Abstract
If the pace of increase in life expectancy in developed countries over the past two centuries continues through the 21st century, most babies born since 2000 in France, Germany, Italy, the UK, the USA, Canada, Japan, and other countries with long life expectancies will celebrate their 100th birthdays. Although trends differ between countries, populations of nearly all such countries are ageing as a result of low fertility, low immigration, and long lives. A key question is: are increases in life expectancy accompanied by a concurrent postponement of functional limitations and disability? The answer is still open, but research suggests that ageing processes are modifiable and that people are living longer without severe disability. This finding, together with technological and medical development and redistribution of work, will be important for our chances to meet the challenges of ageing populations.
Introduction
The remarkable gain of about 30 years in life expectancy in western Europe, the USA, Canada, Australia, and New Zealand—and even larger gains in Japan and some western European countries, such as Spain and Italy—stands out as one of the most important accomplishments of the 20th century. According to the Human Mortality Database, death rates in life-expectancy leaders such as Japan, Spain, and Sweden imply that even if health conditions do not improve, three-quarters of babies will survive to celebrate their 75th birthdays. Most babies born since 2000 in countries with long-lived residents will celebrate their 100th birthdays if the present yearly growth in life expectancy continues through the 21st century (table 1). This forecast is based on the assumption that mortality before age 50 years will remain at 2006 levels. At age 50 years and older, probability of dying decreases by a rate that yields yearly improvements in period life expectancy of 0·2 years. More complex methods can be developed on the basis of the assumption that life expectancies will increase linearly;12 however, such models produce similar estimates to those given in table 1.
Table 1.
Oldest age at which at least 50% of a birth cohort is still alive in eight countries
| 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | |
|---|---|---|---|---|---|---|---|---|
| Canada | 102 | 102 | 103 | 103 | 103 | 104 | 104 | 104 |
| Denmark | 99 | 99 | 100 | 100 | 101 | 101 | 101 | 101 |
| France | 102 | 102 | 103 | 103 | 103 | 104 | 104 | 104 |
| Germany | 99 | 100 | 100 | 100 | 101 | 101 | 101 | 102 |
| Italy | 102 | 102 | 102 | 103 | 103 | 103 | 104 | 104 |
| Japan | 104 | 105 | 105 | 105 | 106 | 106 | 106 | 107 |
| UK | 100 | 101 | 101 | 101 | 102 | 102 | 103 | 103 |
| USA | 101 | 102 | 102 | 103 | 103 | 103 | 104 | 104 |
Data are ages in years. Baseline data were obtained from the Human Mortality Database and refer to the total population of the respective countries.
These scenarios are projections, but we do not have to look to the future for challenges of an ageing population: the oldest-old group (aged >85 years) have over past decades been the most rapidly expanding segment of the population in developed countries. This group is also the most susceptible to disease and disability.13–18 Development of mortality, disease, and disability rates in elderly people will therefore have a fundamental effect on sustainability of modern society.
Mortality
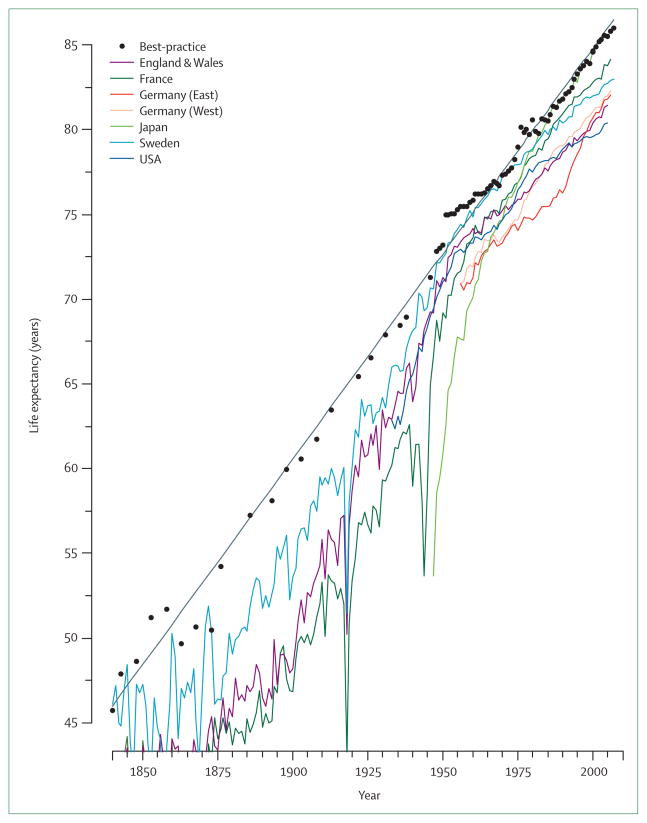
Life expectancy is lengthening almost linearly in most developed countries, with no sign of deceleration. In 2002, Oeppen and Vaupel12 showed that best-practice life expectancy—ie, the highest value recorded in a national population—has risen by 3 months per year since 1840 (figure 1). Data for a further 7 years have since become available, and life expectancy keeps rising. In the record-holding country, Japan, female life expectancy was 86·0 years in 2007,19 surpassing the 85-year limit to human life expectancy that was proposed by Fries20 in 1980, and later elaborated on by Olshansky and colleagues.21 Although with lower life expectancies than that of Japan, most developed countries have had similar yearly increases in life expectancy since 1950 (figure 1). The linear increase in record life expectancy for more than 165 years does not suggest a looming limit to human lifespan. If life expectancy were approaching a limit, some deceleration of progress would probably occur. Continued progress in the longest living populations suggests that we are not close to a limit, and further rise in life expectancy seems likely.
Figure 1. Best-practice life expectancy and life expectancy for women in selected countries from 1840 to 2007.
Linear regression trend depicted by solid grey line with a slope of 0·24 per year. Data from supplementary material of reference 12 and the Human Mortality Database.
Life-expectancy improvements over the past 165 years were not propelled by uniform reductions in mortality at all ages. Until the 1920s, improvements in infant and childhood survival contributed most to the increase in record life expectancies. After successful combating of infectious diseases at young ages, gains in record life expectancy were fuelled by progress at older ages (table 2). This reduction in old-age mortality was unprecedented and unexpected.20,21 Since the 1950s, and especially since the 1970s, mortality at ages 80 years and older has continued to fall, in some countries even at an accelerating pace.14,22–26
Table 2.
Age-specific contributions to the increase in record life expectancy in women from 1850 to 2007
| 1850–1900 | 1900–25 | 1925–50 | 1950–75 | 1975–90 | 1990–2007 | |
|---|---|---|---|---|---|---|
| 0–14 years | 62·13% | 54·75% | 30·99% | 29·72% | 11·20% | 5·93% |
| 15–49 years | 29·09% | 31·55% | 37·64% | 17·70% | 6·47% | 4·67% |
| 50–64 years | 5·34% | 9·32% | 18·67% | 16·27% | 24·29% | 10·67% |
| 65–79 years | 3·17% | 4·44% | 12·72% | 28·24% | 40·57% | 37·22% |
| >80 years | 0·27% | −0·06% | −0·03% | 8·07% | 17·47% | 41·51% |
Data derived from reference 12 and the Human Mortality Database.
