Abstract
Many cancer immunotherapies developed in experimental animals have been tested in clinical trials. Although some have shown modest clinical effects, most have not been effective. Recent studies have identified myeloid-origin cells that are potent suppressors of tumor immunity and therefore a significant impediment to cancer immunotherapy. “Myeloid-derived suppressor cells” (MDSC) accumulate in the blood, lymph nodes, and bone marrow and at tumor sites in most patients and experimental animals with cancer and inhibit both adaptive and innate immunity. MDSC are induced by tumor-secreted and host-secreted factors, many of which are proinflammatory molecules. The induction of MDSC by proinflammatory mediators led to the hypothesis that inflammation promotes the accumulation of MDSC that down-regulate immune surveillance and antitumor immunity, thereby facilitating tumor growth. This article reviews the characterization and suppressive mechanisms used by MDSC to block tumor immunity and describes the mechanisms by which inflammation promotes tumor progression through the induction of MDSC.
The concept that chronic inflammation contributes to tumor initiation and progression was proposed by the German pathologist Rudolf Virchow over 140 years ago (1). Although his hypothesis was overlooked for many years, abundant epidemiological data show a strong correlation between inflammation and cancer incidence. For example, mesothelioma, lung, prostate, bladder, pancreatic, cervical, esophageal, melanoma, and head and neck cancers are frequently associated with long-term inflammation, whereas gall bladder, liver, ovarian, colorectal, and bladder cancers are associated with specific infectious agents (2–4). Additional evidence linking inflammation and cancer comes from studies demonstrating that long-term users of nonsteroidal anti-inflammatory drugs, including aspirin, are at a significantly lower risk of developing colorectal (5), lung, stomach, esophageal (6), and breast (4) cancers. There is also experimental data supporting a causative relationship between chronic inflammation and cancer onset and progression. For example, blocking inflammatory mediators or signaling pathways regulating inflammation reduces tumor incidence and delays tumor growth, while heightened levels of proinflammatory mediators or adoptive transfer of inflammatory cells increases tumor development (4). These findings have renewed interest in Virchow’s hypothesis and have led to studies aimed at clarifying the mechanisms responsible for the association.
Chronic inflammation promotes tumor onset and development through nonimmune and immune mechanisms. The nonimmune mechanisms include the following: 1) the production of reactive oxygen species (ROS)3 such as peroxynitrites, which cause DNA mutations that contribute to genetic instability and the proliferation of malignant cells (2); 2) the production of proangiogenic factors such as vascular endothelial growth factor (VEGF), which promote tumor neovascularization (7); and 3) the production of matrix metalloproteases, which facilitate invasion and metastasis (8). The predominant immune mechanism is the perturbation of myelopoiesis and hemopoiesis, which causes a deficiency in Ag-presenting dendritic cells (DC) and dysfunctional cell-mediated antitumor immunity (9). A major culprit in this latter deficiency is the production of myeloid-derived suppressor cells (MDSC), an immature population of myeloid cells that is present in most cancer patients and mice with transplanted or spontaneous tumors. Because MDSC inhibit both innate and adaptive immunity, they are likely to subvert immune surveillance and prevent an individual’s immune system from eliminating newly transformed cells. In individuals with established cancer, they are likely to be a major factor in preventing the efficacy of immunotherapies, such as cancer vaccines, that require an immunocompetent host (10).
MDSC are present in most patients and experimental animals with cancer
Nonlymphoid hematopoietic suppressor cells were first identified >20 years ago and were called “natural suppressor” cells (11). However, their etiology as myeloid cells and their accumulation and suppressive function in individuals with cancer was not recognized until 10 years later, when excessive numbers of CD34+ myeloid cells were noted in the blood of patients with head and neck squamous cell carcinoma (12, 13) and in mice with lung tumors (14). Subsequent studies characterized MDSC as immature myeloid cells that are precursors of DC, macrophages, and/or granulocytes. Their accumulation has been documented in most patients (15, 16) and mice (17) with cancer, where they are induced by various factors produced by tumor cells and/or by host cells in the tumor microenvironment (9, 18). They also accumulate in response to bacterial (19, 20) and parasitic infection (21), chemotherapy (22), experimentally induced autoimmunity (23, 24), and stress (25). MDSC are considered a major contributor to the profound immune dysfunction of most patients with sizable tumor burdens (26).
In tumor-bearing mice MDSC accumulate in the bone marrow, spleen, and peripheral blood, within primary and meta-static solid tumors, and to a lesser extent in lymph nodes (18, 19, 27–29). In cancer patients they are present in the blood (15, 16, 30 –33), and it is not known whether they are present in other sites. In both patients and experimental animals MDSC levels are driven by tumor burden and by the diversity of factors produced by the tumor and by host cells in the tumor microenvironment.
MDSC are a heterogeneous family of myeloid cells
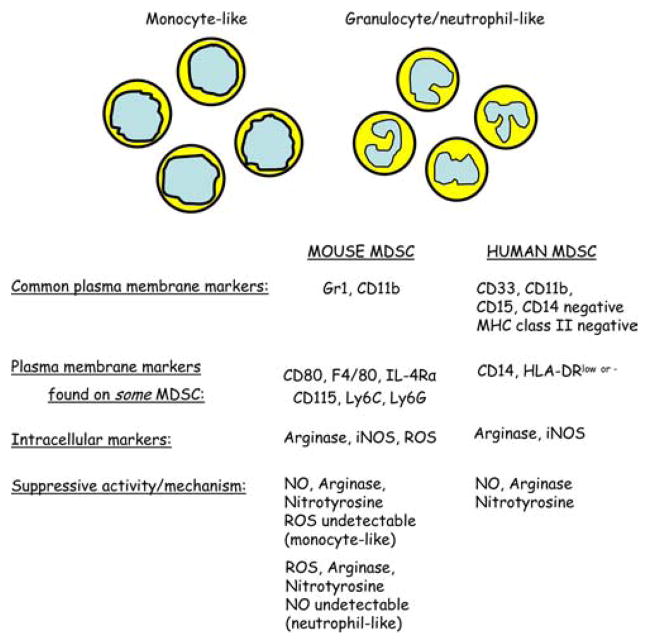
MDSC have been identified in most patients and experimental mice with tumors based on their ability to suppress T cell activation. In mice, MDSC are uniformly characterized by the expression of the cell surface molecules detected by Abs to Gr1 and CD11b. Gr1 includes the macrophage and neutrophil markers Ly6C and Ly6G, respectively, whereas CD11b is characteristic of macrophages. The α-chain of the receptor for IL-4 and IL-13 (IL-4Rα) (34, 35), another macrophage marker (F4/80) (34, 36, 37), M-CSF-1R or c-fms (CD115) (37), and the costimulatory molecule CD80 (B7.1) (38) have also been described on some subsets of MDSC. Similarly, Ly6C and Ly6G have individually been ascribed to MDSC (36, 39, 40). Because the expression of these later markers is restricted to Gr1+CD11b+ suppressive cells induced by only a subset of tumors, aside from Gr1 and CD11b, there are no unambiguous cell surface markers that define all mouse MDSC populations.
The nuclear morphology and content of immunosuppressive substances have also been used to characterize mouse MDSC. MDSC that are mononuclear are considered “monocytic” and typically are CD11b+Ly6G+/−Ly6Chigh, whereas those with multilobed nuclei are “granulocytic/neutrophil-like” and have a CD11b+Ly6G+Ly6Clow phenotype (39–41). MDSC also vary in their content of immunosuppressive substances, with different populations containing arginase (42–44), inducible NO synthase (45), and/or additional ROS (45, 46).
In cancer patients MDSC are typically CD11b+CD33+CD34+CD14−HLA-DR− and can vary in their expression of CD15 and other markers (30, 33, 47, 48). A new population of MDSC was recently identified in melanoma and hepatocarcinoma patients that is CD14+HLA-DR−/low, suggesting that, similarly as tumors in mice, different human tumors are likely to induce different subtypes of MDSC (30, 49).
