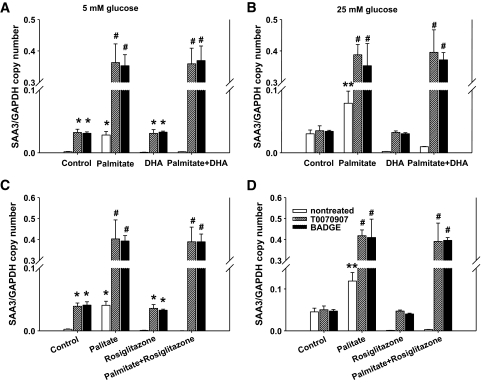
PPARγ dependence of the effect of DHA on adipocyte-derived chemotactic factor expression.
We showed previously that glucose-induced expression of SAA3 and MCP-1 was inhibited by rosiglitazone (11), a PPARγ ligand with anti-inflammatory properties. To evaluate whether anti-inflammatory properties of DHA are dependent on PPARγ, the PPARγ antagonists T0070907 and bisphenol A diglycidyl ether (BADGE) were added to adipocytes with daily replenishment of media containing glucose, palmitate, and/or DHA. Strikingly, both BADGE and T0070907 increased basal levels of expression of SAA3 and MCP-1 in 5 mmol/l glucose and amplified the effect of palmitate in both 5 and 25 mmol/l glucose. They also obliterated the repressive effect of DHA on high glucose–and palmitate-induced gene expression (Fig. 8A and B). In a control experiment, these PPARγ antagonists also abolished the effect of rosiglitazone on SAA3 expression (Fig. 8C and D). These results strongly suggest that DHA is working via a PPARγ-dependent mechanism.
FIG. 8.
The PPARγ antagonists, T0070907 and BADGE, abolish the anti-inflammatory effect of DHA. 3T3–L1 adipocytes differentiated in 5 mmol/l (A and C) or 25 mmol/l (B and D) glucose were cultured in the same media with or without 250 μmol/l of palmitate and/or DHA (250 μmol/l) for 7 days. Some adipocytes were also replenished with the PPARγ antagonists, T0070907 (1 μmol/l) or BADGE (100 μmol/l). As controls for DHA, rosiglitazone (100 nmol/l) was used instead of DHA (C and D). Total RNA was isolated and analyzed by multiplex real-time RT-PCR using SAA3-specific (A, C, and D) or MCP-1–specific (B) primers and probes and normalized to GAPDH. *P < 0.001 vs. 5 mmol/l glucose control. **P < 0.001 vs. 25 mmol/l glucose control. #P < 0.001 vs. 25 mmol/l glucose with palmitate.
DISCUSSION
Our findings indicate that specific SFAs increase the expression of the monocyte chemotactic factors, SAA and MCP-1, by differentiated 3T3-L1 and SGBS adipocytes and by adipocytes derived from MEFs. They extend our previous observations on the effects of glucose excess on these chemotactic factors and HA (11) by showing that SFAs enhance the effect of glucose on SAA and MCP-1 expression. Moreover, SFAs stimulate SAA and MCP-1 expression via a pathway that is both ROS and NFκB dependent, similar to findings observed previously with glucose excess (11) but which is suppressible by exposure to specific PUFAs. Our findings also implicate TLR4 in SFA-stimulated, but not glucose-stimulated, expression of these chemotactic factors. Finally, while SFAs have no effect on HA, specific PUFAs appear to block the increased HA production associated with glucose excess.
Inflammatory gene activation by SFAs in adipocytes has been described previously (12). Our studies extend these observations to genes that are believed to play important roles in monocyte adhesion (HAS2) and chemotaxis (SAA and MCP-1), processes key to recruitment of macrophages into adipose tissue. Moreover, they show that effects observed on gene expression and protein secretion are mirrored by changes in cell adhesion and chemotaxis.
