Abstract
Background
99mTc-mebrofenin hepatobiliary scintigraphy (HBS) was used as a quantitative method to evaluate liver function. The aim of this study was to compare future remnant liver function assessed by 99mTc-mebrofenin hepatobiliary scintigraphy with future remnant liver volume in the prediction of liver failure after major liver resection.
Methods
Computed tomography (CT) volumetry and 99mTc-mebrofenin hepatobiliary scintigraphy were performed prior to major resection in 55 high-risk patients, including 30 patients with parenchymal liver disease. Liver volume was expressed as percentage of total liver volume or as standardized future remnant liver volume. Receiver operating characteristic (ROC) curve analysis was performed to identify a cutoff value for future remnant liver function in predicting postoperative liver failure.
Results
Postoperative liver failure occurred in nine patients. A liver function cutoff value of 2.69%/min/m2 was calculated by ROC curve analysis. 99mTc-mebrofenin hepatobiliary scintigraphy demonstrated better sensitivity, specificity, and positive and negative predictive value compared to future remnant liver volume. Using 99mTc-mebrofenin hepatobiliary scintigraphy, one cutoff value suffices in both compromised and noncompromised patients.
Conclusion
Preoperative 99mTc-mebrofenin hepatobiliary scintigraphy is a valuable technique to estimate the risk of postoperative liver failure. Especially in patients with uncertain quality of the liver parenchyma, 99mTc-mebrofenin HBS proved of more value than CT volumetry.
Keywords: Hepatectomy, Liver failure, Liver function, Liver volume, Mebrofenin, CT volumetry
Introduction
Major liver resection may result in a small postoperative remnant liver, thereby increasing the risk of postoperative liver failure, especially in patients with parenchymal disease.1 Posthepatectomy liver failure is the most frequent cause of mortality after liver resection. Although the causes of liver failure are multifactorial, insufficient postoperative remnant liver function is one of the main contributing factors.
Preoperative computed tomography (CT) volumetry, in which liver volume is used as an indirect measurement of liver function, is widely used to identify patients who should be excluded from a planned liver resection or to select patients who will benefit from preoperative portal vein embolization (PVE).1–5 Future remnant liver (FRL) volume (FRL-V) is expressed as a percentage of total liver volume (%FRL-V),3 or as standardized FRL (sFRL), in which FRL-V is calculated as percentage of total liver volume based on body surface area (BSA).4,6 sFRL recognizes patient characteristics (body weight/BSA) but has only been validated in patients with healthy livers. In patients with a normal liver parenchyma, an %FRL-V or sFRL larger than 25–30% of total preoperative liver volume is considered sufficient for a safe resection,3,4,7–9 whereas in patients with a compromised liver (e.g., fibrosis, steatosis, or cholestasis), a %FRL-V or sFRL of more than 40% is preferred.10 The separate cutoff values indicate the necessity to asses the quality of the liver parenchyma in order to perform an accurate and safe preoperative risk analysis using CT volumetry. Preoperative liver biopsy is currently the most reliable method to assess the quality of the liver parenchyma. Biopsies are not routinely performed due the potential unequal distribution of parenchymal damage11 and the risk of complications.12,13 As a result, the quality of the liver parenchyma frequently remains unknown, rendering preoperative risk analysis by CT volumetry less reliable.
For accurate preoperative risk analysis, additional tests of liver function are required. Dynamic 99mTc-mebrofenin hepatobiliary scintigraphy (HBS) was developed as a quantitative method for evaluating total and regional liver function, including FRL function.14,15 The hepatic uptake of 99mTc-mebrofenin is similar to the uptake of organic anions such as bilirubin.16 After the hepatic uptake, 99mTc-mefrofenin is excreted into the bile canaliculi without undergoing biotransformation during its transport through the hepatocytes. Although 99mTc-mebrofenin is not metabolized, the uptake and intracellular transit are similar to various endogenous and exogenous substances including bilirubin, hormones, drugs, and toxins. In a recent publication, we demonstrated that 99mTc-mebrofenin HBS has potential to predict postoperative liver failure in a patient population including both minor and major liver resections.17 The advantage of using 99mTc-mebrofenin HBS is the fact that the same cutoff value can be used for both patients with a compromised or normal liver parenchyma, which makes the test applicable in patients with an uncertain quality of the liver parenchyma. However, it remains uncertain if 99mTc-mebrofenin HBS is sufficiently accurate to predict liver failure in a population containing high-risk patients requiring major hepatic resection. This study compares preoperative FRL function assessed by HBS with FRL-V, expressed as %FRL-V and sFRL, in the prediction of postoperative liver failure after major liver resection in high-risk patients.
Patients and Methods
Patients
Between May 2000 and November 2006, 213 patients underwent a partial hepatectomy. Of all patients undergoing major liver resection (three or more Couinaud segments), both CT volumetry and HBS were preoperatively performed in 71 patients. Sixteen patients were excluded from the study because of preoperative PVE (n = 15) or partial portal vein thrombosis (n = 1) in the time period between HBS and CT volumetry. Hence, a group of 55 patients was retrospectively analyzed with the approval of our Institutional Review Board with waiver of informed consent. Table 1 summarizes the types of resection performed. Patients with a preoperative suspicion of hilar cholangiocarcinoma underwent an (extended) hemihepatectomy combined with hilar resection and caudate lobe resection. In cholestatic patients, preoperative biliary drainage was performed more than 6 weeks prior to surgery using endoscopic retrograde cholangiopancreatography or percutaneous transhepatic drainage.
Table 1.
