Abstract
The effects of anti-inflammatory plant extracts, such as black tea extract (BTE) and resveratrol (RSV) could modulate cell activation leading to atherosclerosis, however there is little comparative information about how different endothelial cell types are affected by these compounds. In order to compare human endothelial cells derived from different origins (umbilical vein or HUVEC, coronary artery or HCAEC, microvascular or HMVEC) and their interleukin-1β (IL-1β) responsiveness, IL-6 ELISA, RT-PCR, tissue factor assay, and prostacyclin responses using 6-keto PGF1α ELISA were determined. The IL-1β-induced IL-6 levels were dose-dependent with highest responses seen in HCAEC. Significant inhibition of IL-1β responses was achieved with BTE and RSV, with the largest decrease of IL-6 and TF seen in HCAEC. Prostacyclin levels were highest in HUVEC and were inhibited by RSV in all cell types. The differences between the endothelial cell types could account for greater susceptibility of coronary arteries to inflammation and atherogenesis.
1. Introduction
Coronary artery disease, as an important manifestation of atherosclerosis, is one of the most frequent causes of death and disability in the Western world [1]. It has been proposed that inflammation is the driving force in atherosclerosis [2, 3], and strong evidence supports the central role of proinflammatory cytokines, such as interleukin-1β (IL-1β) and interleukin-6 (IL-6) in these pathologies. Human coronary artery endothelial cells (HCAEC) have previously been shown to have a strikingly greater responsiveness than human umbilical vein endothelial cells (HUVEC) [4].
The endothelium is considered a dynamic organ with secretory, metabolic, immunologic roles, in addition to its regulatory function of nutrient transport. Endothelial cells from diverse environments are heterogenous with respect to their surface phenotype, mRNA expression, and levels of IL-6 and procoagulant proteins, such as tissue factor (TF). Within the past decades, the majority of endothelial proinflammatory/coagulation studies have been performed on HUVEC, derived from a vascular bed not present in the adult, making these cells an inappropriate model of endothelial inflammation and coagulation [5, 6].
TF is a pivotal factor found associated with endothelial cells within atherosclerotic plaques [7] that can transform the endothelial cell membrane from an anticoagulant to a procoagulant surface following vascular injury [8]. Unique sensitivity of HCAEC to tumor necrosis factor α (TNFα)-stimulated expression of adhesion molecules (as compared to human aortic endothelial cells) [9] and greater susceptibility of HCAEC to inflammatory stimuli, (as compared to HUVEC and human dermal microvascular endothelial cells (HMVEC)) [4] have been reported. Endothelial cells contribute to homeostasis and vasodilation, also by releasing prostacyclin (PGI2) known to inhibit platelet aggregation and deposition [5]. However, no reports as far as we know, have addressed the comparative influence of IL-1β on PGI2 release, TF activity, or IL-6 protein release from HCAEC versus other endothelial cell types.
Previous epidemiological studies have suggested that black and green tea consumption may have beneficial effects on endothelial function and is associated with a decreased risk of cardiovascular events [10–13]. Black tea inhibited the proliferation of smooth muscle cells involved in the development and progression of atherosclerosis [14] and mechanisms for the beneficial effects of tea including vasculoprotective, antioxidative, antithrombogenic, anti-inflammatory, and lipid-lowering properties of tea flavonoids have been reported [11, 15–18]. Animal studies confirmed that black tea extract (BTE) has anti-inflammatory activity [15], however, its effects on different types of endothelial cells is still not clear.
The polyphenolic stilbene resveratrol (RSV) is found in grape skins, red wine, and peanuts [19, 20]. Trans -RSV has been shown to inhibit TF expression in vascular cells and to act anti-inflammatory [21–23]. RSV also attenuated TNFα-activated HCAEC through the NF-kB pathway [24]. However, it is still largely unknown how BTE and/or RSV affect IL-1β-stimulated inflammatory and coagulation pathways in HCAEC, as a novel model system, compared to HUVEC or other endothelial cell types.
So, our focus has been to elucidate the mechanisms that could modulate IL-1β proinflammatory/procoagulant responses in HCAEC. The specific objectives of this study were to understand the influence of potential anti-inflammatory plant extracts, such as BTE and RSV, on IL-1β-induced primary HCAEC and to compare their IL-6, TF, and prostacyclin responses with other types of endothelial cells.
2. Materials and Methods
2.1. Materials
Lyophilized human IL-1β (Invitrogen - Carlsbad, California, USA), resveratrol and extract from black tea (Sigma - Saint Louis, Missouri, USA) were reconstituted according to manufacturer's instructions to stock concentration and stored until usage at −20°C or −80°C. The black tea extract used in the current report is composed of more than 80% theaflavins (theaflavin and theaflavin gallates). The final concentration of IL-1β was 1000 pg/mL, resveratrol 40 μmol/L, and the final concentration of black tea extract was 40 μg/mL unless otherwise stated.
2.2. Cell Culture
HUVEC, HCAEC, and HMVEC were purchased from Cambrex BioScience (Walkesville, Maryland, USA). The cells were plated onto 12 or 6 well plates or 75 cm2 flasks (TPP, Trasadigen, Switzerland) at 37°C in a humidified atmosphere at 5% CO2. HCAEC and HMVEC were grown in EGM-2M medium (Cambrex BioScience, Walkesville, Maryland, USA) containing 5% fetal bovine serum; for HUVEC we used EGM medium containing 2% fetal bovine serum (Cambrex BioScience, Walkesville, Maryland, USA). For experiments, subconfluent cell cultures were used between 4 and 6 passages in serum-free medium with addition of stimulatory and/or modulatory substances for 24 hours, unless otherwise indicated. Prior to experiments, cells were incubated in serum-free media for 2 hours.
