Abstract
Background. The current treatment of choice in patients with three-vessel coronary disease is coronary artery bypass grafting. The use of the left internal mammary artery in bypass grafting has shown superior long-term outcomes compared with venous grafting. In our study we assess the safety and feasibility of all-arterial coronary artery bypass graft surgery using the procedure as described by Tector et al. in 2001.
Methods. Between June 2001 and February 2007, we studied 133 patients eligible for non-emergency surgical revascularisation. Primary endpoints were death or re-infarction within a 30-day period. Secondary endpoints were the need for emergency coronary surgery, angioplasty and mediastinitis. Long-term follow-up had a mean duration of 33 months postoperatively.
Results. All 133 patients were successfully revascularised, 98% with the off-pump technique. In 93% of the patients (n=124) full arterial grafting was achieved using both internal mammary arteries. Thirty-day mortality was 1.5% (n=2), ten re-thoracotomies were performed, one myocardial infarction and one case of mediastinitis were reported. In the next four years six additional patients died. Most of these deaths were due to non-cardiovascular causes. Two patients required angioplasty because of distal bypass graft failure and one for new native coronary artery disease. Conclusion. All-arterial bypass grafting using both internal mammary arteries with the technique as described by Tector is safe and feasible without excess deep sternal wound infections. Late major adverse cardiac events are rare and due to distal graft dysfunction, which can be treated by percutaneous coronary intervention. (Neth Heart J 2010;18:7-11.)
Keywords: coronary artery disease, bypass grafting, angina, all arterial revascularisation, off-pump CABG
Coronary artery disease is the main cause of death in the Western world. The current treatment of choice in patients with complex three-vessel disease is coronary artery bypass grafting (CABG). This procedure is performed using both arterial and venous grafts. A major concern regarding the use of venous grafts is graft failure. This leads to a higher risk of recurrent angina, new myocardial infarction and the necessity of renewed interventions.1,2
Currently, many efforts are put into the comparison of bypass surgery with drug-eluting stenting to overcome the potential hazards and graft failures after CABG. The initial one-year follow-up results of the SYNTAX trial3 do not show a superiority of one of these techniques despite the fact that all the patients in the surgery group had been grafted with venous material and the left internal mammary artery (LIMA). Earlier, the ARTS trial4 found a need for revascularisation of 7% at three years of follow-up.
Coronary bypass grafting with the use of the LIMA has shown superior long-term outcomes compared with CABG with only venous grafts5,6 with respect to patency and reduced ischaemia rates. However, total arterial revascularisation was limited by technical difficulties. In 2001 Tector et al.7 described a technique in which both intra-thoracic arteries are used as grafts, making it possible to acquire full arterial revascularisation. Total arterial revascularisation may be considered the optimal surgical treatment for extensive coronary artery disease and may become next in line to be compared with optimal stenting using drugeluding stents. While awaiting and facilitating the planning of such comparison, we investigated the merits of off-pump total arterial revascularisation in our consecutive series of patients.
Methods
From June 2001 to February 2007, 799 patients were referred from the Alkmaar Medical Centre to the VU Medical Centre, Amsterdam, for coronary artery bypass grafting. Out of 208 patients operated by one surgeon, 133 received a Tector procedure (16.7%). This procedure was attempted on all non-emergency patients under 70 years of age; it was also attempted on older patients without suitable venous graft material or with general arteriosclerotic disease in order to prevent aortic clamping. Our primary endpoints were death or reinfarction within a 30-day period. Secondary endpoints were the need for emergency coronary surgery, angioplasty and mediastinitis. Preoperative risk was assessed for all patients using Euroscore ratings.8,9 Patient follow-up was done up until four years postoperatively in our outpatient clinic in Alkmaar.
Tector procedure
All procedures were carried out by one experienced surgeon (E.K.J.) and planned as an off-pump procedure. Both mammary arteries were dissected, leaving a small pedicle surrounding the arteries.