Types of Liver Resection with the Corresponding Weight of the Resection Specimen
| procedure | Number of patients | Percentage | Weight resection specimen (g) |
|---|---|---|---|
| Extended right hemihepatectomy | 14 | 25.5 | 975 ± 247 |
| Right hemihepatectomy | 26 | 47.2 | 936 ± 396 |
| Extended left hemihepatectomy | 1 | 1.8 | 443 |
| Left hemihepatectomy | 14 | 25.5 | 348 ± 120 |
| Total | 55 | 100.0 |
Pre- and perioperative factors associated with postoperative morbidity and mortality were analyzed (Table 5). Histopathology of the resection specimen was assessed by an experienced pathologist taking into account features of cholestasis, steatosis, fibrosis, and chronic inflammation.
Table 5.
Overview of the Sensitivity, Specificity, PPV, NPV as well as likelihood ratio’s for FRL-F, %FRL-V, and sFRL in the Prediction of Postoperative Liver Failure
| Outcome parameter | FRL-F | %FRL-V | sFRL |
|---|---|---|---|
| Cutoff value | 2.69%/min/m2 | Normal liver <30% | Normal liver <30% |
| Compromised liver <40% | Compromised liver <40% | ||
| Sensitivity | 89% | 78% | 67% |
| Specificity | 87% | 80% | 87% |
| PPV | 57% | 44% | 50% |
| NPV | 98% | 95% | 93% |
| LR+ | 6.8 | 4.0 | 5.1 |
| LR− | 0.12 | 0.19 | 0.38 |
FRL future remnant liver, FRL-Volperc future remnant liver/total liver volume percentage, PPV positive predictive value, NPV negative predictive value, LR+ likelihood ratio for positive test result, LR− likelihood ratio for negative test result
Postoperative complications were recorded according to the modified classification of surgical complications proposed by Dindo et al.18 In-hospital complications were recorded as well as complications requiring hospital readmission within 3 months related to the operation. Minor complications included grade 1 and grade 2 complications. Major complications were defined as grade 3 and severe complications as grade 4 and grade 5 complications. Liver failure was defined as bilirubin plasma levels >50 µmol/l and/or prothrombin time index <50%,19 elevated plasma ammonia levels combined with signs of hepatic encephalopathy and/or hepatorenal syndrome, requiring intensive care treatment.
Surgical Technique
Surgery was performed under low central venous pressure (<4 cm H2O). Liver parenchymal transsection was performed using Cavitron Ultrasonic Surgical Aspirator (Valley Lab, Boulder, CO, USA). Pringle maneuver was applied in 29 patients (54%) to reduce intraoperative blood loss, with a mean ischemic period of 37 ± 13 min. Intermittent clamping was applied in eight patients (15%).
Scintigraphic Imaging and Data Acquisition
HBS was performed using 99mTc-mebrofenin as previously described.14,15 Briefly, after injection of 85 MBq of 99mTc-mebrofenin (Bridatec; GE-Amersham Health), dynamic images were obtained with a γ-camera (Diacam, Siemens, Milwaukee, WI, USA) for 60 min. During the first 10 min, 60 frames of 10 s were acquired (liver uptake phase) followed by 50 frames of 1 min (liver excretion phase). Total hepatic 99mTc-mebrofenin uptake rate was calculated as described by Ekman et al.20 On preoperative HBS, regions of interest (ROIs) were drawn around the total liver, the heart (serving as blood pool), and the total field of view. From these ROIs, three time–activity curves were generated (Fig. 1). Total hepatic 99mTc-mebrofenin uptake rate, representing total liver function (TL-F), was calculated as percent per minute: (%/min) (of the injected dose) based on these three parameters. Calculations of hepatic 99mTc-mebrofenin uptake rate were performed using measured values obtained between 150 and 350 s postinjection to ensure that hepatic uptake calculations were performed during a phase of homogenous distribution of the agent in the blood pool, before occurrence of the rapid phase of hepatic excretion. To compensate for differences in individual metabolic requirements, TL-F was divided by BSA and expressed as percent per minute per square meter: (%/min/m2). For determination of FRL uptake, a ROI was drawn around the FRL by two independent investigators, blinded for the results, according to the performed resection, and interobserver variation was calculated. The round ligament was used as the border between segment three and four. Cantlie’s line, projected on the liver surface as a plane between the middle of the gallbladder fossa (visible in the late phase of the scintigraphy) and the inferior caval vein, was used as a border between the right and left liver lobes. In addition, the anterior projection of the liver on the CT volumetry was used as a guideline for delineating the FRL on the HBS images (Fig. 1). FRL uptake function (FRL-F) was calculated by dividing counts within the delineated FRL by the total liver counts and multiplying this factor with total liver 99mTc-mebrofenin uptake (TL-F) and expressed as percent per minute per square meter: (%/min/m2). In 33 patients, a postoperative HBS was performed within 3 days after the operation to measure actual remnant liver function.
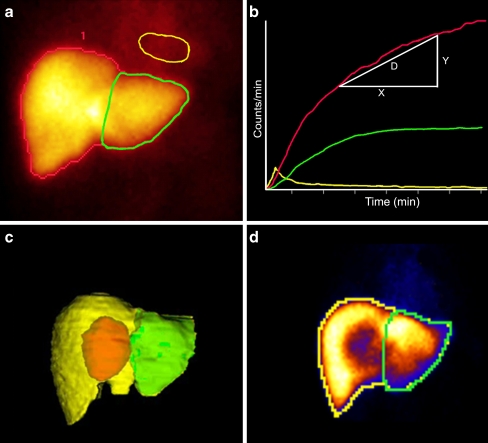
Figure 1.
