Abstract
Objective
To compare the marginal benefit of in-home asthma self-management support provided by community health workers (CHWs) with standard asthma education from clinic-based nurses.
Design
Randomized controlled trial.
Setting
Community and public health clinics and homes.
Participants
Three hundred nine children aged 3 to 13 years with asthma living in low-income households.
Interventions
All participants received nurse-provided asthma education and referrals to community resources. Some participants also received CHW-provided home environmental assessments, asthma education, social support, and asthma-control resources.
Outcome Measures
Asthma symptom–free days, Pediatric Asthma Caretaker Quality of Life Scale score, and use of urgent health services.
Results
Both groups showed significant increases in caretaker quality of life (nurse-only group: 0.4 points; 95% confidence interval [CI], 0.3–0.6; nurse + CHW group: 0.6 points; 95% CI, 0.4–0.8) and number of symptom-free days (nurse only: 1.3 days; 95% CI, 0.5–2.1; nurse + CHW: 1.9 days; 95% CI, 1.1–2.8), and absolute decreases in the proportion of children who used urgent health services in the prior 3 months (nurse only: 17.6%; 95% CI, 8.1%–27.2%; nurse + CHW: 23.1%; 95% CI, 13.6%–32.6%). Quality of life improved by 0.22 more points in the nurse + CHW group (95% CI, 0.00–0.44; P=.049). The number of symptom-free days increased by 0.94 days per 2 weeks (95% CI, 0.02–1.86; P = .046), or 24.4 days per year, in the nurse + CHW group. While use of urgent health services decreased more in the nurse + CHW group, the difference between groups was not significant.
Conclusion
The addition of CHW home visits to clinic-based asthma education yielded a clinically important increase in symptom-free days and a modest improvement in caretaker quality of life.
Asthma is the most common chronic childhood disease, affecting nearly 9% of American children.1 Concern about pediatric asthma has led to the development of effective self-management education programs.2–19 Typically, self-management skills are taught in classes or during individual counseling sessions with clinic staff. However, replication of these self-management programs in real-world settings has been fraught with difficulties.20 Attendance is low and drop-out rates are high.20–24
Home visits are an alternative means for providing self-management support. Recently, several randomized trials demonstrated that home visits improve asthma control.25–32 Most of these studies focused on reducing exposure to household asthma triggers but did not address the medical aspects of self-management, such as effective use of medications and asthma action plans. Evaluation of comprehensive home-visit programs that include both environmental and medical self-management components is needed.
Community health workers (CHWs) are particularly well suited for making visits to low-income, ethnically diverse households that are most affected by asthma health disparities.33–40 However, evidence for the effectiveness of CHWs’ provision of self-management support is needed.
METHODS
The Seattle–King County Healthy Homes II Project was a randomized, controlled, parallel-group study. We tested the hypothesis that adding in-home visits by CHWs to traditional clinic-based education by nurses would improve self-management practices, reduce asthma-trigger exposure, and decrease asthma morbidity beyond that seen with nurse education alone.
PARTICIPANTS
Household eligibility criteria were the presence of a child aged 3 to 13 years with clinician-diagnosed asthma that was persistent or poorly controlled; income below 200% of the 2001 federal poverty threshold or the child enrolled in Medicaid; caretaker primary language of English, Spanish, or Vietnamese; and location in King County, Washington. Asthma was considered persistent or poorly controlled if the caretaker reported that his or her child had symptoms or used β-agonist medications more than twice per week; the child was using daily controller medication; or the child had a hospitalization, emergency department visit, or unscheduled clinic visit for asthma in the past 6 months.
Exclusion criteria were plans to move within the next 12 months, no permanent housing, or participation in another asthma research study. Enrollment occurred between November 2002 and October 2004.
We recruited participants from community and public health clinics (94%), hospitals and emergency departments (5%), and community referrals (1%). Caregivers received grocery gift card incentives ($75) for completing data collection. The Children’s Hospital and Regional Medical Center institutional review board approved the study. We followed community-based participatory research principles.41,42 A steering committee of community residents with asthma and community-based organizations identified the study question, approved the study design, gave advice on implementation, and commented on the findings.
INTERVENTION
We randomly assigned participants to receive asthma education and support only in clinics from nurses (nurse-only group) or in both clinics from nurses and in participants’ homes from CHWs (nurse + CHW group). We used social cognitive theory43–45 and the transtheoretical stages of the change model46–48 to guide development of the intervention.
RANDOMIZATION
We randomly assigned participants to groups using a permuted block design with varying block size. We stratified randomization into 2 asthma-severity levels (mild and moderate/severe persistent). Sequence numbers and group allocation were concealed in sealed, opaque, numbered envelopes that were centrally prepared and sequentially provided to the research nurse, who assigned participants to study groups. The nature of the intervention made it impossible to mask participants and staff to group assignment.
CHW Home Visits
The CHWs shared ethnic backgrounds with participants and had personal or family experience with asthma. Their clients received 1 intake and an average of 4.5 follow-up visits during the course of a year as well as interim telephone communication. At the intake visit, CHWs reviewed participants’ asthma control, self-management practices, and access to medical care. Based on this assessment, results from a home environmental checklist (see “Data Collection” section) and allergy testing, and use of motivational interviewing methods,49–51 CHWs developed a set of protocol-driven client and CHW actions.52–59 At follow-up visits, CHWs assessed progress and reviewed a core set of educational topics (medication use, action plans, effective use of the medical system, medical adherence, and trigger reduction).60–63 Community health workers also provided social support64,65 and advocacy for clients (eg, housing issues, insurance coverage).
Community health workers fit allergen-impermeable bedding encasements on the children’s beds66,67 and gave participants a low-emission vacuum with a power head and embedded dirt finder,68–70 2-layer microfiltration vacuum bags,71 a high-quality doormat, a cleaning kit, and plastic medication boxes.
Clinic Visits With Asthma Nurses
The project employed 2 types of nurses, existing clinic nurses (25% of participants) and a visiting project nurse, all of whom received the same training.13,63,72,73 Nurses conducted a structured intake that they used in conjunction with allergy test results to develop a client-specific asthma-management plan. They also prepared an asthma action plan,74 which was reviewed by the patient’s medical provider. Education began at the initial visit and the nurses offered clients 3 follow-up clinic visits at 3-month intervals.
The nurses referred patients to additional resources, such as social workers and school nurses, and assisted clients in accessing their medical providers (ie, in making appointments). If a child failed to keep an appointment, his or her nurse tried to call the child’s home. After completing exit data collection, members of the nurse-only group received a CHW home visit and the full package of environmental resources. All study participants received spacers and allergen-impermeable bedding encasements, and children aged 7 years or older received a peak flow meter.
Care Coordination
Nurses sent visit notes to providers and contacted them directly as needed. The CHW and nurse discussed mutual clients as needed. The CHW sent home-visit reports to providers and communicated directly with them as issues arose.