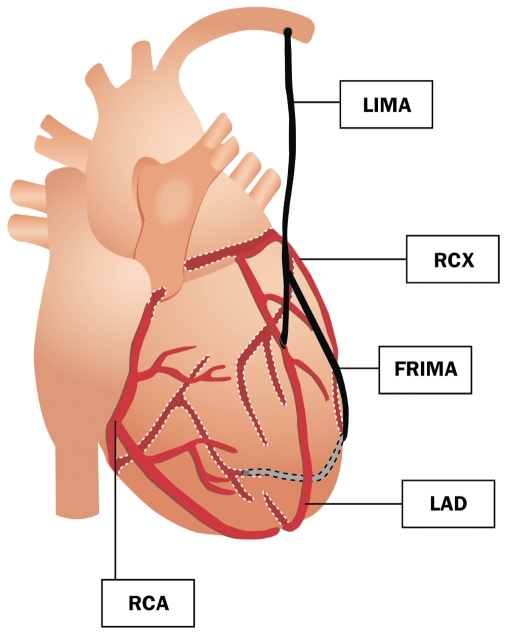
The free right internal mammary artery (FRIMA) graft is attached to the LIMA as a T graft (end to side) slightly distal from the site where the LIMA enters the pericardial cavity, just where it crosses the main pulmonary artery. The T graft anastomosis, approximately 8 mm long, is constructed using a running stitch with 8-0 monofilament suture. This T graft has an average length of 18 to 20 cm. Anterior revascularisation was performed first, using the LIMA to revascularise the left anterior descending coronary artery (LAD). The diagonal branches are bypassed either with the LIMA or FRIMA, depending on the anatomy. Subsequently, anastomoses to the lateral, posterior and inferior parts were made with the FRIMA (figure 1).
Figure 1.
Illustrated postoperative situation with the Tector technique. LIMA=left internal mammary artery, FRIMA=free right internal mammary artery, RCX=ramus circumflex, LAD=left anterior descending coronary artery, RCA=right coronary artery.
Results
Patients
In the six-year period studied, 133 consecutive patients (107 men and 26 women) underwent coronary artery bypass grafting with the intention of total arterial coronary bypass grafting. The patients had a mean age of 67±11 years and 17% had known diabetes. All patients had symptomatic multivessel coronary artery disease, 66% were operated on for an acute coronary syndrome and 41% had experienced a previous myocardial infarction, while four patients underwent previous coronary artery bypass surgery. The majority of the patients had a preserved left ventricular function. The mean preoperative Euroscore and log Euroscore were 3.7 (95% CI 3.2 to 4.2) and 4.5 (95% CI 3.4 to 5.5) respectively (table 1).
Table 1.
Demographic characteristics.
| Variable | N | % |
|---|---|---|
| Mean age (years) | 67 (±11) | |
| Men/women | 107/26 | (80/20) |
| Hypertension | 74 | 56 |
| Hypercholesterolemia (> 5 mmol/l) | 83 | 62 |
| Diabetes mellitus | 23 | 17 |
| Current smoker | 26 | 20 |
| Previous stroke | 13 | 10 |
| Previous myocardial infarction | 54 | 41 |
| Previous coronary angioplasty | 29 | 22 |
| Previous coronary artery bypass | 5 | 4 |
| Left ventricular function | ||
| - Poor (LVEF <35%) | 7 | 5 |
| - Moderate (LVEF 35-50%) | 39 | 30 |
| - Good (LVEF >50%) | 87 | 65 |
| Euroscore >4 | 45 | 34 |
| Multivessel disease | 133 | 100 |
| Operation indication | ||
| Stable angina | 45 | 34 |
| Acute coronary syndrome | 88 | 66 |
LVEF=left ventricular ejection fraction.
Operation
All patients were scheduled for a total arterial revascularisation according to the Tector technique. In all but one patient, the LIMA was used as the primary arterial graft. The remaining patient already had a patent LIMA anastomosed to the LAD at his first operation. The FRIMA was additionally used in all but one patient. The bypass operation could be performed without cardiopulmonary bypass in 98% of the patients. In three procedures it was necessary to convert to on-pump surgery due to haemodynamic instability. All patients were successfully revascularised (i.e. all preoperative planned anastomoses were successfully placed) and left the operating suite alive. Total arterial revascularisation was successful in 93%, while in nine patients (7%) additional venous grafts were needed as arterial grafts had insufficient length to allow for complete revascularisation. The number of proximal and distal anastomoses is given in table 2.