The variation in MDSC phenotype is consistent with the concept that MDSC are a diverse family of cells that are in various intermediate stages of myeloid cell differentiation. MDSC are driven by tumor-secreted factors, and different tumors secrete different combinations of molecules. Therefore, MDSC phenotype will depend on the specific combination of factors within the tumor host. Because the myeloid population contains many different cell types and myeloid cell differentiation is a continuum of processes, MDSC may display diverse phenotypic markers that reflect the spectrum of immature to mature myeloid cells. This heterogeneity suggests that there may be no unique marker or combination of phenotypic markers that precisely defines MDSC, and that suppressive activity is the ultimate defining characteristic. It is also likely that, as this population of cells is further studied, additional subpopulations and markers will be identified.
Whether tumor-induced MDSC are normal cells halted in the intermediate stages of differentiation or whether they have diverged from the normal myeloid differentiation pathway and accumulated mutations is unclear. Direct comparisons of in vitro suppressive activity of splenic Gr1+CD11b+ cells from tumor-free mice vs tumor-bearing mice are not consistent. Most reports indicate that Gr1+CD11b+ cells from tumor-free mice are not suppressive (21, 38, 41, 42, 50), although one study demonstrated that, on a per cell basis, Gr1+CD11b+ cells from tumor-bearing mice and tumor-free mice were equally suppressive (51). These studies used Gr1+CD11b+ cells from tumor-free mice from different locales (blood, spleen, and the peritoneal cavity) and from different mouse strains, so the contradictory findings could be due to heterogeneity in the Gr1+CD11b+ population or to differences between mouse strains. Experiments demonstrating that treatment with all-trans retinoic acid converts MDSC from tumor-bearing mice to DC (47, 52) supports the concept that MDSC are normal intermediaries. If this is the case, then MDSC may play a role in normal homeostasis and the maintenance of tolerance to self-Ags. Additional experiments are clearly needed to clarify this point.
Fig. 1 shows the heterogeneity of mouse and human MDSC with respect to cell surface and internal markers and morphology.
FIGURE 1.
Mouse and human MDSC are heterogeneous populations of immature myeloid cells. Subpopulations of MDSC display different constellations of cell surface and intracellular markers and suppress by different mechanisms. This diversity is likely due to different combinations of factors produced by histologically distinct tumors that cause myeloid cells to arrest at different stages of differentiation.
MDSC suppress multiple immune effectors
MDSC suppress immunity by perturbing both innate and adaptive immune responses. Initial reports demonstrated that MDSC from head and neck cancer patients blocked IL-2 production of anti-CD3-activated intratumoral T cells. These results have been confirmed in patients with a variety of cancers (15, 16). Subsequent studies with mouse MDSC demonstrated that MDSC also block the activation and proliferation of transgenic CD8+ (51, 53–55) and CD4+ (51, 56) T cells cocultured with their cognate Ag. The suppressive activity of MDSC for T cells requires cell-to-cell contact and can be Ag-specific or non-specific and may depend on the MDSC subpopulation. Mouse MDSC suppression of CD8+ T cells has been shown to be MHC restricted and Ag specific (57). However, mouse MDSC also suppress MHC allogeneic, Ag-activated CD4+ T cells, indicating that suppression is also nonspecific (51, 58). Because studies with human MDSC use the blocking of anti-CD3 activation as a measure of suppressive activity, it is not clear whether human MDSC mediate Ag-specific suppression.
Multiple lines of evidence indicate that MDSC are potent inhibitors of antitumor immunity in vivo. Treatments that reduce MDSC levels such as Ab depletion of Gr1+ cells (59), treatment with the chemotherapeutic drug gemcitabine (60, 61) or retinoic acid (47, 52), or the debulking of tumors (51, 58) restore immune surveillance (59), activate T (62) and NK cells (63), and improve the efficacy of cancer vaccines or other immunotherapies in vivo (47, 52, 60, 64). In vivo inactivation of genes that govern MDSC accumulation, such as the STAT3 and STAT6 genes (51, 59, 64, 65) and the nonclassical MHC class I CD1d gene (58, 66), also restores T cell activation and promotes tumor regression and/or resistance to metastatic disease. Heightened cancer risk associated with aging is also attributed to the increasing levels of endogenous MDSC with advancing age, as is the increased growth rate of transplanted tumors in old vs young mice (67). Collectively, these findings identify MDSC as a key cell population that prevents a host’s immune system from responding to malignant cells.
MDSC also indirectly effect T cell activation by inducing T regulatory cells (Tregs), which in turn down-regulate cell-mediated immunity. Depending on the subpopulation of MDSC, Treg induction requires MDSC production of IL-10 and TGFβ (37) or arginase and is independent of TGFβ (68).
MDSC also perturb tumor immunity by skewing it toward a tumor-promoting type 2 phenotype. They do this by producing the type 2 cytokine IL-10 and by down-regulating macrophage production of the type 1 cytokine IL-12. This effect is amplified by macrophages that increase the MDSC production of IL-10 (61).
The role of MDSC in regulating NK cells is controversial. Several studies have demonstrated that MDSC inhibit NK cell cytotoxicity against tumor cells and block NK production of IFN-γ and that these activities require cell contact between the MDSC and target cells (60, 63, 69). This suppression is mediated by blocking expression of NKG2D, a receptor on NK cells that is required for NK activation (63). However, another study demonstrated that MDSC, which suppressed T cell activation, expressed Rae-1, the ligand for NKG2D, and as a result activated NK cells (70). Activated NK cells, in turn, eliminated MDSC. The discrepancy between these studies is most likely due to differences in MDSC subpopulations and further supports the concept that MDSC are a heterogeneous family of immature myeloid cells with diverse functions.
Tumor immunity in mice is also impacted by interactions between NKT cells and MDSC. Type I (invariant or iNKT) NKT cells facilitate tumor rejection (71), whereas type II NKT cells promote tumor progression (66). Type II NKT cells facilitate tumor progression by producing IL-13, which induces the accumulation of MDSC and/or by polarizing macrophages toward a tumor-promoting M2-like phenotype (58, 59, 66). NKT cells also regulate MDSC accumulation in virally infected mice. Influenza-infected mice have elevated levels of MDSC that are significant inhibitors of antiviral immunity; however, activation of iNKT cells blocks MDSC accumulation and restores antiviral immunity (72). Therefore, iNKT and type II NK cells are similar to M1 and M2 (or classically activated and alternatively activated) macrophages (73) in that one population promotes tumor progression while the other population enhances tumor growth by suppressing antitumor immunity.
MDSC use a diversity of mechanisms to suppress T cells
MDSC suppress T cell activation by multiple mechanisms. They suppress CD4+ and CD8+ T cells by their uptake of arginine and high intracellular level of arginase that depletes their surroundings of arginine, an essential amino acid for T cell activation (42, 45, 74). MDSC-produced ROS and peroxynitrite inhibit CD8+ T cells by catalyzing the nitration of the TCR and thereby preventing T cell-peptide-MHC interactions (57).
The development and function of most MDSC require IFN-γ. Both monocytic MDSC (CD11b+ Ly6G− Ly6Chigh) and granulocytic MDSC were reported to be IFN-γ dependent; however, monocytic MDSC suppress via NO (ROS undetectable), whereas granulocytic MDSC suppress via ROS (NO undetectable) (39, 41). Earlier studies also demonstrated that NO (56) and ROS production are IFN-γ dependent (75). However, IFN-γ may not be essential for all MDSC, because MDSC from IFN-γ receptor- deficient and -sufficient mice are equally suppressive for T cell activation (51), (P. Sinha and S. Ostrand-Rosenberg, unpublished observations).
