Abstract
This paper examines how age at immigration influences the association between adult subjective social status and mental health outcomes. The age when people immigrate shapes the capacity and efficiency at which they learn and use a new language, the opportunities to meet and socialize with a wide range of people, and respond to healthy or stressful environments. We hypothesize that adult subjective social status will be more predictive of health outcomes among immigrants who arrive in the US in mid- to late-adulthood compared with immigrants who arrive earlier. To investigate this hypothesis, data on immigrants are drawn from the US first national survey of mental health among Asian Americans (N = 1451). Logistic regression is used to estimate the relationships between adult subjective social status and mood dysfunction, a composite of anxiety and affective disorder symptoms. As predicted, age at immigration moderated the relationship between adult subjective social status and mood dysfunction. Adult subjective social status was related to health among immigrants arriving when they were 25 years and older, but there was no association between subjective social status and mental health among immigrants arriving before the age of 25 years.
Keywords: US, Mental health, Subjective social status, Age at immigration, Developmental context, Asians
Introduction
Past studies on the mental health of immigrants find that foreign-born Asians and Latinos report better mental health than their US-born counterparts (Alegría et al., 2007; Breslau & Chang, 2006; Burnham, Hough, Escobar, Karno, & Timbers, 1987; Takeuchi, Zane et al., 2007; Williams et al., 2007). Socioeconomic status (SES) may be an important determinant of mental health among immigrants. SES is often linked to adaptation and social mobility which are frequently related to various quality of life indicators (Evans-Campbell, Lincoln, & Takeuchi, 2007; Franzini & Fernandez-Esquer, 2006; Rumbaut, 1991). However, empirical studies often treat immigrants as a homogenous group without considering the social factors that may influence the association between SES and mental health. One such factor that captures the heterogeneity of the immigration experience is the developmental context of immigration or the age when immigrants first arrive in a country. Immigrating during childhood, adolescence, or early adulthood, which are formative periods of life, can expose individuals to a particular set of risks with long-ranging consequences for the relationship between adult SES and mental health in adulthood. In this paper, we specifically examine whether age at immigration is a potential moderator in the relationship between adult SES and mental health among a nationally representative sample of Asian immigrants.
Immigration has increased substantially over the past three decades. While the annual naturalization of immigrants peaked at 1 million in 1996, current numbers are still well over the levels of the 1980s (Fix, Passel, & Sucher, 2003). A large share of this immigration has come from Mexico, China, the Philippines, and other Asian and South American countries. The large numbers of immigrants from these diverse countries have radically changed the racial and ethnic profile in the US. Latino Americans are now the largest minority group in America, comprising 13% of the US population (U.S. Census Bureau, 2003). While Asian Americans are not as large as the Latino population, they experienced the largest percentage increase of the major ethnic categories. Since the 2000 U.S. Census allowed respondents to check more than one racial category, there are at least two ways to mark the growth of Asian Americans. Asian Americans grew by 48% (or 3.3 million) if the Asian alone category in the 2000 U.S. Census is used. If multiracial Asians are counted in the Asian category, Asians grew by 5 million or 72%. By comparison, the population of the U.S. in its entirety increased by only 13% (Barnes & Bennett, 2002). Given that 25% of immigrants who come to the US are from Asia, Asian Americans represent an important group to examine how age at immigration influences the association between SES and mental health. Studying Asian Americans is especially important in understanding the development of American children. Nearly one quarter (23%) of all American children under the age of 6 years have parents who were born in Asia (Capps, Fix, Ost, Reardon-Anderson, & Passel, 2004).
Subjective social status and SES
Adult SES is associated with the risk for different physical diseases even among individuals who live above the poverty line (Adler et al., 1994; Marmot, Shipley, & Rose, 1984). While conventional SES measures such as education, income, and occupation are often important predictors of health, subjective social status has increasingly been shown to be an equally critical determinant of physical and mental health among adults (Wilkinson, 1999). In a study by Adler, Epel, Castellazzo, and Ickovics (2000), a new subjective social status measure was demonstrated as significantly related to adult physical and mental health outcomes. Subjective social status was measured using a symbolic ladder with 10 rungs that asked participants to place themselves in comparison with others in the US in relation to common aspects of what it means to be at the top and bottom of society (e.g., the top have the most money and education and the best jobs). This subjective social status measure has been demonstrated to be significantly related to adult physical health outcomes, even after controlling for traditional SES measures among British civil servants, low-income Mexican Americans, ethnically diverse pregnant women, and older Taiwanese (Franzini & Fernandez-Esquer, 2006; Hu, Adler, Goldman, Weinstein, & Seeman, 2005; Ostrove, Adler, Kuppermann, & Washington, 2000; Singh-Manoux, Adler, & Marmot, 2003). A second measure of subjective social status (csubjective social status) asks participants to place themselves in comparison with others in the community that is most important to them. Few studies have reported the association between csubjective social status and health. Despite the substantive increase of research on subjective social status and health, it is only recently that empirical studies have begun to focus on whether subjective social status and csubjective social status operate similarly or differently across a range of groups based on race, ethnicity, nativity, and traditional measures of SES.
The meaning of subjective social status has been debated with some scholars suggesting that subjective social status measures the psychosocial correlates of health inequalities such as relative social rank (Macleod, Davey Smith, Metcalfe, & Hart, 2005). However, subjective social status may be a more nuanced measure of socioeconomic status than current “crude” measures of education, occupation, and income (Adler et al., 1994, 2000). As a predictor of health, measures of subjective social status deserve more research attention as they have demonstrated predictive power when traditional SES measures have not (Adler et al., 1994, 2000).
Age at immigration
We propose that the developmental context, or the age when an immigrant arrives in a new country, may be a critical factor that moderates the association between subjective social status and mental health. The age when people immigrate shapes the capacity and efficiency at which immigrants learn and use a new language, the opportunities to meet and socialize with a wide range of people, and the exposure to healthy or stressful environments. This context may lead to different life course trajectories because the social institutions that affect people’s lives, such as schools, families, and workplaces, vary by age at immigration (Fuligni, 2004; Rumbaut, 2004).
Developmental context can affect SES, subjective social status and mental health in at least two distinct but seemingly paradoxical ways. First, age at immigration can affect SES by influencing the sort of educational experience a person receives. Immigrants who arrive as children or young adults have an easier time than older immigrants learning English and becoming established in US-born peer networks. While their education trajectories may not be identical to US-born individuals, immigrants who come at younger ages are most likely among all immigrant generations to accrue similar rewards and resources from their educational experiences as U.S.-born children. For older immigrants, education may not lead to the same personal, economic and social benefits as for U.S.-born individuals, especially if they are schooled in another country (Zeng & Xie, 2004). Their foreign educational credentials and overseas networks often do not secure as much career advancement as those of U.S.-born residents.