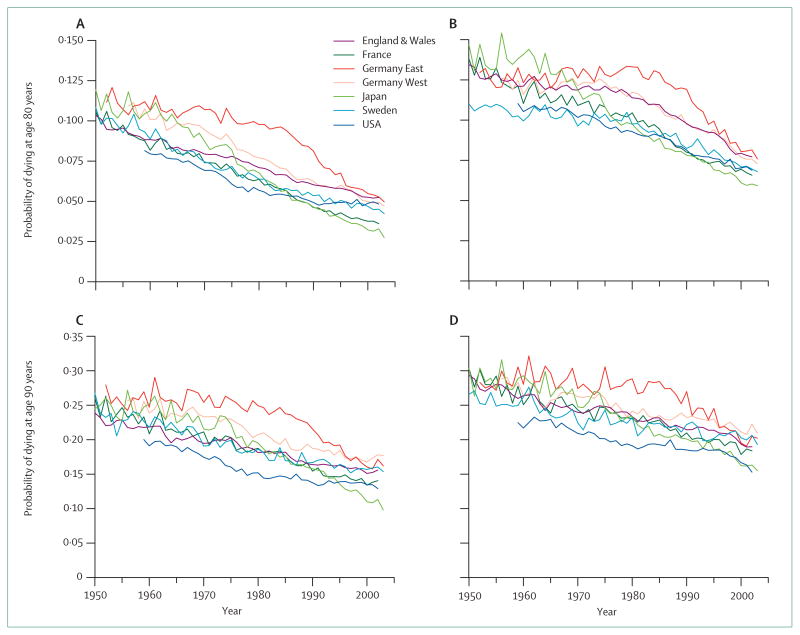
Data from more than 30 developed countries26 showed that in 1950 the probability of survival from age 80 years to 90 years was on average 15–16% for women and 12% for men. In 2002, these values were 37% and 25%. Even in the country with the lowest probability (the Czech Republic), the situation improved remarkably. In Japan—which is the country with residents having the best chances of survival—the probability of surviving from age 80 years to 90 years now exceeds 50% for women. Figure 2 plots the probabilities of survival to their next birthday of people who lived to age 80 or 90 years in seven large developed countries.27 With a few exceptions, mortality generally keeps falling in all selected countries for both sexes at both ages. In 1950, about one in ten 80-year-old women died before their 81st birthdays. About 50 years later, this number was typically less than one in 20. In Japan, it was less than 3%. Male mortality was also halved. The probability of dying for men aged 80 years in the early 1950s was about 14%, and only about 7% half a century later. Deaths of children and young adults are rare in high-income countries. If the pace of increase in life expectancy is to continue, progress in mortality reduction needs to be made in the elderly population and oldest-old groups. A continuous decrease in mortality at old age is reported in most developed countries, but not all (figure 2).
Figure 2. Probability of dying for elderly men and women in selected countries from 1950 to 2003.
(A) Women aged 80 years. (B) Men aged 80 years. (C) Women aged 90 years. (D) Men aged 90 years. Data from reference 27.
In 1980, remaining life expectancy for people aged 80 years was higher in the USA than it was in Sweden, France, England and Wales, and Japan. Manton and Vaupel suggested that elderly Americans were receiving better health care than were elderly citizens of other developed countries.28 However, through the 1980s and 1990s, mortality improvements stagnated for US women (figure 2), not only for the oldest-old population but also for younger elderly people. This stagnation was not due to immigration, because survival of US women is largely unaffected by place of birth. Wang and Preston29 investigated the relation between cohort smoking patterns and adult mortality, and reported that smoking accounts for important anomalies in the recent age and sex pattern of mortality change in the USA. They concluded that because of reductions in smoking that have already occurred, mortality could decrease much faster than was previously projected.
Smoking also seems to be the main underlying reason for divergent trends in Denmark. In the 1950s, mean life expectancy in Denmark was among the highest in the world, a position that was maintained until around 1980, when an extended period of stagnation began, which was most pronounced for women. Denmark’s position fell from third rank of 20 Organisation for Economic Cooperation and Development (OECD) countries in the 1950s to rank 17 for men and 20 for women at the beginning of the new millennium; life expectancy was 3 years lower than in neighbouring Sweden. Cause-specific mortality and morbidity data suggest that the Danish stagnation was caused by lifestyle factors, especially smoking.30,31
Analysis of life disparity in Denmark shows that slowing of progress in reduction of differentials in lifespans occurred at about the same time as did slowing of progress in increasing life expectancy—ie, Danish life expectancy might have stagnated, at least in part, because inequalities in health-related factors did not fall in the 1970s and 1980s. Differing lifespans among Danes are attributable in part to differences in smoking behaviour. Generally, countries that have the least disparity in lifespans are those that enjoy the longest life expectancies.
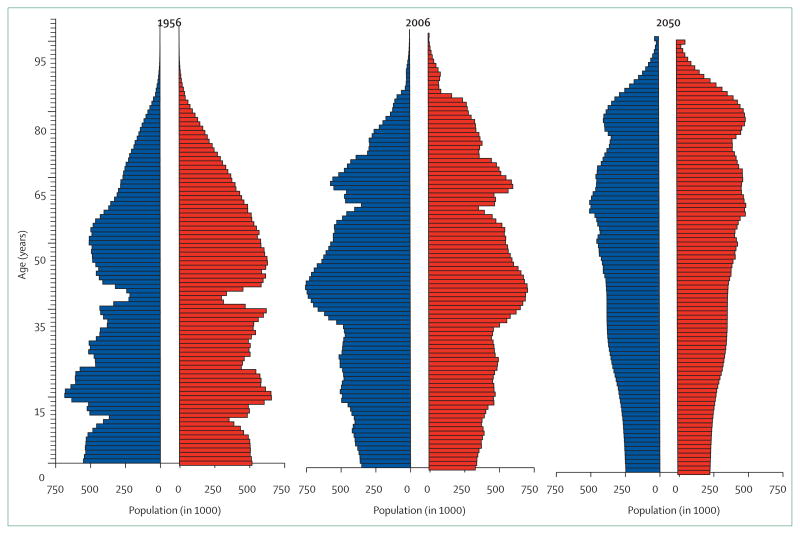
The new demography of low fertility and, to an even greater extent, low mortality32 produces population ageing. Figure 3 summarises the change in age structure of the German population in the half century up to 2006 and the next half century.33 Because of Germany’s losses in the two World Wars, the panel for 1956 is jagged. About one person in ten was aged 65 years or older in Germany in the mid-1950s. Only 1·3% of the population were aged 80 years or older. 50 years later, the proportion of people aged 65 years and older almost doubled (19%), and the pro portion of octogenarians, nonagenarians, and centenarians more than tripled (4·4%). On the assumption of a constant total fertility rate that is slightly higher than at present, more immigration than on average during the past 10 years, and the low scenario for increase in life expectancy, the age structure of the German population in 2050 will be substantially older and smaller than it is nowadays. Future trends in morbidity and disability rates will be crucial determinants of societies’ ability to meet the challenges of population ageing.
Figure 3. Population pyramids for Germany in 1956, 2006, and 2050.