An example is shown of summed HBS images from 150–300 s after i.v. injection of 99mTc-mebrofenin (a). A ROI is drawn around the entire liver (red line) and around the mediastinum (blood pool; yellow line). A third ROI is drawn around the future remnant liver (green line). A blood pool corrected liver-uptake time–activity curve is shown in b. The hepatic 99mTc-mebrofenin uptake is calculated as an increase of 99mTc-mebrofenin uptake (y-axis) per minute over a time period of 200 s (x-axis). c The use of the anterior projection of the liver on the CT volumetry image as a guideline for delineating the FRL on the HBS image (d).
CT Volumetry
Contrast-enhanced CT scans were generated with a helical scanner (Philips, Eindhoven, The Netherlands). Manual 3D reconstructions of the liver were made using reconstructed 5-mm-thick axial slices from 2–3-mm original slices. The total liver as well as tumor(s) and the FRL were manually outlined using portal and hepatic veins as landmarks for segmental division. Integrated software (Mx-View 3.52, Philips Medical Systems) was used to calculate total liver volume (TL-V), tumor volume (TV), and FRL-V. All delineations were made by an experienced radiologist. FRL-V was expressed as percentage of TL-V using the formula:
 |
The nontumorous total liver volume (NTTL-V) was calculated by excluding the tumor volume from the TL-V.
Standardized FRL Measurements
FRL-V was determined using CT volumetry, while total liver volume (calTL-V) was calculated using a formula based on BSA6:  .
.
The sFRL was calculated as the percentage between FRL-V and calculated TL-V.
Preoperative Risk Assessment
Receiver operator characteristics (ROC) curve analysis was used to calculate the optimal cutoff value for FRL-F in predicting postoperative liver failure. Cutoff values were determined based on the following assumptions: Firstly, the chance that liver failure would develop while the test result was above the cutoff value needed to be as low as possible. Secondly, a test result below the cutoff value should accurately select high-risk patient who might benefit from PVE. Based on literature, cutoff values for %FRL-V and sFRL were set at 30% for patients with normal liver parenchyma9 and 40% for patients with a compromised liver.10 Positive predictive values (PPV), negative predictive values (NPV), as well as sensitivity and specificity were determined for each method.
Statistical Analysis
Statistical analysis was performed with GraphPad Prism (GraphPad Software, San Diego, CA, USA) and Statistical Package for Social Sciences (SPSS 12.02, Chicago, IL, USA). ROC curve analysis was used to identify a cutoff value for FRL-F in predicting postoperative liver failure. Univariate analysis of preoperative and intraoperative variables was performed by the independent t test for continuous parameters and by Pearson’s 2tests and Fisher’s exact test for categorical data. Correlation between variables was tested using the Pearson correlation coefficient r. Continuous data were compared by independent sample t test and expressed as mean ± standard deviation. All statistical tests were two-tailed, and differences were considered significant at a P value of ≤0.05.
Results
Patient Characteristics
CT volumetry and 99mTc-mebrofenin HBS were performed in 55 patients (male 26, female 29, mean age 59 ± 13 years). Indications for liver resection are shown in Table 2. Thirty patients were diagnosed with a compromised liver parenchyma based on the histopathological evaluation of the resection specimen by an experienced pathologist, including cirrhosis (n = 2), severe fibrosis (n = 3), steatosis (>30% of the hepatocytes affected; n = 3), severe cholestasis (n = 8), chronic inflammation (n = 3), or a combination of these diseases (n = 11).
Table 2.
Indications for Liver Resection
| Liver metastasis (n = 14) |
| Hilar cholangiocarcinoma (n = 19) |
| Intrahepatic cholangiocarcinoma (n = 3) |
| Hepatocellular carcinoma (n = 6) |
| Benign biliary strictures (n = 7) |
| Benign lesions (n = 6) |
Liver Function and Liver Volume
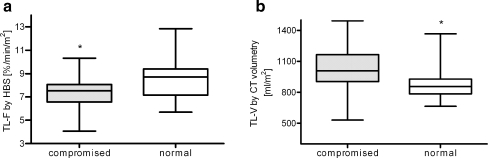
TL-F was significantly lower in patients with parenchymal liver disease (7.4 ± 1.4%/min/m2) as compared to patients with healthy liver parenchyma (8.5 ± 1.7%/min/m2, P = 0.007). NTTL-V was significantly larger in patients with compromised livers (1,037.1 ± 208.0 vs. 877.0 ± 143.3 mL/m2, P = 0.001; Fig. 2).
Figure 2.
Total hepatic 99mTc-mebrofenin uptake according to parenchymal status. Patients with parenchymal liver disease had significantly less liver (uptake) function (gray box, 7.4 ± 1.4%/min/m2) as compared to patients with healthy liver parenchyma (white box, 8.5 ± 1.7%/min/m2, P = 0.007; a). Total liver volume: (NTTL-V) was significantly higher in patients with compromised livers (1,037.1 ± 208.0 vs. 877.0 ± 143.3 mL/m2, P = 0.001; b).
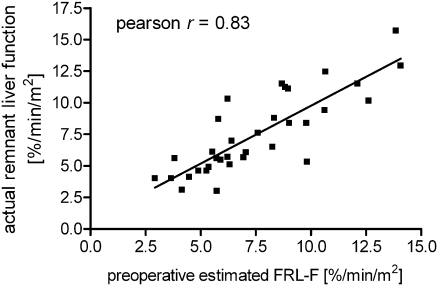
According to the type of resection performed, FRL-F was calculated for each individual patient by two independent observers. The interobserver agreement was excellent (Pearson r = 0.97), and Bland–Altman analysis revealed almost no bias between the two observers (mean bias of 0.00058 with 95% limit of agreement between −0.835 and 0.836). Preoperative FRL-F correlated strongly with actual postoperative remnant liver function determined within 3 days after surgery (Pearson r = 0.83, P < 0.0001; Fig. 3). Liver weight of the resection specimen revealed a strong correlation (Pearson r = 0.91, P < 0.0001) with its volume assessed by CT volumetry, confirming the CT measurements.