Accordingly, conventional measures of SES may be a more important marker of health among immigrants who arrive as children or young adults and less important for immigrants who arrive as older adults. Education consistently demonstrates a stable direct association with positive health (Williams & Collins, 1995). In many respects, education is considered the causal mechanism that leads to economic and social rewards. Progression through the educational pipeline is seen as leading to higher cognitive abilities, better quality and more secure jobs in safe work environments, more opportunities to enhance income, greater capacity to increase wealth, and a wider range of social networks that provide instrumental and emotional support (Mirowsky & Ross, 1998). All these factors are linked to better mental health.
On the other hand, the salutary effects of social mobility may be less pronounced among immigrants who arrive at early ages. In fact, some evidence shows that the earlier timing of immigration can actually increase an adult’s risk for psychiatric disorders among Asian Americans. Immigration during childhood and adolescence, for example, coincides with the risk period for the onset of affective and anxiety disorders. Takeuchi, Hong, Gile, & Alegría (2007) found that age at immigration was linked to lifetime and adult 12-month prevalence of psychiatric disorders. Adult US-born and immigrant Asian Americans who arrived earlier in life were more likely to have both lifetime and 12-month mental disorders compared with immigrants who arrived at later developmental periods in life.
How is immigration at early ages linked to poorer mental health outcomes? Converging findings show that early socioeconomic developmental contexts have a “long reach” and affect the development of biological mechanisms that underlie the ability to regulate stress as adults (Hayward & Gorman, 2004). Emotional and cognitive development matures in early adulthood (Giedd, 2004; Gogtay, Giedd, & Lusk, 2004), so it is likely that disruption during childhood, adolescence, and early adulthood will influence mental health in middle- and late-adulthood. McLoyd (1990) suggests that families experiencing economic stress may produce a greater risk for socioemotional problems among children because poverty and few economic resources limit the capacity for supportive, consistent, and involved parenting. Psychological studies of adolescents and young adults also suggest that young immigrants may face unique psychosocial stressors that may influence later-adult mental health. For example, they simultaneously negotiate dominant US values expressed in peer groups, school, and society with competing dominant values of their home country expressed in their families and communities (Benet-Martinez, Leu, Lee, & Morris, 2002; Fuligni, 2004; Hong, Morris, Chiu, & Benet-Martinez, 2000). These stressors may result in enduring family cultural conflict in adulthood (Leu et al., in preparation).
We build on past studies to examine how age at immigration shapes the relationship between adult subjective social status measures and mental health among Asian immigrants in the US. Immigrants who arrive in middle- and late-adulthood are less likely to have experienced sociocultural disruption and economic instability while growing up, compared with those who immigrate as children, adolescents, or young adults. If this is true, adult measures of subjective social status may be more relevant to adult mental health outcomes among immigrants who arrived in middle to late adulthood, compared with those who arrived at an earlier age. Stressful early developmental contexts, such as the cultural and socioeconomic challenges that accompany immigration, may be so powerful that they are more predictive of adult mental health outcomes than even subjective social status in adulthood. We test our prediction by using age at immigration as a proxy for the developmental context of immigration.
Hypothesis 1
We examine age at immigration as a moderator in the relationship between adult subjective social status and mental health outcomes. We expect to find a stronger relationship between adult subjective social status and mental health among Asian American immigrants who arrived as mid- to late-adults, compared with those who arrived at an earlier age.
Hypothesis 2
We also test whether the moderation replicates when using the community subjective social status measure (csubjective social status). The csubjective social status measure allows participants to compare themselves with any community.
Methods
We selected Asian American data from the National Latino and Asian American Survey, which used a multi-frame, stratified probability sampling scheme. The scheme has been described in detail elsewhere (Heeringa et al., 2004), but a summary follows. Samples were drawn using three methods. In the first, participants were recruited with a multistage stratified area probability sampling design: (a) city or contiguous census blocks were sampled based on population density in each neighborhood; (b) dwelling units were sampled within each block; (c) one adult was sampled within each selected dwelling unit. In the second method, census blocks with at least 5% of Asian households were over-sampled. In the third method, to increase the sample size, a second respondent from a previously sampled household was recruited. Weighting corrections were constructed to control for differences in selection probability.
Among the surveyed Asian Americans (N = 2095), 454 were US-born, 1639 were foreign-born, and 2 did not identify a place of birth. Interviews were offered in English, Mandarin, Cantonese, Tagalog, and Vietnamese. The three largest ethnic groups represented were Chinese (32%), Filipino (20%), and Vietnamese (16%). Participants self-identified with national origins in the regions of East Asia, Southeast Asia, South Asia, and Central Asia.
This analysis only included data from foreign-born Asian American participants aged 25 years and older (N = 1451). Age at immigration, dichotomized at age 25 years, was tested as a potential moderator of the relationship between subjective social status and mental health. The age of 25 years was used as a psychosocial marker to distinguish between immigrants who experienced disruption during formative years (i.e., childhood, adolescence, early adulthood) versus later-adult years (i.e., middle- and late-adulthood). Recent psychological evidence suggests that social and cognitive development does not reach maturation until roughly the age of 25 years (Giedd, 2004; Gogtay et al., 2004). We theorize that the influence of age at immigration on the relationship between subjective social status and mental health is a psychosocial, as opposed to a biological, phenomenon. Age at immigration may capture a developmental context that includes influences of the family, US peers, and institutional practices (i.e., formal education). Therefore, age at immigration was treated as a categorical rather than continuous variable. This practice is consistent with related research on generations and immigrant health (Rumbaut, 2004; Takeuchi, Hong et al., 2007).
Measures
Mood dysfunction
Our dependent variable was the presence of mood dysfunction in the 12 months prior to the interview (12-month period prevalence). Mood dysfunction was a composite formed by the presence of at least one clinical or sub-clinical symptom of anxiety or affective disorder, as measured by the Composite International Diagnostic Interview (CIDI; World Health Organization). The CIDI is the most widely used structured diagnostic interview and was designed to be used across cultures. A composite variable was used because separate analyses of anxiety (e.g., generalized anxiety disorder, agoraphobia, social phobia, post-traumatic stress disorder, and panic disorder) and affective disorders (e.g., dysthymia and major depressive episodes) produced similar results.
Subjective social status
Our independent variable was subjective social status, as measured by a symbolic ladder with 10 rungs, where the first and tenth rung represent the lowest and highest social status, respectively (Adler et al., 2000; Cantril, 1965). Two dimensions of status were assessed. In one, subjective social status, respondents were asked to, “Think of this ladder as representing where people stand in the US. At the top of the ladder are the people who are the best off, those who have the most money, most education, and best jobs. At the bottom are the people who are the worst off, those who have the least money, least education, and worst jobs or no job. What is the number to the right of the rung where you think you stand at this time in your life, relative to other people in the United States?”