2.3. Measurement of Secreted Interleukin-6 and Prostacyclin Metabolite 6-Keto PGF1α
IL-6 from cell culture supernatants was measured and analyzed by human IL-6 ELISA from BioSource International (Camarillo, California, USA) according to manufacturer's instructions. Enzyme immunoassay (EIA) 6-keto PGF1α (Cayman diagnostica, Michigan, USA) was used to measure the concentration of nonenzymatically converted metabolite of prostacyclin or PGI2 in cell culture supernatants with competitive EIA according to the instructions of the manufacturer. 6-keto PGF1α is a stable product of PGI2.
2.4. RNA Isolation and Reverse Transcription Polymerase Chain Reaction (RT-PCR) Analysis
Before RT-PCR, total RNA from endothelial cell cultures was isolated using Total RNA Isolation System (Promega, USA) following manufacturer's instructions. The purity and amount of RNA were determined by measuring the OD at a ratio of 260 to 280 nm. 1 μg of total RNA were transcribed into DNA by Reverse Transcription System (Promega, USA) and PCR was performed for β-actin, IL-6, and TF (Table 1). β-actin was used as a control for normalization.
Table 1.
Primer sequences and PCR conditions.
| Primer sequences | Denat. t/T | Anneal. t/T | Extens. t/T | No. of cycles | |
|---|---|---|---|---|---|
| β-actin | sense 5′-ATC TGG CAC CAC ACC TTC TAC AAT GAG CTG CG–3′ | 1 min/94°C | 1 min/59°C | 1.5 min/72°C | 25 |
| antisense 5′-CGT CAT ACT CCT GCT TGC TGA TCC ACA TCT GC–3′ | |||||
|
| |||||
| IL-6 | sense 5′-ATG AAC TCC TTC TCC ACA AGC GC-3′ | 1 min/94°C | 1 min/51°C | 1.5 min/72°C | 30 |
| antisense 5′-GAA GAG CCC TCA GGC TGG ACT G-3′ | |||||
|
| |||||
| TF | sense 5′-ACT ACT GTT TCA GTG TTC AAG CAG TGA TTC-3′ | 1 min/94°C | 1 min/52°C | 1.5 min/72°C | 35 |
| antisense 5′-ATT CAG TGG GGA GTT CTC CTT CCC AGC TCTG-3′ | |||||
t/T: time and temperature, Denat.: denaturation, Anneal.: annealing, Extens.: extension.
2.5. Tissue Factor Activity Assay
Tissue factor activity was measured following the Actichrome TF (American diagnostica, Stamford, Connecticut, USA) procedure. After cell treatment in 12 well plates, the medium was removed and 150 μL/well of TBS/Triton X-100 buffer was added. Cells were then scraped and frozen at −80°C for 15 minutes and then thawed at 37°C. This freeze-thaw cycle was repeated twice. Subsequently, cells were kept at 37°C for another half an hour. Cell lysates were then mixed with Factor VIIa and Factor X in 96 well plates. Following a 15-minute incubation at 37°C, Spectrozyme FXa was added for 20 minutes and the reaction was stopped with glacial acetic acid. The absorbance at 405 nm was read on the Tecan Sunrise Colorimeter. The standard curve was constructed from provided standards and corresponding sample concentrations were calculated.
2.6. Statistical Analysis
All experiments were repeated three times and the mRNA expression studies were shown as 1 representative gel of two performed. Data are presented as a mean ± standard deviation (SD). Means were compared between the treated and control groups using Student's t-test. P values less than .05 were determined to be statistically significant.
3. Results
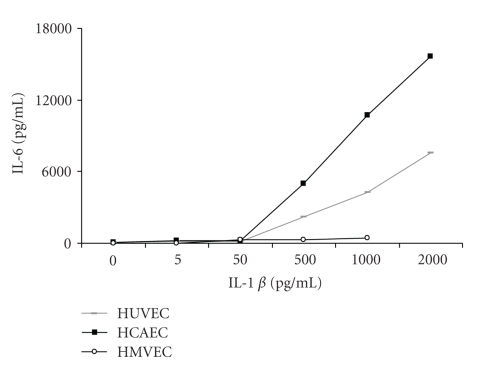
In order to determine the inflammatory/coagulation responses of primary human endothelial cells, in particular HCAEC, stimulated with different doses of IL-1β, we measured released IL-6 protein (Figure 1). Semiconfluent primary HUVEC, HCAEC, and HMVEC were incubated in 6-well plates with increasing doses of IL-1β (from 0 to 2000 pg/mL) for 24 hours in serum-free media. Released protein levels of IL-6 were measured in supernatants by ELISA, and in parallel, mRNA expressions of β-actin, IL-6, and TF were determined using RT-PCR. A comparison of released IL-6 protein levels in the endothelial cell types showed highest levels coming from HCAEC (approximately 2-fold higher than from HUVEC) and the lowest from HMVEC (Figure 1). The first rapidly increased IL-6 protein levels were seen at an IL-1β concentration of 500 pg/mL in HCAEC and HUVEC, in comparison to HMVEC where responses were consistently low. The mRNA expression results show that IL-6, as well as TF mRNA expression dose dependently increased with IL-1β in all cell types (data not shown).