Comparisons of several fatty acids yielded some surprising findings. For example, while the SFAs, laurate, myristate, and palmitate, all increased the expression of these chemotactic factors, stearate had no effect despite being only two carbon atoms longer than palmitate. The reason for this discrepancy is unclear but could represent failure of stearate to activate TLR4 or other components of the signal transduction pathway used by the other SFAs studied. The possibility that stearate was cytotoxic was excluded by experiments showing no stearate-mediated apoptosis. Our findings also differ from a previous report that myristate, palmitate, and stearate, but not laurate, increased cytokine expression by macrophages (12). These differences may represent cell-specific differences in response to SFAs between adipocytes and macrophages.
Of the unsaturated fatty acids, oleate and linoleate had no effect on SAA and MCP-1 expression. However, both EPA and DHA strongly suppressed gene expression in both high-glucose conditions and/or after exposure to palmitate. Similar findings were observed with arachidonate, which is not an n-3 fatty acid. Although relatively high doses of n-3 fatty acids were used for these experiments, a dose-response experiment with DHA revealed similar suppression of glucose and palmitate-mediated stimulation at lower concentrations. These findings suggest that n-3 fatty acids have anti-inflammatory effects on activation of these genes in adipocytes. Anti-inflammatory properties of n-3 fatty acids have been reported (31,32), including in adipose tissue (33) and in mice, where feeding fish oil resulted in adipocyte hypertrophy without inflammatory gene expression or insulin resistance (33). Moreover, EPA, DHA, and arachidonate further increased levels of adiponectin, an anti-inflammatory adipocytokine.
We found evidence that lipid accumulation and chemotactic factor gene expression could be dissociated in adipocytes. For example, while all SFAs studied induced adipocyte triglyceride accumulation, stearate and oleate had no effect on chemotactic factor gene expression. Moreover, all PUFAs studied reduced adipocyte triglyceride content, but only linoleate failed to inhibit glucose or palmitate-mediated gene expression. Although increased adipocyte size is associated with adipose tissue macrophage accumulation (1–3) and increased insulin resistance (34) in vivo, dissociation between adipocyte hypertrophy and adipose tissue inflammation also has been reported in several animal models. For example, mice fed a fish oil–enriched diet became obese with hypertrophic adipocytes but did not develop adipose tissue macrophage accumulation or insulin resistance (33). Overexpression of acyl CoA:diacylglycerol acyltransferase 1 (35) or phosphoenolpyruvate carboxykinase (36) resulted in hypertrophic obesity without insulin resistance, suggesting that adipose tissue in these mouse models was not macrophage enriched. Very obese ob/ob mice with modest adiponectin overexpression were insulin sensitive without macrophage accumulation in adipose tissue (37). Thus, the ability to expand adipose tissue mass appropriately in response to nutrient excess may preclude the development of adipose tissue inflammation and insulin resistance (37). Therefore, the mechanism by which adipocytes become hypertrophic may be more important in determining whether macrophages will accumulate in adipose tissue and lead to insulin resistance and systemic inflammation rather than the presence of adipocyte hypertrophy, per se. Our findings suggest that dietary FFA composition (i.e., SFA enriched versus PUFA enriched) may underlie at least some of the dissociation between obesity and adipose tissue inflammation. While we confirmed our previous observation that glucose excess increased HA accumulation (11), none of the SFAs tested, nor oleate or linoleate, affected HA content in either 5 or 25 mmol/l glucose. However, EPA, DHA, and arachidonate suppressed glucose-stimulated HA accumulation and SAA3 and MCP-1 expression in these adipocytes. Monocyte adhesion and chemotaxis are critical to tissue macrophage accumulation (38), and HA plays an important role in monocyte adhesion by binding to CD44 and other receptors on monocytes (39). Absence of CD44 markedly decreased macrophage accumulation in the artery wall (40). In experiments assessing monocyte adhesion and chemotaxis, changes in both processes closely mirrored the effects seen with HA content and the expression of SAA3 and MCP-1, respectively. Conditions that altered HA content led to parallel changes in monocyte adhesion, and conditions that altered the expression of SAA3 and MCP-1 were mirrored by changes in chemotaxis.