Table 2.
Procedure characteristics.
| Variable | Patients n=133 (%) | |
|---|---|---|
| Re-operation | 4 (3) | |
| Target vessels | LAD | 131 (99) |
| LCX | 119 (89) | |
| RCA | 97 (73) | |
| LIMA use | 131 (99) | |
| RIMA use | 131 (99) | |
| No. of proximal anastomoses | 0 | 125 (94) |
| 1 | 7 (5) | |
| 2 | 1 (1) | |
| No. of distal anastomoses | 1 | 0 |
| 2 | 4 (3) | |
| 3 | 40 (30) | |
| 4 | 56 (42) | |
| 5 | 30 (23) | |
| 6 | 3 (2) | |
| Off-pump procedures | 130 (98) | |
| Grafts | Arterial only | 124 (93) |
| Additional venous grafts | 9 (7) | |
| Technical outcome | Successful revascularisation | 133 (100) |
LIMA=left internal mammary artery, RIMA=right internal mammary artery, LAD=left anterior descending coronary artery, LCX=left circumflex artery, RCA=right coronary artery.
Thirty-day follow-up
In the 30-day follow-up period, two deaths (1.5%) were registered. One death was an 84-year-old male with a recent myocardial infarction, impaired left ventricular function and absent venous graft material, who died in the intensive care unit within 24 hours after the procedure, due to persistent cardiac failure. One death was a 73-year-old male with an uneventful recovery who was treated with acenocoumarol for atrial fibrillation. On the 17th day after the procedure he suffered a haematothorax that required resuscitation and a re-exploration. No active bleeding was found. The patient died 26 days after the procedure due to irreversible neurological damage. Only one patient (0.8%) suffered a postoperative myocardial infarction necessitating percutaneous intervention of the LIMA and FRIMA bypass graft.
There was a need for re-exploration for bleeding in ten patients (7.5%), six for surgical bleeding and four for haematological reasons (table 3).
Table 3.
Clinical endpoints at 30 days.
| Event at 30 days | Patients n=133 (%) |
|---|---|
| Death | 2 (1.5) |
| Re-infarction | 1* (0.7) |
| Angioplasty | 1* (0.7) |
| Rethoracotomy | 10 (7.5) |
| - Surgical bleeding | 6 (4.5) |
| - Coagulation disorder | 4 (3) |
| Deep sternal wound infection | 1 (0.7) |
* This is the same patient.
Late follow-up
All patients had a long-term follow-up with a median duration of 33 (1 to 74) months. After the initial hospitalisation period, six additional patients died. All of these deaths were non-cardiovascular; two died in a nursing home due to advanced age, two had a fatal CVA, one died following a trauma and one patient died in a diabetic coma. None of the patients suffered a myocardial infarction after their hospital discharge and repeat cardiovascular surgery was not necessary. Two patients were treated with percutaneous coronary intervention for late bypass graft dysfunction. In both patients the distal FRIMA graft was diseased and dysfunctional (at 13 and 19 months postoperatively). Both underwent successful PCI with stenting of the right coronary artery, with good long-term results. One patient had a percutaneous coronary intervention for new native coronary artery disease (table 4).
Table 4.
Clinical endpoints after 30 days, up until four years.
| Additional events after 30 days | Patients n=133 (%) |
|---|---|
| Death | 6 (4.5) |
| - In nursing home | 2 |
| - CVA | 2 |
| - Trauma | 1 |
| - Diabetic coma | 1 |
| Re-infarction | 0 |
| Re-CABG | 0 |
| Angioplasty | 3 (2.3) |
CVA=cerebral vascular accident, CABG=coronary artery bypass graft.
Discussion
Total arterial coronary bypass grafting using the Tector technique seems safe and is a feasible approach to treat multi-vessel coronary artery disease with a success of 98% at 30-day follow-up with two deaths and one myocardial infarction necessitating PCI. At late followup two patients had a PCI procedure for FRIMA graft dysfunction and one for new native coronary artery disease. These safety results are comparable with the 2.3% 30-day mortality described by Tector and colleagues4 and to the 2% overall in-hospital mortality found by Baskett et al. in a study of 71,470 patients undergoing CABG.8 Therefore, total arterial coronary bypass grafting using the Tector technique seems safe and is a feasible approach to treat multi-vessel coronary artery disease.