In the second measure, csubjective social status, respondents were asked to, “Think of this ladder as representing where people stand in their communities. People define community in different ways; please de fine it in whatever way is most meaningful for you. At the top of the ladder are the people who have the highest standing in their community. At the bottom are the people who have the lowest standing in their community. What is the number to the right of the rung where you think you stand at this time in your life, relative to other people in your community?”
SES
Two conventional measures of SES were analyzed. Educational attainment was measured by having respondents indicate the number of years of schooling they had completed; it was coded into several dummy variables in the analyses representing meaningful educational milestones. These dummy variables represent receipt of less than a high school education (0–11 years); high school graduate (12 years); some college (13–15 years); and college graduate and beyond (16 or more years). In analyses, we treat 16 or more years of education, the largest group, as the reference category. Household income is the sum of the midpoints of the following income measures: personal, spouse, other family members, social security, government assistance, and other sources. Because of a large number of missing values (270 missing), this variable was imputed using hot deck methods based on the variables of ethnicity, sex, age, education, household composition, and employment status. We divided household income by 1000 and collapsed it into four categories that we represent as a series of meaningful dichotomies, using $80,000 or more as the reference group. We control for the family size in order to make household income interpretable at the individual level.
Demographic variables
Gender, ethnicity, US citizenship, marital status, English language proficiency, current age, and age at immigration were also examined. Ethnicity was categorized into one of four groups (Vietnamese, Filipino, Chinese, and Other Asian), where Chinese was the reference group as the largest ethnicity represented. US citizenship was dichotomized non-citizen versus citizen (reference group). Marital status was dichotomized married versus non-married (reference group). English language proficiency is a scale which asks the respondent to rank his or her ability to speak, read and write in English. For these three measures, response categories range from (1) poor to (4) excellent, yielding minimum and maximum scores from 3 to 12.
Current age and age at immigration were single-item measurements. Current age was divided by 10 in the multivariate regressions and descriptive statistics for easier interpretation, but still treated as a continuous variable. Age at immigration was dichotomized at age 25 years, and its influence on mood dysfunction was measured using a dummy variable for participants who moved to the US before the age of 25 years.
Statistical analysis
Our main analysis consists of a series of nested multivariate survey logistic regression models which assess the net effect of adult subjective social status on the presence of mood dysfunction. All of the analyses adjust for the hierarchical nature of the multistage survey data using SAS-callable SUDAAN procedures. The SUDAAN procedures allow for the incorporation of complex survey sampling methods, including designs with stratification, clustering, and unequal sampling weights, in the point and standard error (SE) estimation.
Table 1 provides descriptive statistics for the total sample, and stratifies the sample by age at immigration. t-Tests were used to compare the weighted means for all variables in the age at immigration.
Table 1.
Weighted means for all the variables in the analyses, total sample and stratified by age at immigration
| Variables | Total samples |
Age at immigration |
||
|---|---|---|---|---|
| (N = 1451) | <25 years (N = 607) | ≥25 years (N = 844) | t-Value | |
| Mood dysfunction | 0.11 | 0.13 | 0.09 | 2.14* |
| Subjective social status (subjective social status) |
5.77 | 6.17 | 5.48 | 4.62*** |
| Community subjective social status (csubjective social status) |
6.20 | 6.43 | 6.03 | 2.84** |
| Education | ||||
| 0–11 years | 0.19 | 0.12 | 0.24 | 4.11*** |
| 12 years | 0.15 | 0.15 | 0.15 | 0.27 |
| 13–15 years | 0.20 | 0.27 | 0.16 | 4.71*** |
| 16 or more years | 0.46 | 0.46 | 0.46 | 0.08 |
| Household income | ||||
| Less than $17,000 | 0.15 | 0.07 | 0.21 | 4.62*** |
| $17,000–$44,999 | 0.19 | 0.16 | 0.20 | 1.95 |
| $45,000–$79,999 | 0.23 | 0.25 | 0.23 | 0.87 |
| $80,000 or more | 0.43 | 0.52 | 0.36 | 3.89*** |
| Family size | 2.90 | 2.96 | 2.86 | 0.83 |
| Married | 0.80 | 0.76 | 0.83 | 2.23* |
| Age | 44.86 | 38.63 | 49.39 | 9.35*** |
| Male | 0.46 | 0.47 | 0.45 | 0.64 |
| Ethnicity | ||||
| Vietnamese | 0.16 | 0.14 | 0.17 | 1.36 |
| Filipino | 0.20 | 0.2 | 0.21 | 0.19 |
| Chinese | 0.32 | 0.27 | 0.35 | 2.37* |
| Other Asian | 0.32 | 0.39 | 0.28 | 3.01** |
| Non-citizen | 0.39 | 0.25 | 0.48 | 6.55*** |
| English language proficiency | 7.83 | 8.97 | 7.01 | 8.34*** |
| Age at immigration < 25 | 0.42 | – | – | |
0.01 < p ≤ 0.05
0.001 < p ≤ 0.01
p ≤ 0.001.
Table 2 reports the results from a series of survey logistic regressions which focus on the relationship of subjective social status to the outcome of mood dysfunction. We report unstandardized maximum likelihood coefficients and their significance levels. We perform this analysis in six steps. Model 1 tests the unadjusted bivariate relationship of subjective social status with mood dysfunction. Models 2 and 3 sequentially add traditional SES and demographic measures to determine if the effects of subjective social status on mood dysfunction remain after their inclusion in the analyses. In Model 4, we test the direct effect of age at immigration on mood dysfunction. In Models 5 and 6, we assess whether the effects of subjective social status on mood dysfunction depend on current age or age at immigration by incorporating interaction terms; given the high correlation between current age and age at immigration, each variable was tested separately as a potential moderator.
Table 2.