Figure 1.
Dose dependent responses of HUVEC, HCAEC, and HMVEC to IL-1β (0–2000 pg/mL) as measured by ELISA of released IL-6 protein levels from cell supernatants. Results are expressed as a mean of three separate experiments.
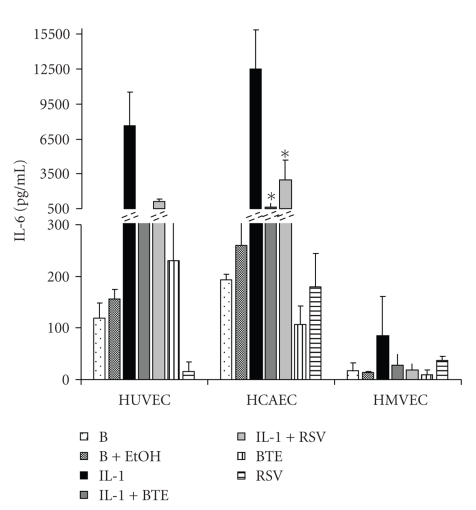
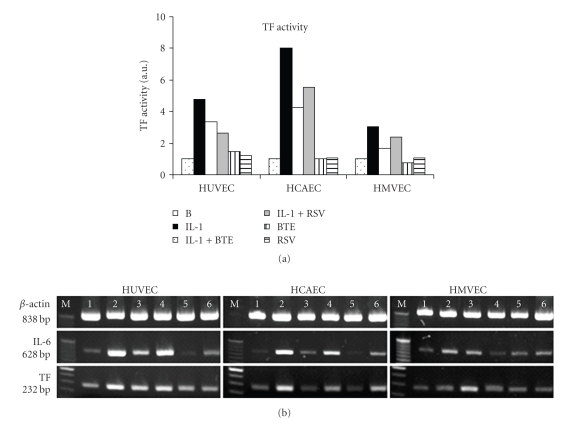
To investigate the effects of modulatory molecules on IL-1β-stimulated endothelial cells, we measured the IL-6 protein levels in the presence or absence of BTE and RSV. Both BTE and RSV significantly inhibited IL-6 protein levels of HCAEC (Figure 2). IL-1β-induced TF activity showed the highest response in HCAEC and was inhibited by BTE and RSV in all three endothelial cell types (Figure 3(a)). The IL-1β-induced mRNA expression of IL-6 and TF in all endothelial cell types is down-regulated with BTE and RSV (Figure 3(b)).
Figure 2.
Released IL-6 protein levels as measured by ELISA of supernatants from HUVEC, HCAEC, and HMVEC incubated with IL-1β (1000 pg/mL) for 24 hours in the absence or presence of BTE (40 μg/mL) and RSV (40 μM). Data represent the mean ± SD of three separate experiments. *P < .05 compared with IL-1β levels of expression.
Figure 3.
(a) TF activity was measured in the indicated treatments. Data are presented as arbitrary units, which indicate fold-change above background TF levels and were generated from the mean of three separate experiments. (b) mRNA expressions of β-actin, IL-6, and TF are shown from HUVEC, HCAEC, and HMVEC incubated with IL-1β (1000 pg/mL) in the absence or presence of BTE (40 μg/mL) and RSV (40 μM). The treatments of cell cultures were background control (lane 1), IL-1β 1000 pg/mL (lane 2), IL-1β + BTE (lane 3), IL-1β + RSV (lane 4), BTE (lane 5), and RSV (lane 6). Results shown are from one representative experiment of two separate ones performed.
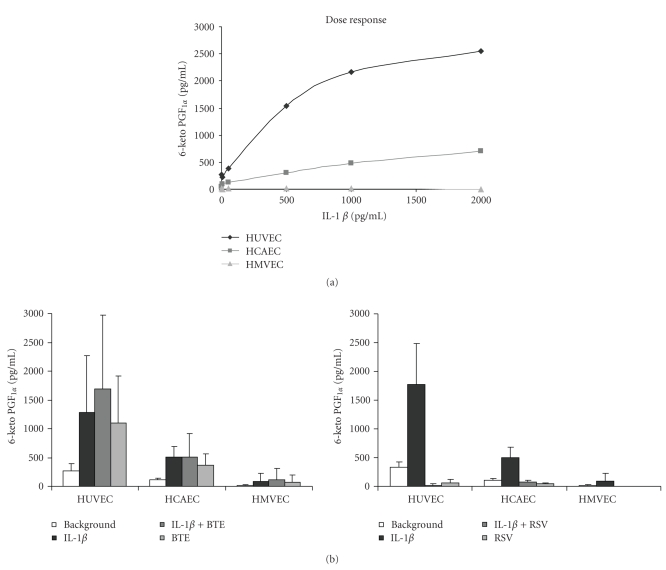
To investigate the effects of IL-1β on homeostasis of endothelial cells, released prostacyclin PGI2 was measured as 6-keto PGF1α in cell supernatants (Figure 4). To determine whether the responses were dose dependent, HCAEC, HUVEC, and HMVEC were incubated with increasing concentrations of IL-1β (Figure 4(a)). The highest responses were shown in HUVEC, which were around 3-4 fold higher than in HCAEC. PGF1α levels from IL-1β-stimulated HMVEC were below the detection limit. Contrary to IL-6 levels and TF activity, BTE addition did not cause inhibition of IL-1β-stimulated prostacyclin release (Figure 4(b), left panel). However, RSV abrogated IL-1β-induced 6-keto PGF1α levels in all three cell types (Figure 4(b), right panel).