Arterial revascularisation
As early as the 1970s, reports were published that support the eligibility of arterial coronary bypasses over the use of venous grafts with regard to patency. An early recognised concern with venous grafts is graft failure, which may occur at two time intervals: either early failure due to technical difficulties or late failure due to progressive atherosclerosis of especially venous grafts or native coronary arteries. However, total arterial coronary bypass grafting has eluded surgeons for several decades due to technical difficulties. For example, the use of internal mammary arteries is limited by its anatomy. The LIMA has a limited range; particularly the inferior and posterior parts of the heart cannot be reached. Different techniques exist to achieve complete arterial revascularisation. Among others, the use of the radial artery10 and gastro-epiploic artery11 have been proposed. Various studies, however, showed improved survival rates and a smaller need for revascularisation when using both the internal mammary arteries.12-16 This procedure uses the RIMA as a free graft (FRIMA) which is subsequently anastomosed end-to-side to the LIMA. This enables surgeons to locate the FRIMA approximately 10 cm closer to the inferior and posterior superficial coronary arteries, making full arterial revascularisation possible for most patients with the use of internal thoracic arteries only.
Off-pump surgery
Another advantage of this Tector series was the opportunity to use an off-pump operation technique, which may facilitate a faster recovery.17 Off-pump coronary artery bypass surgery may overcome the unwanted effects of the use of cardiopulmonary bypass which induces whole body inflammation, generates micro-embolism and the need to cross-clamp the atheromatous aorta.18 Therefore, if cardiopulmonary bypass can be avoided, a reduced postoperative morbidity and mortality rate may be expected. Several randomised studies19-22 have indeed shown that offpump bypass surgery is equally safe with similar complete revascularisation rates as standard bypass surgery with a reduced enzyme release,23,24 a reduced length of stay,21 improved short-term cognitive recovery22 and reduced major adverse cardiac events (MACE) rate.25 This in turn results in lower costs.26
Favourable results of off-pump CABG may particularly become apparent in high-risk patients: advanced age, diabetics, acute myocardial infarction and patients with an atheromatous aorta. Patients may achieve excellent results after either type of coronary bypass surgery. Individual outcomes likely depend on other factors as well, such as the skill of the surgeon, the quality of the institution and the availability of quality programmes such as critical pathways. These elements also apply to our series: a delicate cooperation between two hospitals, using dedicated surgeons and a critical pathway led by a nurse practitioner,27 led to a successful arterial revascularisation programme with excellent short-term and mid-term outcomes.
Limitations
We aimed to describe the safety and feasibility of this technique in a collaboration between two teaching hospitals. It is a relatively small population, with exclusion of emergency surgery. It is, however, a representative sample of our outpatient clinic population, including diabetics.
We describe a short period of follow-up with relatively good results with respect to death and reoccurrence of myocardial infarction. It would be of interest to follow this population for a longer period of time and compare them with conventional CABG. We have made no attempt to studygraft patency, which is an extremely important component ofthe safety and efficacy of coronary artery bypass for any patient population. Puskas et al.28 showed early graft patency rates equal to literature data for on-pump procedures. If a difference in long-term patency rates between on- and off-pump existed, it should be evident in early and midterm results.
Conclusion
All-arterial bypass grafting using both internal mammary arteries with the technique as described by Tector is safe and feasible without excess deep sternal wound infections. Late major adverse cardiac events are rare and due to distal graft dysfunction, which can be treated by percutaneous coronary intervention.