The effects of subjective social status on mood dysfunction using survey logistic regression (N = 1451)
| Variables | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 |
|---|---|---|---|---|---|---|
| Subjective social status (subjective social status) |
−0.13* | −0.17** | −0.15** | −0.16** | 0.38 | −0.31*** |
| Education | ||||||
| 0–11 years | −0.41 | −0.34 | −0.46 | −0.59 | −0.54 | |
| 12 years | −0.20 | −0.18 | −0.30 | −0.24 | −0.26 | |
| 13–15 years | −0.05 | −0.08 | −0.17 | −0.12 | −0.15 | |
| 16 or more years | ||||||
| Household income | ||||||
| Less than $17,000 | 0.27 | 0.01 | 0.08 | 0.00 | 0.03 | |
| $17,000–$44,999 | −0.56 | −0.71* | −0.69* | −0.71* | −0.65* | |
| $45,000–$79,999 | 0.18 | 0.21 | 0.22 | 0.17 | 0.21 | |
| $80,000 or more | ||||||
| Family size | −0.18* | −0.15 | −0.14 | −0.12 | −0.13 | |
| Married | −0.77** | −0.69* | −0.72* | −0.73* | ||
| Age (in 10-year increments) | −0.08 | 0.02 | 0.63 | 0.01 | ||
| Male | −0.32 | −0.32 | −0.30 | −0.32 | ||
| Ethnicity | ||||||
| Vietnamese | −0.03 | −0.05 | −0.12 | −0.06 | ||
| Filipino | −0.16 | −0.14 | −0.07 | −0.07 | ||
| Chinese | ||||||
| Other Asian | 0.22 | 0.18 | 0.21 | 0.23 | ||
| Non-citizen | −0.05 | 0.15 | 0.10 | 0.18 | ||
| English language proficiency | −0.04 | −0.07 | −0.08 | −0.07 | ||
| Age at immigration < 25 | 0.68* | 0.68* | −1.22 | |||
| Interactions | ||||||
| Age × subjective social status | −0.12* | |||||
| Age at immigration < 25 × subjective social status | 0.34* | |||||
| Intercept | −1.37*** | −0.59 | 0.70 | 0.08 | −2.72 | 0.84 |
0.01 < p ≤ 0.05
0.001 < p ≤ 0.01
p ≤ 0.001.
In this approach, outlined by Baron and Kenny (1986), current age and age at immigration are determined to moderate the relationship between subjective social status and mood dysfunction if there is a significant interaction. The analyses presented in Table 3 replicate those presented in Table 2, but substituting csubjective social status for subjective social status in all analyses.
Table 3.
The effects of csubjective social status on mood dysfunction using survey logistic regression (N = 1451)
| Variables | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 |
|---|---|---|---|---|---|---|
| Community subjective social status (csubjective social status) |
−0.10 | −0.11* | −0.10 | −0.10 | 0.20 | −0.23** |
| Education | ||||||
| 0–11 years | −0.29 | −0.27 | −0.38 | −0.42 | −0.43 | |
| 12 years | −0.09 | −0.10 | −0.22 | −0.20 | −0.12 | |
| 13–15 years | −0.02 | −0.05 | −0.14 | −0.13 | −0.13 | |
| 16 or more years | ||||||
| Household income | ||||||
| Less than $17,000 | 0.42 | 0.10 | 0.17 | 0.13 | 0.10 | |
| $17,000–$44,999 | −0.47 | −0.67 | −0.64 | −0.62 | −0.64 | |
| $45,000–$79,999 | 0.26 | 0.28 | 0.30 | 0.30 | 0.30 | |
| $80,000 or more | ||||||
| Family size | −0.18* | −0.14 | −0.14 | −0.13 | −0.13 | |
| Married | −0.83** | −0.77** | −0.77** | −0.75** | ||
| Age (in 10-year increments) | −0.08 | 0.02 | 0.39 | 0.02 | ||
| Male | −0.31 | −0.31 | −0.30 | −0.31 | ||
| Ethnicity | ||||||
| Vietnamese | −0.03 | −0.03 | −0.07 | −0.08 | ||
| Filipino | −0.17 | −0.15 | −0.14 | −0.17 | ||
| Chinese | ||||||
| Other Asian | 0.25 | 0.21 | 0.21 | 0.20 | ||
| Non-citizen | −0.03 | 0.16 | 0.14 | 0.19 | ||
| English language proficiency | −0.06 | −0.09 | −0.09 | −0.08 | ||
| Age at Immigration < 25 | 0.65* | 0.64* | −1.12 | |||
| Interactions | ||||||
| Age × subjective social status | −0.06 | |||||
| Age at immigration < 25 × subjective social status | 0.29* | |||||
| Intercept | −1.47*** | −0.93* | 0.50 | −0.12 | −1.87 | 0.47 |
0.01 < p ≤ 0.05
0.001 < p ≤ 0.01
p ≤ 0.001.
Results
Descriptive statistics and comparisons
Descriptive statistics
We limited data to foreign-born participants aged 25 years and older (N = 1451). Eleven percent of the sample reported mood dysfunction in the past 12 months (see Table 1). Weighted 12-month period prevalence was based on the presence of at least one clinical or sub-threshold report of an anxiety disorder in the past 12 months (5.2% clinical and 5.0% sub-threshold panic disorder, agoraphobia, social phobia, post-traumatic stress disorder, and generalized anxiety disorder). It was also based on the presence of at least one clinical and sub-threshold report of an affective disorder in the past 12 months (3.4 % clinical and 3.3 % sub-threshold major depressive episode and dysthymia). Participants could have reported multiple dysfunctions.
Respondents reported a mean age at immigration of 28 years (SE = 0.71). The median was 26 years and the mode was 24 years. Age at immigration scores ranged from 0 to 82. On average, participants spent an average of 17 (SE = 0.76) years in the US (not shown in Table 1), and were aged 45 (SE = 0.93) years at the interview. Forty-two percent of participants immigrated before the age of 25 years (N = 607); 58% at or after age 25 years (N = 844).
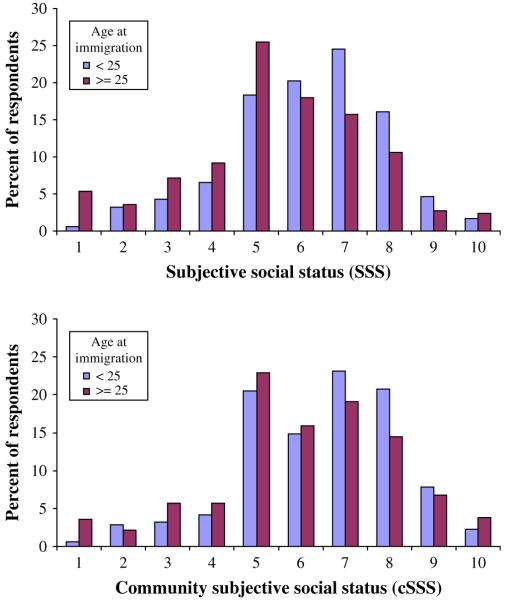
Respondents scored a mean of 5.8 (SE = 0.09) on the subjective social status measure, and a mean of 6.20 (SE = 0.10) on the csubjective social status measure. Fig. 1 illustrates the distributions of subjective social status and csubjective social status rankings, ranging from 1 to 10, and using the two categories of age at immigration (<25 versus ≥25 years).