The immunosuppressive molecule TGF-β has also been implicated in MDSC function. MDSC with the phenotype CD11b+Gr-1int (where “int” is “intermediate”) and induced by a mouse fibrosarcoma or colon carcinoma when stimulated with IL-13 through the IL-13Rα are activated to produce TGF-β (59, 76). In the same report, CD11b+Gr-1high MDSC did not produce suppressive TGF-β. Experiments with a transplanted and spontaneous mammary carcinoma demonstrated increased levels of TGF-β in the tumor microenvironment if the tumor cells were deficient for the type II TGF-β receptor. These authors demonstrated that a deficiency in the receptor resulted in an increase in CXCL5 in the tumor microenvironment. CXCL5, in turn, chemoattracted CXCR2-expressing Gr1+CD11b+ MDSC. Because Gr1+CD11b+ cells from tumor-bearing but not tumor-free mice produced high levels of TGF-β, tumor-infiltrating MDSC were the likely source of the heightened TGF-β in the tumor microenvironment. In addition to demonstrating that some MDSC use TGF-β to suppress, these reports indicate that at least some tumor-driven Gr1+CD11b+ cells are distinct from normally differentiating myeloid cells (8).
MDSC also suppress by down-regulating the TCR-associated ζ-chain (58, 77, 78), a phenomenon that occurs in most cancer patients (77) and is caused by inflammation (78). In the absence of the ζ-chain, CD4+ and CD8+ T cells are unable to transmit the required signals for activation.
Two additional suppressive mechanisms have been recently identified. MDSC down-regulate L-selectin (CD62L), a plasma membrane molecule necessary for the homing of naive T cells to lymph nodes. As a result, activation of CD4+ and CD8+ T cells is reduced because they are unable to migrate to lymph nodes where they would normally be activated by tumor Ags (E. M. Hanson, V. K. Clements, P. Sinha, D. Ilkovitch, and S. Ostrand-Rosenberg. Myeloid-derived suppressor cells down-regulate L-selectin expression on CD4+ and CD8+ T cells. Submitted for publication).
Recent work demonstrates that MDSC also block T cell activation by depriving the environment of cysteine, an amino acid that is essential for T cell activation. T cells lack the enzyme to convert methionine to cysteine and the membrane transporter to import cystine, which could be reduced intracellularly to cysteine, and therefore must obtain their cysteine from extracellular sources. Under healthy conditions, APCs (i.e., DC and macrophages) synthesize cysteine from methionine and import extracellular cystine and convert it to cysteine. Surplus cysteine is then exported during Ag presentation and imported by T cells. MDSC are also unable to convert methionine to cysteine, so they are fully dependent on importing cystine for conversion to cysteine. When MDSC are present in high concentrations they import most of the available cystine, depriving DC and macrophages of cystine. Because MDSC do not export cysteine, their immediate environment is cysteine deficient and T cells are unable to synthesize the necessary proteins for activation (M. Srivastava, P. Sinha, and S. Ostrand-Rosenberg. Myeloid-derived suppressor cells inhibit T cell activation by sequestering cystine and cysteine. Submitted for publication).
Fig. 2 diagrams the target cells impacted by MDSC and the suppressive mechanisms used by MDSC and illustrates the wide-ranging impact that these cells have on the immune system.
FIGURE 2.
MDSC suppress antitumor immunity through a variety of diverse mechanisms. T cell activation is suppressed by the production of arginase and ROS, the nitration of the TCR, cysteine deprivation, and the induction of Tregs. Innate immunity is impaired by the down-regulation of macrophage-produced IL-12, the increase in MDSC production of IL-10, and the suppression of NK cell cytotoxicity. Ag presentation is limited by the expansion of MDSC at the expense of DC.
Inflammation drives the accumulation and suppressive activity of MDSC
MDSC accumulation and activation are driven by multiple factors, many of which are identified with chronic inflammation. Early studies demonstrated that the inflammation-associated molecules VEGF and GM-CSF were associated with the accumulation of MDSC (14, 15) and suggested that inflammation might facilitate immune suppression (77). However, it was not until the proinflammatory cytokines IL-1β (79, 80) and IL-6 (81) and the bioactive lipid PGE2 (44) were shown to induce MDSC that the significance of the association with inflammation was appreciated. These later studies suggested that another mechanism by which inflammation promotes tumor progression is through the induction of MDSC that block immune surveillance and antitumor immunity, thereby removing barriers that could eliminate premalignant and malignant cells. Fig. 3 shows the proinflammatory mediators that induce MDSC and are discussed in the following sections.
FIGURE 3.
MDSC are induced and/or activated by multiple proinflammatory mediators. MDSC accumulate in the blood, bone marrow, lymph nodes, and at tumor sites in response to proinflammatory molecules produced by tumor cells or by host cells in the tumor microenvironment. These factors include PGE2, IL-1β, IL-6, VEGF, S100A8/A9 proteins, and the complement component C5a.
IL-1β and IL-6 induce MDSC
The ability of IL-1β to induce MDSC was demonstrated in mice with transplanted mammary carcinoma or fibrosarcoma tumors. Mice inoculated with wild-type tumor cells secreting IL-1β developed significantly higher levels of Gr+CD11b+ MDSC as compared with mice carrying the same tumors but not secreting IL-1β (79, 80). A later study using mouse mammary carcinoma cells transfected with a secreted form of IL-6 showed the same effect (81). The effect of secreted IL-1β was confirmed by another report in which IL-1β was driven by a stomach-specific promoter and the resulting transgenic mice developed elevated levels of MDSC and stomach cancer (82). IL-1β-induced accumulation of MDSC was independent of host T cells, B cells, and NK cells, and the MDSC had increased levels of ROS and enhanced suppressive activity against CD4+ and CD8+T cells relative to MDSC induced in less inflammatory environments. IL-1β-induced MDSC were also longer lived in vivo than MDSC induced in less inflammatory environments (79). Consistent with the down-regulation of antitumor immunity by MDSC, IL-1β-secreting tumors were more invasive and progressed more rapidly than non-IL-1β-producing tumors (80, 83). Similarly, mice treated with IL-1R antagonist, the naturally occurring inhibitor of IL-1β (80), or mice deficient for the IL-1R had slower growing tumors, whereas mice deficient for the IL-1Ra had higher MDSC levels (81). MDSC levels in tumor-bearing mice correlated with response to IL-1β in that IL-1R-deficient and IL-1Ra-deficient mice had reduced and elevated levels of MDSC, respectively, relative to wild-type mice. Although MDSC do not express IL-1R (79), they do express IL-6R (81), suggesting that IL-1β does not directly interact with MDSC. Because IL-6 is downstream of IL-1β in inflammatory responses, the observed effects of IL-1β could be due to IL-6.
In addition to increasing the levels of MDSC, IL-1β heightens the cross-talk between MDSC and macrophages and vice versa. MDSC from mice with IL-1β-secreting tumors produce more IL-10 than MDSC generated in an IL-1β-deficient environment. Similarly, MDSC from an IL-1β-enriched tumor microenvironment are more potent down-regulators of macrophage-produced IL-12. Experiments with TLR4-deficient mice demonstrated that these effects are mediated by signaling through the LPS-TLR4 pathway. However, TLR4 knockout mice with bacterially induced sepsis still accumulate high levels of MDSC, indicating that MDSC are also activated through TLR4-independent pathways. This alternative pathway is likely to be mediated by other TLR ligands, because mice deleted for MyD88, an adaptor protein in the signaling pathway of most TLRs, do not accumulate high levels of MDSC in response to sepsis (20). Therefore, TLRs differentially regulate MDSC accumulation, and activation through TLR4 is critical for MDSC-mediated exacerbation of a tumor-promoting type 2 phenotype that favors tumor progression (84).
Collectively, these findings indicate that limiting inflammation by reducing IL-1β levels or by preventing IL-1β binding to its receptor reduces MDSC accumulation and suppressive activity, delays tumor growth, enhances antitumor immunity, and is a potential strategy for limiting immune suppression and favoring antitumor immunity.