Figure 3.
Scatter plot showing the correlation between preoperative FRL-F and actual postoperative remnant liver function measured within 3 days after surgery (33 patients, Pearson r = 0.81, P < 0.0001).
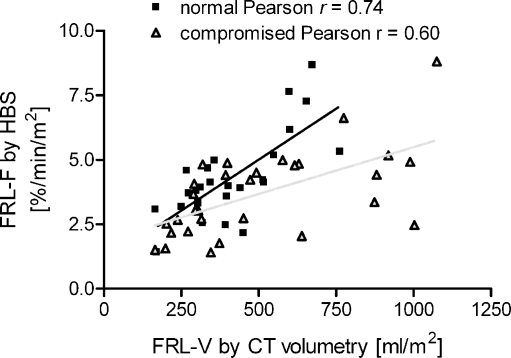
FRL-V correlated well with FRL-F (Pearson r = 0.72, P = 0.0001) in patients with normal livers. In contrast, patients with a compromised liver demonstrated only a moderate correlation between FRL-V and FRL-F (Pearson r = 0.61, P < 0.0003). The slope coefficient of the linear regression curve indicated that FRL-V is associated with significantly (P = 0.0015, analysis of covariance test) reduced FRL-F in compromised livers as compared to normal livers (Fig. 4).
Figure 4.
Scatter plot showing the correlation between FRL-F and FRL-V. In patients with normal livers (black line), FRL-V correlated well with FRL-F (Pearson r = 0.71, P = 0.0001). Patients with compromised livers (gray line) showed a moderate correlation between FRL volume and FRL function (Pearson r = 0.61, P < 0.0003).
Postoperative Complications
In 42 of the 55 (76%) patients, one or more complications occurred following liver resection (Table 3). Minor and major complications were evident in 14 patients (25%) and 13 patients (24%), respectively. Fifteen patients (27%) developed severe complications requiring ICU treatment, and the mortality rate was 15%. Patients with severe complications had significantly lower FRL-F as compared to patients with no complications (P = 0.0043), minor complications (P = 0.0028), or major complications (P = 0.0046)
Table 3.
Postoperative Complications
| Grade 0 (n = 13) | No complications |
| Grade 1* (n = 5) | Minor complications |
| Grade 2* (n = 9) | Minor complications |
| Grade 3a (n = 12) | Major complications |
| Grade 3b (n = 1) | Major complications |
| Grade 4a (n = 5) | Severe complications |
| Grade 4b (n = 2) | Severe complications |
| Grade 5 (n = 8) | Severe complications |
Grade 1 needed no therapy except analgetics, diuretics, anti-emetics, and physiotherapy. Grade 2 complications required pharmacological treatment. Grade 3 complications required surgical, endoscopic, or radiological intervention (grade 3a under local anesthetics, grade 3b under general anesthetics). Grade 4 complications included life-threatening complications requiring ICU management (grade 4a with single organ dysfunction, grade 4b with multi-organ failure). Grade 5 complications resulted in death
*One patient could have multiple grade 1 or 2 complications
Nine patients (16%) developed postoperative liver failure, of which eight patients died. In four patients, liver failure was evident within 1 week after the operation. Five patients developed liver failure within several weeks after the operation in conjunction with signs of sepsis. Evidence of a compromised liver was seen in eight patients (89%), and in seven patients, an extended hemihepatectomy had been performed. The FRL-F was significantly lower in patients with postoperative liver failure (2.18% vs. 4.32%/min/m2, P = 0.0001).
Preoperative and Intraoperative Parameters Associated with Liver Failure
Univariate analysis revealed that elderly patients (P = 0.043), small %FRL-V (P = 0.024), small sFRL (P = 0.012), small FRL-F (P = 0.001), resection type (P = 0.001), prolonged operating time (P = 0.0018), increased blood loss (P = 0.0018) during the operation, and the presence of a compromised liver parenchyma (P = 0.024) were significantly associated with postoperative liver failure (Table 4). Due to a small sample size in the liver failure group (n = 9), no multivariate analysis was performed.
Table 4.