OUTCOME MEASURES
Primary prespecified outcomes were asthma symptom–free days (self-reported number of 24-hour periods during the prior 2 weeks without wheeze, tightness in chest, cough, shortness of breath, slowing down activities because of asthma, or nighttime awakening because of asthma), Pediatric Asthma Caregiver Quality of Life Scale75 score (range, 1–7, with higher scores indicating better quality of life), and self-reported asthma-related urgent health services use during the last 3 months (emergency department, hospital, or unscheduled clinic visit). Secondary prespecified outcomes included asthma attack frequency (“a time when asthma symptoms were worse, limiting activity more than usual or making you seek medical care”), rescue medication use, days with activity limited by asthma, and missed work and school days due to asthma. Intermediate outcomes included participants’ report of asthma self-management behaviors, controller and rescue medication use, exposure to triggers in the home, asthma self-regulation,76 and social support and self-efficacy specific to asthma. We considered participants adherent to asthma-medication use if, during the past 2 weeks, they (1) took medications every day as recommended by their physicians, (2) did not forget to take medication on any day, (3) did not stop using medication on any day, and (4) did not on any day take less medication than prescribed.77
A child was considered to be exposed to tobacco smoke if his or her caregiver reported that at least 1 cigarette was smoked in the home in the past week. Spacer use was adequate if it was used most or all of the time in the past 14 days. We developed scales to measure social support specific to controlling asthma (Cronbach α=0.87) and self-efficacy in performing asthma-management actions (Cronbach α=0.86) (data available on request from authors). The asthma-control action score (range, −1 to 11) consisted of medical and trigger-reduction components (use of humidifier is given a score of −1, while other items each contribute 1 point). We used a modified version of the national guideline definition of asthma severity.13 We used standard US census categories to collect self-reported race and ethnicity data.
DATA COLLECTION
Baseline data were collected prior to randomization. Community health workers completed standardized home inspections and questionnaires using a home environmental checklist for participants both in the nurse-only and nurse + CHW groups. The checklist included items on exposure to allergens and tobacco smoke and home conditions contributing to exposures (eg, carpeting, food debris and storage, moisture problems). Research nurses at a general clinical research center collected clinical data and performed skin-prick testing for allergies to dust mite mix, regional mold mix, cats, dogs, cockroaches, and rodents.78,79
We attempted to collect exit data exactly 1 year after baseline data collection. Difficulties in scheduling appointments led to delays for some participants. Half had data collected less than 13 months after baseline and 70.5% less than 15 months (range, 247–737 days). Research nurses collected clinical exit data, and a CHW who did not work with the participant collected environmental data.
SAMPLE SIZE
A group size of 153 participants (the number completing the study) had 80% power to detect differences of 1.35 symptom-free days, 0.33 points in the quality of life score, and 19% in urgent health services use between groups, with α set at 0.05. The minimum clinically significant difference in quality of life is 0.5 points.78
STATISTICAL ANALYSIS
We report the results of an as-randomized analysis that used the baseline value of the outcome variable of interest as the exit value for participants who did not complete the study. We examined baseline differences between groups with the t or χ2 tests and paired t, signed-rank, or McNemar tests for within-group baseline-to-exit changes.
To compare the magnitude of baseline-to-exit changes between groups, we used robust linear and logistic regression models.80 Models included the outcome (exit value) as the dependent variable, group assignment as the primary independent variable, the baseline value of the dependent variable, and covariates (seasons of enrollment and exit, asthma severity at baseline, race/ethnicity, and housing tenure). We identified 2 asthma seasons based on observed monthly variation in symptoms and use of urgent health services among study participants (high season, December–January; low season, February–November). We tested for confounding by participant characteristics (child’s age and sex; household income; and caretaker’s employment status, education, and relationship to his or her child) by using a coefficient change of at least 10% in the group assignment variable as indicative of confounding. No confounding was present, so these variables were not included in the models.
We computed the number needed to treat for categorical variables using the reciprocal of the risk difference, and for continuous variables using the method of Guyatt et al.81 We used Stata, version 9.0 (Stata Corp, College Station, Texas), for analyses. P < .05 indicated a statistically significant difference. All analyses were 2-tailed.
RESULTS
PARTICIPATION
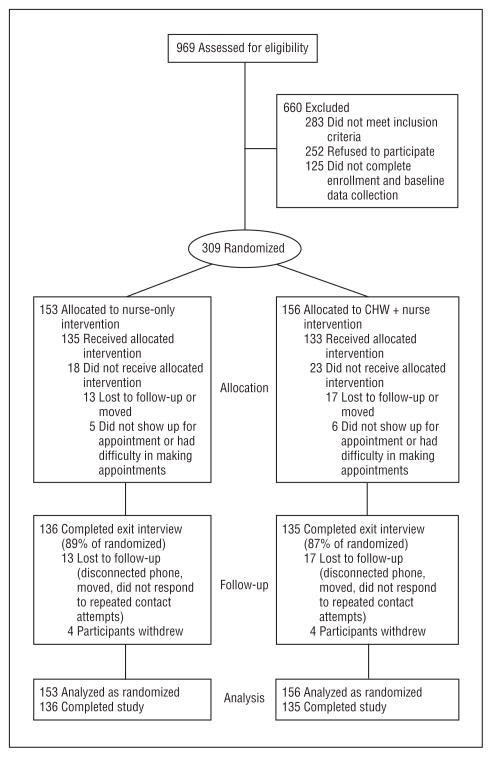
We identified 1474 children who had provider-diagnosed asthma and reached 969 of their caregivers (66%) (Figure). We enrolled 309 eligible and interested households. Random assignment produced study arms that were balanced with respect to most characteristics, though the nurse-only group had more African American children, fewer Asian children, and more families who owned their homes (Table 1). Of those enrolled, 135 in the nurse-only group and 133 in the nurse + CHW group received the intervention as allocated.
Figure.
Participant flowchart. CHW indicates community health worker.
Table 1.
Baseline Characteristics of Study Participants
| % |
|||||||
|---|---|---|---|---|---|---|---|
| Enrolled in Study |
Completed Study |
||||||
| Characteristic | Nurse-Only Group | Nurse + CHW Group | Total | Nurse-Only Group | Nurse + CHW Group | Total | Dropped Out |
| Completed phase, No. (%) | 153 | 156 | 309 | 136 (89) | 135 (87) | 271 | 38 |
| Demographic Characteristics | |||||||