Fig. 1.
Subjective social status (subjective social status) and community subjective social status (csubjective social status) by age at immigration.
The sample was 54% female. The mean household income was $87,240 (median = $64,500), and immigrants who arrived before the age of 25 years reported significantly higher mean income ($99,710; median = $84,500) than immigrants who arrived at or after the age of 25 years ($78,180; median = $54,000).
Descriptive comparisons by age at immigration
Immigrants who arrived before the age of 25 years had a greater prevalence of mood dysfunction than did those who came at or after the age of 25 years (13% versus 9%). Consistent with other studies, this suggests that immigrants who arrive in mid- to late-adulthood report better adult mental health than those who arrive earlier. This finding is notable given that immigrants who arrived before age 25 years attain higher levels of educational achievement and income than those who arrived when they were older (Table 1).
Many significant differences across age categories, as opposed to age at immigration categories, were also found for subjective social status, education, income, family size, Filipino and Other Asian ethnicity, and age at immigration (not reported). These suggest possible cohort effects. Cohort effects by age at immigration were investigated using the following categories: 1 = before 1965 (N = 67); 2 = 1965–1980 (N = 370); 3 = 1980–1990 (N = 436); 4 = 1990 and after (N = 578). We found no significant direct or indirect effects of cohort. Instead, the cross-sectional data allowed us to test two theoretically-driven hypotheses about adult subjective social status as a predictor, and age at immigration as a moderator, of mental health.
Hypothesis 1
Subjective social status as a predictor of mental health
Table 2 presents the results of six models that examined the relationship between subjective social status, including traditional SES measures, and mood dysfunction. Subjective social status was a significant predictor of mood dysfunction (B = –0.15 (0.06), p = 0.009) after adjusting for traditional SES markers and relevant demographic measures (Model 3). Higher ratings of subjective social status were associated with lower chance of mood dysfunction, consistent with evidence in the existing literature on subjective social status. Neither education nor income predicted mood dysfunction in any consistent direction.
Testing current age and age at immigration as moderators
We tested the hypothesis that age at immigration moderated the relationship between subjective social status and mood dysfunction. Given the high correlation between current age and age at immigration, we also separately tested current age as a moderator. We created interaction terms between subjective social status and age at immigration (dichotomized at age 25 years), and between subjective social status and current age. We divided current age by 10 to increase the interpretability of the results but still treated it as a continuous variable in the analyses.
Current age was a significant moderator of the relationship between subjective social status and mood dysfunction as shown in Table 2, (B = –0.12 (0.05), p = 0.016) (Model 5). Subjective social status was more predictive of mood dysfunction among older respondents (i.e., age 66 years and older) than among younger respondents (i.e., ages 25–35 years). There is a crossover effect around the mean value of subjective social status demonstrating the interaction. Subjective social status was more predictive of mood dysfunction among people who were older (i.e., age 66 years and older) than among people who were younger (i.e., age 25–35 years) at the extreme low end of subjective social status. In this model, the direct effect of age remained positively related to mood dysfunction (B = 0.63 (0.28), p = 0.027), being married remained negatively related to mood dysfunction (B = –0.72 (0.29), p = 0.015), and those with household income of $17,000–$44,999 were less likely to report mood dysfunction compared to those with household income of $80,000 or more (B = –0.71 (0.32), p = 0.029). Age at immigration was also a significant predictor (B = 0.68 (0.28), p = 0.017).
Age at immigration was a significant moderator of the relationship between subjective social status and mood dysfunction (B = 0.34 (0.13), p = 0.011) (Model 6). As seen in Fig. 2, subjective social status was predictive of mood dysfunction among people who immigrated to the US at or after the age of 25 years, but not among those who immigrated before the age of 25 years. As in previous models, being married was negatively associated with mood dysfunction (B = –0.73 (0.28), p = 0.011), and those with household income of $17,000–$44,999 were less likely to report mood dysfunction compared to those with household income of $80,000 or more (B = –0.65 (0.32), p = 0.047). Subjective social status remained a significant predictor of mood dysfunction (B = –0.31 (0.09), p = 0.001) after the inclusion of an interaction term with age at immigration.
Fig. 2.
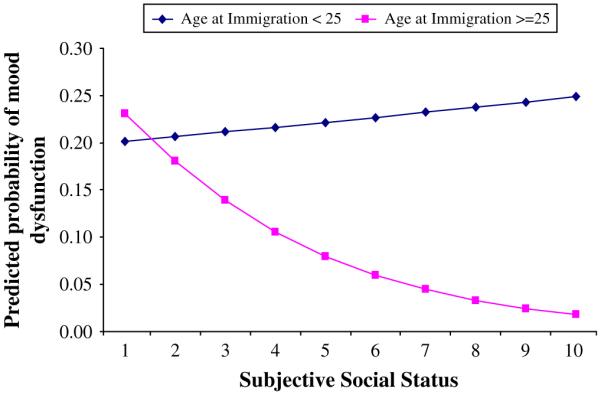
Moderating effects of age at immigration in the relationship between subjective social status (subjective social status) and mood dysfunction. Note: Data come from Table 2, Model 6.
This finding was replicated when analyzing affective and anxiety disorders separately (results not shown). Using the same series of nested multivariate survey logistic regression models, age at immigration was a significant moderator in the relationship between subjective social status and affective disorders. There was also evidence of a trend that age at immigration moderated the relationship between subjective social status and anxiety disorders.
Hypothesis 2
Csubjective social status as a predictor of mental health
Table 3 presents six models that examined the relationship between csubjective social status and mood dysfunction. Each model builds upon the previous; the final two models test for moderation effects. Csubjective social status was a significant predictor of mood dysfunction (B = –0.11 (0.06), p = 0.043) after adjusting for traditional SES markers (Model 2). Higher ratings of csubjective social status were associated with lower chance of mood dysfunction. Neither education nor household income was a significant predictor of mental health. In Model 3, however, csubjective social status was no longer a significant predictor of mood dysfunction either, after including relevant demographic measures.
Testing current age and age at immigration as moderators
We tested the hypothesis that age at immigration moderated the relationship between csubjective social status and mood dysfunction. Ratings of csubjective social status were significantly correlated with ratings of subjective social status (r = 0.70, p < 0.001). Given a high correlation between current age and age at immigration, we also separately tested current age as a moderator.
Current age was not a significant moderator (B = –0.06 (0.05), p = 0.204) (Model 5). In this model, marital status (B = –0.77 (0.27), p = 0.007) and age at immigration (dichotomized at age 25 yeas) (B = 0.64 (0.28), p = 0.027) remained significant predictors of mood dysfunction. Those who were not married and that immigrated before the age of 25 years had higher predicted probability of mood dysfunction compared to married individuals who immigrated at later ages.