Figure 4.
(a) IL-1β dose-dependent prostacyclin release, as measured by 6 keto-PGF1α, from HUVEC, HCAEC, and HMVEC. Concentrations of IL-1β were 0–2000 pg/mL. Data represent the mean of three separate experiments. (b) PGF1α levels measured in the indicated endothelial cell types treated with IL-1β (1000 pg/mL) and/or BTE (40 μg/mL) [left panel] or IL-1β (1000 pg/mL) and/or RSV (40 μM) [right panel]. Data represent the mean ± SD of three separate experiments.
4. Discussion
In this report, HCAEC were used as a model cell system, shown to be highly responsive to IL-1β-stimulated IL-6 released protein levels, TF activity, and inhibition of these by BTE and RSV. Studies on HCAEC reported in literature have looked at different stimulating molecules, such as IL-1α and TNFα, activated protein C, lipopolysaccharide [25–28], and their effects on different cytokine and chemokine expression, indicating unique cell type patterns and/or levels of expression.
Lakota et al. previously indicated that HCAEC display greater susceptibility to inflammation and potential atherogenesis than HUVEC or HMVEC [4]. This is in accord with IL-1β-stimulated HCAEC data indicated in this report. Among the most accessible natural substances used worldwide are black tea, green tea, and wine, which have been suggested to be important modulators of cardiovascular disease (CVD). Both black and green tea have shown acute beneficial effects on aortic stiffness and wave reflections, as reported by Vlachopoulos et al. [29]. Since aortic stiffness and wave reflections are markers of CVD and prognostic factors of cardiovascular risk, they are important parameters to be studied in healthy individuals [29]. Many epidemiological studies of flavonoid consumption however have been performed with mixed results. One possible explanation for the lack of cardiovascular protection in some of the studies is the difference in infusion time, stirring, leaf size, and measurements in plasma/whole blood changes, although different brands and addition of milk did not show significant variances [30]. However, flavonoids were reported to bind to protein, which causes variations in bioavailability and also results in changed biological activity especially in the case of binding to specific receptors and/or enzymes [31, 32]. However, overall, the evidence suggests that individuals with the highest flavonoid intake have modestly reduced risks for CVD (as reviewed in Vita JA, 2005 [33]). For tea, this conclusion is supported by a meta-analysis with 10 cohort studies and seven case-control studies included, which suggested an overall reduction in CVD risk of around 11% with consumption of 3 cups of tea per day [34]. A meta-analysis was also performed recently on the association between green or black tea consumption and the risk of stroke [35]. Data from 9 studies involving 4 378 strokes among 194 965 individuals were pooled. The authors conclude that although a randomized clinical trial would be necessary to confirm the effect, this meta-analysis suggests that regardless of their country of origin, individuals consuming 3 cups of tea per day had a 21% lower risk of ischemic stroke than those consuming less than 1 cup per day. In a large sample (6 597 subjects) of the elderly (over 65 years), Debette et al. reported for the first time that carotid plaques were less frequent with increasing tea consumption in women [36].
Usually 1 g of tea is used for 100 mL of infusion [30, 32]. In the process of manufacturing, the black tea leaf catechins are allowed to oxidize into theaflavins which give the black tea its characteristic colour and taste. The black tea flavonoid content accounts for 20%–30% catechins, 10% theaflavins and 50%–60% thearubigins [37], and both catechins as well as theaflavins have been shown to act as cardio-protectants in cardiomyocytes [38]. Thearubigins are poorly characterised and the bioavailability of theaflavins is poorly understood [37].
The present data in HUVEC, HCAEC, and HMVEC indicate that BTE significantly abrogates IL-1β-induced IL-6 protein released levels similarly to RSV (Figure 2), while also decreasing both TF activity levels and expression (Figure 3). However, BTE does not seem to have any effects on IL-1β-induced PGI2 in any of the three cell types (Figure 4(b), left panel). These differences imply that cytokine-specific processes and differential signaling pathways might be involved. Since black tea consumption has been previously associated with a decreased risk of cardiovascular events [10, 11], signaling events in response to BTE are relevant. Bovine aortic endothelial cells when exposed to BTE showed eNOS activity mediated through p38 MAPK and estrogen receptors leading to phosphatidylinositol 3-kinase/Akt pathway and eNOS generation [39, 40] and vasorelaxation of aortic rat rings [40].
RSV-mediated cardio-protection is achieved through the preconditioning effect and thus achieves a number of cardio-protective functions (reviewed in [19]), such as effecting release and/or generation of inflammatory mediators and attenuation of various soluble intercellular cytokines. RSV functions in scavenging free radicals and inhibiting lipid peroxidation, up-regulation of inducible NO synthase, vascular endothelial growth factor, kinase insert domain-containing receptor, and endothelial NO synthase. Adenosine receptors also have an important function in the RSV preconditioning.
Dealcoholized wine (1 cup) delivered in a single oral dose to healthy subjects less than 40 years old was found to increase endothelium-dependent vasodilation [41]. The authors indicate that this adds support to the hypothesis that antioxidant properties of red wine, rather than ethanol, may protect against cardiovascular diseases, however more research is needed on subjects with coronary heart disease. Usually the concentrations of RSV in cellular models of CVD protection are 0.1–100 μmol/ L [42], although some studies showed different effects in low/high doses in enhancing proliferation and inducing apoptosis [43].