Horizontal bars are proportional to number of men (blue) and women (red). Data for 2050 are based on the German Federal Statistical Office’s 1-W1 scenario, which assumes a roughly constant total fertility rate of 1·4, yearly net migration of 100 000 and life expectancy in 2050 reaching 83·5 years for men and 88·0 years for women. Data from reference 33 and the Human Mortality Database.
Health
Because health is a multidimensional notion, several indicators are needed to capture trends. On the basis of Verbrugge and Jette’s34 framework, health deterioration can be described by risk factors that lead to diseases and conditions that can cause loss of function, and, dependent on the environmental context, can result in disability. To assess trends in health, investigators have to analyse trends in these different levels of health, bearing in mind that different indicators show different phases of the disease and disability processes, and thus might follow different trends. Studies of health trends are complex because (1) indicators of morbidity, functional limitations, and disability have been applied inconsistently; (2) study designs, participation rates, and wording of questions have changed over time; and (3) institutional populations are excluded from many health surveys despite the burden this population places on health-care systems and despite changes in institutionalisation rates.
We focus on trends and patterns in highly developed industrial countries, which have the most complete data for developments in health, despite difficulties with trend assessment. In view of the discussion by Vallin and Meslé35 about convergences and divergences in health transition and mortality, we expect similar trends in these countries, with the addition, however, of latecomers and forerunners.
Disease
The prevalence of diseases in the elderly population has generally increased over time. Most survey data are based on self-reported morbidity. Although self-reported data are often assumed to underestimate true prevalence, investigators36 report higher prevalences in a Dutch population of diabetes mellitus, cardiac disease, lower-back complaints, and asthma on the basis of self-reports than of medical records. However, increasing trends have generally been shown for both self-reports and medical records.36–38 These trends might partly show improved medical knowledge and health-service use in elderly people, without changes in underlying conditions. For instance, initially silent diseases, such as type 2 diabetes, hypertension, and some cancers, now get diagnosed earlier and receive better treatment than they did previously. This progress leads to a longer period of morbidity, but with an improved functional status.39
A rise in prevalence of chronic diseases, including heart disease, arthritis, and diabetes, was recorded in elderly people between the 1980s and 1990s in the USA,40,41 12 OECD countries,42 the Netherlands,36 and Sweden.37,43 Increases in pain and psychological distress,44 general fatigue, dizziness, leg ulcers, heart problems, hyper tension, and musculoskeletal pain,36,45 and worsening lung function34 have been reported for the elderly population in Sweden between 1991 and 2002. Reports suggest a general increase in multiple symptoms,36,45 although in the Netherlands improvements have been noted for some diseases—eg, prevalences of cardiac disease, asthma, osteoarthritis, depression based on family doctors’ registers, and lower-back complaints.36
Total cancer incidence has been rising, mainly because of population ageing, but also because of some cancers, such as prostate cancer in men, lung and breast cancer in women, and colorectal cancer and melanoma in both sexes. The most consistent decrease in Europe was noted for gastric and cervical cancers and male lung cancer. Survival rates for cancer have generally increased. Reduced exposure to carcinogens (eg, tobacco smoke), earlier diagnosis, and therapeutic improvements account for part of this change, but overall the distribution of cancer has shifted towards less aggressive cancers, with the notable exception of lung cancer in women.46
An increase in disease and chronic conditions has been reported in people aged 65–69 years;47 for example, in arthritis and chronic airways obstructions in the UK. At working ages in the USA, rises have been noted for asthma, chronic bronchitis, diabetes, congestive heart failure, and arthritis.48 A comparison of baby boomers—ie, people born during the post-World War 2 baby boom, between 1946, and 1966, dependent on country—with the preceding cohort49 reveals fewer musculoskeletal conditions, but an increase in cardiovascular disease, lung problems, and diabetes.
The rise in prevalence of cardiovascular disease is thought to result from disparate trends in mortality versus incidence. Cardiovascular mortality fell more than did incidence of cardiovascular disease. Data for stroke incidence is mixed. Results of four studies showed increasing stroke incidence from the 1970s to the 1980s, five showed decreasing incidence from the late 1970s to the 1990s, and eight showed no change.50 High prevalence of cardiovascular disease could be due to increased duration of time lived with the disease, potentially because of improved medical care, and possibly early diagnosis.36
Obesity is a widely discussed risk factor that threatens improvements in health.51–54 It has been increasing in almost all populations,38,42 with an estimated 3·8% per year average rise in people aged 65 years or older during the 1990s in the Netherlands,42 closely followed by the USA, UK, and Italy. Obesity increases probability of transition from good health to disability, reduces chance of recovery,55,56 and increases risk of death,56 although mortality in elderly people who are obese seems not to be raised, and could even be lower than in their non-obese counterparts.55 Obesity is related to various poor health outcomes, including raised risk of diabetes, arthritis, and stroke. The number of diabetes cases, even if prevalence of obesity remains stable until 2030, is estimated to more than double worldwide57 because of population ageing, with the largest rise in people aged 65 years and older.
Definitions of obesity vary,58 and the relation between obesity and disability is complex. The consequences of obesity can be modified by increased use of anti-hypertensives59 and lipid-lowering drugs,60 which reduce risk of cardiovascular disease and resulting disabilities. Reductions in disability reported in non-obese elderly individuals might not occur within an obese elderly population.61
Evidence about hypertension is mixed. Crimmins1 reported a fall in the USA since the 1960s at ages 65–74 years. Conversely, Ostchega and colleagues62 report a rise at ages 60 years and older. Lafortune and Balestat42 report rates of increase in 12 OECD countries ranging from 3·9% per year in Canada to 6·3% per year in Italy. Rosen and Haglund43 suggest an increase for Swedish men from the 1980s to 2000. In the USA, awareness and treatment of hypertension in elderly people has been growing over time;59 however, elderly women (aged 70 years and older) are less aware and thus less often treated than are men.62 Qureshi and colleagues63 report different trends for severity of hypertension: prehypertension rose, stage I hypertension (140–159/90–99 mm Hg) remained constant, and stage II hypertension fell. Crimmins and colleagues38 report increases in systolic blood pressure for the USA.
Little is known about trends in cognitive function and dementia. Freedman and colleagues2 report a reduction in cognitive impairment in the mid-1990s in the USA. However, these results were contested by Rodgers and coworkers64 using the same data with adjustments for learning effects and some methodological issues. Manton and colleagues65 report a fall in severe cognitive impairment of 55% in men and 45% in women between 1982 and 1999, mainly because of a decrease in incidence of mixed dementia but not Alzheimer’s disease. Langa and co-workers66 reported a compression of cognitive morbidity between 1993 and 2004, in Americans aged 70 years or older, with a decreasing number of people reaching a threshold of significant cognitive impairment, and increasing mortality in those with cognitive impairment. A fall in prevalence of dementia is reported for Australia between 1998 and 2003, whereas data for Japan (1998–2004) and Sweden (1988–2004) suggest an increase.42,45
Functional limitations and disability
Improvements in mobility measured by single indices have been reported by many investigators in the USA.2 The yearly rate of improvement is typically around 1%. In Spain, between 1986 and 1999, improvements were reported on the basis of the Rosow-Breslau scale of items pertaining to stooping or kneeling, reaching or extending arms, pulling or pushing large objects, and handling or picking up of small objects.67,68 A similar trend in the USA from the late 1970s to the late 1990s was reported in the Framingham Heart Study.69 In Japan, in the 10 years from 1993 to 2002, the prevalence of functional limitations did not change at ages 66 years and older, with the exception of 16–17% improvements in stooping, lifting, and the absence of any limitations.70
Investigators note a rise in severe hearing impairments for Sweden between 1991 and 2002,37,71 a fall in hearing problems for Spain67 between 1986 and 1999, and constant rates for the USA.40,72 Vision has improved in Sweden,71 Spain,67 and the USA,73,74 which is also the result of developments in cataract surgery—which is the most frequently done surgical procedure in developed countries. Few operations have changed so much in recent years.75
Table 3 shows yearly changes in mobility, based on indicators that are geared toward the highest level of physical functioning, such as walking and climbing stairs. Large improvements are reported for Spain,67 the USA,69 and the Netherlands,36 smaller gains for Finland,80 and stagnation for Japan.70 In northern Europe there was stagnation, but improvements were reported in southern Europe.77
Table 3.