Comparison of Pre- and Intraoperative Parameters in Patients with or Without Liver Failure
| Patients with liver failure (n = 9) | Patients without liver failure (n = 46) | P value | |
|---|---|---|---|
| Demographics | |||
| Male/female | 7:2 | 19:27 | 0.069a |
| Age | 67.1 ± 6.0 (58–67) | 57.1 ± 13.7 (18–78) | 0.027b |
| BMI | 25.1 ± 2.1 | 24.0 ± 3.6 | 0.33b |
| FRL volume | |||
| %FRL-V (%) | 35.0 ± 22.0 | 49.7% ± 17.8 | 0.013b |
| sFRL (%) | 35.2 ± 9.2 | 49.2% ± 3.6 | 0.018b |
| FRL-F (%/min/m2) | 2.2 ± 0.6 | 4.3% ± 1.6 | 0.001b |
| Comorbidity | |||
| Diabetes (yes/no) | 2:7 | 5:41 | 0.32a |
| Chronic hepatitis (yes/no) | 2:7 | 3:43 | 0.18a |
| Vascular disease(yes/no) | 3:6 | 9:37 | 0.39a |
| Compromised liver (yes/no) | 8:1 | 22:24 | 0.024a |
| Resection type | |||
| Left hemihepatectomy | 1 | 13 | |
| Right hemihepatectomy | 1 | 25 | 0.001c |
| Extended hemihepatectomy | 7 | 8 | |
| Preoperative laboratory values | |||
| AST | 51.4 ± 19.1 | 48.2 ± 32.4 | 0.24b |
| ALT | 57.9 ± 27.2 | 65.6 ± 65.6 | 0.55b |
| Bilirubin | 19.9 ± 14.9 | 14.2 ± 12.0 | 0.20b |
| AF | 265.2 ± 204.6 | 280.1 ± 260.5 | 0.76b |
| GGT | 409.9 ± 272.7 | 392.7 ± 605.7 | 0.13b |
| Albumin | 39.4 ± 5.8 | 39.5 ± 5.9 | 0.84b |
| Prothrombin time | 13.0 ± 1.5 | 13.1 ± 0.90 | 0.63b |
| Intraoperative parameters | |||
| Blood loss (mL) | 5,200 cc ± 2,673 | 3,025 ± 2,464 | 0.021b |
| Operating time (min) | 507.4 ± 135.1 | 382.3 ± 131 | 0.011b |
| Pringle maneuver yes/intermittent/no | 3:2:3 | 26:6:14 | 0.62c |
| Pringle time (min) | 35.0 ± 5.0 | 36.71 ± 13.5 | 0.96b |
| Intermittent total ischemia time (min) | 40.0 | 47.6 | 0.5b |
AST aspartate aminotransferase, ALT alanine aminotransferase, AF alkaline phosphatase, GGT gamma-glutamyltransferase, BMI body mass index
aFisher’s exact test
bMann–Whitney U test
c χ 2 test
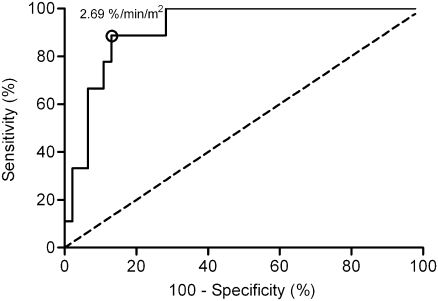
Preoperative Prediction of Postoperative Liver Failure
ROC analysis revealed that a cutoff value for FRL-F of 2.69%/min/m2 was able to identify patients who developed postoperative liver failure with a sensitivity of 89% and a specificity of 87% (Fig. 5). The risk of postoperative liver failure in patients with a FRL-F above 2.69%/min/m2 was 2.4% (with a NPV of 97.6% and a likelihood ratio for a negative test result of 0.12). The PPV was 57.1% with a likelihood ratio for a positive test result of 6.8. Table 5 summarizes the sensitivity, specificity, PPV, NPV, and likelihood ratios of the different tests. For an accurate use of %FRL-V and sFRL, two cutoff values were used, and patients were divided in patients with a normal liver parenchyma and patients with a compromised liver parenchyma based on the histopathology of the resection specimen. Using 99mTc-mebrofenin HBS, one cutoff value sufficed in both compromised and noncompromised patients. Assuming that, of all the patients, the quality of the liver parenchyma was preoperatively known, sensitivity, specificity, and positive and negative predictive values were still better for FRL-F compared to %FRL-V and sFRL (Table 5).
Figure 5.
Receiver operator characteristic curve analysis of FRL-F in the prediction of liver failure. A cutoff value for FRL-F of 2.69%/min/ m2 identified patients with a significant risk of developing postoperative liver failure (area under the curve = 0.916; 95% confidence interval 0.837–0.994).
Discussion
Accurate measurement of liver function before liver resection is crucial in the assessment of resectability, especially in patients requiring major liver resection. The availability of preoperative PVE to induce hypertrophy of the FRL has further increased the importance of preoperative assessment of regional hepatic function.7,21–24 In the present study, dynamic planar 99mTc-mebrofenin HBS was used to measure liver function. This technique can be implemented in every hospital with a nuclear medicine department, is easy to perform, and has a small interobserver variability. More importantly, preoperative estimated function of the future remnant liver (FRL-F) correlates strongly with actual postoperative liver function,14 indicating that dynamic planar 99mTc-mebrofenin HBS is an accurate method to assess FRL-F.
In this study, we compared FRL-F measured by 99mTc-mebrofenin HBS with two parameters based on CT volumetry, which are widely accepted parameters to determine the possible extent of resection.1–5 Patients with a compromised liver had a significantly lower liver function compared to patients with normal liver parenchyma, whereas their liver volume was significantly larger. FRL-V showed a strong relation with FRL-F in patients with normal liver parenchyma. In contrast, FRL-V and FRL-F only moderately correlated in patients with compromised liver parenchyma in whom FRL-V was associated with reduced FRL-F. The impact of different parenchymal diseases such as steatosis, cholestasis, and fibrosis on liver function and liver volume is unknown and may vary among individuals. In addition, parenchymal damage is often not equally distributed,11 which can partially explain the moderate correlation between FRL-V and FRL-F in patients with compromised livers. ROC curve analysis yielded an FRL-F cutoff of 2.69%/min/m2 for the prediction of postoperative liver failure. This cutoff value is comparable to the cutoff value determined in a patient population including both minor and major resections.17
A reliable preoperative test should primarily establish whether patients with a FRL-F above the critical threshold can be safely resected. One patient developed liver failure despite a FRL-F above 2.69%/min/m2 (Table 6). This cirrhotic patient developed massive necrosis after left hemihepatectomy, due to an obliterated right hepatic artery and a compromised portal venous system. When CT volumetry would have been used as selection criterion for operation, two patients developed liver failure despite a %FRL-V of more than 40% (Table 6). Standardized FRL wrongly predicted a safe resection in three patients (Table 6). Although the formula generally used to calculate TL-V based on BSA is used for all patients, it is derived from patients with normal liver parenchyma. In our study, patients with a compromised liver had significantly larger liver volumes resulting in a relatively larger FRL-V in relation to their BSA. As a consequence, there is an overestimation of liver function in these patients.