When RSV in humans is absorbed around 75% is excreted via feces and urine. Serum levels were independent from meals and its lipid content [44], but RSV is rapidly metabolized into glucuronides and sulfates [20], which stay in the blood for 9 hours [45]. Biologic activity of metabolites was not elucidated yet [20, 42], and it is suggested that prolonged administration could lead to increased concentrations [42, 46]. It is necessary to apply caution when interpreting the literature data translating concentrations of RSV on potential cardiovascular effects.
To our knowledge, this is the first report to show the effects of RSV on IL-1β-induced IL-6 and TF responses in HCAEC, which could serve in cardioprotective processes similar to the ones described previously [24, 42, 47, 48]. RSV has been shown to inhibit TF (at 5–100 μmol/L) in HUVEC [21] at comparable concentrations to the 40 μM used in the present report, to reduce expression of adhesion molecules on stimulated human saphenus vein endothelial cells [49], to inhibit adhesion of activated platelets to collagen or fibrinogen [50] and lower ICAM, VCAM [24, 51]. RSV was also reported to enhance the inhibitory activity of PGI2 on platelet aggregation in low doses [52], as well as to inhibit TNFα-induced NAD(P)H oxidase and NF-κB activation and inflammatory markers (at 0.1–10 μmol/L) [24, 42, 51], similarly to our results. In porcine coronary arteries, short term treatment with RSV significantly inhibited MAPK activities, with reduced phosphorylation seen of ERK1/2, JNK-1 and p38 MAPK [53, 54], and STAT3 phosphorylation [55]. RSV was also found to inhibit protein kinase C in 2 μM concentration [56].
The data shown in HUVEC (Figure 4) indicates a similar level of IL-1β-stimulated PGI2 (measured using 6-keto PGF1 α) as shown by Olszanecki et al. [57]. All three cell types HUVEC, HCAEC, and HMVEC indicate a similar vasoregulatory role for IL-1β, while RSV addition abrogated PGI2 levels (Figure 4(b), right panel).
RSV has also been shown to decrease the expression of vasoconstrictor endothelin and increase eNOS in HUVEC, which might counterbalance PGI2 inhibition [58] and decrease NAD(P)H oxidase activity [59].
In conclusion, a growing body of evidence indicates that inflammation not only provides the baseline for future atherosclerotic events, but is a necessity for coronary plaque formation and coagulation leading to thrombosis. The unique responsiveness of HCAEC could account for the greater susceptibility of coronary arteries to inflammation and atherogenesis leading to cardiovascular pathology and substances, such as BTE and RSV, also influence these effects at the cellular level.
Acknowledgments
The authors would like to thank Natasa Pisek and Luka Oman for their technical contribution to the data. The work was supported by Ministry of High Education, Science and Technology of the Republic of Slovenia, Grant no. P3 0314 to Rozman Blaz and by the Marie Curie International Reintegration Grant MC-IRG 28414 to Sodin-Semrl Snezna. No conflicts of interest are reported.
References
- 1.Woods A, Brull DJ, Humphries SE, Montgomery HE. Genetics of inflammation and risk of coronary artery disease: the central role of interleukin-6. European Heart Journal. 2000;21(19):1574–1583. doi: 10.1053/euhj.1999.2207. [DOI] [PubMed] [Google Scholar]
- 2.Ross R. Atherosclerosis—an inflammatory disease. New England Journal of Medicine. 1999;340(2):115–126. doi: 10.1056/NEJM199901143400207. [DOI] [PubMed] [Google Scholar]
- 3.Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. New England Journal of Medicine. 2005;352(16):1685–1695. doi: 10.1056/NEJMra043430. [DOI] [PubMed] [Google Scholar]
- 4.Lakota K, Mrak-Poljsak K, Rozman B, Kveder T, Tomsic M, Sodin-Semrl S. Serum amyloid A activation of inflammatory and adhesion molecules in human coronary artery and umbilical vein endothelial cells. European Journal of Inflammation. 2007;5(2):73–81. [Google Scholar]
- 5.Cines DB, Pollak ES, Buck CA, et al. Endothelial cells in physiology and in the pathophysiology of vascular disorders. Blood. 1998;91(10):3527–3561. [PubMed] [Google Scholar]
- 6.Stoltz JF, Muller S, Kadi A, Decot V, Menu P, Bensoussan D. Introduction to endothelial cell biology. Clinical Hemorheology and Microcirculation. 2007;37(1-2):5–8. [PubMed] [Google Scholar]
- 7.Hatakeyama K, Asada Y, Marutsuka K, Sato Y, Kamikubo Y, Sumiyoshi A. Localization and activity of tissue factor in human aortic atherosclerotic lesions. Atherosclerosis. 1997;133(2):213–219. doi: 10.1016/s0021-9150(97)00132-9. [DOI] [PubMed] [Google Scholar]