PGE2 induces MDSC
PGE2 and/or cyclooxygenase (COX)-2, which is required for the conversion of arachidonic acid to PGE2, are potent inflammatory mediators. They are produced by many tumors and are major contributors to the inflammatory tumor milieu (85, 86). Tumor-infiltrating macrophages also produce PGE2, further amplifying inflammation at the tumor site (87). PGE2 facilitates tumor growth through several nonimmune mechanisms, including promoting angiogenesis, protecting against apoptosis, and stimulating tumor cell proliferation and metastasis (88). Because COX-2 and PGE2 had been shown to increase arginase levels in mouse CD11b+ macrophages (89), the role of PG in MDSC induction was examined. PGE2 was identified as an inducer of MDSC because coculture of E prostanoid agonists, but not antagonists, induced mouse lineage-depleted, c-kit+ bone marrow precursor cells to differentiate into suppressive Gr+CD11b+MDSC. Mouse MDSC express all four PGE2 receptors (EP1–4). However, tumor-bearing mice deficient for a single receptor (EP-2) displayed reduced tumor growth and their MDSC were less suppressive as compared with MDSC from wild-type mice. Treatment of tumor-bearing mice with a COX-2 inhibitor (SC58236) reduced MDSC levels and delayed tumor progression (44). Using arginase levels as a measure of suppressive activity, PGE2 was also shown to up-regulate CD11b+CD14−CD15+ MDSC in patients with renal cancer (90). Therefore, elevated levels of PGE2 promote tumor progression through nonimmune mechanisms and by limiting antitumor immunity through the induction of higher levels and more suppressive MDSC.
Proinflammatory S100 proteins regulate MDSC accumulation
The S100A8 and S100A9 proteins are members of a large family of proteins that includes inflammatory and noninflammatory molecules. Heterodimeric S100A8/A9 complexes are calcium-binding proteins that are released by neutrophils and activated monocytes (91). They are elevated in patients with a variety of inflammatory diseases (92, 93) where they amplify inflammation by chemoattracting leukocytes that produce additional proinflammatory mediators (94). Several lines of evidence demonstrate that S100A8/A9 proteins regulate MDSC accumulation and suppressive activity. MDSC expressing S100A8/A9 accumulate in all regions of dysplasia and adenoma in a colitis-associated colon cancer model (95). MDSC from mice with a mammary carcinoma have receptors for S100A8/A9 complexes and secrete S100A8/A9 themselves (29). Ab blocking of the receptors in tumor-bearing mice reduces the quantity of MDSC in tumors and secondary lymphoid organs (29). Mice genetically deficient for S100A9 are resistant to challenge with a colon carcinoma but become susceptible if adoptively transferred with MDSC from wild-type mice (96). S100A8/A9 heterodimers mediate these effects through at least two mechanisms: 1) they block the differentiation of myeloid precursors into differentiated DC and macrophages through a STAT3-dependent mechanism (96); and 2) they chemoattract MDSC to tumor sites through a NF-κB-dependent pathway (29). Therefore, similarly as IL-1β, IL-6, and PGE2, S100A8/A9 proteins facilitate the accumulation of MDSC. However, unlike the other mediators, MDSC also produce S100A8/A9 proteins, providing for an autocrine feedback loop that sustains the accumulation and retention of MDSC while concomitantly chemoattracting additional proinflammatory mediators. As a result, S100A8/A9 proteins control a network of inflammatory mediators and are therefore also a promising target for reducing/eliminating MDSC (29, 96).
Complement component C5a induces MDSC
In addition to its classical role in Ab-mediated cell lysis, the complement system is a key player in innate immunity to infection and in inflammatory reactions (97). In both the classical and lectin pathways, C5 convertase (which includes C3a) generates C5a from C5. C5a, also known as anaphylatoxin, and C3a have inherent inflammatory activity, are chemoattractants, and localize to endothelial cells within solid tumors (97, 98). The first hint that complement components regulate tumor growth came from the observation that a transplanted cervical tumor grew more slowly in C3-deficient mice as compared with wild-type mice (99). Further studies using C5a receptor-deficient mice indicated that C5a also facilitated tumor progression and that it mediated its effects by binding to C5a receptors on MDSC. Tumor-bearing mice contained both granulocytic/neutrophil-like and monocytic MDSC, and both MDSC sub-populations expressed C5a receptors. However, C5a affected the two subpopulations differently. C5a increased the migration of granulocytic/neutrophil-like MDSC, but not monocytic MDSC, into solid tumors and peripheral lymphoid organs. It also increased the expression of ROS and reactive nitrogen species in monocytic but not granulocytic/neutrophil-like, MDSC. Both of these activities resulted in more potent MDSC that were more suppressive for T cells (99). The direct induction of MDSC by these complement components identifies additional proinflammatory mediators that could be targeted to eliminate MDSC.
Conclusions
MDSC cause immune suppression in most cancer patients, where they are an impediment to all immunotherapies that require an active immune response by the host. They may also facilitate the transformation of premalignant cells and promote tumor growth and metastasis by suppressing innate and adaptive immune surveillance that would otherwise eliminate abnormal cells. The induction of MDSC by proinflammatory factors identifies the immune system as another contributing mechanism by which chronic inflammation contributes to the onset and progression of cancer.
Elimination of MDSC is a priority for cancer patients who are candidates for active immunotherapy. Likewise, limiting the accumulation and retention of MDSC during chronic inflammation may reduce the risk of developing cancers. The proinflammatory mediators that induce MDSC are particularly attractive targets for limiting this suppressor cell population, although there are several unknowns that make it difficult to decide which mediators to target. For example, it is not known whether the various proinflammatory factors induce MDSC through independent or overlapping pathways. If the pathways are independent, then it will be necessary to block individual pathways. In contrast, if the pathways merge, then a single drug aimed at a common molecule may be effective. Future studies may identify additional proinflammatory mediators or factors that independently or coordinately regulate the accumulation of MDSC.
The heterogeneity of MDSC also complicates finding a single strategy for eliminating the cells. Pathologically distinct tumors produce different arrays and quantities of proinflammatory factors that induce MDSC. As a result, there is phenotypic heterogeneity between MDSC induced by histologically distinct tumors. There is also phenotypic heterogeneity within the MDSC population induced within a single individual. This heterogeneity may require identifying and then specifically targeting the relevant proinflammatory mediator(s) for individual patients or for the specific type of tumor.
Regardless of the complexity of MDSC induction, reduction of this inhibitory population is essential, and a comprehensive understanding of the proinflammatory mediators that regulate MDSC will provide valuable information for future drug design.
Footnotes
Abbreviations used in this paper: ROS, reactive oxygen species; COX, cyclooxygenase; DC, dendritic cell; iNKT, invariant NKT; MDSC, myeloid-derived suppressor cell; Treg, regulatory T cell; VEGF, vascular endothelial growth factor.
Disclosures
The authors have no financial conflict of interest.
This work was supported by National Institutes of Health Grants R01CA115880 and R01CA84232 and by the Susan G. Komen for the Cure Foundation.