References
- 1.Virani SS, Alam M, Mendoza CE, Arora H, Ferreira AC, de Marchena E. Clinical significance, angiographic characteristics, and short-term outcomes in 30 patients with early coronary artery graft failure. Neth Heart J. 2009;17:13–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Eagle KA, Guyton RA, Davidoff R, Ewy GA, Fonger J, Gardner TJ, et al. ACC/AHA guidelines for coronary artery bypass graft surgery: executive summary and recommendations : A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to revise the 1991 guidelines for coronary artery bypass graft surgery). Circulation. 1999;100:1464–80. [DOI] [PubMed] [Google Scholar]
- 3.The Synergy Between Percutaneous Coronary Intervention With TAXUS and Cardiac Surgery: The SYNTAX Study. Presented by Dr. Patrick Serruys at the European Society of Cardiology Congress, Munich, Germany, August/September 2008. [Google Scholar]
- 4.Serruys PW, Unger F, Sousa JE, Jatene A, Bonnier HJ, Schonberger JP, et al. Comparison of coronary-artery bypass surgery and stenting for the treatment of multivessel disease. N Engl J Med. 2001;344:1117–24. [DOI] [PubMed] [Google Scholar]
- 5.FitzGibbon GM, Kafka HP, Leach AJ, Keon WJ, Hooper GD, Burton JR. Coronary bypass graft fate and patient outcome: angiographic follow-up of 5,065 grafts related to survival and reoperation in 1,388 patients during 25 years. J Am Coll Cardiol. 1996;26:616–26. [DOI] [PubMed] [Google Scholar]
- 6.Cameron A, Davis KB, Green GE, Myers WO, Pettinger M. Clinical implications of internal mammary artery bypass grafts: the Coronary Artery Surgery Study experience. Circulation. 1988;77:815–9. [DOI] [PubMed] [Google Scholar]
- 7.Tector AJ, McDonald ML, Kress DC, Downey FX, Schmahl TM. Purely internal thoracic artery grafts: outcomes. Ann Thorac Surg. 2001;72:450–5. [DOI] [PubMed] [Google Scholar]
- 8.Roques F, Nashef SA, Michel P, Gauducheau E, de Vincentiis C, Baudet E, et al. Risk factors and outcome in European cardiac surgery: analysis of the EuroSCORE multinational database of 19030 patients. Eur J Cardiothorac Surg. 1999;15:816–22. [DOI] [PubMed] [Google Scholar]
- 9.Roques F, Michel P, Goldstone AR, Nashef SA. The logistic EuroSCORE. Eur Heart J. 2003;24:881–2. [DOI] [PubMed] [Google Scholar]
- 10.Verma S, Szmitko PE, Weisel RD, Bonneau D, Latter D, Errett L, et al. Should radial arteries be used routinely for coronary artery bypass grafting? Circulation. 2004;110:e40–e46. [DOI] [PubMed] [Google Scholar]
- 11.Esaki J, Koshiji T, Okamoto M, Tsukashita M, Ikuno T, Sakata R. Gastroepiploic artery grafting does not improve the late outcome in patients with bilateral internal thoracic artery grafting. Ann Thorac Surg. 2007;83:1024–9. [DOI] [PubMed] [Google Scholar]
- 12.Cameron A, Davis KB, Green G, Schaff HV. Coronary bypass surgery with internal-thoracic-artery grafts—effects on survival over a 15-year period. N Engl J Med. 1996;334:216–9. [DOI] [PubMed] [Google Scholar]
- 13.Fiore AC, Naunheim KS, Dean P, Kaiser GC, Pennington G, Willman VL, et al. Results of internal thoracic artery grafting over 15 years: single versus double grafts. Ann Thorac Surg. 1990;49:202–8. [DOI] [PubMed] [Google Scholar]
- 14.Buxton BF, Komeda M, Fuller JA, Gordon I. Bilateral internal thoracic artery grafting may improve outcome of coronary artery surgery. Risk-adjusted survival. Circulation. 1998;96:II1–II6. [PubMed] [Google Scholar]
- 15.Lytle BW, Blackstone EH, Loop FD, Houghtaling PL, Arnold JH, Akhrass R, et al. Two internal thoracic artery grafts are better than one. J Thorac Cardiovasc Surg. 1999;117:855–72. [DOI] [PubMed] [Google Scholar]