EPA, DHA, and arachidonate inhibited both HA content and chemotactic factor expression, similar to the effects of the PPARγ agonist rosiglitazone, suggesting that these PUFAs might be working via a PPARγ-dependent mechanism. Moreover, these PUFAs increased the expression of adiponectin, which is regulated by PPARγ (41). The experiment using the PPARγ antagonists further supports a role for PPARγ.
The observation that baseline expression of these chemotactic factors is increased by PPARγ antagonism is mirrored by findings in other tissues. For example, the absence of PPARα is associated with an increased baseline expression of adhesion molecules in endothelial cells (42) and expression of the inflammatory molecules SAA1 and SAA2 in liver (16). Thus, PPAR isoforms may exert a “braking” effect on the expression of several inflammatory genes, suppression of which is removed by deficiency or antagonism of the nuclear receptor. In the current study, the PPARγ antagonists also overrode the effects of DHA in suppressing the expression of SAA3 and MCP-1, suggesting that DHA is working via a PPARγ mechanism.
A common pathway for inflammatory gene activation is via NFκB. In the present study, NFκB nuclear translocation mirrored the effect seen with chemotactic factor expression, suggesting that they are linked. SFAs that activated SAA3 and MCP-1 expression were associated with NFκB translocation, FFAs that had no effect on chemotactic factor expression had no effect on NFκB translocation, and FFAs that inhibited gene expression also inhibited nuclear translocation stimulated by either high-glucose conditions or palmitate. Several other studies (13,25,43,44) indicate that SFAs activate NFκB, whereas PUFAs do not. Future studies will need to use chemical and molecular inhibitors to directly link NFκB activation with chemotactic factor gene expression.
Another common feature associated with SAA3 and MCP-1 gene activation was ROS generation, as assessed by CM-DCF fluorescence. ROS can play important roles in signal transduction, including activation of NFκB (45). Although ROS have been implicated in activating several NFκB-mediated inflammatory signals (46), their direct role has been challenged as being potentially facilitatory rather than causal (47). Our data show that high glucose and palmitate, conditions that lead to increased expression of SAA3 and MCP-1, also increased ROS generation in adipocytes. These findings suggest that ROS-mediated activation of NFκB in response to certain nutrients is linked to generation of these chemotactic factors.
The finding that palmitate-mediated activation of chemotactic factor gene expression is markedly inhibited by silencing TLR4 is consistent with previous observations that suggest that the TLR4 pathway can be activated by certain SFAs (12,13,48). While the specific SFAs that activate TLR4 may differ between macrophages and adipocytes (12,13,48), others have also observed activation of TLR4 by palmitate and myristate in adipocytes (12). The effect of stearate on TLR4 activation is not known. However, our data suggest that it may not activate TLR4 in adipocytes. Since there is no evidence that glucose exerts effects via the TLR4 signaling pathway, the absence of inhibition of glucose-mediated activation of SAA3 and MCP-1 gene expression by TLR4 silencing is not surprising.
Our findings have important implications for understanding the obese state in vivo in that the specific nature of the nutrient leading to obesity could potentially result in different degrees of activation, or even suppression, of chemotactic factors in adipocytes. This in turn could affect macrophage accumulation in adipose tissue, an important determinant of insulin resistance. Thus, nutritional excess from SFAs and glucose, rather than high glucose levels, per se, are likely to be proinflammatory and might have more adverse metabolic consequences than obesity resulting from excess consumption of stearate, oleate, or PUFAs. Conversely, fish oil consumption might actually have anti-inflammatory effects in adipose tissue despite weight gain and obesity. Indeed, findings consistent with our in vitro observations have been made in several mouse models. Thus, consumption by LDL receptor–deficient mice of a diet rich in SFAs and sucrose led to SAA3 and MCP-1 overexpression and accumulation of macrophages in adipose tissue, together with increased insulin resistance (49). Deficiency of TLR4 was associated with reduced insulin resistance in response to diet-induced obesity (12), and mice fed a diet rich in fish oils had large fat cells yet little macrophage accumulation and insulin resistance (33). Whether differences in dietary composition have similar effects in human obesity remains to be determined.