- 8.Marmur JD, Rossikhina M, Guha A, et al. Tissue factor is rapidly induced in arterial smooth muscle after balloon injury. Journal of Clinical Investigation. 1993;91(5):2253–2259. doi: 10.1172/JCI116452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McDouall RM, Farrar MW, Khan S, Yacoub MH, Allen SP. Unique sensitivities to cytokine regulated expression of adhesion molecules in human heart-derived endothelial cells. Endothelium. 2001;8(1):25–40. doi: 10.3109/10623320109063155. [DOI] [PubMed] [Google Scholar]
- 10.Duffy SJ, Keaney JF, Jr., Holbrook M, et al. Short- and long-term black tea consumption reverses endothelial dysfunction in patients with coronary artery disease. Circulation. 2001;104(2):151–156. doi: 10.1161/01.cir.104.2.151. [DOI] [PubMed] [Google Scholar]
- 11.Stangl V, Lorenz M, Stangl K. The role of tea and tea flavonoids in cardiovascular health. Molecular Nutrition and Food Research. 2006;50(2):218–228. doi: 10.1002/mnfr.200500118. [DOI] [PubMed] [Google Scholar]
- 12.Alexopoulos N, Vlachopoulos C, Aznaouridis K, et al. The acute effect of green tea consumption on endothelial function in healthy individuals. European Journal of Cardiovascular Prevention and Rehabilitation. 2008;15(3):300–305. doi: 10.1097/HJR.0b013e3282f4832f. [DOI] [PubMed] [Google Scholar]
- 13.Ardalan MR, Tarzamni MK, Shoja MM, et al. Black tea improves endothelial function in renal transplant recipients. Transplantation Proceedings. 2007;39(4):1139–1142. doi: 10.1016/j.transproceed.2007.04.010. [DOI] [PubMed] [Google Scholar]
- 14.Yokozawa T, Dong E, Nakagawa T, Kim DW, Hattori M, Nakagawa H. Effects of Japanese black tea on atherosclerotic disorders. Bioscience, Biotechnology and Biochemistry. 1998;62(1):44–48. doi: 10.1271/bbb.62.44. [DOI] [PubMed] [Google Scholar]
- 15.Nag Chaudhuri AK, Karmakar S, Roy D, Pal S, Pal M, Sen T. Anti-inflammatory activity of Indian black tea (Sikkim variety) Pharmacological Research. 2005;51(2):169–175. doi: 10.1016/j.phrs.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 16.Lorenz M, Urban J, Engelhardt U, Baumann G, Stangl K, Stangl V. Green and black tea are equally potent stimuli of NO production and vasodilation: new insights into tea ingredients involved. Basic Research in Cardiology. 2009;104(1):100–110. doi: 10.1007/s00395-008-0759-3. [DOI] [PubMed] [Google Scholar]
- 17.Lü H, Hua P, Yu J, Jiang X, Leng H. Study on the effect of theaflavins on the adhesion between monocyte and endothelial cells. Zhong Yao Cai. 2005;28(4):304–306. [PubMed] [Google Scholar]
- 18.Yoshida H, Ishikawa T, Hosoai H, et al. Inhibitory effect of tea flavonoids on the ability of cells to oxidize low density lipoprotein. Biochemical Pharmacology. 1999;58(11):1695–1703. doi: 10.1016/s0006-2952(99)00256-7. [DOI] [PubMed] [Google Scholar]
- 19.Das S, Santani DD, Dhalla NS. Experimental evidence for the cardioprotective effects of red wine. Experimental and Clinical Cardiology. 2007;12(1):5–10. [PMC free article] [PubMed] [Google Scholar]
- 20.Wenzel E, Somoza V. Metabolism and bioavailability of trans-resveratrol. Molecular Nutrition and Food Research. 2005;49(5):472–481. doi: 10.1002/mnfr.200500010. [DOI] [PubMed] [Google Scholar]
- 21.Pendurthi UR, Williams JT, Rao LVM. Resveratrol, a polyphenolic compound found in wine, inhibits tissue factor expression in vascular cells: a possible mechanism for the cardiovascular benefits associated with moderate consumption of wine. Arteriosclerosis, Thrombosis, and Vascular Biology. 1999;19(2):419–426. doi: 10.1161/01.atv.19.2.419. [DOI] [PubMed] [Google Scholar]
- 22.Manna SK, Mukhopadhyay A, Aggarwal BB. Resveratrol suppresses TNF-induced activation of nuclear transcription factors NF-κB, activator protein-1, and apoptosis: potential role of reactive oxygen intermediates and lipid peroxidation. Journal of Immunology. 2000;164(12):6509–6519. doi: 10.4049/jimmunol.164.12.6509. [DOI] [PubMed] [Google Scholar]
- 23.Takada Y, Bhardwaj A, Potdar P, Aggarwal BB. Nonsteroidal anti-inflammatory agents differ in their ability to suppress NF-κB activation, inhibition of expression of cyclooxygenase-2 and cyclin D1, and abrogation of tumor cell proliferation. Oncogene. 2004;23(57):9247–9258. doi: 10.1038/sj.onc.1208169. [DOI] [PubMed] [Google Scholar]
- 24.Csiszar A, Smith K, Labinskyy N, Orosz Z, Rivera A, Ungvari Z. Resveratrol attenuates TNF-α-induced activation of coronary arterial endothelial cells: role of NF-κB inhibition. American Journal of Physiology. 2006;291(4):H1694–H1699. doi: 10.1152/ajpheart.00340.2006. [DOI] [PubMed] [Google Scholar]