Studies of yearly changes in mobility-related disabilities in high-income countries
| Region | Age (years) | Length of follow-up (years) | Institutional population included | Sample size | Indicator | Yearly change (age-adjusted) | p value | |
|---|---|---|---|---|---|---|---|---|
| 1987–200136 | Netherlands | >55 | 14 | No | 2708–3474 | Men: walking up stairs, carrying 5–10 kg, lifting object while standing, walking 400 m | –4·86% | 0·05 |
| 1987–200136 | Netherlands | >55 | 14 | No | 2708–3474 | Women: walking up stairs, carrying 5–10 kg, lifting object while standing, walking 400 m | –3·64% | 0·05 |
| 1986–199967 | Spain | >65 | 13 | Part | 750 192 men | Walking up stairs, walking out of house, chairfast, bedfast, serious difficulty standing up or getting out of bed or chair | –3·56% | ·· |
| 1986–199967 | Spain | >65 | 13 | Part | 1 323 261 women | Walking up stairs, walking out of house, chairfast, bedfast, serious difficulty standing up or getting out of bed or chair | –2··57% | ·· |
| 1991/92–1996/9747 | UK | 65–69 | 5 | Yes | 689–687 | Walking up stairs, chairfast, bedfast | 5·00% | 0·09 |
| 1985/89–1993/9976 | Finland | 65–79 | 8 | Yes, but under- represented | 2213–2911 | Men: use of stairs | –1·70% | ·· |
| 1985/89–1993/9976 | Finland | 65–79 | 8 | Yes, but under- represented | 2213–2911 | Men: walking outside | –3·29% | ·· |
| 1985/89–1993/9976 | Finland | 65–79 | 8 | Yes, but under- represented | 2251–2934 | Women: use of stairs | –0·52% | ·· |
| 1985/89–1993/9976 | Finland | 65–79 | 8 | Yes, but under- represented | 2251–2934 | Women: walking outside | −1·88% | ·· |
| 1993–200270 | Japan | >66 | 9 | No | 1786–2391 | Walking 200–300 m | −1·47% | ns |
| 1993–200270 | Japan | >66 | 9 | No | 1786–2391 | Standing | −0·37% | ns |
| 1993–200270 | Japan | >66 | 9 | No | 1786–2391 | Walking up stairs | −1·83% | ns |
| 1993–200270 | Japan | >66 | 9 | No | 1786–2391 | Use of stairs or walking | −1·74% | ns |
| 1988–200077 | Europe | >70 | 12 | No | 3496 | Men: moving outdoors, walking up stairs, walking 400 m, carrying 5 kg | −0·17% | ns |
| 1988–200077 | Europe | >70 | 12 | No | 3496 | Women: moving outdoors, walking up stairs, walking 400 m, carrying 5 kg | −0·33% | ns |
| 1992–200237,44,45,78* | Sweden | >77 | 10 | Yes | 537–561 | Walking 100 m, walking up stairs, rising from chair, standing | 4·00% | 0·01 |
| 1977–199969 | USA | 79–88 | 22 | No | 177–174 | Women: walking up stairs to 2nd floor | −3·34% | 0·01† |
| 1977–199969 | USA | 79–88 | 22 | No | 177–174 | Women: walking 0·5 miles | −2·62% | 0·01† |
| 1977–199969 | USA | 79–88 | 22 | No | 103–119 | Men: walking up stairs to 2nd floor | −4·55% | 0·01† |
| 1977–199969 | USA | 79–88 | 22 | No | 103–119 | Men: walking 0·5 miles | −0·61% | 0·01† |
| 1895 cohort vs 1905 cohort79 | Denmark | >100 | 10 | Yes | 50–78 | Community-dwelling women: walking indoors | −7·50% | 0·01 |
| 1895 cohort vs 1905 cohort79 | Denmark | >100 | 10 | Yes | 50–78 | Community-dwelling women: getting outdoors | −5·13% | 0·01 |
| 1895 cohort vs 1905 cohort79 | Denmark | >100 | 10 | Yes | 50–78 | Community-dwelling women: walking up stairs | −4·50% | 0·01 |
| 1895 cohort vs 1905 cohort79 | Denmark | >100 | 10 | Yes | 110–107 | Women in institutions: walking indoors | −1·82% | 0·23 |
| 1895 cohort vs 1905 cohort79 | Denmark | >100 | 10 | Yes | 110–107 | Women in institutions: getting outdoors | −4·19% | 0·01 |
| 1895 cohort vs 1905 cohort79 | Denmark | >100 | 10 | Yes | 110–107 | Women in institutions: walking up stairs | −2·67% | 0·01 |
Calculation of yearly change based on prevalences: (last year–first year)/first year/number of years in follow-up×100. Calculation of yearly change based on odds ratio: −(1−OR)/number of years in follow-up×100. Positive values show an increase in disability. Negative values show a reduction in disability. ns=not significant.
Data are derived from reference 37.
Significant for any limitations of the Rosow-Breslau scale: heavy work around the house, walk up or down stairs to second floor, walk 0·5 miles.
Disability is usually measured by a set of items on self-reported limitations with severity of disability ranked by the number of positively answered items. Disabilities in activities of daily living (ADL) show dependence of an individual on others, with need for assistance in daily life. The activities of feeding, dressing, bathing or showering, transferring from bed and chair, and continence are central to self-care and are called basic ADL. Disability in instrumental ADL refers to disabilities affecting a broad range of activities, such as telephone use, shopping, housekeeping, preparation of food, doing laundry, use of various types of transport, handling of drugs, and management of finances. Some international surveys use only a short general question on being hampered or disabled.9
Increasing evidence exists that disability prevalence, measured by these indices, has been falling (table 4). During the 1980s and 1990s, reductions in disability have been reported as 0·4–2·7% per year.2 Parker and Thorslund11 conclude that most ADL indices are improving, although some evidence is mixed, and that indices for instrumental ADL are mostly improving or stagnating. National datasets have often reported conflicting evidence about severe forms of personal-care disability, such as limitations of bathing, dressing, and moving. Taking into account differing wording, sampling strategies, and inclusion of institutional populations in four US health surveys, a general reduction of 1·0–2·5% per year is evident in the community-based elderly population with reported difficulties with ADL.83 A series of studies, some in populations with the highest reported life expectancies, have lent support to this evidence.