Supplementary Material
ACKNOWLEDGMENTS
Supported in part by National Institutes of Health Grants HL94352, HL92969, and HL18645 and by the German Research Foundation DFG (WA 1096/3-3).
No potential conflicts of interest relevant to this article were reported.
Parts of this study were presented at the Annual Scientific Meeting of the Obesity Society, Phoenix, Arizona, 3–7 October 2008.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
REFERENCES
- 1.Wellen KE, Hotamisligil GS: Obesity-induced inflammatory changes in adipose tissue. J Clin Invest 2003;112:1785–1788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Xu H, Barnes GT, Yang Q, Tan G, Yang D, Chou CJ, Sole J, Nichols A, Ross JS, Tartaglia LA, Chen H: Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. J Clin Invest 2003;112:1821–1830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weisberg SP, McCann D, Desai M, Rosenbaum M, Leibel RL, Ferrante AW, Jr: Obesity is associated with macrophage accumulation in adipose tissue. J Clin Invest 2003;112:1796–1808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bullo M, Garcia-Lorda P, Megias I, Salas-Salvado J: Systemic inflammation, adipose tissue tumor necrosis factor, and leptin expression. Obes Res 2003;11:525–531 [DOI] [PubMed] [Google Scholar]
- 5.Maachi M, Pieroni L, Bruckert E, Jardel C, Fellahi S, Hainque B, Capeau J, Bastard JP: Systemic low-grade inflammation is related to both circulating and adipose tissue TNFalpha, leptin and IL-6 levels in obese women. Int J Obes Relat Metab Disord 2004;28:993–997 [DOI] [PubMed] [Google Scholar]
- 6.Cancello R, Clement K: Is obesity an inflammatory illness? Role of low-grade inflammation and macrophage infiltration in human white adipose tissue. Bjog 2006;113:1141–1147 [DOI] [PubMed] [Google Scholar]
- 7.Weisberg SP, Hunter D, Huber R, Lemieux J, Slaymaker S, Vaddi K, Charo I, Leibel RL, Ferrante AW, Jr: CCR2 modulates inflammatory and metabolic effects of high-fat feeding. J Clin Invest 2006;116:115–124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kirk EA, Sagawa ZK, McDonald TO, O'Brien KD, Heinecke JW: Monocyte chemoattractant protein deficiency fails to restrain macrophage infiltration into adipose tissue [corrected]. Diabetes 2008;57:1254–1261 [DOI] [PubMed] [Google Scholar]
- 9.Inouye KE, Shi H, Howard JK, Daly CH, Lord GM, Rollins BJ, Flier JS: Absence of CC chemokine ligand 2 does not limit obesity-associated infiltration of macrophages into adipose tissue. Diabetes 2007;9:2242–2250 [DOI] [PubMed] [Google Scholar]
- 10.Chen A, Mumick S, Zhang C, Lamb J, Dai H, Weingarth D, Mudgett J, Chen H, MacNeil DJ, Reitman ML, Qian S: Diet induction of monocyte chemoattractant protein-1 and its impact on obesity. Obes Res 2005;13:1311–1320 [DOI] [PubMed] [Google Scholar]
- 11.Han CY, Subramanian S, Chan CK, Omer M, Chiba T, Wight TN, Chait A: Adipocyte-derived serum amyloid A3 and hyaluronan play a role in monocyte recruitment and adhesion. Diabetes 2007;56:2260–2273 [DOI] [PubMed] [Google Scholar]