- 25.Briones MA, Phillips DJ, Renshaw MA, Hooper WC. Expression of chemokine by human coronary-artery and umbilical-vein endothelial cells and its regulation by inflammatory cytokines. Coronary Artery Disease. 2001;12(3):179–186. doi: 10.1097/00019501-200105000-00004. [DOI] [PubMed] [Google Scholar]
- 26.Hooper WC, Phillips DJ, Renshaw MA, Evatt BL, Benson JM. The up-regulation of IL-6 and IL-8 in human endothelial cells by activated protein C. Journal of Immunology. 1998;161(5):2567–2573. [PubMed] [Google Scholar]
- 27.Franscini N, Bachli EB, Blau N, Leikauf M-S, Schaffner A, Schoedon G. Gene expression profiling of inflamed human endothelial cells and influence of activated protein C. Circulation. 2004;110(18):2903–2909. doi: 10.1161/01.CIR.0000146344.49689.BB. [DOI] [PubMed] [Google Scholar]
- 28.Zeuke S, Ulmer AJ, Kusumoto S, Katus HA, Heine H. TLR4-mediated inflammatory activation of human coronary artery endothelial cells by LPS. Cardiovascular Research. 2002;56(1):126–134. doi: 10.1016/s0008-6363(02)00512-6. [DOI] [PubMed] [Google Scholar]
- 29.Vlachopoulos C, Alexopoulos N, Dima I, Aznaouridis K, Andreadou I, Stefanadis C. Acute effect of black and green tea on aortic stiffness and wave reflections. Journal of the American College of Nutrition. 2006;25(3):216–223. doi: 10.1080/07315724.2006.10719535. [DOI] [PubMed] [Google Scholar]
- 30.Kyle JAM, Morrice PC, McNeill G, Duthie GG. Effects of infusion time and addition of milk on content and absorption of polyphenols from black tea. Journal of Agricultural and Food Chemistry. 2007;55(12):4889–4894. doi: 10.1021/jf070351y. [DOI] [PubMed] [Google Scholar]
- 31.Hasalam E. Plant Phenols: Vegetable Tannins Revisited. Cambridge, UK: Cambrige University Press; 1989. [Google Scholar]
- 32.Yang CS, Chung JY, Yang G-Y, Chhabra SK, Lee M-J. Tea and tea polyphenols in cancer prevention. Journal of Nutrition. 2000;130(2, supplement):472S–478S. doi: 10.1093/jn/130.2.472S. [DOI] [PubMed] [Google Scholar]
- 33.Vita JA. Polyphenols and cardiovascular disease: effects on endothelial and platelet function. The American Journal of Clinical Nutrition. 2005;81(1, supplement):292S–297S. doi: 10.1093/ajcn/81.1.292S. [DOI] [PubMed] [Google Scholar]
- 34.Peters U, Poole C, Arab L. Does tea affect cardiovascular disease? A meta-analysis. American Journal of Epidemiology. 2001;154(6):495–503. doi: 10.1093/aje/154.6.495. [DOI] [PubMed] [Google Scholar]
- 35.Arab L, Liu W, Elashoff D. Green and black tea consumption and risk of stroke: a meta-analysis. Stroke. 2009;40(5):1786–1792. doi: 10.1161/STROKEAHA.108.538470. [DOI] [PubMed] [Google Scholar]
- 36.Debette S, Courbon D, Leone N, et al. Tea consumption is inversely associated with carotid plaques in women. Arteriosclerosis, Thrombosis, and Vascular Biology. 2008;28(2):353–359. doi: 10.1161/ATVBAHA.107.151928. [DOI] [PubMed] [Google Scholar]
- 37.Riemersma RA, Rice-Evans CA, Tyrrell RM, Clifford MN, Lean MEJ. Tea flavonoids and cardiovascular health. QJM. 2001;94(5):277–282. doi: 10.1093/qjmed/94.5.277. [DOI] [PubMed] [Google Scholar]
- 38.Dreger H, Lorenz M, Kehrer A, Baumann G, Stangl K, Stangl V. Characteristics of catechin- and theaflavin-mediated cardioprotection. Experimental Biology and Medicine. 2008;233(4):427–433. doi: 10.3181/0710-RM-292. [DOI] [PubMed] [Google Scholar]
- 39.Anter E, Chen K, Shapira OM, Karas RH, Keaney JF., Jr. p38 mitogen-activated protein kinase activates eNOS in endothelial cells by an estrogen receptor α-dependent pathway in response to black tea polyphenols. Circulation Research. 2005;96(10):1072–1078. doi: 10.1161/01.RES.0000168807.63013.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lorenz M, Urban J, Engelhardt U, Baumann G, Stangl K, Stangl V. Green and black tea are equally potent stimuli of NO production and vasodilation: new insights into tea ingredients involved. Basic Research in Cardiology. 2009;104(1):100–110. doi: 10.1007/s00395-008-0759-3. [DOI] [PubMed] [Google Scholar]
- 41.Agewall S, Wright S, Doughty RN, Whalley GA, Duxbury M, Sharpe N. Does a glass of red wine improve endothelial function? European Heart Journal. 2000;21(1):74–78. doi: 10.1053/euhj.1999.1759. [DOI] [PubMed] [Google Scholar]
- 42.Opie LH, Lecour S. The red wine hypothesis: from concepts to protective signalling molecules. European Heart Journal. 2007;28(14):1683–1693. doi: 10.1093/eurheartj/ehm149. [DOI] [PubMed] [Google Scholar]