| Child | |||||||
| Age, mean, y | 8.0 | 8.0 | 8.0 | 7.9 | 7.9 | 7.9 | 8.5 |
| Male sex | 62.8 | 64.7 | 63.8 | 62.5 | 64.4 | 63.5 | 65.8 |
| Caregiver | |||||||
| Ethnicitya,b | |||||||
| White | 13.7 | 9.0 | 11.3 | 13.2 | 7.4 | 10.3 | 18.4 |
| African Americana,b | 26.1 | 14.1 | 20.1 | 26.5 | 14.1 | 20.3 | 18.4 |
| Vietnamese | 8.5 | 13.5 | 11.0 | 7.4 | 14.1 | 10.7 | 13.2 |
| Other Asiana,b | 1.3 | 10.3 | 5.8 | 1.5 | 9.6 | 5.5 | 7.9 |
| Hispanic | 46.4 | 49.4 | 47.9 | 47.8 | 51.9 | 49.8 | 34.2 |
| Other | 3.9 | 3.9 | 3.9 | 3.7 | 3.0 | 3.3 | 7.9 |
| Preferred language | |||||||
| English | 52.3 | 45.5 | 48.9 | 51.5 | 43.0 | 47.2 | 60.5 |
| Spanish | 39.9 | 41.7 | 40.8 | 41.9 | 43.0 | 42.4 | 29.0 |
| Vietnamese | 7.8 | 12.8 | 10.4 | 6.6 | 14.1 | 10.3 | 10.5 |
| Household income | |||||||
| <100% of 2001 federal poverty level | 54.6 | 46.5 | 50.5 | 55.6 | 45.5 | 50.6 | 50.0 |
| 100%–200% of 2001 federal poverty level | 45.4 | 53.5 | 49.5 | 44.4 | 54.5 | 49.4 | 50.0 |
| Education | |||||||
| <High school | 43.4 | 42.6 | 43.0 | 45.2 | 44.0 | 44.6 | 31.6 |
| High school or GED diploma | 31.6 | 25.8 | 28.7 | 31.9 | 24.6 | 28.3 | 31.6 |
| Some college | 20.4 | 27.1 | 23.8 | 19.3 | 27.6 | 23.4 | 26.3 |
| College graduate | 4.6 | 4.5 | 4.6 | 3.7 | 3.7 | 3.7 | 10.5 |
| Currently employed | 45.8 | 48.7 | 47.2 | 45.6 | 48.1 | 46.8 | 50.0 |
| Age, y | |||||||
| <45 | 87.5 | 92.3 | 89.9 | 86.0 | 91.8 | 88.9 | 97.3 |
| >45 | 12.5 | 7.7 | 10.1 | 14.0 | 8.2 | 11.1 | 2.7 |
| Rented home, including public housinga,b | 68.6 | 84.6 | 76.7 | 70.6 | 84.4 | 77.5 | 71.1 |
| Asthma Characteristics | |||||||
| Asthma severity | |||||||
| Mild, intermittent | 22.9 | 17.3 | 20.1 | 22.1 | 16.3 | 19.2 | 26.3 |
| Mild, persistent | 42.5 | 39.7 | 41.1 | 44.1 | 40.7 | 42.4 | 31.6 |
| Moderate, persistent | 27.5 | 32.1 | 29.8 | 27.2 | 31.1 | 29.2 | 34.2 |
| Severe, persistent | 7.2 | 10.9 | 9.1 | 6.6 | 11.9 | 9.2 | 7.9 |
| Used urgent health services in last 3 mo | 49.0 | 47.4 | 48.2 | 47.1 | 49.6 | 48.3 | 47.4 |
| Caregiver quality of life score, mean | 5.6 | 5.6 | 5.6 | 5.6 | 5.6 | 5.6 | 5.6 |
| No. of symptom-free days/2 wk, mean | 9.5 | 9.3 | 9.4 | 9.4 | 9.1 | 9.2 | 10.5 |
| No. of days/2 wk with activity limited by asthma, mean | 1.9 | 1.8 | 1.9 | 2.0 | 1.9 | 2.0 | 1.1 |
| No. of asthma attacks within last 3 mo, mean | 2.1 | 2.6 | 2.4 | 2.0 | 2.8 | 2.4 | 1.9 |
| No. of days/2 wk used β2-agonist, mean | 3.2 | 3.7 | 3.5 | 3.1 | 3.9 | 3.5 | 3.2 |
| No. of days/2 wk used controller medications, mean | 4.6 | 5.2 | 4.9 | 4.6 | 5.2 | 4.9 | 4.9 |
| Child missed school within 2-wk period | 25.2 | 22.8 | 24.0 | 22.7 | 25.0 | 23.8 | 25.0 |
| Adult missed work within 2-wk period | 13.6 | 10.9 | 12.2 | 12.7 | 12.7 | 12.7 | 8.8 |
| Positive skin test for ≥1 allergen | 56.2 | 64.7 | 60.5 | 55.2 | 65.9 | 60.5 | 60.5 |
| Smoker in home | 45.1 | 38.5 | 41.8 | 47.1 | 37.8 | 42.4 | 36.8 |
| Pet in home | 23.5 | 23.1 | 23.3 | 21.3 | 22.2 | 21.8 | 34.2 |
| Mold | 41.2 | 47.4 | 44.3 | 42.7 | 45.2 | 43.9 | 47.4 |
| Water damage/moisture/leak | 27.5 | 31.4 | 29.5 | 28.7 | 31.9 | 30.3 | 23.7 |
| Roaches, observed or reported | 12.4 | 16.0 | 14.2 | 14.0 | 17.0 | 15.5 | 5.3 |
| Rodents, observed or reported | 10.5 | 8.3 | 9.4 | 11.0 | 8.9 | 10.0 | 5.3 |
| No. of triggers in the home, mean | 1.5 | 1.5 | 1.5 | 1.5 | 1.5 | 1.5 | 1.4 |
Abbreviations: CHW, community health worker; GED, general education development.
Significant difference (P<.05) between nurse + CHW and nurse-only groups among all enrolled.
Significant difference (P<.05) between nurse + CHW and nurse-only groups among participants who completed the study.
The study was completed by 271 of the participants (88%): 136 in the nurse-only group (89%) and 135 in the nurse + CHW group (87%), including 3 children who were randomly assigned but did not receive the intervention. Among participants completing the study, members of the 2 groups were similar at baseline except for the aforementioned differences in race and housing tenure.
PRIMARY OUTCOMES
Within-Group Changes
Caretaker quality of life increased in both groups (Table 2) (nurse-only group: 0.4 points; 95% confidence interval [CI], 0.3–0.6; nurse + CHW group: 0.6 points; 95% CI, 0.4–0.8). The number of symptom-free days in the past 2 weeks increased (nurse-only group: 1.3 days; 95% CI, 0.5–2.1; nurse + CHW group: 1.9 days; 95% CI, 1.1–2.8), while the proportion of participants who used urgent health services in the prior 3 months decreased (nurse-only group: 17.6% absolute decrease; 95% CI, 8.1%–27.2%; nurse + CHW group: 23.1%; 95% CI, 13.6%–32.6%).
Table 2.
Within-Group and Between-Group Intervention Effects on Outcomes
| Nurse-Only Group (n=153) |
Nurse + CHW Group (n= 156) |
Intervention Effect |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic | Baseline | Exit | Change (95% CI) | P Value | Baseline | Exit | Change (95% CI) | P Value | Coefficient/ORa (95% CI) | P Valueb |
| Primary Outcomes | ||||||||||
| Symptom-free days/2 wk, mean | 9.5 | 10.8 | 1.3 (0.5 to 2.1) | .003 | 9.3 | 11.3 | 1.9 (1.1 to 2.8) | <.001 | 0.94 (0.02 to 1.86) | .046 |
| Caregiver quality of life score, mean | 5.6 | 6.0 | 0.4 (0.3 to 0.6) | <.001 | 5.6 | 6.2 | 0.6 (0.4 to 0.8) | <.001 | 0.22 (0.00 to 0.44) | .049 |
| Used urgent health services within last 3 mo, % | 49.0 | 31.4 | −17.6 (−27.2 to −0.08) | <.001 | 47.4 | 24.4 | −23.1 (−32.6 to −13.6) | <.001 | 0.69 (0.38 to 1.26) | .23 |
| Secondary Outcomes | ||||||||||
| No. of days/2 wk with activity limitation, mean | 1.9 | 1.1 | −0.8 (−1.4 to −0.2) | .01 | 1.8 | 0.9 | −0.9 (−1.5 to −0.4) | .002 | −0.22 (−0.79 to 0.36) | .46 |
| No. of days/2 wk used β2-agonist, mean | 3.2 | 2.6 | −0.5 (−1.2 to 0.1) | .08 | 3.7 | 2.1 | −1.6 (−2.4 to −0.7) | <.001 | −0.59 (−1.45 to 0.26) | .18 |
| No. of asthma attacks within last 3 mo, mean | 2.1 | 1.2 | −0.8 (−1.8 to 0.1) | .07 | 2.6 | 0.8 | −1.8 (−2.7 to −0.9) | <.001 | −0.50 (−1.04 to 0.04) | .07 |
| Child missed school ≥1 times/2 wk, % | 18.3 | 11.8 | −6.5 (−13.4 to 0.00) | .04 | 16.7 | 9.0 | −7.7 (−15.1 to −.00) | .03 | 0.81 (0.35 to 1.88) | .62 |
| Adult missed work ≥1 times/2 wk, % | 12.4 | 6.5 | −5.9 (−11.7 to 0.00) | .03 | 9.6 | 3.8 | −5.8 (−11.8 to 0.00) | .04 | 0.60 (0.20 to 1.78) | .35 |
Abbreviations: CHW, community health worker; CI, confidence interval; OR, odds ratio.