Table 6.
Overview of the Results of the Three Different Preoperative Tests in Patients with Liver Failure
| Liver parenchyma | FRL-F (%/min/m2) | %FRL-V (%) | sFRL (%) | |
|---|---|---|---|---|
| 1 | Normal | 2.17 | 46 | 57 |
| 2 | Compromised | 2.52 | 38 | 24 |
| 3 | Compromised | 2.67 | 22 | 38 |
| 4 | Compromised | 1.56 | 20 | 23 |
| 5 | Compromised | 2.22 | 32 | 31 |
| 6 | Compromised | 1.41 | 29 | 41 |
| 7 | Compromised | 2.17 | 24 | 25 |
| 8 | Compromised | 1.51 | 16 | 19 |
| 9 | Compromised | 3.36 | 88 | 101 |
The marked values indicate a false negative result of the test
Secondly, a preoperative test should be accurate in selecting high-risk patients who might benefit from PVE, without treating patients unnecessarily. Despite having a FRL-F below the critical value of 2.69%/min/m2, 43% of these high-risk patients did not develop liver failure. In literature, a similar percentage was reported when using CT volumetry for the prediction of postoperative hepatic dysfunction.8 Additional negative predictive factors, including high body mass index, significant intraoperative blood loss, and prolonged operating time, were described in patients with hepatic dysfunction, underlining the multifactorial cause of postoperative liver failure. In our study, univariate analysis revealed that, besides small FRL volume and function, increased intraoperative blood loss, prolonged operating time, a compromised liver parenchyma and older age were associated with liver failure. Unfortunately, a multivariate analysis was not possible in our study due to the small number of patients with postoperative liver failure. Cutoff values for the prediction of postoperative complications and hepatic dysfunction have been reported using CT volumetry,3,4,7–9 indocyanine green clearance test,25 galactose elimination capacity,26 and 99mTc-GSA scintigraphy.27–30 These cutoff values were, however, mostly not based on accurate risk calculations and no or inappropriate multivariate analyses had been performed.
Morbidity and mortality rates reported in our study were high, which is explained by the patients selected for this study. We only included patients undergoing major liver resection of which the majority (55%) had parenchymal liver disease. A relatively high proportion (39%) of patients had undergone resection on the suspicion of hilar cholangiocarcinoma, including six patients who had developed postoperative liver failure. These patients require large resections and biliary anastomoses, with increased risk of postoperative morbidity and mortality, reported up to 10–20%.31–33 The overall postoperative mortality in patients operated for benign lesions or liver metastasis in our institution is 2%.34 In addition, none of the patients included in this study had undergone PVE. In some patients who developed postoperative liver failure, PVE would be indicated in retrospect; however, in these patients, the performed resection was larger than anticipated because of unexpected intraoperative findings. Patients included in this study may be different from patient populations in other clinical practices in which most patients have noncompromised livers. However, the fact that postoperative morbidity and mortality were considerable did add necessary power to the study in which risk assessment was the primary goal. Further research is, however, warranted for subgroup analysis of different patient populations.
The main advantage of HBS lies in the fact that liver function is measured, taking into account the presence of underlying parenchymal liver disease. Hence, one cutoff value for the prediction of liver failure suffices in all possible patients regardless of the quality of the liver parenchyma. In contrast, volumetric assessment of the FRL requires two distinct cutoff values for patients with a compromised or noncompromised liver, assuming that the quality of the liver parenchyma is known. Especially in patients with uncertain quality of liver parenchyma, preoperative HBS is therefore of more value than %FRL-V or sFRL. The results of our study have led us to use HBS routinely, in addition to CT volumetry, in all patients considered for major liver resection. Preoperative PVE is performed when FRL-F is lower than 2.69%/min/m2 or %FRL-V is less than 30%. Although around 40% of these patients will not develop liver failure, the risk of a potentially lethal complication outweighs the relatively low complication rate observed after PVE.35
Conclusion
HBS is a simple technique that can be implemented in every hospital with a nuclear medicine department. It is a valuable technique to estimate the risk of postoperative liver failure in high-risk patients undergoing major liver resection. Especially in patients with uncertain quality of the liver parenchyma, 99mTc-mebrofenin HBS is of more value than CT volumetry since only one cutoff value can be used in both normal and compromised livers. Therefore, additional HBS can improve risk assessment in patients requiring extensive liver resection.