Age at immigration was a significant moderator of the relationship between csubjective social status and mood dysfunction (B = 0.29 (0.12), p = 0.020) (Model 6). As seen in Fig. 3, csubjective social status was predictive of mood dysfunction among people who immigrated to the US at or after the age of 25 years, but not among those who immigrated before the age of 25 years. Like in previous models, being married was negatively associated with mood dysfunction (B = –0.75 (0.26), p = 0.006), as was csubjective social status (B = –0.23 (0.08), p = 0.006). Individuals who were married and with higher values of csubjective social status had lower predicted probability of mood dysfunction compared to unmarried individuals with lower csubjective social status.
Fig. 3.

Moderating effects of age at immigration in the relationship between community subjective social status (csubjective social status) and mood dysfunction. Note: Data come from Table 3, Model 6.
This finding was replicated when analyzing affective and anxiety disorders separately (results not shown). Using the same series of nested multivariate survey logistic regression models, age at immigration was a significant moderator in the relationship between csubjective social status and affective disorders. Age at immigration also moderated the relationship between csubjective social status and anxiety disorders.
Discussion
Our data demonstrate worse mental health among Asian immigrants who arrived before age 25 years, despite greater educational and income gains at the time of the survey, compared with immigrants who arrived later.
There was a reliable association between mood dysfunction and adult subjective social status, which provides further evidence that subjective social status may be as or more important in predicting immigrant health as traditional measures of socioeconomic status. Education and income did not predict mood dysfunction, probably because the distributions were skewed to the lower and upper extremes of the categories.
As hypothesized, we found consistent evidence that developmental contexts may shape the relationship between adult subjective social status and mental health. Age at immigration moderated the relationship between subjective social status and mood dysfunction. Subjective social status predicted mood dysfunction among immigrants who came at or after age 25 years, but did not predict mood dysfunction among immigrants who came before age 25 years. This moderation was replicated using csubjective social status, eliminating the interpretation that the moderation effect was driven by different comparison groups, as opposed to different developmental contexts. Lastly, the moderation was replicated with both subjective social status and csubjective social status when anxiety and affective dysfunction were analyzed separately.
Significance of findings
Subjective social status and csubjective social status
Very few studies have examined how subjective social status and csubjective social status relate to health outcomes. Csubjective social status is especially relevant to studying immigrant health, given that immigrants may use a range of comparison groups that are not limited to US populations. For example, Franzini and Fernandez-Esquer (2006) found that low-income Mexican Americans differed in their comparison groups depending on nativity (i.e., born in the US or Mexico) and primary language (i.e., English or Spanish). For example, US-born English speaking Mexican Americans were most likely, and Mexico-born Spanish speaking Mexican Americans were least likely to compare themselves with English speaking Anglo Americans.
Replication of the moderation effect with subjective social status and csubjective social status eliminates the interpretation of age at immigration as only a marker of differences in comparison groups. Immigrants may compare themselves with different groups depending on their age at immigration, but this does not explain the moderating influence of age at immigration on the relationship between subjective social status/csubjective social status and mood dysfunction. Instead, it seems that age at immigration is a valid proxy for developmental contexts.
Epidemiological paradox
Similar to health outcomes among other immigrant groups, we found evidence of an “epidemiological paradox” (Scribner, 1991). As seen in Table 1, immigrants who came at an earlier age had a higher prevalence of mood dysfunction despite gains in subjective social status, education, and income. This finding is consistent with social epidemiological evidence that suggests declines from the first to second immigrant generation in coronary heart disease among Japanese immigrants (Marmot & Syme, 1976) and among Italian immigrants (Lasker, Egolf, & Wolf, 1994). It is also consistent with patterns of preterm or low birth-weight births to immigrant Latinas (Scribner, 1991), hypertension rates among West-Indian or Caribbean immigrants in the US (Read, Emerson, & Tarlov, 2005), and psychiatric disorders among Asian Americans (Breslau & Chang, 2006; Frisbie, Cho, & Hummer, 2001; Hwang, Chun, Takeuchi, Myers, & Siddarth, 2005; Takeuchi, Hong et al., 2007).
The epidemiological paradox has generally been discussed as a loss of protective sociocultural factors from one generation to the next, producing racial and ethnic health disparities in comparison with White Americans. However, other findings from the NLAAS data suggest that the decline in health may also be explained as the increased socioemotional burden of racial discrimination from one generation to the next. For example, Asian immigrants who arrived before the age of 25 years reported more discrimination than those who arrived at older ages, despite having better English proficiency (Leu et al., in preparation). The findings of Gee, Spencer, Chen, and Takeuchi (2006) and Viruell-Fuentes (2007) further support this interpretation in other racial minority immigrant groups.
This study provides preliminary evidence that developmental contexts need to be considered in understanding the epidemiological paradox. In analyses not reported here, we replicated the interaction effect when age at immigration was dichotomized at 18 years. This suggests that neither 18 nor 25 years are special biological ages marking a critical window of development. Rather, both ages 18 and 25 years may approximate meaningful shifts in developmental trajectories for immigrants depending on the life stage in which they immigrate to the US. Theoretical contributions from psychology and a life course perspective are needed to illuminate important interactions between psychosocial, sociological, and developmental factors in determining ethnic minority immigrant health (Ben-Shlomo & Kuh, 2002; Hertzman, 1999).
Racial/ethnic disparities
The foreign-born comprise over 75% of the Asian American population, almost 60% of the US Latino population, and over 10% of the total US population (U.S. Census Bureau, 2003). It is likely that understanding the social and developmental determinants of health among immigrants will also illuminate the social and developmental determinants of racial/ethnic health disparities (Read et al., 2005; Williams, 1999). Williams (1999) suggests that with greater time in the US, the health status of an immigrant declines. Our findings suggest that immigrating at earlier ages may also contribute to declines in immigrant mental health.
Limitations
There are obvious limits to claims of causality with cross-sectional data. Using reports of mood dysfunction within 12 months of the interview lends some strength to the idea that psychosocial elements of the immigrant experience contributes to adult health, and not vice versa in this study. A longitudinal study needs to be conducted to parse out the influences of current age versus age at immigration in predicting health outcomes, and to determine the causal effects of specific stressors.
It is also reasonable to wonder whether there may be differences in reporting mood dysfunction, assuming greater social stigma of mental disorders among Asian immigrants who came at a later age. However, another study using the Asian American data from the NLAAS found no evidence that foreign-born Asian Americans were less likely to endorse extreme categories in self-rated physical and mental health than native-born (Erosheva, Walton, & Takeuchi, 2007). Additionally, there was no evidence of imbalances in endorsement of any particular self-rated health category between the two groups.