References
- 1.Balkwill F, Mantovani A. Inflammation and cancer: back to Virchow? Lancet. 2001;357:539–545. doi: 10.1016/S0140-6736(00)04046-0. [DOI] [PubMed] [Google Scholar]
- 2.Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420:860–867. doi: 10.1038/nature01322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shacter E, Weitzman SA. Chronic inflammation and cancer. Oncology (Williston Park, N Y) 2002;16:217–226. 229. discussion 230–232. [PubMed] [Google Scholar]
- 4.Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454:436–444. doi: 10.1038/nature07205. [DOI] [PubMed] [Google Scholar]
- 5.Garcia-Rodriguez LA, Huerta-Alvarez C. Reduced risk of colorectal cancer among long-term users of aspirin and nonaspirin nonsteroidal antiinflammatory drugs. Epidemiology. 2001;12:88–93. doi: 10.1097/00001648-200101000-00015. [DOI] [PubMed] [Google Scholar]
- 6.Baron JA, Sandler RS. Nonsteroidal anti-inflammatory drugs and cancer prevention. Annu Rev Med. 2000;51:511–523. doi: 10.1146/annurev.med.51.1.511. [DOI] [PubMed] [Google Scholar]
- 7.Ellis LM, Hicklin DJ. VEGF-targeted therapy: mechanisms of anti-tumour activity. Nat Rev Cancer. 2008;8:579–591. doi: 10.1038/nrc2403. [DOI] [PubMed] [Google Scholar]
- 8.Yang L, Huang J, Ren X, Gorska AE, Chytil A, Aakre M, Carbone DP, Matrisian LM, Richmond A, Lin PC, Moses HL. Abrogation of TGFβ signaling in mammary carcinomas recruits Gr-1+CD11b+ myeloid cells that promote metastasis. Cancer Cell. 2008;13:23–35. doi: 10.1016/j.ccr.2007.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gabrilovich D. Mechanisms and functional significance of tumour-induced dendritic-cell defects. Nat Rev Immunol. 2004;4:941–952. doi: 10.1038/nri1498. [DOI] [PubMed] [Google Scholar]
- 10.Marx J. Cancer immunology. Cancer’s bulwark against immune attack: MDS cells. Science. 2008;319:154–156. doi: 10.1126/science.319.5860.154. [DOI] [PubMed] [Google Scholar]
- 11.Strober S. Natural suppressor (NS) cells, neonatal tolerance, and total lymphoid irradiation: exploring obscure relationships. Annu Rev Immunol. 1984;2:219–237. doi: 10.1146/annurev.iy.02.040184.001251. [DOI] [PubMed] [Google Scholar]
- 12.Pak AS, Wright MA, Matthews JP, Collins SL, Petruzzelli GJ, Young MR. Mechanisms of immune suppression in patients with head and neck cancer: presence of CD34+ cells which suppress immune functions within cancers that secrete granulocyte-macrophage colony-stimulating factor. Clin Cancer Res. 1995;1:95–103. [PubMed] [Google Scholar]
- 13.Young MR, Kolesiak K, Wright MA, Gabrilovich DI. Chemoattraction of femoral CD34+ progenitor cells by tumor-derived vascular endothelial cell growth factor. Clin Exp Metastasis. 1999;17:881–888. doi: 10.1023/a:1006708607666. [DOI] [PubMed] [Google Scholar]
- 14.Young MR, Wright MA. Myelopoiesis-associated immune suppressor cells in mice bearing metastatic Lewis lung carcinoma tumors: γ interferon plus tumor necrosis factor α synergistically reduces immune suppressor and tumor growth-promoting activities of bone marrow cells and diminishes tumor recurrence and metastasis. Cancer Res. 1992;52:6335–6340. [PubMed] [Google Scholar]
- 15.Almand B, Clark JI, Nikitina E, van Beynen J, English NR, Knight SC, Carbone DP, Gabrilovich DI. Increased production of immature myeloid cells in cancer patients: a mechanism of immunosuppression in cancer. J Immunol. 2001;166:678–689. doi: 10.4049/jimmunol.166.1.678. [DOI] [PubMed] [Google Scholar]
- 16.Diaz-Montero CM, Salem ML, Nishimura MI, Garrett-Mayer E, Cole DJ, Montero AJ. Increased circulating myeloid-derived suppressor cells correlate with clinical cancer stage, metastatic tumor burden, and doxorubicin-cyclophosphamide chemotherapy. Cancer Immunol Immunother. 2009;58:49–59. doi: 10.1007/s00262-008-0523-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sica A, Bronte V. Altered macrophage differentiation and immune dysfunction in tumor development. J Clin Invest. 2007;117:1155–1166. doi: 10.1172/JCI31422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Marigo I, Dolcetti L, Serafini P, Zanovello P, Bronte V. Tumor-induced tolerance and immune suppression by myeloid derived suppressor cells. Immunol Rev. 2008;222:162–179. doi: 10.1111/j.1600-065X.2008.00602.x. [DOI] [PubMed] [Google Scholar]
- 19.Haile LA, von Wasielewski R, Gamrekelashvili J, Kruger C, Bachmann O, Westendorf AM, Buer J, Liblau R, Manns MP, Korangy F, Greten TF. Myeloid-derived suppressor cells in inflammatory bowel disease: a new immunoregulatory pathway. Gastroenterology. 2008;135:871–881. 881.e1–5. doi: 10.1053/j.gastro.2008.06.032. [DOI] [PubMed] [Google Scholar]
- 20.Delano MJ, Scumpia PO, Weinstein JS, Coco D, Nagaraj S, Kelly-Scumpia KM, O’Malley KA, Wynn JL, Antonenko S, Al-Quran SZ, et al. MyD88-dependent expansion of an immature GR-1+CD11b+ population induces T cell suppression and Th2 polarization in sepsis. J Exp Med. 2007;204:1463–1474. doi: 10.1084/jem.20062602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brys L, Beschin A, Raes G, Ghassabeh GH, Noel W, Brandt J, Brombacher F, De Baetselier P. Reactive oxygen species and 12/15-lipoxygenase contribute to the antiproliferative capacity of alternatively activated myeloid cells elicited during helminth infection. J Immunol. 2005;174:6095–6104. doi: 10.4049/jimmunol.174.10.6095. [DOI] [PubMed] [Google Scholar]
- 22.Angulo I, de las Heras FG, Garcia-Bustos JF, Gargallo D, Munoz-Fernandez MA, Fresno M. Nitric oxide-producing CD11b+Ly-6G(Gr-1)+CD31(ER-MP12)+ cells in the spleen of cyclophosphamide-treated mice: implications for T-cell responses in immunosuppressed mice. Blood. 2000;95:212–220. [PubMed] [Google Scholar]
- 23.Zhu B, Bando Y, Xiao S, Yang K, Anderson AC, Kuchroo VK, Khoury SJ. CD11b+Ly-6Chi suppressive monocytes in experimental auto-immune encephalomyelitis. J Immunol. 2007;179:5228–5237. doi: 10.4049/jimmunol.179.8.5228. [DOI] [PubMed] [Google Scholar]
- 24.Kerr EC, Raveney BJ, Copland DA, Dick AD, Nicholson LB. Analysis of retinal cellular infiltrate in experimental autoimmune uveoretinitis reveals multiple regulatory cell populations. J Autoimmun. 2008;31:354–361. doi: 10.1016/j.jaut.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 25.Makarenkova VP, Bansal V, Matta BM, Perez LA, Ochoa JB. CD11b+/Gr-1+ myeloid suppressor cells cause T cell dysfunction after traumatic stress. J Immunol. 2006;176:2085–2094. doi: 10.4049/jimmunol.176.4.2085. [DOI] [PubMed] [Google Scholar]
- 26.Gabrilovich DI, Nagaraj S. Myeloid-derived suppressor cells as regulators of the immune system. Nat Rev Immunol. 2009;9:162–174. doi: 10.1038/nri2506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kusmartsev S, Nagaraj S, Gabrilovich DI. Tumor-associated CD8+ T cell tolerance induced by bone marrow-derived immature myeloid cells. J Immunol. 2005;175:4583–4592. doi: 10.4049/jimmunol.175.7.4583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Serafini P, Carbley R, Noonan KA, Tan G, Bronte V, Borrello I. High-dose granulocyte-macrophage colony-stimulating factor-producing vaccines impair the immune response through the recruitment of myeloid suppressor cells. Cancer Res. 2004;64:6337–6343. doi: 10.1158/0008-5472.CAN-04-0757. [DOI] [PubMed] [Google Scholar]