The coefficient of the group assignment term is reported for continuous variables and the logistic OR (nurse + CHW vs nurse-only groups) is reported for categorical variables.
Difference between groups adjusted for baseline differences in asthma severity, race/ethnicity, housing tenure, and season.
Intervention Effects
After adjustment, caretaker quality of life improved more in the nurse + CHW group than in the nurse-only group (0.22 points; 95% CI, 0.00–0.44; P=.049), though the difference did not exceed the clinical threshold of 0.5 points (Table 2).82 The number of symptom-free days increased by 0.94 more days per 2 weeks (95% CI, 0.02–1.86; P=.046), or 24.4 more days per year, in the nurse + CHW group. The number needed to treat to increase symptom-free days by 1 day per 2 weeks was 15. The odds ratio comparing use of urgent health services in the nurse + CHW group with the nurse-only group was 0.69 (95% CI, 0.38–1.26; P=.23). The findings were similar when we restricted analysis to only participants who completed the study (data not shown).
The addition of CHW visits was equally effective among prespecified subgroups of participants. In separate regression models for each of the 3 primary outcomes, we did not observe any significant interactions between group allocation and the child’s age, baseline asthma severity, baseline symptom-free days, or caretaker’s race/ethnicity and education.
SECONDARY OUTCOMES
All secondary outcomes improved significantly in the nurse + CHW group, while only days with activity limitation and missed days of school or work did so in the nurse-only group (Table 2). There were no significant differences between groups.
BEHAVIOR CHANGES
A composite measure of behavior changes (asthma-control action score) improved significantly in both groups (Table 3). Participants in the nurse + CHW group adopted an average of 2.0 new behaviors compared with 1.3 in the nurse-only group, a significant difference. The difference was attributable to increased trigger-control actions rather than medical self-management actions. Social support, self-regulation, and self-efficacy improved equally in both groups, and there were no significant across-group differences.
Table 3.
Within-Group and Between-Group Intervention Effects on Intermediary Variables
| Nurse-Only Group (n=153) |
Nurse + CHW Group (n=156) |
Intervention Effect |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic | Baseline | Exit | Change (95% CI) | P Value | Baseline | Exit | Change (95% CI) | P Value | Coefficient/OR (95% CI)a | P Valueb |
| No. of days controller used in past 2 wk, mean | 4.6 | 5.8 | 1.1 (0.2 to 2.0) | .01 | 5.2 | 6.4 | 1.2 (0.2 to 2.2) | .02 | −0.03 (−1.3 to 1.3) | .97 |
| Used controller daily, % | 24.8 | 37.3 | 12.4 (4.7 to 20.2) | .001 | 30.1 | 39.7 | 9.6 (1.1 to 18.2) | .02 | 2.8 (1.1 to 7.1) | .03 |
| Asthma-control action score, mean | 5.6 | 6.8 | 1.3 (0.9 to 1.6) | <.001 | 5.6 | 7.6 | 2.0 (1.6 to 2.3) | <.001 | 0.55 (0.14 to 0.96) | .009 |
| Medical self-management score, mean | 1.6 | 2.1 | 0.5 (0.3 to 0.7) | <.001 | 1.6 | 2.3 | 0.7 (0.5 to 0.9) | <.001 | 0.11 (−0.15 to 0.38) | .40 |
| Medication adherence, % | 39.2 | 41.9 | 2.7 (−8.0 to 13.5) | .6 | 39.0 | 50.6 | 11.7 (2.4 to 21.0) | .009 | 1.28 (0.75 to 2.17) | .37 |
| Spacer used most/all the time, % | 39.7 | 49.6 | 9.9 (−0.1 to 19.9) | .04 | 42.1 | 56.6 | 14.5 (4.8 to 24.1) | .002 | 1.26 (0.73 to 2.20) | .41 |
| Have an action plan, % | 32.6 | 70.7 | 38.1 (27.7 to 48.5) | <.001 | 33.8 | 68.2 | 34.5 (24.5 to 44.4) | <.001 | .71 (0.40 to 1.24) | .23 |
| Nonurgent health services visit ≥1 times within past 12 mo, % | 58.7 | 53.3 | −5.3 (−15.2 to 4.5) | .26 | 54.3 | 59.6 | 5.3 (−4.7 to 15.3) | .27 | 1.31 (0.77 to 2.22) | .32 |
| Environmental trigger reduction, mean | 3.9 | 4.7 | 0.78 (0.58 to 0.98) | <.001 | 4.0 | 5.3 | 1.27 (1.05 to 1.48) | <.001 | 0.43 (0.16 to 0.69) | .002 |
| Vacuums child’s bedroom ≥2 times per 14 d, % | 64.1 | 66.0 | 2.0 (−7.1 to 11.0) | .65 | 62.6 | 85.2 | 22.6 (13.8 to 31.3) | <.001 | 3.00 (1.56 to 5.77) | .001 |
| Washes sheets weekly in hot water, % | 36.4 | 43.7 | 7.3 (−2.0 to 16.6) | .10 | 37.7 | 53.2 | 15.6 (6.5 to 24.7) | .001 | 1.40 (0.84 to 2.34) | .20 |
| Doormat at every outside door, % | 56.3 | 64.2 | 7.9 (0.1 to 15.8) | .03 | 64.5 | 75.5 | 11.0 (1.6 to 20.3) | .02 | 1.78 (0.97 to 32.5) | .06 |
| No pet, % | 76.5 | 70.6 | −5.9 (−13.6 to 1.8) | .11 | 76.9 | 75.6 | −1.3 (−6.9 to 4.4) | .62 | 1.18 (0.58 to 2.40) | .65 |
| Has a mattress cover, % | 7.3 | 63.6 | 56.3 (47.1 to 65.5) | <.001 | 7.9 | 67.8 | 59.9 (50.8 to 68.9) | <.001 | 1.06 (0.63 to 1.79) | .83 |
| No cigarettes smoked inside within past week, % | 80.4 | 83.7 | 3.3 (−3.2 to 9.8) | .28 | 85.3 | 92.3 | 7.1 (1.3 to 12.8) | .008 | 1.73 (0.72 to 4.19) | .22 |
| Uses kitchen and/or bathroom fan, % | 84.8 | 90.1 | 5.3 (−1.1 to 11.7) | .07 | 86.9 | 90.2 | 3.3 (−2.3 to 8.9) | .2 | 0.76 (0.32 to 1.78) | .53 |
| Uses a humidifier, % | 10.6 | 10.6 | 0 | >.99 | 18.7 | 9.0 | −9.7 (−16.7 to −2.6) | .004 | 0.57 (0.23 to 1.39) | .21 |
| Asthma self-regulation score, meanc | 21.0 | 22.8 | 1.9 (1.3 to 2.5) | <.001 | 21.1 | 22.8 | 1.6 (1.1 to 2.2) | <.001 | −0.37 (−1.1 to 0.3) | .28 |
| Social support score, meand | 27.3 | 30.7 | 3.4 (1.3 to 5.4) | .001 | 27.6 | 31.2 | 3.7 (1.8 to 5.5) | <.001 | 0.48 (−2.0 to 3.0) | .71 |
| Self-efficacy score, meane | 24.1 | 28.4 | 4.3 (3.4 to 5.2) | <.001 | 24.9 | 29.1 | 4.2 (3.3 to 5.0) | <.001 | 0.39 (−0.61 to 1.40) | .44 |
Abbreviations: CHW, community health worker; CI, confidence interval; OR, odds ratio.
The coefficient of the group assignment term is reported for continuous variables and the logistic OR (nurse + CHW vs nurse-only groups) is reported for categorical variables.
Difference across groups adjusted for baseline differences, season, and within-group correlation.
Range, 9–27 points.