- 16.Tarrio RF, Cuenca JJ, Gomes V, Campos V, Herrera JM, Rodriguez F, et al. Off-pump total arterial revascularization: our experience. J Card Surg. 2004;19:389–95. [DOI] [PubMed] [Google Scholar]
- 17.Puskas JD, Edwards FH, Pappas PA, O'Brien S, Peterson ED, Kilgo P, et al. Off-pump techniques benefit men and women and narrow the disparity in mortality after coronary bypass grafting. Ann Thorac Surg. 2007;84:1447–54. [DOI] [PubMed] [Google Scholar]
- 18.Sellke FW, DiMaio JM, Caplan LR, Ferguson TB, Gardner TJ, Hiratzka LF, et al. Comparing on-pump and off-pump coronary artery bypass grafting: numerous studies but few conclusions: a scientific statement from the American Heart Association council on cardiovascular surgery and anesthesia in collaboration with the interdisciplinary working group on quality of care and outcomes research. Circulation. 2005;111:2858–64. [DOI] [PubMed] [Google Scholar]
- 19.Gerola LR, Buffolo E, Jasbik W, Botelho B, Bosco J, Brasil LA, et al. Off-pump versus on-pump myocardial revascularization in lowrisk patients with one or two vessel disease: perioperative results in a multicenter randomized controlled trial. Ann Thorac Surg. 2004;77:569–73. [DOI] [PubMed] [Google Scholar]
- 20.Straka Z, Widimsky P, Jirasek K, Stros P, Votava J, Vanek T, et al. Off-pump versus on-pump coronary surgery: final results from a prospective randomized study PRAGUE-4. Ann Thorac Surg. 2004;77:789–93. [DOI] [PubMed] [Google Scholar]
- 21.Nathoe HM, van Dijk D, Jansen EW, Suyker WJ, Diephuis JC, van Boven WJ. et al. A comparison of on-pump and off-pump coronary bypass surgery in low-risk patients. N Engl J Med. 2003;346:394–402. [DOI] [PubMed] [Google Scholar]
- 22.van Dijk D, Jansen EW, Hijman R, Nierich AP, Diephuis JC, Moons KG, et al. Cognitive outcome after off-pump and on-pump coronary artery bypass graft surgery: a randomized trial. JAMA. 2002;287:1405–12. [DOI] [PubMed] [Google Scholar]
- 23.Wildhirt SM, Schulze C, Conrad N, Sreejayan N, Reichenspurner H, von Ritter C, et al. Reduced myocardial cellular damage and lipid peroxidation in off-pump versus conventional coronary artery bypass grafting Eur J Med Res. 2000;5:222–8. [PubMed] [Google Scholar]
- 24.Thielmann M, Massoudy P, Marggraf G, Assenmacher E, Kienbaum P, Piotrowski J, et al. Impact of intraoperative myocardial cellular damage on early hemodynamics after off-pump versus on-pump coronary artery bypass surgery. Eur J Med Res. 2005;10:218–26. [PubMed] [Google Scholar]
- 25.Magee MJ, Alexander JH, Hafley G, Ferguson TB Jr, Gibson CM, Harrington RA, et al. Coronary artery bypass graft failure after on-pump and off-pump coronary artery bypass: findings from PREVENT IV. Ann Thorac Surg. 2008;85:494–9. [DOI] [PubMed] [Google Scholar]
- 26.Puskas JD, Williams WH, Mahoney EM, Huber PR, Block PC, Duke PG, et al. Off-pump vs conventional coronary artery bypass grafting: early and 1-year graft patency, cost, and quality-of-life outcomes: a randomized trial. JAMA. 2004;291:1841–9. [DOI] [PubMed] [Google Scholar]
- 27.Broers C, Hogeling-Koopman J, Burgersdijk C, Cornel JH, van der Ploeg T, Umans VA. Safety and efficacy of a nurse-led clinic for post-operative coronary artery bypass grafting patients. Int J Cardiol. 2006;106:111–5. [DOI] [PubMed] [Google Scholar]
- 28.Puskas JD, Wright CE, Ronson RS, Brown WM, III, Gott JP, Guyton RA. Clinical outcomes and angiographic patency in 125 consecutive off-pump coronary bypass patients. Heart Surg Forum. 1999;2:216–21. [PubMed] [Google Scholar]