- 29.Sinha P, Okoro C, Foell D, Freeze HH, Ostrand-Rosenberg S, Srikrishna G. Proinflammatory S100 proteins regulate the accumulation of myeloid-derived suppressor cells. J Immunol. 2008;181:4666–4675. doi: 10.4049/jimmunol.181.7.4666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Filipazzi P, Valenti R, Huber V, Pilla L, Canese P, Iero M, Castelli C, Mariani L, Parmiani G, Rivoltini L. Identification of a new subset of myeloid suppressor cells in peripheral blood of melanoma patients with modulation by a granulocyte-macrophage colony-stimulation factor-based antitumor vaccine. J Clin Oncol. 2007;25:2546–2553. doi: 10.1200/JCO.2006.08.5829. [DOI] [PubMed] [Google Scholar]
- 31.Lathers DM, Achille N, Kolesiak K, Hulett K, Sparano A, Petruzzelli GJ, Young MR. Increased levels of immune inhibitory CD34+ progenitor cells in the peripheral blood of patients with node positive head and neck squamous cell carcinomas and the ability of these CD34+ cells to differentiate into immune stimulatory dendritic cells. Otolaryngol Head Neck Surg. 2001;125:205–212. doi: 10.1067/mhn.2001.117871. [DOI] [PubMed] [Google Scholar]
- 32.Pandit R, Lathers DM, Beal NM, Garrity T, Young MR. CD34+ immune suppressive cells in the peripheral blood of patients with head and neck cancer. Ann Otol Rhinol Laryngol. 2000;109:749–754. doi: 10.1177/000348940010900809. [DOI] [PubMed] [Google Scholar]
- 33.Zea AH, Rodriguez PC, Atkins MB, Hernandez C, Signoretti S, Zabaleta J, McDermott D, Quiceno D, Youmans A, O’Neill A, et al. Arginase-producing myeloid suppressor cells in renal cell carcinoma patients: a mechanism of tumor evasion. Cancer Res. 2005;65:3044–3048. doi: 10.1158/0008-5472.CAN-04-4505. [DOI] [PubMed] [Google Scholar]
- 34.Umemura N, Saio M, Suwa T, Kitoh Y, Bai J, Nonaka K, Ouyang GF, Okada M, Balazs M, Adany R, et al. Tumor-infiltrating myeloid-derived suppressor cells are pleiotropic-inflamed monocytes/macrophages that bear M1- and M2-type characteristics. J Leukocyte Biol. 2008;83:1136–1144. doi: 10.1189/jlb.0907611. [DOI] [PubMed] [Google Scholar]
- 35.Gallina G, Dolcetti L, Serafini P, De Santo C, Marigo I, Colombo MP, Basso G, Brombacher F, Borrello I, Zanovello P, et al. Tumors induce a subset of inflammatory monocytes with immunosuppressive activity on CD8+ T cells. J Clin Invest. 2006;116:2777–2790. doi: 10.1172/JCI28828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rossner S, Voigtlander C, Wiethe C, Hanig J, Seifarth C, Lutz MB. Myeloid dendritic cell precursors generated from bone marrow suppress T cell responses via cell contact and nitric oxide production in vitro. Eur J Immunol. 2005;35:3533–3544. doi: 10.1002/eji.200526172. [DOI] [PubMed] [Google Scholar]
- 37.Huang B, Pan PY, Li Q, Sato AI, Levy DE, Bromberg J, Divino CM, Chen SH. Gr-1+CD115+ immature myeloid suppressor cells mediate the development of tumor-induced T regulatory cells and T-cell anergy in tumor-bearing host. Cancer Res. 2006;66:1123–1131. doi: 10.1158/0008-5472.CAN-05-1299. [DOI] [PubMed] [Google Scholar]
- 38.Yang R, Cai Z, Zhang Y, Yutzy WH, IV, Roby KF, Roden RB. CD80 in immune suppression by mouse ovarian carcinoma-associated Gr-1+CD11b+ myeloid cells. Cancer Res. 2006;66:6807–6815. doi: 10.1158/0008-5472.CAN-05-3755. [DOI] [PubMed] [Google Scholar]
- 39.Youn JI, Nagaraj S, Collazo M, Gabrilovich DI. Subsets of myeloid-derived suppressor cells in tumor-bearing mice. J Immunol. 2008;181:5791–5802. doi: 10.4049/jimmunol.181.8.5791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sawanobori Y, Ueha S, Kurachi M, Shimaoka T, Talmadge JE, Abe J, Shono Y, Kitabatake M, Kakimi K, Mukaida N, Matsushima K. Chemokine-mediated rapid turnover of myeloid-derived suppressor cells in tumor-bearing mice. Blood. 2008;111:5457–5466. doi: 10.1182/blood-2008-01-136895. [DOI] [PubMed] [Google Scholar]
- 41.Movahedi K, Guilliams M, Van den Bossche J, Van den Bergh R, Gysemans C, Beschin A, De Baetselier P, Van Ginderachter JA. Identification of discrete tumor-induced myeloid-derived suppressor cell subpopulations with distinct T cell-suppressive activity. Blood. 2008;111:4233–4244. doi: 10.1182/blood-2007-07-099226. [DOI] [PubMed] [Google Scholar]
- 42.Kusmartsev S, Nefedova Y, Yoder D, Gabrilovich DI. Antigen-specific inhibition of CD8+ T cell response by immature myeloid cells in cancer is mediated by reactive oxygen species. J Immunol. 2004;172:989–999. doi: 10.4049/jimmunol.172.2.989. [DOI] [PubMed] [Google Scholar]
- 43.Bronte V, Serafini P, De Santo C, Marigo I, Tosello V, Mazzoni A, Segal DM, Staib C, Lowel M, Sutter G, et al. IL-4-induced arginase 1 suppresses allo-reactive T cells in tumor-bearing mice. J Immunol. 2003;170:270–278. doi: 10.4049/jimmunol.170.1.270. [DOI] [PubMed] [Google Scholar]
- 44.Sinha P, V, Clements K, Fulton AM, Ostrand-Rosenberg S. Prostaglandin E2 promotes tumor progression by inducing myeloid-derived suppressor cells. Cancer Res. 2007;67:4507–4513. doi: 10.1158/0008-5472.CAN-06-4174. [DOI] [PubMed] [Google Scholar]
- 45.Bronte V, Serafini P, Mazzoni A, Segal DM, Zanovello P. L-arginine metabolism in myeloid cells controls T-lymphocyte functions. Trends Immunol. 2003;24:302–306. doi: 10.1016/s1471-4906(03)00132-7. [DOI] [PubMed] [Google Scholar]
- 46.Kusmartsev S, Gabrilovich DI. Inhibition of myeloid cell differentiation in cancer: the role of reactive oxygen species. J Leukocyte Biol. 2003;74:186–196. doi: 10.1189/jlb.0103010. [DOI] [PubMed] [Google Scholar]
- 47.Mirza N, Fishman M, Fricke I, Dunn M, Neuger AM, Frost TJ, Lush RM, Antonia S, Gabrilovich DI. All-trans-retinoic acid improves differentiation of myeloid cells and immune response in cancer patients. Cancer Res. 2006;66:9299–9307. doi: 10.1158/0008-5472.CAN-06-1690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Srivastava MK, Bosch JJ, Thompson JA, Ksander BR, Edelman MJ, Ostrand-Rosenberg S. Lung cancer patients’ CD4+ T cells are activated in vitro by MHC II cell-based vaccines despite the presence of myeloid-derived suppressor cells. Cancer Immunol Immunother. 2008;57:1493–1504. doi: 10.1007/s00262-008-0490-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hoechst B, Ormandy LA, Ballmaier M, Lehner F, Kruger C, Manns MP, Greten TF, Korangy F. A new population of myeloid-derived suppressor cells in hepatocellular carcinoma patients induces CD4+CD25+Foxp3+ T cells. Gastroenterology. 2008;135:234–243. doi: 10.1053/j.gastro.2008.03.020. [DOI] [PubMed] [Google Scholar]