- 12.Shi H, Kokoeva MV, Inouye K, Tzameli I, Yin H, Flier JS: TLR4 links innate immunity and fatty acid-induced insulin resistance. J Clin Invest 2006;116:3015–3025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Suganami T, Tanimoto-Koyama K, Nishida J, Itoh M, Yuan X, Mizuarai S, Kotani H, Yamaoka S, Miyake K, Aoe S, Kamei Y, Ogawa Y: Role of the Toll-like receptor 4/NF-kappaB pathway in saturated fatty acid-induced inflammatory changes in the interaction between adipocytes and macrophages. Arterioscler Thromb Vasc Biol 2007;27:84–91 [DOI] [PubMed] [Google Scholar]
- 14.Lin Y, Berg AH, Iyengar P, Lam TK, Giacca A, Combs TP, Rajala MW, Du X, Rollman B, Li W, Hawkins M, Barzilai N, Rhodes CJ, Fantus IG, Brownlee M, Scherer PE: The hyperglycemia-induced inflammatory response in adipocytes: the role of reactive oxygen species. J Biol Chem 2005;280:4617–4626 [DOI] [PubMed] [Google Scholar]
- 15.Wabitsch M, Brenner RE, Melzner I, Braun M, Moller P, Heinze E, Debatin KM, Hauner H: Characterization of a human preadipocyte cell strain with high capacity for adipose differentiation. Int J Obes Relat Metab Disord 2001;25:8–15 [DOI] [PubMed] [Google Scholar]
- 16.Han CY, Chiba T, Campbell JS, Fausto N, Chaisson M, Orasanu G, Plutzky J, Chait A: Reciprocal and coordinate regulation of serum amyloid A versus apolipoprotein A-I and paraoxonase-1 by inflammation in murine hepatocytes. Arterioscler Thromb Vasc Biol 2006;26:1806–1813 [DOI] [PubMed] [Google Scholar]
- 17.Chang MY, Han CY, Wight TN, Chait A: Antioxidants inhibit the ability of lysophosphatidylcholine to regulate proteoglycan synthesis. Arterioscler Thromb Vasc Biol 2006;26:494–500 [DOI] [PubMed] [Google Scholar]
- 18.Wilkinson TS, Bressler SL, Evanko SP, Braun KR, Wight TN: Overexpression of hyaluronan synthases alters vascular smooth muscle cell phenotype and promotes monocyte adhesion. J Cell Physiol 2006;206:378–385 [DOI] [PubMed] [Google Scholar]
- 19.Frevert CW, Wong VA, Goodman RB, Goodwin R, Martin TR: Rapid fluorescence-based measurement of neutrophil migration in vitro. J Immunol Methods 1998;213:41–52 [DOI] [PubMed] [Google Scholar]
- 20.Guo W, Wong S, Xie W, Lei T, Luo Z: Palmitate modulates intracellular signaling, induces endoplasmic reticulum stress, and causes apoptosis in mouse 3T3–L1 and rat primary preadipocytes. Am J Physiol Endocrinol Metab 2007;293:E576–E586 [DOI] [PubMed] [Google Scholar]
- 21.Uhlar CM, Whitehead AS: Serum amyloid A, the major vertebrate acute-phase reactant. Eur J Biochem 1999;265:501–523 [DOI] [PubMed] [Google Scholar]
- 22.Ruan H, Hacohen N, Golub TR, Van Parijs L, Lodish HF: Tumor necrosis factor-alpha suppresses adipocyte-specific genes and activates expression of preadipocyte genes in 3T3–L1 adipocytes: nuclear factor-κB activation by TNF-α is obligatory. Diabetes 2002;51:1319–1336 [DOI] [PubMed] [Google Scholar]
- 23.Bokarewa M, Nagaev I, Dahlberg L, Smith U, Tarkowski A: Resistin, an adipokine with potent proinflammatory properties. J Immunol 2005;174:5789–5795 [DOI] [PubMed] [Google Scholar]
- 24.Fain JN, Madan AK: Regulation of monocyte chemoattractant protein 1 (MCP-1) release by explants of human visceral adipose tissue. Int J Obes (Lond) 2005;29:1299–1307 [DOI] [PubMed] [Google Scholar]
- 25.Ajuwon KM, Spurlock ME: Palmitate activates the NF-kappaB transcription factor and induces IL-6 and TNFalpha expression in 3T3–L1 adipocytes. J Nutr 2005;135:1841–1846 [DOI] [PubMed] [Google Scholar]