Range, 10–50 points.
Range, 11–33 points.
PROCESS MEASURES
Of the 156 participants in the nurse + CHW group, all received an initial CHW intake visit and 153 received at least 1 CHW follow-up visit. Community health workers made a mean of 3.1 follow-up visits to each participant (median, 3.0; range, 0–5). The mean and median intervals between first and last intervention visits were 52.6 weeks and 51.9 weeks, respectively.
Nurses completed an initial intervention visit with 269 participants (87%) and a mean of 1.0 additional follow-up visits. The number of follow-up visits ranged from 0 to 5. All participants were included in the analysis as assigned, whether or not they completed intervention visits.
COMMENT
The goal of this study was to determine if the addition of in-home asthma self-management support from CHWs would yield additional benefits in asthma control beyond those produced by in-clinic support from asthma nurses. Adding in-home visits resulted in clinically important increases in symptom-free days. While the number of symptom-free days increased in both groups, CHW visits yielded 24 additional symptom-free days per year. Home visits yielded modest increases in caretaker quality of life in both groups, but the increase was clinically significant only in the nurse + CHW group. The addition of CHW visits produced a small, significant improvement. Use of urgent health services decreased in both groups; the addition of CHW visits did not further reduce use. The gains from home visits were equivalent across caregivers of all race/ethnic groups and educational attainments and in children of all ages and degrees of asthma severity and control.
Analysis of intermediate measures suggests that the improved outcomes in the nurse + CHW group may have come from increased caretaker efforts to control asthma. The asthma-control action score increased to a greater extent in the nurse + CHW group, driven primarily by trigger-reduction actions. The CHWs supported participant trigger-control actions by both coaching and providing resources, such as vacuums and bedding covers. Use of controller medications increased equally in both groups. Of note, in our first Healthy Homes study, which focused only on reduction of environmental triggers, use of controller medications did not increase.25 Our data are consistent with the hypothesis that improved trigger control is a key pathway through which home interventions improve outcomes. Most effective home-visit programs described in the literature have focused on indoor trigger-reduction activities.25–27,83
Our study is similar to previously reported home-visit studies in its enrollment of minorities and participants with low income; inclusion of indoor environmental trigger reduction; provision of resources to reduce exposures; magnitude of improvements in quality of life25,27,31 and symptom-free days (about 0.8 days per 2 weeks)25,26; and decreases in urgent health services use. This study (and 2 other studies26,32) differs from others in that home visits were made by CHWs; other studies have used professional home visitors. The average number of visits of this study was on the low end of the range (range, 3–9). Understanding the relationship between visit frequency and outcomes merits further study.
It should be quite feasible for organizations that serve similar populations to replicate our program. Using protocols and assessment tools adapted from this project, we have continued to provide CHW services in subsequent service-delivery projects to more than 600 clients.38,84 Local asthma coalitions, health departments, and community health centers have also used our Healthy Homes model to develop CHW programs (replication materials are available at our Web site: http://www.metrokc.gov/health/asthma/healthyhomes/).
Home-visit programs have employed several types of health professionals, such as nurses30 and physicians,29 in addition to CHWs. Using CHWs may be a particularly well-suited strategy to reduce asthma disparities. Community health workers are successful in promoting behavior changes among minorities and clients with low incomes because they come from the same community, share culture and life experiences, and readily establish trusting relationships.34,36,40 More research is needed to clarify the relative benefits of home visits made by different types of visitors.
Providing asthma education in the home offers several advantages over clinic-based approaches, particularly in populations affected by asthma disparities. These populations face significant logistical and psychosocial barriers to attending asthma classes or clinic-based asthma education.33 Home visits may be the only way to reach many of these patients.
Our conclusions are subject to several limitations. We could not mask participants to group assignment given the nature of the intervention. Loss to follow-up could have biased results, but 88% of participants completed the study, with a similar proportion in both groups. Baseline characteristics were similar between groups in those who completed the study.
Our participants were low-income, predominantly minority children with significant asthma. The findings should be generalizable to members of this population who prefer to receive asthma support in their homes. However, 37% of potentially eligible families refused participation and 18% did not complete enrollment, suggesting that in-home visits will not be attractive to all families. Families that did not participate did not differ from those that did with respect to child’s age, asthma-symptom days, use of urgent health services, or degree of neighborhood poverty.
We considered designing the study as a comparison of CHW home visits alone with clinic-based nurse education. While this would have been a useful comparison, our primary goal was to compare the benefit of adding CHW home visits to usual care. Current guidelines13 and evidence1–20 support providing asthma education; therefore, we defined usual care as asthma education in clinical settings. We felt that it would have been unethical not to provide such education to a comparison group.18,19 While lack of such a group raises the concern that the changes in the nurse-only group may have been caused by regression to the mean, temporal trends, or Hawthorne effects,85 the improvements seen in this group are consistent with those observed in other studies.18,19
Resources were not sufficient to permit follow-up of participants after completion of the study to assess the durability of intervention effects. Other studies have shown that benefits from CHW home-visit programs continue after participation in the program.25,26
We did not find a difference between the 2 groups in the use of urgent health services, and the difference in quality of life was small. Our sample size may not have been sufficient to avoid a type II error for urgent use, as the smallest difference we could detect (19%) was greater than the observed difference (5.5%). We may have seen more of an effect if we had included all possible in-home interventions (eg, HEPA [high-efficiency particulate air] filters or professional house-cleaning services), but we did not do so to contain costs and make replication more feasible. Both groups received allergen-proof bedding covers, which may have some benefit in reducing trigger exposure,69,70 thereby decreasing observed differences.
CONCLUSIONS
We conclude that adding in-home asthma self-management support from CHWs to in-clinic education from an asthma nurse improves asthma control in a pediatric, low-income, multiethnic population. Participants who received home visits had more symptom-free days and a small increase in caretaker quality of life relative to those receiving only clinic-based services.
Evidence now supports the effectiveness of multiple methods for providing asthma self-management support, including home visits by CHWs and other health professionals, clinic-based individual education, and group education. Perhaps an optimal strategy is to offer patients options for self-management support, recognizing that many patients may choose not to participate in classes or to go to a clinic for asthma education, while others may not desire a visitor in their homes.
Acknowledgments
Financial Disclosure: None reported.
Funding/Support: This study was primarily funded by grant 1R01-ES11378 from the National Institutes of Environmental Health Sciences (Dr Krieger). Additional support was provided by the Allies Against Asthma Program of the Robert Wood Johnson Foundation; grant U50/CCU011820-02 from the Centers of Disease Control and Prevention Urban Research Centers Cooperative Agreement; and grant MO1-RR-00037 from the National Institutes of Health to the University of Washington General Clinical Research Center.
Role of the Sponsors: None of the funders or donors played a role in study conduct; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript.
Footnotes
Author Contributions: Study concept and design: Krieger, Takaro, Song, and Beaudet. Acquisition of data: Krieger, Takaro, Song, Beaudet, and Edwards. Analysis and interpretation of data: Krieger, Takaro, Song, and Beaudet. Drafting of the manuscript: Krieger and Song. Critical revision of the manuscript for important intellectual content: Krieger, Takaro, Song, Beaudet, and Edwards. Statistical analysis: Krieger and Song. Obtained funding: Krieger. Administrative, technical, and material support: Krieger, Takaro, Song, Beaudet, and Edwards. Study supervision: Krieger and Takaro.
Additional Contributions: Cindy Mai, Margarita Mendoza, and Carol Allen served as CHWs. Karen Brozovich (and Ms Edwards) provided nurse services. Lisa Carol Ross was the project research coordinator. Jeannette Nickens and Scott Jones provided administrative support. University of Washington General Clinical Research Center staff at Children’s Hospital and Medical Center were instrumental in data collection. Kristy Seidel, MS, of the University of Washington General Clinical Research Center, provided statistical consultation.