Future directions
With these findings, understanding the causal relationship between adult subjective social status and mental health among immigrants necessitates an examination of developmental trajectories and longitudinal relationships between psychosocial factors and health. Future research using a longitudinal developmental design, for example, may help determine whether the relationship between social position and mental health changes from childhood, adolescence, early adulthood, to mid- and late-adulthood as it does for some chronic health outcomes (Chen, 2004). This may be especially important in order to map mental health trajectories to their social contexts in both countries of origin and countries of arrival. Health trajectories may also be specific to cultural groups and to specific diseases given the particular historical development of social contexts and the different etiology of illnesses.
Alternatively, using recall measures of social position in different developmental stages in a cross-sectional database may also help illuminate the developmental context for the association between social position and health (Haas, 2007). Clearly, there is a need for more in-depth research in the area to better understand the mental health of diverse immigrant Americans.
Footnotes
This project was funded by the Robert Wood Johnson Foundation to understand the social determinants of health in diverse populations from an interdisciplinary perspective.
References
- Adler NE, Boyce T, Chesney MA, et al. Socioeconomic status and health: the challenge of the gradient. American Psychologist. 1994;49(1):15–24. doi: 10.1037//0003-066x.49.1.15. [DOI] [PubMed] [Google Scholar]
- Adler NE, Epel ES, Castellazzo G, Ickovics JR. Relationship of subjective and objective social status with psychological and physiological functioning: preliminary data in healthy White women. Health Psychology. 2000;19(6):586–592. doi: 10.1037//0278-6133.19.6.586. [DOI] [PubMed] [Google Scholar]
- Alegría M, Mulvaney-Day N, Torres M, Polo A, Cao Z, Canino G. Prevalence of psychiatric disorders across Latino subgroups in the United States. American Journal of Public Health. 2007;97:68–75. doi: 10.2105/AJPH.2006.087205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes JS, Bennett CE. The Asian population 2000, Census 2000 Brief. US Census Bureau; Washington, D.C.: 2002. [Google Scholar]
- Baron RM, Kenny DA. The moderatore–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Benet-Martinez V, Leu J, Lee F, Morris M. Negotiating biculturalism: cultural frame-switching in biculturals with ‘Oppositional’ vs. ‘Compatible’ cultural identities. Journal of Cross-Cultural Psychology. 2002;33(4):492–516. [Google Scholar]
- Ben-Shlomo Y, Kuh D. A life course approach to chronic disease epidemiology: conceptual models, empirical challenges and interdisciplinary perspectives. International Journal of Epidemiology. 2002;31:285–293. [PubMed] [Google Scholar]
- Breslau J, Chang DF. Psychiatric disorders among foreign-born and US-born Asian-Americans in a US national survey. Social Psychiatry and Psychiatric Epidemiology. 2006;41(12):943–950. doi: 10.1007/s00127-006-0119-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burnham MA, Hough RL, Escobar JI, Karno M, Timbers DM. Six-month prevalence of specific psychiatric disorders among Mexican-Americans and non-Hispanic Whites in Los Angeles. Archives of General Psychiatry. 1987;44:687–694. doi: 10.1001/archpsyc.1987.01800200013003. [DOI] [PubMed] [Google Scholar]
- Cantril H. The pattern of human concerns. Rutgers University Press; New Brunswick, NJ: 1965. [Google Scholar]
- Capps R, Fix ME, Ost J, Reardon-Anderson J, Passel JS. The health and well-being of young children of immigrants. The Urban Institute; 2004. [Google Scholar]
- Chen E. Why socioeconomic status affects the health of children: a psychosocial perspective. Current Directions in Psychological Science. 2004;13:112–115. [Google Scholar]
- Erosheva E, Walton EC, Takeuchi DT. Self-rated health among foreign- and US-born Asian Americans: a test of comparability. Medical Care. 2007;45(1):80–87. doi: 10.1097/01.mlr.0000241114.90614.9c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans-Campbell T, Lincoln KD, Takeuchi DT. Race and mental health: past debates, new opportunities. In: Avison WR, McLeod JD, Pescosolido BA, editors. Mental health, social mirror. Springer; New York: 2007. [Google Scholar]
- Fix M, Passel J, Sucher K. Trends in naturalization. The Urban Institute; Washington, D.C.: 2003. Immigrant Families and Workers Brief No. 3. [Google Scholar]
- Franzini L, Fernandez-Esquer ME. The association of subjective social status and health in low-income Mexican-origin individuals in Texas. Social Science & Medicine. 2006;63:788–804. doi: 10.1016/j.socscimed.2006.01.009. [DOI] [PubMed] [Google Scholar]
- Frisbie WP, Cho Y, Hummer RA. Immigration and the health of Asian and Pacific Islander adults in the United States. American Journal of Epidemiology. 2001;153(4):372–380. doi: 10.1093/aje/153.4.372. [DOI] [PubMed] [Google Scholar]
- Fuligni AJ. Convergence and divergence in the developmental contexts of immigrants to the United States. In: Schaie W, Elder G, editors. Historical influences on lives and aging. Springer Publishing Company, Inc.; New York: 2004. [Google Scholar]
- Gee GC, Spencer MS, Chen J, Takeuchi D. A nationwide study of discrimination and chronic health conditions among Asian Americans. American Journal of Public Health. 2007;97:1275–1282. doi: 10.2105/AJPH.2006.091827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giedd JN. Structural magnetic resonance imaging of the adolescent brain. In: Dahl RE, Spear LP, editors. Adolescent brain development: Vulnerability and opportunities. New York Academy of Science; New York: 2004. [DOI] [PubMed] [Google Scholar]
- Gogtay N, Giedd JN, Lusk L, et al. Dynamic mapping of human cortical development during childhood through early adulthood. Proceedings of the National Academy of Sciences of the United States of America. 2004;101(21):8174–8179. doi: 10.1073/pnas.0402680101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haas SA. The long-term effects of poor childhood health: an assessment and application of retrospective reports. Demography. 2007;44(1):113–135. doi: 10.1353/dem.2007.0003. [DOI] [PubMed] [Google Scholar]
- Hayward MD, Gorman BK. The long arm of childhood: the influence of early-life social conditions on men’s mortality. Demography. 2004;41(1):87–107. doi: 10.1353/dem.2004.0005. [DOI] [PubMed] [Google Scholar]