- 43.Szende B, Tyihák E, Király-Véghely Z. Dose-dependent effect of resveratrol on proliferation and apoptosis in endothelial and tumor cell cultures. Experimental and Molecular Medicine. 2000;32(2):88–92. doi: 10.1038/emm.2000.16. [DOI] [PubMed] [Google Scholar]
- 44.Vitaglione P, Sforza S, Galaverna G, et al. Bioavailability of trans-resveratrol from red wine in humans. Molecular Nutrition and Food Research. 2005;49(5):495–504. doi: 10.1002/mnfr.200500002. [DOI] [PubMed] [Google Scholar]
- 45.Saiko P, Szakmary A, Jaeger W, Szekeres T. Resveratrol and its analogs: defense against cancer, coronary disease and neurodegenerative maladies or just a fad? Mutation Research. 2008;658(1-2):68–94. doi: 10.1016/j.mrrev.2007.08.004. [DOI] [PubMed] [Google Scholar]
- 46.Bertelli AAE, Giovannini L, Stradi R, Bertelli A, Tillement J-P. Plasma, urine and tissue levels of trans- and cis-resveratrol (3,4′,5-trihydroxystilbene) after short-term or prolonged administration of red wine to rats. International Journal of Tissue Reactions. 1996;18(2-3):67–71. [PubMed] [Google Scholar]
- 47.Pellegatta F, Bertelli AAE, Staels B, Duhem C, Fulgenzi A, Ferrero ME. Different short- and long-term effects of resveratrol on nuclear factor-κB phosphorylation and nuclear appearance in human endothelial cells. American Journal of Clinical Nutrition. 2003;77(5):1220–1228. doi: 10.1093/ajcn/77.5.1220. [DOI] [PubMed] [Google Scholar]
- 48.Das DK, Maulik N. Resveratrol in cardioprotection: a therapeutic promise of alternative medicine. Molecular Interventions. 2006;6(1):36–47. doi: 10.1124/mi.6.1.7. [DOI] [PubMed] [Google Scholar]
- 49.Ferrero ME, Bertelli AAE, Fulgenzi A, et al. Activity in vitro of resveratrol on granulocyte and monocyte adhesion to endothelium. American Journal of Clinical Nutrition. 1998;68(6):1208–1214. doi: 10.1093/ajcn/68.6.1208. [DOI] [PubMed] [Google Scholar]
- 50.Olas B, Wachowicz B, Saluk-Juszczak J, Zieliński T. Effect of resveratrol, a natural polyphenolic compound, on platelet activation induced by endotoxin or thrombin. Thrombosis Research. 2002;107(3-4):141–145. doi: 10.1016/s0049-3848(02)00273-6. [DOI] [PubMed] [Google Scholar]
- 51.Park H-J, Jeong S-K, Kim S-R, et al. Resveratrol inhibits Porphyromonas gingivalis lipopolysaccharide-induced endothelial adhesion molecule expression by suppressing NF-κB activation. Archives of Pharmacal Research. 2009;32(4):583–591. doi: 10.1007/s12272-009-1415-7. [DOI] [PubMed] [Google Scholar]
- 52.Wu C-C, Wu C-I, Wang W-Y, Wu Y-C. Low concentrations of resveratrol potentiate the antiplatelet effect of prostaglandins. Planta Medica. 2007;73(5):439–443. doi: 10.1055/s-2007-967173. [DOI] [PubMed] [Google Scholar]
- 53.El-Mowafy AM, White RE. Resveratrol inhibits MAPK activity and nuclear translocation in coronary artery smooth muscle: reversal of endothelin-1 stimulatory effects. FEBS Letters. 1999;451(1):63–67. doi: 10.1016/s0014-5793(99)00541-4. [DOI] [PubMed] [Google Scholar]
- 54.Kang O-H, Jang H-J, Chae H-S, et al. Anti-inflammatory mechanisms of resveratrol in activated HMC-1 cells: pivotal roles of NF-κB and MAPK. Pharmacological Research. 2009;59(5):330–337. doi: 10.1016/j.phrs.2009.01.009. [DOI] [PubMed] [Google Scholar]
- 55.Wung BS, Hsu MC, Wu CC, Hsieh CW. Resveratrol suppresses IL-6-induced ICAM-1 gene expression in endothelial cells: effects on the inhibition of STAT3 phosphorylation. Life Sciences. 2005;78(4):389–397. doi: 10.1016/j.lfs.2005.04.052. [DOI] [PubMed] [Google Scholar]
- 56.Slater SJ, Seiz JL, Cook AC, Stagliano BA, Buzas CJ. Inhibition of protein kinase C by resveratrol. Biochimica et Biophysica Acta. 2003;1637(1):59–69. doi: 10.1016/s0925-4439(02)00214-4. [DOI] [PubMed] [Google Scholar]
- 57.Olszanecki R, Gebska A, Korbut R. Production of prostacyclin and prostaglandin E2 in resting and IL-1β-stimulated A549, HUVEC and hybrid EA.hy 926 cells. Journal of Physiology and Pharmacology. 2006;57(4):649–660. [PubMed] [Google Scholar]
- 58.Nicholson SK, Tucker GA, Brameld JM. Effects of dietary polyphenols on gene expression in human vascular endothelial cells. Proceedings of the Nutrition Society. 2008;67(1):42–47. doi: 10.1017/S0029665108006009. [DOI] [PubMed] [Google Scholar]
- 59.Orallo F, Alvarez E, Camiña M, Leiro JM, Gómez E, Fernandez P. The possible implication of trans-Resveratrol in the cardioprotective effects of long-term moderate wine consumption. Molecular Pharmacology. 2002;61(2):294–302. doi: 10.1124/mol.61.2.294. [DOI] [PubMed] [Google Scholar]