Table 4.
Studies of yearly changes in disabilities affecting activities of daily living in high-income countries
| Region | Age (years) | Length of follow-up (years) | Institutional population included | Sample size | Indicator | Yearly change (age-adjusted) | p value | |
|---|---|---|---|---|---|---|---|---|
| 1984–199651 | USA | 40–59 | 12 | No | NHIS | Unable to attend to personal care needs: severe disability | 1·20% | ns |
| 1984–199651 | USA | 40–59 | 12 | No | NHIS | Unable to attend to or restricted in personal care needs: severe and moderate disability | 1·62% | 0·05 |
| 1997/98–2005/0649 | USA | 40–59 | 8 | No | NHIS | ADL | 2·17% | 0·01 |
| 1997/98–2005/0649 | USA | 40–59 | 8 | No | NHIS | IADL | −0·97% | ns |
| 1984–199651 | USA | 60–69 | 12 | No | NHIS | Unable to attend to personal care needs: severe disability | −0·09% | ns |
| 1984–199651 | USA | 60–69 | 12 | No | NHIS | Unable to attend to or restricted in personal care needs: severe and moderate disability | −0·31% | ns |
| 1991/92–1996/9747 | UK | 65–69 | 5 | Yes | 689–687 | IADL/ADL | 6·80% | 0·06 |
| 1987–200136 | Netherlands | >55 | 14 | No | 2708–3474 | Men: ADL | −4·57% | 0·05 |
| 1987–200136 | Netherlands | >55 | 14 | No | 2708–3474 | Women: ADL | −4·29% | 0·05 |
| 1993–199968 | Spain | >64 | 6 | No | 1283 | ADL | −9·54% | 0·05 |
| 1980/81–1991/9281 | France | >65 | 11 | No | 5000 | Being hampered or disabled | −1·60% | ·· |
| 1991/92–2002/0381 | France | >65 | 11 | No | 5000 | Being hampered or disabled | −5·50% | ·· |
| 1982–199482 | USA | >65 | 12 | Yes | NLTCS | ADL low disability levels | −0·90% | ·· |
| 1994–2004/0582 | USA | >65 | 10 | Yes | NLTCS | ADL low disability levels | −1·70% | ·· |
| 1982–199482 | USA | >65 | 12 | Yes | NLTCS | ADL high disability levels | −1·40% | ·· |
| 1994–2004/0582 | USA | >65 | 10 | Yes | NLTCS | ADL high disability levels | −2·40% | ·· |
| 1986–199967 | Spain | >65 | 13 | Part | 750 192 men | ADL and function | −3·97% | ·· |
| 1986–199967 | Spain | >65 | 13 | Part | 1 323 261 women | ADL and function | −3·29% | ·· |
| 1986–199967 | Spain | >65 | 13 | Part | 750 192 | Men: BADL | 0·50% | ·· |
| 1986–199967 | Spain | >65 | 13 | Part | 1 323 261 | Women: BADL | 1·92% | ·· |
| 1993/95–2001/0380 | Finland | 65–84 | 8 | Yes | 1972–1905 | Women: BADL | −6·25% | 0·05 |
| 1993/95–2001/0380 | Finland | 65–84 | 8 | Yes | 2021–1908 | Men: BADL | −5·13% | 0·05 |
| 1993–200270 | Japan | >66 | 9 | No | 1786–2391 | Any IADL/ADL | −3·99% | 0·00 |
| 1993–200270 | Japan | >66 | 9 | No | 1786–2391 | Any limitation | −1·94% | 0·10 |
| 1988–200077 | Europe | >70 | 12 | No | 3496 | Women: self-care disability | −7·20% | 0·03 |
| 1988–200077 | Europe | >70 | 12 | No | 3496 | Men: self-care disability | −2·60% | 0·05 |
| 1982–200183 | USA | >70 | 19 | Yes | 7500–12 000 | Difficulty, needs/receives help | 1·0−2·5% | ·· |
| 1982–200384 | USA | >70 | 21 | No | 178 384 (all waves) | ADL/IADL | −1·38% | 0·01 |
| 1995–200485 | USA | >75 | 9 | No | 23 229 (all waves) | ADL | −1·46% | 0·01 |
| 1995–200485 | USA | >75 | 9 | No | 23 229 (all waves) | IADL | 1·06% | ns |
| 1992–200237 | Sweden | >77 | 10 | Yes | 537–561 | IADL | −0·70% | ns |
| 1992–200237 | Sweden | >77 | 10 | Yes | 537–561 | ADL | 0·70% | ns |
| 1977–199969 | USA | 79–88 | 22 | No | 177–174 | Women: ADL and function | −2·43% | 0·00 |
| 1977–199969 | USA | 79–88 | 22 | No | 103–119 | Men: ADL and function | −2·10% | 0·00 |
| 1895 cohort vs 1905 cohort79 | Denmark | >100 | 10 | Yes | 162–189 | Women: BADL | −1·19% | 0·01 |
| 1895 cohort vs 1905 cohort79 | Denmark | >100 | 10 | Yes | 45–36 | Men: BADL | 0·61% | ns |
Calculation of yearly change based on prevalences: (last year–first year)/first year/number of years in follow-up x100. Calculation of yearly change based on odds ratio: −(1−OR)/number of years in follow-up x100. Positive values show an increase in disability. Negative values show a reduction in disability. NHIS=National Health Interview Survey. ns=not significant. ADL=activities of daily living. IADL=instrumental activities of daily living. NLTCS=National Long Term Care Survey. BADL=basic activities of daily living.
In Japan, between 1993 and 2002, six of ten indices for ADL and instrumental ADL improved substantially after adjustment for age. Deterioration was mainly in disabilities affecting instrumental ADL. The proportion of people reporting any disability fell by 4·4% per year.70 For a general disability question about being hampered or disabled, a large yearly fall of 5·5% between 1991 and 1992, and between 2002 and 2003, was reported for France,81 after a smaller fall of 1·6% in the previous decade. Changes in survey design, methods of data collection, and exact wording of the question might have caused acceleration of the trend in the later period.
Two studies in Spain had contradictory results—ie, large yearly reductions of about 10% in prevalence of disabilities affecting ADL,68 and a worsening of an index of basic ADL by 0·5% for men and 1·9% for women per year,67 in the presence of strong improvements in functional limitations. Finland benefited from large reductions in risk disability affecting basic ADL. Between 1993 and 1995, and 2001 and 2003, the index decreased yearly by 6·3% for women and 5·1% for men.76 Small improvements are documented for the Netherlands36 and the USA.69,84,85 Contrary to the results of most studies, increases in disabilities affecting ADL and functional limitations are reported for elderly Swedish people, starting from the mid 1990s,71 after decreases between the 1980s and 1990s. Disabilities affecting ADL and instrumental ADL might be increasing in young old people in the UK47 and in baby boomers in the USA.49
Health expectancies
Health expectancies combine information about life expectancy and prevalence of good health, and thus directly address whether the period of morbidity or disability at the end of life is shortening or lengthening. Dependent on the measure of health, several health expectancies can be estimated:86 disease-free health expectancy, life expectancy in perceived good health, and disability-free life expectancy. Trends in these three measures differ. Life years with morbidity have been increasing in parallel with the increase in some diseases and conditions. Life years in good self-perceived health have been generally rising,87 whereas trends in life years with disability have evolved differently dependent on severity of disability: a decrease for the most severe levels of disability and an increase for the least severe levels.9 Additionally, several one-country studies exist, but comparative analysis has been hampered by scarcity of harmonised long-term surveys that include health measures.