- 26.Ruan H, Pownall HJ, Lodish HF: Troglitazone antagonizes tumor necrosis factor-alpha-induced reprogramming of adipocyte gene expression by inhibiting the transcriptional regulatory functions of NF-kappaB. J Biol Chem 2003;278:28181–28192 [DOI] [PubMed] [Google Scholar]
- 27.Yu JG, Javorschi S, Hevener AL, Kruszynska YT, Norman RA, Sinha M, Olefsky JM: The effect of thiazolidinediones on plasma adiponectin levels in normal, obese, and type 2 diabetic subjects. Diabetes 2002;51:2968–2974 [DOI] [PubMed] [Google Scholar]
- 28.Cominacini L, Pasini AF, Garbin U, Davoli A, Tosetti ML, Campagnola M, Rigoni A, Pastorino AM, Lo Cascio V, Sawamura T: Oxidized low density lipoprotein (ox-LDL) binding to ox-LDL receptor-1 in endothelial cells induces the activation of NF-kappaB through an increased production of intracellular reactive oxygen species. J Biol Chem 2000;275:12633–12638 [DOI] [PubMed] [Google Scholar]
- 29.Krey G, Braissant O, L'Horset F, Kalkhoven E, Perroud M, Parker MG, Wahli W: Fatty acids, eicosanoids, and hypolipidemic agents identified as ligands of peroxisome proliferator-activated receptors by coactivator-dependent receptor ligand assay. Mol Endocrinol 1997;11:779–791 [DOI] [PubMed] [Google Scholar]
- 30.Neschen S, Morino K, Rossbacher JC, Pongratz RL, Cline GW, Sono S, Gillum M, Shulman GI: Fish oil regulates adiponectin secretion by a peroxisome proliferator-activated receptor-γ–dependent mechanism in mice. Diabetes 2006;55:924–928 [DOI] [PubMed] [Google Scholar]
- 31.Kris-Etherton PM, Harris WS, Appel LJ: Fish consumption, fish oil, omega-3 fatty acids, and cardiovascular disease. Circulation 2002;106:2747–2757 [DOI] [PubMed] [Google Scholar]
- 32.Singer P, Shapiro H, Theilla M, Anbar R, Singer J, Cohen J: Anti-inflammatory properties of omega-3 fatty acids in critical illness: novel mechanisms and an integrative perspective. Intensive Care Med 2008;34:1580–1592 [DOI] [PubMed] [Google Scholar]
- 33.Saraswathi V, Gao L, Morrow JD, Chait A, Niswender KD, Hasty AH: Fish oil increases cholesterol storage in white adipose tissue with concomitant decreases in inflammation, hepatic steatosis, and atherosclerosis in mice. J Nutr 2007;137:1776–1782 [DOI] [PubMed] [Google Scholar]
- 34.Li J, Yu X, Pan W, Unger RH: Gene expression profile of rat adipose tissue at the onset of high-fat-diet obesity. Am J Physiol Endocrinol Metab 2002;282:E1334–E1341 [DOI] [PubMed] [Google Scholar]
- 35.Chen HC, Stone SJ, Zhou P, Buhman KK, Farese RV, Jr: Dissociation of obesity and impaired glucose disposal in mice overexpressing acyl coenzyme a: diacylglycerol acyltransferase 1 in white adipose tissue. Diabetes 2002;51:3189–3195 [DOI] [PubMed] [Google Scholar]
- 36.Franckhauser S, Munoz S, Pujol A, Casellas A, Riu E, Otaegui P, Su B, Bosch F: Increased fatty acid re-esterification by PEPCK overexpression in adipose tissue leads to obesity without insulin resistance. Diabetes 2002;51:624–630 [DOI] [PubMed] [Google Scholar]