- 50.Zhou R, He PL, Ren YX, Wang WH, Zhou RY, Wan H, Ono S, Fujiwara H, Zuo JP. Myeloid suppressor cell-associated immune dysfunction in CSA1M fibrosarcoma tumor-bearing mice. Cancer Sci. 2007;98:882–889. doi: 10.1111/j.1349-7006.2007.00465.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sinha P, V, Clements K, Ostrand-Rosenberg S. Reduction of myeloid-derived suppressor cells and induction of M1 macrophages facilitate the rejection of established metastatic disease. J Immunol. 2005;174:636–645. doi: 10.4049/jimmunol.174.2.636. [DOI] [PubMed] [Google Scholar]
- 52.Kusmartsev S, Cheng F, Yu B, Nefedova Y, Sotomayor E, Lush R, Gabrilovich D. All-trans-retinoic acid eliminates immature myeloid cells from tumor-bearing mice and improves the effect of vaccination. Cancer Res. 2003;63:4441–4449. [PubMed] [Google Scholar]
- 53.Bronte V, Wang M, Overwijk WW, Surman DR, Pericle F, Rosenberg SA, Restifo NP. Apoptotic death of CD8+ T lymphocytes after immunization: induction of a suppressive population of Mac-1+/Gr-1+ cells. J Immunol. 1998;161:5313–5320. [PMC free article] [PubMed] [Google Scholar]
- 54.Bronte V, Apolloni E, Cabrelle A, Ronca R, Serafini P, Zamboni P, Restifo NP, Zanovello P. Identification of a CD11b+/Gr-1+/CD31+ myeloid progenitor capable of activating or suppressing CD8+ T cells. Blood. 2000;96:3838–3846. [PMC free article] [PubMed] [Google Scholar]
- 55.Gabrilovich DI, Velders MP, Sotomayor EM, Kast WM. Mechanism of immune dysfunction in cancer mediated by immature Gr-1+ myeloid cells. J Immunol. 2001;166:5398–5406. doi: 10.4049/jimmunol.166.9.5398. [DOI] [PubMed] [Google Scholar]
- 56.Mazzoni A, Bronte V, Visintin A, Spitzer JH, Apolloni E, Serafini P, Zanovello P, Segal DM. Myeloid suppressor lines inhibit T cell responses by an NO-dependent mechanism. J Immunol. 2002;168:689–695. doi: 10.4049/jimmunol.168.2.689. [DOI] [PubMed] [Google Scholar]
- 57.Nagaraj S, Gupta K, Pisarev V, Kinarsky L, Sherman S, Kang L, Herber DL, Schneck J, Gabrilovich DI. Altered recognition of antigen is a mechanism of CD8+ T cell tolerance in cancer. Nat Med. 2007;13:828–835. doi: 10.1038/nm1609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sinha P, V, Clements K, Ostrand-Rosenberg S. Interleukin-13-regulated M2 macrophages in combination with myeloid suppressor cells block immune surveillance against metastasis. Cancer Res. 2005;65:11743–11751. doi: 10.1158/0008-5472.CAN-05-0045. [DOI] [PubMed] [Google Scholar]
- 59.Terabe M, Matsui S, Park JM, Mamura M, Noben-Trauth N, Donaldson DD, Chen W, Wahl SM, Ledbetter S, Pratt B, et al. Transforming growth factor-β production and myeloid cells are an effector mechanism through which CD1d-restricted T cells block cytotoxic T lymphocyte-mediated tumor immunosurveillance: abrogation prevents tumor recurrence. J Exp Med. 2003;198:1741–1752. doi: 10.1084/jem.20022227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Suzuki E, Kapoor V, Jassar AS, Kaiser LR, Albelda SM. Gemcitabine selectively eliminates splenic Gr-1+/CD11b+ myeloid suppressor cells in tumor-bearing animals and enhances antitumor immune activity. Clin Cancer Res. 2005;11:6713–6721. doi: 10.1158/1078-0432.CCR-05-0883. [DOI] [PubMed] [Google Scholar]
- 61.Sinha P, V, Clements K, Bunt SK, Albelda SM, Ostrand-Rosenberg S. Cross-talk between myeloid-derived suppressor cells and macrophages subverts tumor immunity toward a type 2 response. J Immunol. 2007;179:977–983. doi: 10.4049/jimmunol.179.2.977. [DOI] [PubMed] [Google Scholar]
- 62.Pan PY, Wang GX, Yin B, Ozao J, Ku T, Divino CM, Chen SH. Reversion of immune tolerance in advanced malignancy: modulation of myeloid-derived suppressor cell development by blockade of stem-cell factor function. Blood. 2008;111:219–228. doi: 10.1182/blood-2007-04-086835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Li H, Han Y, Guo Q, Zhang M, Cao X. Cancer-expanded myeloid-derived suppressor cells induce anergy of NK cells through membrane-bound TGF-β1. J Immunol. 2009;182:240–249. doi: 10.4049/jimmunol.182.1.240. [DOI] [PubMed] [Google Scholar]
- 64.Nefedova Y, Nagaraj S, Rosenbauer A, Muro-Cacho C, Sebti SM, Gabrilovich DI. Regulation of dendritic cell differentiation and antitumor immune response in cancer by pharmacologic-selective inhibition of the Janus-activated kinase 2/signal transducers and activators of transcription 3 pathway. Cancer Res. 2005;65:9525–9535. doi: 10.1158/0008-5472.CAN-05-0529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kortylewski M, Kujawski M, Wang T, Wei S, Zhang S, Pilon-Thomas S, Niu G, Kay H, Mule J, Kerr WG, et al. Inhibiting Stat3 signaling in the hematopoietic system elicits multicomponent antitumor immunity. Nat Med. 2005;11:1314–1321. doi: 10.1038/nm1325. [DOI] [PubMed] [Google Scholar]
- 66.Terabe M, Swann J, Ambrosino E, Sinha P, Takaku S, Hayakawa Y, Godfrey DI, Ostrand-Rosenberg S, Smyth MJ, Berzofsky JA. A non-classical non-Vα14Jα18 CD1d-restricted (type II) NKT cell is sufficient for down-regulation of tumor immunosurveillance. J Exp Med. 2005;202:1627–1633. doi: 10.1084/jem.20051381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Grizzle WE, Xu X, Zhang S, Stockard CR, Liu C, Yu S, Wang J, Mountz JD, Zhang HG. Age-related increase of tumor susceptibility is associated with myeloid-derived suppressor cell mediated suppression of T cell cytotoxicity in recombinant inbred BXD12 mice. Mech Ageing Dev. 2007;128:672–680. doi: 10.1016/j.mad.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 68.Serafini P, Mgebroff S, Noonan K, Borrello I. Myeloid-derived suppressor cells promote cross-tolerance in B-cell lymphoma by expanding regulatory T cells. Cancer Res. 2008;68:5439–5449. doi: 10.1158/0008-5472.CAN-07-6621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Liu C, Yu S, Kappes J, Wang J, Grizzle WE, Zinn KR, Zhang HG. Expansion of spleen myeloid suppressor cells represses NK cell cytotoxicity in tumor-bearing host. Blood. 2007;109:4336–4342. doi: 10.1182/blood-2006-09-046201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Nausch N, I, Galani E, Schlecker E, Cerwenka A. Mononuclear myeloid-derived “suppressor” cells express RAE-1 and activate natural killer cells. Blood. 2008;112:4080–4089. doi: 10.1182/blood-2008-03-143776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Stewart TJ, Smyth MJ, Fernando GJ, Frazer IH, Leggatt GR. Inhibition of early tumor growth requires Jα18-positive (natural killer T) cells. Cancer Res. 2003;63:3058–3060. [PubMed] [Google Scholar]
- 72.De Santo C, Salio M, Masri SH, Lee LY, Dong T, Speak AO, Porubsky S, Booth S, Veerapen N, Besra GS, et al. Invariant NKT cells reduce the immunosuppressive activity of influenza A virus-induced myeloid-derived suppressor cells in mice and humans. J Clin Invest. 2008;118:4036–4048. doi: 10.1172/JCI36264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Allavena P, Sica A, Garlanda C, Mantovani A. The Yin-Yang of tumor-associated macrophages in neoplastic progression and immune surveillance. Immunol Rev. 2008;222:155–161. doi: 10.1111/j.1600-065X.2008.00607.x. [DOI] [PubMed] [Google Scholar]