The European Health Expectancy Monitoring Unit is developing a common indicator of disability-free life expectancy named healthy life years (HLY). Time trends are available for 14 European countries between 1995 and 2003. People whose answers to the European Community Household Panel question “Are you hampered in your daily activities by any physical or mental health problem, illness or disability?” were “moderate” or “severe” are defined as disabled. On the basis of this measure, differences in HLY in European countries are large. Even among countries with similar yearly rates of increase in life expectancy, some countries show a rise (men: Austria, Belgium, Italy, Finland, Germany; women: Belgium, Italy, Sweden), others stagnation (men: France, Greece, Ireland, Spain; women: Austria, Denmark, UK, Finland, France, Spain, UK) or reduction (men: Denmark, Portugal, Netherlands, Sweden, UK; women: Germany, Greece, Ireland, Netherlands, Portugal) in the proportion of life spent disability-free at ages 65 years and older.88
Inequalities in HLY are even larger if all 25 countries of the EU are considered:89 at age 50 years the range is 14·5 years in men, and 13·7 years in women. A metaregression with various macro-level indicators that cover the broad areas of wealth and expenditure, labour-force participation, and number of years of education shows that gross domestic product and expenditure on care for elderly people were positively associated with HLYs at age 50 years for both sexes, whereas for men only long-term employment was negatively and life-long learning positively associated. A series of studies have reported larger improvements in disability-free life expectancy than in life expectancy.1,39,67,90–92 A comparison of four health surveys in France93 concludes that gains in life expectancy over recent decades might have added years with moderate difficulties but not years with severe difficulties. This finding is lent support by reports from Germany94,95 and Belgium.92
Notably, almost all research about trends in health has been addressed to population averages that need not be typical of individual experience. Research in health has thus turned towards individual trajectories of health;96 application to time trends, however, is still missing. Continued improvement of health trajectories depends on improvement in elderly people, although the foundation for this progress might partly be based on enhanced living conditions and lifestyle early in life. Progress towards improvement of health is likely to depend on public health efforts to—for example, combat smoking, obesity, low levels of exercise, poor diets, and excess drinking, and to provide improved living conditions and care for elderly people with several ailments.97
Although mortality is higher for men than for women at all ages, women have more functional limitations and more difficulties with ADL and instrumental ADL. For women compared with men, both incidence and prevalence of limitations are higher at all ages. The male advantage has been substantiated by results of physical performance tests up to the highest ages, and is larger in nonagenarians and centenarians than in octogenarians.98 Sex differences in morbid conditions and diseases are more complex. For example, the increase in incidence of coronary heart disease starts about 10 years earlier in men than in women, but the male-female gap decreases after age 60 years and is small after 80 years. Women tend to have more reported symptoms, more non-life-threatening diseases, and more physical and psychological symptoms.98 The most common explanations of the health disadvantage of women pertain to differences in biology between men and women, illness and health behaviour and reporting, physicians’ diagnostic patterns, and health-care access, treatment, and use.
Time trends in disability and functional limitations usually apply to both sexes. With respect to disability affecting ADL or instrumental ADL, studies for the Netherlands,36 Spain,67 Finland,80 and Europe77 report larger reductions for women than for men, whereas in the USA69 equal trends are reported, although for mobility limitations men generally fared better than did women.
Consequences of mortality, disease, and disability
Are we living not only longer, but also better? Most evidence for people aged younger than 85 years suggests postponement of limitations and disabilities, despite an increase in chronic diseases and conditions. This apparent contradiction is at least partly accounted for by early diagnosis, improved treatment, and amelioration of prevalent diseases so that they are less disabling.1,6,11,99 An estimated 14–22% of the overall fall in disability can be attributed to reductions in disabilities associated with cardiovascular diseases.100 Trends in disability might also show underlying trends in other domains. The rising use of assistive technology and improvements in housing standards, public transport, accessibility of buildings, changes in social policies, shifting gender roles, and the social perception of disability also might have contributed to loosening of the link between disease and functional limitation or disability.4,11 Finally, increasing levels of educational attainment and income in elderly people, improved living and workplace conditions, reduced poverty, changes in marital status towards a rising proportion of couples in elderly people, and improvements in early childhood conditions might have contributed to the fall in disability.6,56 Hence, people aged younger than 85 years are living longer and, on the whole, are able to manage their daily activities for longer than were previous cohorts.
For people aged older than 85 years, the situation is less clear. Data are sparse and widespread concern exists that exceptional longevity has grim results both for individuals and for societies. The failure of success hypothesis states that a cohort with a rising proportion of individuals surviving to some late age will have increased disease and disability at that age. The alternative hypothesis is that exceptionally old people generally enjoy the success of success—ie, increases in the proportion of the population surviving to the highest ages are accompanied by concurrent postponements of physical and cognitive disability.
Data for exceptionally old people are few and inconsistent. Comparisons between centenarians from the Danish 1895–96 and 1905 cohorts suggest that although nearly 50% more people from the 1905 cohort reached age 100 years than did people in the 1895–96 cohort, no increase was reported in physical or cognitive disability level and, on the contrary, some improvement was detected for women.78,101 This finding is in agreement with research in young-elderly people (aged younger than 85 years) showing that prevalence of disability is decreasing and that individuals are not only living longer than they did in previous years, but also have improved functional states in successive cohorts because of prevention of disease and disabilities in addition to treatments and environmental changes compensating for consequences of disease.2,5,8,37,38,77,102,103
Other researchers have reported less encouraging results for exceptionally old people. Data from Japan, the country with the highest proportion of people surviving to age 100 years, suggest that more recent cohorts of Japanese centenarians have worse health than did previous cohorts.104 Cross-country and cross-sex comparisons also suggest that increased survival to the highest ages is associated with worse health; Danish centenarians have worse physical function than do Chinese centenarians, and female centenarians have worse function than do male centenarians.105 These findings are consistent with the common view in clinical medicine and among some gerontologists that the substantial rise in proportion of exceptionally long-lived individuals in successive birth cohorts is the result of help given to an increasing proportion of frail and ill people into advanced old age, with huge personal and societal costs.106
Even paediatric progress has generated worry. Gruenberg107 suggested that survival of frail children could lead to a geriatric failure of paediatric success. However, on the basis of analyses of US trends in self-reported health, Waidmann108 asserted that there was an illusion of failure: mortality reduction did not necessarily mean worsening of health in the population. Whether continued increases in survival to exceptionally-old age will lead to a failure of success or a success of success in the health of the oldest-old population remains to be seen.