Acknowledgments
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Shirabe K, Shimada M, Gion T, Hasegawa H, Takenaka K, Utsunomiya T, Sugimachi K. Postoperative liver failure after major hepatic resection for hepatocellular carcinoma in the modern era with special reference to remnant liver volume. J Am Coll Surg. 1999;188:304–309. doi: 10.1016/S1072-7515(98)00301-9. [DOI] [PubMed] [Google Scholar]
- 2.Kubota K, Makuuchi M, Kusaka K, Kobayashi T, Miki K, Hasegawa K, Harihara Y, Takayama T. Measurement of liver volume and hepatic functional reserve as a guide to decision-making in resectional surgery for hepatic tumors. Hepatology. 1997;26:1176–1181. doi: 10.1053/jhep.1997.v26.pm0009362359. [DOI] [PubMed] [Google Scholar]
- 3.Shoup M, Gonen M, D’Angelica M, Jarnagin WR, DeMatteo RP, Schwartz LH, Tuorto S, Blumgart LH, Fong Y. Volumetric analysis predicts hepatic dysfunction in patients undergoing major liver resection. J Gastrointest Surg. 2003;7:325–330. doi: 10.1016/S1091-255X(02)00370-0. [DOI] [PubMed] [Google Scholar]
- 4.Vauthey JN, Chaoui A, Do KA, Bilimoria MM, Fenstermacher MJ, Charnsangavej C, Hicks M, Alsfasser G, Lauwers G, Hawkins IF, Caridi J. Standardized measurement of the future liver remnant prior to extended liver resection: methodology and clinical associations. Surgery. 2000;127:512–519. doi: 10.1067/msy.2000.105294. [DOI] [PubMed] [Google Scholar]
- 5.Abdalla EK, Hicks ME, Vauthey JN. Portal vein embolization: rationale, technique and future prospects. Br J Surg. 2001;88:165–175. doi: 10.1046/j.1365-2168.2001.01658.x. [DOI] [PubMed] [Google Scholar]
- 6.Vauthey JN, Abdalla EK, Doherty DA, Gertsch P, Fenstermacher MJ, Loyer EM, Lerut J, Materne R, Wang X, Encarnacion A, Herron D, Mathey C, Ferrari G, Charnsangavej C, Do KA, Denys A. Body surface area and body weight predict total liver volume in Western adults. Liver Transpl. 2002;8:233–240. doi: 10.1053/jlts.2002.31654. [DOI] [PubMed] [Google Scholar]
- 7.Abdalla EK, Barnett CC, Doherty D, Curley SA, Vauthey JN. Extended hepatectomy in patients with hepatobiliary malignancies with and without preoperative portal vein embolization. Arch Surg. 2002;137:675–680. doi: 10.1001/archsurg.137.6.675. [DOI] [PubMed] [Google Scholar]
- 8.Schindl MJ, Redhead DN, Fearon KC, Garden OJ, Wigmore SJ. The value of residual liver volume as a predictor of hepatic dysfunction and infection after major liver resection. Gut. 2005;54:289–296. doi: 10.1136/gut.2004.046524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yigitler C, Farges O, Kianmanesh R, Regimbeau JM, Abdalla EK, Belghiti J. The small remnant liver after major liver resection: how common and how relevant? Liver Transpl. 2003;9:S18–S25. doi: 10.1053/jlts.2003.50194. [DOI] [PubMed] [Google Scholar]
- 10.Clavien PA, Emond J, Vauthey JN, Belghiti J, Chari RS, Strasberg SM. Protection of the liver during hepatic surgery. J Gastrointest Surg. 2004;8:313–327. doi: 10.1016/j.gassur.2003.12.006. [DOI] [PubMed] [Google Scholar]
- 11.Ratziu V, Charlotte F, Heurtier A, Gombert S, Giral P, Bruckert E, Grimaldi A, Capron F, Poynard T. Sampling variability of liver biopsy in nonalcoholic fatty liver disease. Gastroenterology. 2005;128:1898–1906. doi: 10.1053/j.gastro.2005.03.084. [DOI] [PubMed] [Google Scholar]
- 12.Lindor KD, Bru C, Jorgensen RA, Rakela J, Bordas JM, Gross JB, Rodes J, McGill DB, Reading CC, James EM, Charboneau JW, Ludwig J, Batts KP, Zinsmeister AR. The role of ultrasonography and automatic-needle biopsy in outpatient percutaneous liver biopsy. Hepatology. 1996;23:1079–1083. doi: 10.1002/hep.510230522. [DOI] [PubMed] [Google Scholar]
- 13.McGill DB, Rakela J, Zinsmeister AR, Ott BJ. A 21-year experience with major hemorrhage after percutaneous liver biopsy. Gastroenterology. 1990;99:1396–1400. doi: 10.1016/0016-5085(90)91167-5. [DOI] [PubMed] [Google Scholar]
- 14.Bennink RJ, Dinant S, Erdogan D, Heijnen BH, Straatsburg IH, van Vliet AK, van Gulik TM. Preoperative assessment of postoperative remnant liver function using hepatobiliary scintigraphy. J Nucl Med. 2004;45:965–971. [PubMed] [Google Scholar]
- 15.Erdogan D, Heijnen BH, Bennink RJ, Kok M, Dinant S, Straatsburg IH, Gouma DJ, van Gulik TM. Preoperative assessment of liver function: a comparison of 99mTc-mebrofenin scintigraphy with indocyanine green clearance test. Liver Int. 2004;24:117–123. doi: 10.1111/j.1478-3231.2004.00901.x. [DOI] [PubMed] [Google Scholar]
- 16.Krishnamurthy S, Krishnamurthy GT. Technetium-99m-iminodiacetic acid organic anions: review of biokinetics and clinical application in hepatology. Hepatology. 1989;9:139–153. doi: 10.1002/hep.1840090123. [DOI] [PubMed] [Google Scholar]
- 17.Dinant S, de Graaf W, Verwer BJ, Bennink RJ, van Lienden KP, Gouma DJ, van Vliet AK, van Gulik TM. Risk assessment of posthepatectomy liver failure using hepatobiliary scintigraphy and CT volumetry. J Nucl Med. 2007;48:685–692. doi: 10.2967/jnumed.106.038430. [DOI] [PubMed] [Google Scholar]