Hoover (Techtronic Industries Co Ltd, Glenwillow, Ohio) provided low-emission vacuums at a discount. Group Health Cooperative of Puget Sound donated enrollment in their Free & Clear tobacco cessation program. The Seattle City Waste Management Division donated green cleaning kits and pails.
Carol Allen, Gail Johnson, Jeffery Hummel, Penny Nelson, John Roberts, James Stout, and Cor VanNiel served on the project steering committee. David Evans, Thomas Platts-Mills, Gail Shapiro, and James Stout served in the scientific advisory group. Evon Hampton, Celese McDuffie, Kelly (Trinh) Nguyen, Thuy Son Nguyen, Ha Vu Minh Ouh Duong, Brianna Painter, Lauretta Perkins, Debra E. Rosenthal, Ana Salinas, Joann Sampson, Nura Sayed, Mary Tranh, Jennifer Tudor, Kim Tyler, Rosie Williams, and Patricia Gayton served in the parent advisory group.
References
- 1.Akinbami L. The State of Childhood Asthma, United States, 1980–2005: Advance Data From Vital and Health Statistics [No. 381] Hyattsville, MD: National Center for Health Statistics; 2006. [PubMed] [Google Scholar]
- 2.Clark NM, Feldman CH, Evans D, Levision MJ, Mellins RB. The impact of health education on frequency and cost of health care use by low income children with asthma. J Allergy Clin Immunol. 1986;78(1 pt 1):108–115. doi: 10.1016/0091-6749(86)90122-3. [DOI] [PubMed] [Google Scholar]
- 3.Fireman P, Friday GA, Gira C, Vierthaler WA, Michaels L. Teaching self-management skills to asthmatic children and their parents in an ambulatory care setting. Pediatrics. 1981;68(3):341–348. [PubMed] [Google Scholar]
- 4.Lewis CE, Lewis M, De la Sota A, Kaplan M. A randomized trial of A.C.T. for Kids. Pediatrics. 1984;74(4):478–486. [PubMed] [Google Scholar]
- 5.Wilson SR, Latini D, Starr NJ, et al. Education of parents of infants and very young children with asthma: a developmental evaluation of the Wee Wheezers program. J Asthma. 1996;33(4):239–254. doi: 10.3109/02770909609055365. [DOI] [PubMed] [Google Scholar]
- 6.Wolf FM, Guevara JP, Grum CM, Clark NM, Cates CJ. Educational interventions for asthma in children. Cochrane Database Syst Rev. 2003;(1):CD000326. doi: 10.1002/14651858.CD000326. [DOI] [PubMed] [Google Scholar]
- 7.Haby MM, Waters E, Robertson CF, Gibson PG, Ducharme FM. Interventions for educating children who have attended the emergency room for asthma. Cochrane Database Syst Rev. 2001;(1):CD001290. doi: 10.1002/14651858.CD001290. [DOI] [PubMed] [Google Scholar]
- 8.Ronchetti R, Indinnimeo L, Bonci E, et al. Asthma self-management programmes in a population of Italian children: a multicentric study. Italian Study Group on Asthma Self-Management Programmes. Eur Respir J. 1997;10(6):1248–1253. doi: 10.1183/09031936.97.10061248. [DOI] [PubMed] [Google Scholar]
- 9.Lucas DO, Zimmer LO, Paul JE, et al. Two-year results from the asthma self-management program: long-term impact on health care services, costs, functional status, and productivity. J Asthma. 2001;38(4):321–330. doi: 10.1081/jas-100001491. [DOI] [PubMed] [Google Scholar]
- 10.de Oliveira MA, Feresin SM, Bruno VF, de Bittencourt AR, Fernandes AL. Evaluation of an educational programme for socially deprived asthma patients. Eur Respir J. 1999;14(4):908–914. doi: 10.1034/j.1399-3003.1999.14d30.x. [DOI] [PubMed] [Google Scholar]
- 11.Wilson-Pessano SR, McNabb WL. The role of patient education in the management of childhood asthma. Prev Med. 1985;14(6):670–687. doi: 10.1016/0091-7435(85)90066-0. [DOI] [PubMed] [Google Scholar]
- 12.McNabb WL, Wilson-Pessano SR, Hughes GW, Scamagas P. Self-management education of children with asthma: AIR WISE. Am J Public Health. 1985;75 (10):1219–1220. doi: 10.2105/ajph.75.10.1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.National Asthma Education and Prevention Program. Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma No. 07-4051. Bethesda, MD: National Heart, Lung, and Blood Institute; 2007. [Google Scholar]
- 14.Evans R, III, Gergen PJ, Mitchell H, et al. A randomized clinical trial to reduce asthma morbidity among inner-city children: results of the National Cooperative Inner-City Asthma Study. J Pediatr. 1999;135(3):332–338. doi: 10.1016/s0022-3476(99)70130-7. [DOI] [PubMed] [Google Scholar]
- 15.Janson SL, Fahy JV, Covington JK, Paul SM, Gold WM, Boushey HA. Effects of individual self-management education on clinical, biological, and adherence outcomes in asthma. Am J Med. 2003;115(8):620–626. doi: 10.1016/j.amjmed.2003.07.008. [DOI] [PubMed] [Google Scholar]
- 16.Levy ML, Robb M, Allen J, Doherty C, Bland JM, Winter RJ. A randomized controlled evaluation of specialist nurse education following accident and emergency department attendance for acute asthma. Respir Med. 2000;94(9):900–908. doi: 10.1053/rmed.2000.0861. [DOI] [PubMed] [Google Scholar]
- 17.Lahdensuo A, Haahtela T, Herrala J, et al. Randomised comparison of guided self management and traditional treatment of asthma over one year. BMJ. 1996;312(7033):748–752. doi: 10.1136/bmj.312.7033.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Greineder DK, Loane KC, Parks P. A randomized controlled trial of a pediatric asthma outreach program. J Allergy Clin Immunol. 1999;103(3 pt 1):436–440. doi: 10.1016/s0091-6749(99)70468-9. [DOI] [PubMed] [Google Scholar]
- 19.Kelly CS, Morrow AL, Shults J, Nakas N, Strope GL, Adelman RD. Outcomes evaluation of a comprehensive intervention program for asthmatic children enrolled in Medicaid. Pediatrics. 2000;105(5):1029–1035. doi: 10.1542/peds.105.5.1029. [DOI] [PubMed] [Google Scholar]
- 20.Wood P, Tumiel-Berhalter L, Owen S, Taylor K, Kattan M. Implementation of an asthma intervention in the inner city. Ann Allergy Asthma Immunol. 2006;97(1 suppl 1):S20–S24. doi: 10.1016/s1081-1206(10)60781-8. [DOI] [PubMed] [Google Scholar]
- 21.Muntner P, Sudre P, Uldry C, et al. Predictors of participation and attendance in a new asthma patient self-management education program. Chest. 2001;120 (3):778–784. doi: 10.1378/chest.120.3.778. [DOI] [PubMed] [Google Scholar]
- 22.Yoon R, McKenzie DK, Miles DA, Bauman A. Characteristics of attenders and non-attenders at an asthma education programme. Thorax. 1991;46(12):886–890. doi: 10.1136/thx.46.12.886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Abdulwadud O, Abramson M, Forbes A, et al. Attendance at an asthma educational intervention: characteristics of participants and non-participants. Respir Med. 1997;91(9):524–529. doi: 10.1016/s0954-6111(97)90085-8. [DOI] [PubMed] [Google Scholar]
- 24.Lemaigre V, Van den Bergh O, Van Hasselt K, De Peuter S, Victoir A, Verleden G. Understanding participation in an asthma self-management program. Chest. 2005;128(5):3133–3139. doi: 10.1378/chest.128.5.3133. [DOI] [PubMed] [Google Scholar]