Traditionally, man has three major periods of life: childhood, adulthood, and old age. Old age is now evolving into two segments, a third age (young old) and a fourth age (oldest old). Some students of ageing have asserted that the prospects for healthy longevity are poor.21,109,110 For example, Baltes and Smith106 envisioned that in the third age, functioning and dignity are usually conserved, whereas the fourth age will generally be characterised by vulnerability, with little identity, psychological autonomy, and personal control. The expectation is that developments will lead to an increasing number of individuals in successive birth cohorts reaching their tenth and 11th decades in frail states of health, with many existing in a vegetative state. In other words, exceptional longevity within a cohort is expected to lead to exceptional levels of oldest-old disability.
This hypothesis was tested in the Danish 1905 Cohort Survey, which longitudinally assessed the entire Danish 1905 cohort from 1998 to 2005.14 In the aggregate, this cohort had only a small reduction in the proportion of independent individuals at four assessments between age 92 and 100 years: 39%, 36%, 32%, and 33%—a nearly constant proportion of individuals in the cohort were independent over the 7–8 years of follow-up. However, for participants who survived until 2005, prevalence of independence fell by more than a factor of two—from 70% in 1998 to 33% in 2005. Similar results were obtained for other functional outcomes, such as grip strength, cognitive composite score, and symptoms of depression. Additional analyses of missing data due to death and non-response suggest that the discrepancy between population trajectory and individual trajectory is due to increased mortality in dependent individuals. Frail and disabled people die first, leaving the most robust in the cohort. Hence, overall characteristics of the cohort remain nearly unchanged.
The finding that 30–40% of a contemporary cohort of nonagenarians is independent from age 92–100 years might also be valid beyond age 100 years. In a study of 32 US supercentenarians (age 110–119 years), about 40% needed little assistance or were independent,111 suggesting that supercentenarians are not more disabled than are people aged 92 years. These studies do not accord with the prediction that the fourth age for man is in a vegetative state. On the contrary, findings suggest that the characteristics of a cohort do not change much between ages 92 and 100 years (and maybe even 119 years) in central domains, such as physical and cognitive functions.
The levelling off in disability level for a cohort at the highest ages suggests that care costs per individual do not increase in the tenth and 11th decades of life. Lubitz and colleagues112 showed that the expected cumulative lifetime health expenditures for individuals in good health at age 70 years were not greater than were expenditures for less healthy people, despite greater longevity of healthier elderly people. Thus, health promotion efforts aimed at people aged 65 years and younger might improve health and longevity of elderly people without increasing health expenditure. Individuals who survive longest have a health profile that is, in many respects, similar to that of individuals who are a decade or so younger. This finding suggests that most individuals can expect to deteriorate physically before death, but postponement of this process enables people to live to advanced ages without great disability.
Population ageing poses severe challenges for the traditional social welfare state. An often-used indicator is the old-age dependency ratio, which divides the number of people at retirement ages (>65 years) by the number of people at working ages (15–64 years). In Germany in 1956, there were about 15–16 pensioners for every 100 people at working ages. Half a century later, there were 29 people aged older than 65 years for every 100 people aged 15–64 years. The German Federal Statistical Office33 projects another doubling of this index to about 60, half a century from now. Large increases in both number and proportion of elderly individuals are forthcoming not only in Germany but also in other European countries, Japan, the USA, and many other countries. Population ageing is a worldwide occurrence.
A reasonable strategy to cope with the economic implications of population ageing is to raise the typical age of retirement, and most governments are moving in this direction. Improvements in health and functioning along with shifting of employment from jobs that need strength to jobs needing knowledge imply that a rising proportion of people in their 60s and 70s are capable of contributing to the economy. Because many people in their 60s and 70s would prefer part-time work to full-time labour, an increase in jobs that need 15, 20, or 25 h of work per week seems likely. If part-time work becomes common for elderly people, then more opportunities for part-time work might open up for young people. If people in their 60s and early 70s worked much more than they do nowadays, then most people could work fewer hours per week than is currently common—if they worked correspondingly more years of their longer lives. The average amount of work per year of life could stay at about the same as it is at present.113
The 20th century was a century of redistribution of income. The 21st century could be a century of redistribution of work. Redistribution would spread work more evenly across populations and over the ages of life. Individuals could combine work, education, leisure, and child-rearing in varying amounts at different ages. This vision is starting to receive some preliminary attention.113 Preliminary evidence suggests that shortened working weeks over extended working lives might further contribute to increases in life expectancy and health. Redistribution of work will, however, not be sufficient to meet the coming challenges. Even if the health of individuals at any particular age improves, there could be an increased total burden if the number of individuals at that age rises sufficiently. Health care often needs service sector or family-member labour by individuals; this labour is not easily substituted by machines, although assistive technology is likely to reduce the need for personal care in high-income countries.114,115
Very long lives are not the distant privilege of remote future generations—very long lives are the probable destiny of most people alive now in developed countries (table 1).12 Increasing numbers of people at old and very old ages will pose major challenges for health-care systems. Present evidence, however, suggests that people are not only living longer than they did previously, but also they are living longer, with less disability and fewer functional limitations.
Search strategy and selection criteria
A series of reviews has dealt with population ageing and trends in health in the USA1–6 and internationally.7–11 This Review builds on this work and includes new evidence available since 2004 from the International Network on Health Expectancies and Disability Process, the TRENDS network, and reports identified in PubMed and reference lists. We searched PubMed for reports published in 2005 and later using the search terms “active life expectancy”, “BMI/body mass index”, “chronic conditions”, “cognitive functioning”, “diabetes”, “disability free life”, “expectancy”, “disability”, “elderly”, “functioning”, “health expectancy”, “health”, “hypertension”, “impairment”, “incidence”, “life expectancy”, “limitation”, “longevity”, “mobility”, “mortality”, “(multi) morbidity”, “old age”, “overweight”, “physical activity”, “prevalence”, “self rated health”, “stroke”, and “trends”. We also included frequently cited older reports. To include the newest available demographic data, we used the Human Mortality Database.
Acknowledgments
We thank Bernard Jeune for his helpful comments and suggestions. KC and JWV are supported by a grant from NIH/NIA, Grant No P01 AG08761. The Danish Ageing Research Centre is supported by a grant from the VELUX foundation.
Footnotes
For the Human Mortality Database see http://www.mortality.org/
Contributors
All authors contributed to the design of the Review. KC and JWV provided the outline. GD and RR were responsible for data acquisition and analysis. All authors contributed to drafting and critical revision.
Conflicts of interest
We declare that we have no conflicts of interest.