- 18.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Balzan S, Belghiti J, Farges O, Ogata S, Sauvanet A, Delefosse D, Durand F. The “50–50 criteria” on postoperative day 5: an accurate predictor of liver failure and death after hepatectomy. Ann Surg. 2005;242:824–828. doi: 10.1097/01.sla.0000189131.90876.9e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ekman M, Fjalling M, Holmberg S, Person H. IODIDA clearance rate: a method for measuring hepatocyte uptake function. Transplant Proc. 1992;24:387–388. [PubMed] [Google Scholar]
- 21.Makuuchi M, Thai BL, Takayasu K, Takayama T, Kosuge T, Gunven P, Yamazaki S, Hasegawa H, Ozaki H. Preoperative portal embolization to increase safety of major hepatectomy for hilar bile duct carcinoma: a preliminary report. Surgery. 1990;107:521–527. [PubMed] [Google Scholar]
- 22.Nagino M, Nimura Y, Kamiya J, Kondo S, Uesaka K, Kin Y, Hayakawa N, Yamamoto H. Changes in hepatic lobe volume in biliary tract cancer patients after right portal vein embolization. Hepatology. 1995;21:434–439. [PubMed] [Google Scholar]
- 23.Azoulay D, Castaing D, Krissat J, Smail A, Hargreaves GM, Lemoine A, Emile JF, Bismuth H. Percutaneous portal vein embolization increases the feasibility and safety of major liver resection for hepatocellular carcinoma in injured liver. Ann Surg. 2000;232:665–672. doi: 10.1097/00000658-200011000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Azoulay D, Castaing D, Smail A, Adam R, Cailliez V, Laurent A, Lemoine A, Bismuth H. Resection of nonresectable liver metastases from colorectal cancer after percutaneous portal vein embolization. Ann Surg. 2000;231:480–486. doi: 10.1097/00000658-200004000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lau H, Man K, Fan ST, Yu WC, Lo CM, Wong J. Evaluation of preoperative hepatic function in patients with hepatocellular carcinoma undergoing hepatectomy. Br J Surg. 1997;84:1255–1259. doi: 10.1002/bjs.1800840917. [DOI] [PubMed] [Google Scholar]
- 26.Redaelli CA, Dufour JF, Wagner M, Schilling M, Husler J, Krahenbuhl L, Buchler MW, Reichen J. Preoperative galactose elimination capacity predicts complications and survival after hepatic resection. Ann Surg. 2002;235:77–85. doi: 10.1097/00000658-200201000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fujioka H, Kawashita Y, Kamohara Y, Yamashita A, Mizoe A, Yamaguchi J, Azuma T, Furui J, Kanematsu T. Utility of technetium-99m-labeled-galactosyl human serum albumin scintigraphy for estimating the hepatic functional reserve. J Clin Gastroenterol. 1999;28:329–333. doi: 10.1097/00004836-199906000-00009. [DOI] [PubMed] [Google Scholar]
- 28.Kim YK, Nakano H, Yamaguchi M, Kumada K, Takeuchi S, Kitamura N, Takahashi H, Hasebe S, Midorikawa T, Sanada Y. Prediction of postoperative decompensated liver function by technetium-99m galactosyl-human serum albumin liver scintigraphy in patients with hepatocellular carcinoma complicating chronic liver disease. Br J Surg. 1997;84:793–796. doi: 10.1002/bjs.1800840616. [DOI] [PubMed] [Google Scholar]
- 29.Satoh K, Yamamoto Y, Nishiyama Y, Wakabayashi H, Ohkawa M. 99mTc-GSA liver dynamic SPECT for the preoperative assessment of hepatectomy. Ann Nucl Med. 2003;17:61–67. doi: 10.1007/BF02988261. [DOI] [PubMed] [Google Scholar]
- 30.Nanashima A, Yamaguchi H, Shibasaki S, Morino S, Ide N, Takeshita H, Sawai T, Nakagoe T, Nagayasu T, Ogawa Y. Relationship between indocyanine green test and technetium-99m galactosyl serum albumin scintigraphy in patients scheduled for hepatectomy: clinical evaluation and patient outcome. Hepatol Res. 2004;28:184–190. doi: 10.1016/j.hepres.2003.11.010. [DOI] [PubMed] [Google Scholar]
- 31.Jarnagin WR, Fong Y, DeMatteo RP, Gonen M, Burke EC, Bodniewicz BJ, Youssef BM, Klimstra D, Blumgart LH. Staging, resectability, and outcome in 225 patients with hilar cholangiocarcinoma. Ann Surg. 2001;234:507–517. doi: 10.1097/00000658-200110000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dinant S, Gerhards MF, Busch ORC, Obertop H, Gouma DJ, van Gulik TM. The importance of complete excision of the caudate lobe in resection of hilar cholangiocarcinoma. HPB. 2005;7:263–267. doi: 10.1080/13651820500372376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Belghiti J, Hiramatsu K, Benoist S, Massault P, Sauvanet A, Farges O. Seven hundred forty-seven hepatectomies in the 1990s: an update to evaluate the actual risk of liver resection. J Am Coll Surg. 2000;191:38–46. doi: 10.1016/S1072-7515(00)00261-1. [DOI] [PubMed] [Google Scholar]
- 34.Erdogan D, Busch OR, Gouma DJ, van Gulik TM. Morbidity and mortality after liver resection for benign and malignant hepatobiliary lesions. Liver Int. 2008;29:175–180. doi: 10.1111/j.1478-3231.2008.01806.x. [DOI] [PubMed] [Google Scholar]
- 35.Giraudo G, Greget M, Oussoultzoglou E, Rosso E, Bachellier P, Jaeck D. Preoperative contralateral portal vein embolization before major hepatic resection is a safe and efficient procedure: a large single institution experience. Surgery. 2008;143:476–482. doi: 10.1016/j.surg.2007.12.006. [DOI] [PubMed] [Google Scholar]