- 25.Krieger JW, Takaro TK, Song L, Weaver M. The Seattle-King County Healthy Homes project: a randomized, controlled trial of a community health worker intervention to decrease exposure to indoor asthma triggers. Am J Public Health. 2005;95(4):652–659. doi: 10.2105/AJPH.2004.042994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Morgan WJ, Crain EF, Gruchalla RS, et al. Inner-City Asthma Study Group: results of a home-based environmental intervention among urban children with asthma. N Engl J Med. 2004;351(11):1068–1080. doi: 10.1056/NEJMoa032097. [DOI] [PubMed] [Google Scholar]
- 27.Eggleston PA, Butz A, Rand C, et al. Home environmental intervention in inner-city asthma: a randomized controlled clinical trial. Ann Allergy Asthma Immunol. 2005;95(6):518–524. doi: 10.1016/S1081-1206(10)61012-5. [DOI] [PubMed] [Google Scholar]
- 28.Bonner S, Zimmerman BJ, Evans D, Irigoyen M, Resnick D, Mellins RB. An individualized intervention to improve asthma management among urban Latino and African-American families. J Asthma. 2002;39(2):167–179. doi: 10.1081/jas-120002198. [DOI] [PubMed] [Google Scholar]
- 29.Carter MC, Perzanowski MS, Raymond A, et al. Home intervention in the treatment of asthma among inner-city children. J Allergy Clin Immunol. 2001;108 (5):732–737. doi: 10.1067/mai.2001.119155. [DOI] [PubMed] [Google Scholar]
- 30.Brown JV, Bakeman R, Celano MP, Demi AS, Kobrynski L, Wilson SR. Home-based asthma education of young low-income children and their families. J Pediatr Psychol. 2002;27(8):667–688. doi: 10.1093/jpepsy/27.8.677. [DOI] [PubMed] [Google Scholar]
- 31.Klinnert MD, Liu AH, Pearson MR, et al. Outcome of a randomized multifaceted intervention with low-income families of wheezing infants. Arch Pediatr Adolesc Med. 2007;161(8):783–790. doi: 10.1001/archpedi.161.8.783. [DOI] [PubMed] [Google Scholar]
- 32.Parker EA, Israel BA, Robins TG, et al. Evaluation of community action against asthma: a community health worker intervention to improve children’s asthma-related health by reducing household environmental triggers for asthma. Health Educ Behav. 2008;35(3):376–395. doi: 10.1177/1090198106290622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gold DR, Wright R. Population disparities in asthma. Annu Rev Public Health. 2005;26:89–113. doi: 10.1146/annurev.publhealth.26.021304.144528. [DOI] [PubMed] [Google Scholar]
- 34.Swider SM. Outcome effectiveness of community health workers: an integrative literature review. Public Health Nurs. 2002;19(1):11–20. doi: 10.1046/j.1525-1446.2002.19003.x. [DOI] [PubMed] [Google Scholar]
- 35.Butz AM, Malveaux FJ, Eggleston P, et al. Use of community health workers with inner-city children who have asthma. Clin Pediatr (Phila) 1994;33(3):135–141. doi: 10.1177/000992289403300302. [DOI] [PubMed] [Google Scholar]
- 36.Love MB, Gardner K, Legion V. Community health workers: who they are and what they do. Health Educ Behav. 1997;24(4):510–522. doi: 10.1177/109019819702400409. [DOI] [PubMed] [Google Scholar]
- 37.Krieger JK, Takaro TK, Allen C, et al. The Seattle-King County Healthy Homes Project: implementation of a comprehensive approach to improving indoor environmental quality for low-income children with asthma. Environ Health Perspect. 2002;110(suppl 2):311–322. doi: 10.1289/ehp.02110s2311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Friedman AR, Butterfoss FD, Krieger JW, et al. Allies community health workers: bridging the gap. Health Promot Pract. 2006;7(2 suppl):96S–107S. doi: 10.1177/1524839906287065. [DOI] [PubMed] [Google Scholar]
- 39.Lewin SA, Dick J, Pond P, et al. Lay health workers in primary and community health care. Cochrane Database Syst Rev. 2005;(1):CD004015. doi: 10.1002/14651858.CD004015.pub2. [DOI] [PubMed] [Google Scholar]
- 40.Perez M, Findley SE, Mejia M, Martinez J. The impact of community health worker training and programs in NYC. J Health Care Poor Underserved. 2006;17(1 suppl):26–43. doi: 10.1353/hpu.2006.0011. [DOI] [PubMed] [Google Scholar]
- 41.Israel BA, Eng E, Schulz A, Parker E. Methods in Community-Based Participatory Research for Health. San Francisco, CA: Jossey-Bass; 2005. [Google Scholar]
- 42.Minkler M, Wallerstein N. Community-Based Participatory Research for Health. San Francisco, CA: Jossey-Bass; 2003. [Google Scholar]
- 43.Bandura A. Social Learning Theory. Englewood Cliffs, NJ: Prentice-Hall; 1977. [Google Scholar]
- 44.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice Hall; 1986. [Google Scholar]
- 45.Baranowski T, Perry CL, Parcel GS. How individuals, environments and health behavior interact: social cognitive theory. In: Glanz K, Lewis FM, Rimer BK, editors. Health Behavior and Health Education: Theory, Research, and Practice. 2. San Francisco, CA: Jossey-Bass; 1997. [Google Scholar]
- 46.Prochaska JO, DiClemente CC. Stages of and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol. 1983;51 (3):390–395. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- 47.Prochaska JO, Norcross JC, DiClemente CC. Changing for Good. New York, NY: Morrow; 1994. [Google Scholar]
- 48.Prochaska JO, Redding CO, Evers KE. The transtheoretical model and stages of change. In: Glanz K, Lewis FM, Rimer BK, editors. Health Behavior and Health Education: Theory, Research, and Practice. 2. San Francisco, CA: Jossey-Bass; 1997. [Google Scholar]
- 49.Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. New York, NY: Guilford Press; 2002. [Google Scholar]
- 50.Colby SM, Monti PM, Barnett NP. Brief motivational interviewing in a hospital setting for adolescent smoking: a preliminary study. J Consult Clin Psychol. 1998;66(3):574–578. doi: 10.1037//0022-006x.66.3.574. [DOI] [PubMed] [Google Scholar]
- 51.Harland J, White M, Drinkwater C, Chinn D, Farr L, Howel D. The Newcastle exercise project: a randomized controlled trial of methods to promote physical activity in primary care. BMJ. 1999;319(7213):828–831. doi: 10.1136/bmj.319.7213.828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.National Asthma Education and Prevention Program. Expert Panel Report 2: Guidelines for the Diagnosis and Management of Asthma. Bethesda, MD: National Institutes of Health, National Heart, Lung and Blood Institute; 1997. [NIH publication No. 97-4051] [Google Scholar]
- 53.Etzel RA, Balk SJ. Handbook of Pediatric Environmental Health. Elk Grove Village, IL: American Academy of Pediatrics; 1999. [Google Scholar]
- 54.Institute of Medicine. Clearing the Air: Asthma and Indoor Air Exposures. Washington, DC: National Academy Press; 2000. [PubMed] [Google Scholar]
- 55.Bierman C. Environmental control of asthma. Immunol Allergy Clin North Am. 1996;16(4):753–765. [Google Scholar]
- 56.Ashley P, Menkedick JR, Wooton MA, et al. Healthy Homes Issues: Asthma. Healthy Homes Initiative (HHI) Background Information, Version 3. [Accessed October 27, 2008];US Department of Housing and Urban Development. 2006 http://www.hud.gov/offices/lead/library/hhi/Asthma_Final_Revised_04-26-06.pdf.