- Heeringa SG, Wagner J, Torres M, Duan N, Adams T, Berglund P. Sample designs and sampling methods for the Collaborative Psychiatric Epidemiology Studies (CPES) International Journal of Methods in Psychiatric Research. 2004;13(4):221–240. doi: 10.1002/mpr.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hertzman C. The biological embedding of early experiences and its effects on health in adulthood. In: Adler NE, Marmot M, McEwen BS, Stewart J, editors. Socioeconomic status and health in industrial nations: Social, psychological, and biological pathways. Annals of the New York Academy of Sciences; New York: 1999. pp. 85–95. [DOI] [PubMed] [Google Scholar]
- Hong YY, Morris MW, Chiu CY, Benet-Martinez V. Multicultural minds: a dynamic constructivist approach to culture and cognition. American Psychologist. 2000;55(7):709–720. doi: 10.1037//0003-066x.55.7.709. [DOI] [PubMed] [Google Scholar]
- Hu P, Adler NE, Goldman N, Weinstein M, Seeman TE. Relationship between subjective social status and measures of health in older Taiwanese persons. Journal of the American Geriatrics Society. 2005;53:483–488. doi: 10.1111/j.1532-5415.2005.53169.x. [DOI] [PubMed] [Google Scholar]
- Hwang W-C, Chun C-A, Takeuchi DT, Myers HF, Siddarth P. Age of first onset major depression in Chinese Americans. Cultural Diversity & Ethnic Minority Psychology. 2005;11(1):16–27. doi: 10.1037/1099-9809.11.1.16. [DOI] [PubMed] [Google Scholar]
- Lasker JN, Egolf BP, Wolf S. Community social change and mortality. Social Science & Medicine. 1994;39(1):53–62. doi: 10.1016/0277-9536(94)90165-1. [DOI] [PubMed] [Google Scholar]
- Leu J, Walton E, Yen I, Gansky SA, Adler N, Takeuchi D. Gender and subjective social status among Asian American immigrants. University of Washington; in preparation. [Google Scholar]
- Macleod J, Davey Smith G, Metcalfe C, Hart C. Is subjective social status a more important determinant of health than objective social status? Evidence from a prospective observational study of Scottish men. Social Science & Medicine. 2005;61(9):1916–1929. doi: 10.1016/j.socscimed.2005.04.009. [DOI] [PubMed] [Google Scholar]
- McLoyd VC. The impact of economic hardship on Black families and children: psychological distress, parenting, and socioemotional development. Child Development. 1990;61(2):311–346. doi: 10.1111/j.1467-8624.1990.tb02781.x. [DOI] [PubMed] [Google Scholar]
- Marmot MG, Shipley MJ, Rose G. Inequalities in death: specific explanations of a general pattern? The Lancet. 1984;323:1003–1006. doi: 10.1016/s0140-6736(84)92337-7. [DOI] [PubMed] [Google Scholar]
- Marmot MG, Syme SL. Acculturation and coronary heart disease in Japanese-Americans. American Journal of Epidemiology. 1976;104(3):225–247. doi: 10.1093/oxfordjournals.aje.a112296. [DOI] [PubMed] [Google Scholar]
- Mirowsky J, Ross K. Education, personal control, life-style, and health: a human capital hypothesis. Research on Aging. 1998;20:415–449. [Google Scholar]
- Ostrove JM, Adler NE, Kuppermann M, Washington AE. Objective and subjective assessments of socioeconomic status and their relationship to self-rated health in an ethnically diverse sample of pregnant women. Health Psychology. 2000;19(6):613–618. doi: 10.1037//0278-6133.19.6.613. [DOI] [PubMed] [Google Scholar]
- Read JG, Emerson MO, Tarlov A. Implications of black immigrant health for US racial disparities in health. Journal of Immigrant Health. 2005;7(3):205–212. doi: 10.1007/s10903-005-3677-6. [DOI] [PubMed] [Google Scholar]
- Rumbaut RG. Ethnic minorities and mental health. Annual Review of Sociology. 1991;17:351–383. [Google Scholar]
- Rumbaut RG. Ages, life stages, and generational cohorts: decomposing the immigrant first and second generations in the United States. The International Migration Review. 2004;38(3):1160–1205. [Google Scholar]
- Scribner RA. Infant mortality among Hispanics: the epidemiological paradox. The Journal of the American Medical Association. 1991;265(16):2065–2066. [PubMed] [Google Scholar]
- Singh-Manoux A, Adler NE, Marmot MG. Subjective social status: its determinants and its association with measures of ill-health in the Whitehall II study. Social Science & Medicine. 2003;56:1321–1333. doi: 10.1016/s0277-9536(02)00131-4. [DOI] [PubMed] [Google Scholar]
- Takeuchi D, Hong S, Gile K, Alegría M. Developmental contexts and mental disorders among Asian Americans. Research in Human Development. 2007;4(1–2):49–69. doi: 10.1080/15427600701480998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takeuchi DT, Zane N, Hong S, et al. Immigration-related factors and mental disorders among Asian Americans. American Journal of Public Health. 2007;97:84–90. doi: 10.2105/AJPH.2006.088401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau . Census 2000, Summary File 3. U.S. Census Bureau; Washington, D.C.: 2003. [Google Scholar]
- Viruell-Fuentes EA. Beyond acculturation: immigration, discrimination, and health research among Mexicans in the United States. Social Science & Medicine. 2007;65(7):1524–1535. doi: 10.1016/j.socscimed.2007.05.010. [DOI] [PubMed] [Google Scholar]
- Wilkinson RG. Health, hierarchy, and social anxiety. In: Adler NE, Marmot M, McEwen BS, Stewart J, editors. Socioeconomic status and health in industrial nations: Social, psychological, and biological pathways. Annals of the New York Academy of Sciences; New York: 1999. pp. 48–63. [DOI] [PubMed] [Google Scholar]
- Williams DR. Race, socioeconomic status, and health: the added effects of racism and discrimination. In: Adler NE, Marmot M, McEwen BS, Stewart J, editors. Socioeconomic status and health in industrial nations: Social, psychological, and biological pathways. Annals of the New York Academy of Sciences; New York: 1999. pp. 173–188. [DOI] [PubMed] [Google Scholar]
- Williams DR, Collins C. U.S. socioeconomic and racial differences in health: patterns and explanations. Annual Review of Sociology. 1995;21:349–386. [Google Scholar]
- Williams DR, Haile R, Gonzalez HM, Neighbors H, Baser R, Jackson J. The mental health of black Caribbean immigrants: results from the National Survey of American Life. American Journal of Public Health. 2007;97:52–59. doi: 10.2105/AJPH.2006.088211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng Z, Xie Y. Asian-Americans’ earnings disadvantage reexamined: the role of place of education. The American Journal of Sociology. 2004;109:1075–1108. [Google Scholar]