- 37.Kim JY, van de Wall E, Laplante M, Azzara A, Trujillo ME, Hofmann SM, Schraw T, Durand JL, Li H, Li G, Jelicks LA, Mehler MF, Hui DY, Deshaies Y, Shulman GI, Schwartz GJ, Scherer PE: Obesity-associated improvements in metabolic profile through expansion of adipose tissue. J Clin Invest 2007;117:2621–2637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wilkinson PC: Relation between locomotion, chemotaxis and clustering of immune cells. Immunology 1990;69:127–133 [PMC free article] [PubMed] [Google Scholar]
- 39.de La Motte CA, Hascall VC, Calabro A, Yen-Lieberman B, Strong SA: Mononuclear leukocytes preferentially bind via CD44 to hyaluronan on human intestinal mucosal smooth muscle cells after virus infection or treatment with poly(I.C). J Biol Chem 1999;274:30747–30755 [DOI] [PubMed] [Google Scholar]
- 40.Cuff CA, Kothapalli D, Azonobi I, Chun S, Zhang Y, Belkin R, Yeh C, Secreto A, Assoian RK, Rader DJ, Pure E: The adhesion receptor CD44 promotes atherosclerosis by mediating inflammatory cell recruitment and vascular cell activation. J Clin Invest 2001;108:1031–1040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bouskila M, Pajvani UB, Scherer PE: Adiponectin: a relevant player in PPARgamma-agonist-mediated improvements in hepatic insulin sensitivity?. Int J Obes (Lond) 29 Suppl2005;1:S17– 23 [DOI] [PubMed] [Google Scholar]
- 42.Ziouzenkova O, Perrey S, Asatryan L, Hwang J, MacNaul KL, Moller DE, Rader DJ, Sevanian A, Zechner R, Hoefler G, Plutzky J: Lipolysis of triglyceride-rich lipoproteins generates PPAR ligands: evidence for an antiinflammatory role for lipoprotein lipase. Proc Natl Acad Sci U S A 2003;100:2730–2735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Laine PS, Schwartz EA, Wang Y, Zhang WY, Karnik SK, Musi N, Reaven PD: Palmitic acid induces IP-10 expression in human macrophages via NF-kappaB activation. Biochem Biophys Res Commun 2007;358:150–155 [DOI] [PubMed] [Google Scholar]
- 44.Suganami T, Nishida J, Ogawa Y: A paracrine loop between adipocytes and macrophages aggravates inflammatory changes: role of free fatty acids and tumor necrosis factor alpha. Arterioscler Thromb Vasc Biol 2005;25:2062–2068 [DOI] [PubMed] [Google Scholar]
- 45.Foncea R, Carvajal C, Almarza C, Leighton F: Endothelial cell oxidative stress and signal transduction. Biol Res 2000;33:89–96 [DOI] [PubMed] [Google Scholar]
- 46.Schmidt KN, Amstad P, Cerutti P, Baeuerle PA: The roles of hydrogen peroxide and superoxide as messengers in the activation of transcription factor NF-kappa B. Chem Biol 1995;2:13–22 [DOI] [PubMed] [Google Scholar]
- 47.Bowie A, O'Neill LA: Oxidative stress and nuclear factor-kappaB activation: a reassessment of the evidence in the light of recent discoveries. Biochem Pharmacol 2000;59:13–23 [DOI] [PubMed] [Google Scholar]
- 48.Lee JY, Hwang DH: The modulation of inflammatory gene expression by lipids: mediation through Toll-like receptors. Mol Cells 2006;21:174–185 [PubMed] [Google Scholar]
- 49.Subramanian S, Han CY, Chiba T, McMillen TS, Wang SA, Haw A, 3rd, Kirk EA, O'Brien KD, Chait A: Dietary cholesterol worsens adipose tissue macrophage accumulation and atherosclerosis in obese LDL receptor-deficient mice. Arterioscler Thromb Vasc Biol 2008;28:685–691 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.