- 57.Tovey E, Marks G. Methods and effectiveness of environmental control. J Allergy Clin Immunol. 1999;103(2 pt 1):179–191. doi: 10.1016/s0091-6749(99)70488-4. [DOI] [PubMed] [Google Scholar]
- 58.Platts-Mills TA, Vaughan JW, Carter MC, Woodfolk JA. The role of intervention in established allergy: avoidance of indoor allergens in the treatment of chronic allergic disease. J Allergy Clin Immunol. 2000;106(5):787–804. doi: 10.1067/mai.2000.110548. [DOI] [PubMed] [Google Scholar]
- 59.Eggleston PA. Improving indoor environments: reducing allergen exposures. J Allergy Clin Immunol. 2005;116(1):122–126. doi: 10.1016/j.jaci.2005.04.012. [DOI] [PubMed] [Google Scholar]
- 60.American Academy of Allergy Asthma and Immunology. Pediatric Asthma: Promoting Best Practice. Milwaukee, WI: American Academy of Allergy Asthma and Immunology; 1999. [Google Scholar]
- 61.Roter DL, Hall JA, Merisca R, Nordstrom B, Cretin D, Svarstad B. Effectiveness of interventions to improve patient compliance: a meta-analysis. Med Care. 1998;36(8):1138–1161. doi: 10.1097/00005650-199808000-00004. [DOI] [PubMed] [Google Scholar]
- 62.Clark NM, Nothwehr F, Gong M, et al. Physician-patient partnership in managing chronic illness. Acad Med. 1995;70(11):957–959. doi: 10.1097/00001888-199511000-00008. [DOI] [PubMed] [Google Scholar]
- 63.Meichenbaum D, Turk D. Facilitating Treatment Adherence: A Practitioner’s Guidebook. New York, NY: Plenum Press; 1987. [Google Scholar]
- 64.Heaney CA, Israel BA. Social networks and social support. In: Glanz K, Lewis FM, Rimer BK, editors. Health Behavior and Health Education: Theory, Research, and Practice. 2. San Francisco, CA: Jossey-Bass; 1997. [Google Scholar]
- 65.Berkman LF, Glass T. Social Integration, Social Networks, Social Support, and Health. In: Berkman LF, Kawachi I, editors. Social Epidemiology. New York, NY: Oxford University Press; 2000. pp. 137–173. [Google Scholar]
- 66.Ehnert B, Lau-Schadendorf S, Weber A, Buettner P, Schou C, Wahn U. Reducing domestic exposure to dust mite allergen reduces bronchial hyperreactivity in sensitive children with asthma. J Allergy Clin Immunol. 1992;90(1):135–138. doi: 10.1016/s0091-6749(06)80024-2. [DOI] [PubMed] [Google Scholar]
- 67.Platts-Mills TA. Allergen avoidance in the treatment of asthma and rhinitis. N Engl J Med. 2003;349(3):207–208. doi: 10.1056/NEJMp030082. [DOI] [PubMed] [Google Scholar]
- 68.Popplewell EJ, Innes VA, Lloyd-Hughes S, et al. The effect of high-efficiency and standard vacuum-cleaners on mite, cat and dog allergen levels and clinical progress. Pediatr Allergy Immunol. 2000;11(3):142–148. doi: 10.1034/j.1399-3038.2000.00058.x. [DOI] [PubMed] [Google Scholar]
- 69.Munir AK, Einarsson R, Dreborg SK. Vacuum cleaning decreases the levels of mite allergens in house dust. Pediatr Allergy Immunol. 1993;4(3):136–143. doi: 10.1111/j.1399-3038.1993.tb00082.x. [DOI] [PubMed] [Google Scholar]
- 70.Roberts JW, Clifford WS, Glass G, Hummer PG. Reducing dust, lead, dust mites, bacteria, and fungi in carpets by vacuuming. Arch Environ Contam Toxicol. 1999;36(4):477–484. doi: 10.1007/pl00022756. [DOI] [PubMed] [Google Scholar]
- 71.Vaughan JW, Woodfolk JA, Platts-Mills TA. Assessment of vacuum cleaners and vacuum cleaner bags recommended for allergic subjects. J Allergy Clin Immunol. 1999;104(5):1079–1083. doi: 10.1016/s0091-6749(99)70092-8. [DOI] [PubMed] [Google Scholar]
- 72.National Cooperative Inner City Asthma Study. A Guide for Helping Children with Asthma. Bethesda, MD: National Institute of Allergy and Infectious Diseases; [Google Scholar]
- 73.Wilson SR, Starr-Schneidkraut N. State of the art in asthma education: the US experience. Chest. 1994;106(4 suppl):197S–205S. doi: 10.1378/chest.106.4_supplement.197s. [DOI] [PubMed] [Google Scholar]
- 74.Gibson PG, Powell H. Written action plans for asthma: an evidence-based review of the key components. Thorax. 2004;59(2):94–99. doi: 10.1136/thorax.2003.011858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Juniper EF, Guyatt GH, Feeny DH, Ferrie PJ, Griffith LE, Townsend M. Measuring quality of life in the parents of children with asthma. Qual Life Res. 1996;5(1):27–34. doi: 10.1007/BF00435966. [DOI] [PubMed] [Google Scholar]
- 76.Clark NM, Gong M, Kaciroti N. A model of self-regulation for control of chronic disease. Health Educ Behav. 2001;28(6):769–782. doi: 10.1177/109019810102800608. [DOI] [PubMed] [Google Scholar]
- 77.Brooks CM, Richards JM, Kohler CL, et al. Assessing adherence to asthma medication and inhaler regimens: a psychometric analysis of adult self-report scales. Med Care. 1994;32(3):298–307. doi: 10.1097/00005650-199403000-00008. [DOI] [PubMed] [Google Scholar]
- 78.Nelson H. Clinical application of immediate skin testing. In: Spector SL, editor. Provocative Challenge Procedures. Boca Raton, FL: CRC Press; 1983. p. 148. [Google Scholar]
- 79.Demoly P, Piette V, Bousquet J. In vivo methods for the study of allergy. In: Adkinson N, editor. Middleton’s Allergy: Principles and Practice. 6. New York, NY: Mosby-Year Book Inc; 1998. chap 38. [Google Scholar]
- 80.Ryan TP. Modern Regression Analysis. New York, NY: Wiley Interscience; 1997. [Google Scholar]
- 81.Guyatt GH, Juniper EF, Walter SD, Griffith LE, Goldstein RS. Interpreting treatment effects in randomised trials. BMJ. 1998;316(7132):690–693. doi: 10.1136/bmj.316.7132.690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Juniper EF, Guyatt GH, Willan A, Griffith LE. Determining a minimal important change in a disease-specific quality of life questionnaire. J Clin Epidemiol. 1994;47(1):81–87. doi: 10.1016/0895-4356(94)90036-1. [DOI] [PubMed] [Google Scholar]
- 83.Hoppin P, Jacobs M, Stillman L. Investing in Best Practices for Asthma: A Business Case for Education and Environmental Interventions. Boston, MA: New England Asthma Regional Council; 2007. [Google Scholar]
- 84.Public Health–Seattle & King County. [Accessed January 28, 2008];King County Steps to Health. http://www.kingcounty.gov/healthServices/health/chronic/steps.aspx.
- 85.Greineder DK, Loane KC, Parks P. Outcomes for control patients referred to a pediatric asthma outreach program: an example of the Hawthorne effect. Am J Manag Care. 1998;4(2):196–202. [PubMed] [Google Scholar]