- 74.Bronte V, Zanovello P. Regulation of immune responses by L-arginine metabolism. Nat Rev Immunol. 2005;5:641–654. doi: 10.1038/nri1668. [DOI] [PubMed] [Google Scholar]
- 75.Kusmartsev S, Gabrilovich DI. Immature myeloid cells and cancer-associated immune suppression. Cancer Immunol Immunother. 2002;51:293–298. doi: 10.1007/s00262-002-0280-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Fichtner-Feigl S, Terabe M, Kitani A, Young CA, Fuss I, Geissler EK, Schlitt HJ, Berzofsky JA, Strober W. Restoration of tumor immuno-surveillance via targeting of interleukin-13 receptor-α2. Cancer Res. 2008;68:3467–3475. doi: 10.1158/0008-5472.CAN-07-5301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Baniyash M. TCR zeta-chain downregulation: curtailing an excessive inflammatory immune response. Nat Rev Immunol. 2004;4:675–687. doi: 10.1038/nri1434. [DOI] [PubMed] [Google Scholar]
- 78.Ezernitchi AV, Vaknin I, Cohen-Daniel L, Levy O, Manaster E, Halabi A, Pikarsky E, Shapira L, Baniyash M. TCRζ down-regulation under chronic inflammation is mediated by myeloid suppressor cells differentially distributed between various lymphatic organs. J Immunol. 2006;177:4763–4772. doi: 10.4049/jimmunol.177.7.4763. [DOI] [PubMed] [Google Scholar]
- 79.Bunt SK, Sinha P, Clements VK, Leips J, Ostrand-Rosenberg S. Inflammation induces myeloid-derived suppressor cells that facilitate tumor progression. J Immunol. 2006;176:284–290. doi: 10.4049/jimmunol.176.1.284. [DOI] [PubMed] [Google Scholar]
- 80.Song X, Krelin Y, Dvorkin T, Bjorkdahl O, Segal S, Dinarello CA, Voronov E, Apte RN. CD11b+/Gr-1+ immature myeloid cells mediate suppression of T cells in mice bearing tumors of IL-1β-secreting cells. J Immunol. 2005;175:8200–8208. doi: 10.4049/jimmunol.175.12.8200. [DOI] [PubMed] [Google Scholar]
- 81.Bunt SK, Yang L, Sinha P, Clements VK, Leips J, Ostrand-Rosenberg S. Reduced inflammation in the tumor microenvironment delays the accumulation of myeloid-derived suppressor cells and limits tumor progression. Cancer Res. 2007;67:10019–10026. doi: 10.1158/0008-5472.CAN-07-2354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Tu S, Bhagat G, Cui G, Takaishi S, Kurt-Jones EA, Rickman B, Betz KS, Penz-Oesterreicher M, Bjorkdahl O, Fox JG, Wang TC. Overexpression of interleukin-1β induces gastric inflammation and cancer and mobilizes myeloid-derived suppressor cells in mice. Cancer Cell. 2008;14:408–419. doi: 10.1016/j.ccr.2008.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Voronov E, Shouval DS, Krelin Y, Cagnano E, Benharroch D, Iwakura Y, Dinarello CA, Apte RN. IL-1 is required for tumor invasiveness and angiogenesis. Proc Natl Acad Sci USA. 2003;100:2645–2650. doi: 10.1073/pnas.0437939100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bunt SK, Clements VK, Hanson EM, Sinha P, Ostrand-Rosenberg S. Inflammation enhances myeloid-derived suppressor cell cross-talk by signaling through Toll-like receptor 4. J Leuk Biol. 2009 doi: 10.1189/jlb.0708446. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Taketo MM. Cyclooxygenase-2 inhibitors in tumorigenesis (part II) J Natl Cancer Inst. 1998;90:1609–1620. doi: 10.1093/jnci/90.21.1609. [DOI] [PubMed] [Google Scholar]
- 86.Taketo MM. Cyclooxygenase-2 inhibitors in tumorigenesis (part I) J Natl Cancer Inst. 1998;90:1529–1536. doi: 10.1093/jnci/90.20.1529. [DOI] [PubMed] [Google Scholar]
- 87.Alleva DG, Burger CJ, Elgert KD. Tumor growth increases Ia− macrophage synthesis of tumor necrosis factor-α and prostaglandin E2: changes in macrophage suppressor activity. J Leukocyte Biol. 1993;53:550–558. doi: 10.1002/jlb.53.5.550. [DOI] [PubMed] [Google Scholar]
- 88.Wang D, DuBois RN. Pro-inflammatory prostaglandins and progression of colorectal cancer. Cancer Lett. 2008;267:197–203. doi: 10.1016/j.canlet.2008.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Rodriguez PC, Hernandez CP, Quiceno D, Dubinett SM, Zabaleta J, Ochoa JB, Gilbert J, Ochoa AC. Arginase I in myeloid suppressor cells is induced by COX-2 in lung carcinoma. J Exp Med. 2005;202:931–939. doi: 10.1084/jem.20050715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ochoa AC, Zea AH, Hernandez C, Rodriguez PC. Arginase, prostaglandins, and myeloid-derived suppressor cells in renal cell carcinoma. Clin Cancer Res. 2007;13:721s–726s. doi: 10.1158/1078-0432.CCR-06-2197. [DOI] [PubMed] [Google Scholar]
- 91.Foell D, Wittkowski H, Vogl T, Roth J. S100 proteins expressed in phagocytes: a novel group of damage-associated molecular pattern molecules. J Leukocyte Biol. 2007;81:28–37. doi: 10.1189/jlb.0306170. [DOI] [PubMed] [Google Scholar]
- 92.Foell D, Frosch M, Sorg C, Roth J. Phagocyte-specific calcium-binding S100 proteins as clinical laboratory markers of inflammation. Clin Chim Acta. 2004;344:37–51. doi: 10.1016/j.cccn.2004.02.023. [DOI] [PubMed] [Google Scholar]
- 93.Gebhardt C, Nemeth J, Angel P, Hess J. S100A8 and S100A9 in inflammation and cancer. Biochem Pharmacol. 2006;72:1622–1631. doi: 10.1016/j.bcp.2006.05.017. [DOI] [PubMed] [Google Scholar]
- 94.Hiratsuka S, Watanabe A, Aburatani H, Maru Y. Tumour-mediated upregulation of chemoattractants and recruitment of myeloid cells predetermines lung metastasis. Nat Cell Biol. 2006;8:1369–1375. doi: 10.1038/ncb1507. [DOI] [PubMed] [Google Scholar]
- 95.Turovskaya O, Foell D, Sinha P, Vogl T, Newlin R, Nayak J, Nguyen M, Olsson A, Nawroth PP, Bierhaus A, et al. RAGE, carboxylated glycans and S100A8/A9 play essential roles in colitis-associated carcinogenesis. Carcinogenesis. 2008;29:2035–2043. doi: 10.1093/carcin/bgn188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Cheng P, Corzo CA, Luetteke N, Yu B, Nagaraj S, Bui MM, Ortiz M, Nacken W, Sorg C, Vogl T, et al. Inhibition of dendritic cell differentiation and accumulation of myeloid-derived suppressor cells in cancer is regulated by S100A9 protein. J Exp Med. 2008;205:2235–2249. doi: 10.1084/jem.20080132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Markiewski MM, Lambris JD. The role of complement in inflammatory diseases from behind the scenes into the spotlight. Am J Pathol. 2007;171:715–727. doi: 10.2353/ajpath.2007.070166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Guo RF, Ward PA. Role of C5a in inflammatory responses. Annu Rev Immunol. 2005;23:821–852. doi: 10.1146/annurev.immunol.23.021704.115835. [DOI] [PubMed] [Google Scholar]
- 99.Markiewski MM, DeAngelis RA, Benencia F, Ricklin-Lichtsteiner SK, Koutoulaki A, Gerard C, Coukos G, Lambris JD. Modulation of the antitumor immune response by complement. Nat Immunol. 2008;9:1225–1235. doi: 10.1038/ni.1655. [DOI] [PMC free article] [PubMed] [Google Scholar]