References
- 1.Crimmins EM. Trends in the health of the elderly. Annu Rev Public Health. 2004;25:79–98. doi: 10.1146/annurev.publhealth.25.102802.124401. [DOI] [PubMed] [Google Scholar]
- 2.Freedman VA, Martin LG, Schoeni RF. Recent trends in disability and functioning among older adults in the United States: a systematic review. JAMA. 2002;288:3137–246. doi: 10.1001/jama.288.24.3137. [DOI] [PubMed] [Google Scholar]
- 3.Spillman BC. Changes in elderly disability rates and the implications for health care utilization and cost. Milbank Q. 2004;82:157–94. doi: 10.1111/j.0887-378X.2004.00305.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wolf DA, Hunt K, Knickman J. Perspectives on the recent decline in disability at older ages. Milbank Q. 2005;83:365–95. doi: 10.1111/j.1468-0009.2005.00406.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Manton KG. Recent declines in chronic disability in the elderly US population: risk factors and future dynamics. Annu Rev Public Health. 2008;29:91–113. doi: 10.1146/annurev.publhealth.29.020907.090812. [DOI] [PubMed] [Google Scholar]
- 6.Schoeni RF, Freedman VA, Martin LG. Why is late-life disability declining? Milbank Q. 2008;86:47. doi: 10.1111/j.1468-0009.2007.00513.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jacobzone S, Cambois E, Robine JM. Is the health of older persons in OECD countries improving fast enough to compensate for population ageing? OECD Economic Studies. 2000;30:149–90. [Google Scholar]
- 8.Robine JM, Michel JP. Looking forward to a general theory on population aging. J Gerontol A Biol Sci Med Sci. 2004;59:M590–97. doi: 10.1093/gerona/59.6.m590. [DOI] [PubMed] [Google Scholar]
- 9.Robine J-M, Romieu I, Michel JP. Trends in health expectancies. In: Robine J-M, Jagger C, Mathers CD, Crimmins EM, Suzman RM, editors. Determining health expectancies. Chichester: John Wiley & Sons; 2003. pp. 75–104. [Google Scholar]
- 10.Wen X. Trends in the prevalence of disability and chronic conditions among the older population: implications for survey design and measurement of disability. Aust J Ageing. 2004;23:3–6. [Google Scholar]
- 11.Parker MG, Thorslund M. Health trends in the elderly population: getting better and getting worse. Gerontologist. 2007;47:150. doi: 10.1093/geront/47.2.150. [DOI] [PubMed] [Google Scholar]
- 12.Oeppen J, Vaupel JW. Broken limits to life expectancy. Science. 2002;296:1029–31. doi: 10.1126/science.1069675. [DOI] [PubMed] [Google Scholar]
- 13.Engberg H, Oksuzyan A, Jeune B, Vaupel JW, Christensen K. Centenarians—a useful model for healthy aging? A 29 year follow-up of hospitalizations among 40 000 Danes born in 1905. Aging Cell. 2009;8:270–76. doi: 10.1111/j.1474-9726.2009.00474.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Christensen K, McGue M, Petersen I, Jeune B, Vaupel JW. Exceptional longevity does not result in excessive levels of disability. Proc Natl Acad Sci USA. 2008;105:13274–79. doi: 10.1073/pnas.0804931105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vaupel JW, Carey JR, Christensen K, et al. Biodemographic trajectories of longevity. Science. 1998;280:855–60. doi: 10.1126/science.280.5365.855. [DOI] [PubMed] [Google Scholar]
- 16.Suzman RM, Willis DP, Manton KG. The oldest old. New York: Oxford University Press; 1992. [Google Scholar]
- 17.Smith J. Well-being and health from age 70 to 100 years: findings from the Berlin Aging Study. Eur Rev. 2001;9:461–77. [Google Scholar]
- 18.Suzman R, Riley MW. Introducing the “oldest old”. Milbank Mem Fund Q Health Soc. 1985;63:177–86. [PubMed] [Google Scholar]
- 19.Ministry of Health, Labour, and Welfare, Japan. [accessed July 25, 2009];Life tables. 2009 http://www.mhlw.go.jp/english/database/db-hw/vs02.html.
- 20.Fries JF. Aging, natural death and the compression of morbidity. N Engl J Med. 1980;303:130–35. doi: 10.1056/NEJM198007173030304. [DOI] [PubMed] [Google Scholar]
- 21.Olshansky SJ, Carnes BA, Désesguelles A. Prospects for longevity. Science. 2001;291:1491–92. doi: 10.1126/science.291.5508.1491. [DOI] [PubMed] [Google Scholar]
- 22.Kannisto V. Monographs on population aging 1. Odense: Odense University Press; 1994. Development of oldest-old mortality, 1950–1990: evidence from 28 developed countries. [Google Scholar]
- 23.Kannisto V. Monographs on population aging 3. Odense: Odense University Press; 1996. The advancing frontier of survival. [Google Scholar]
- 24.Kannisto V, Lauritsen J, Thatcher AR, Vaupel JW. Reductions in mortality at advanced ages: several decades of evidence from 27 countries. Popul Dev Rev. 1994;20:793–810. [Google Scholar]
- 25.Vaupel JW. The remarkable improvements in survival at older ages. Philos Trans R Soc Lond B Biol Sci. 1997;352:1799–804. doi: 10.1098/rstb.1997.0164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rau R, Soroko E, Jasilionis D, Vaupel JW. Continued reductions in mortality at advanced ages. Popul Dev Rev. 2008;34:747–68. [Google Scholar]
- 27.Max Planck Institute for Demographic Research. [accessed Sept 12, 2009];Kannisto-Thatcher Database on Old Age Mortality. http://www.demogr.mpg.de/databases/ktdb.
- 28.Manton KG, Vaupel JW. Survival after the age of 80 in the United States, Sweden, France, England, and Japan. N Engl J Med. 1995;333:1232–35. doi: 10.1056/NEJM199511023331824. [DOI] [PubMed] [Google Scholar]
- 29.Wang H, Preston SH. Forecasting United States mortality using cohort smoking histories. Proc Natl Acad Sci USA. 2009;106:393–98. doi: 10.1073/pnas.0811809106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Juel K, Sørensen J, Brønnum-Hansen H. Risk factors and public health in Denmark. Scand J Public Health. 2008;36 (suppl 1):11–227. doi: 10.1177/1403494808097590. [DOI] [PubMed] [Google Scholar]
- 31.Juel K. Life expectancy and mortality in Denmark compared to Sweden. What is the effect of smoking and alcohol? Ugeskr Laeger. 2008;170:2423–27. [PubMed] [Google Scholar]
- 32.Preston SH, Himes C, Eggers M. Demographic conditions responsible for population aging. Demography. 1989;26:691–704. [PubMed] [Google Scholar]
- 33.Statistisches Bundesamt, Wiesbaden, Germany. Statistisches Bundesamt 2006. Bevölkerung Deutschlands bis 2050. Ergebnisse der 11 koordinierten Bevölkerungsvoraus-berechnung.
- 34.Verbrugge LM, Jette AM. The disablement process. Soc Sci Med. 1994;38:1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- 35.Vallin J, Meslé F. Convergences and divergences: an analytical framework of national and sub-national trends in life expectancy. Genus. 2005;61:83–123. [Google Scholar]
- 36.Puts MTE, Deeg DJH, Hoeymans N, Nusselder WJ, Schellevis FG. Changes in the prevalence of chronic disease and the association with disability in the older Dutch population between 1987 and 2001. Age Ageing. 2008;37:187–93. doi: 10.1093/ageing/afm185. [DOI] [PubMed] [Google Scholar]
- 37.Parker MG, Ahacic K, Thorslund M. Health changes among Swedish oldest old: prevalence rates from 1992 and 2002 show increasing health problems. J Gerontol A Biol Sci Med Sci. 2005;60:1351–55. doi: 10.1093/gerona/60.10.1351. [DOI] [PubMed] [Google Scholar]
- 38.Crimmins EM, Alley D, Reynolds SL, Johnston M, Karlamangla A, Seeman T. Changes in biological markers of health: older Americans in the 1990s. J Gerontol A Biol Sci Med Sci. 2005;60:1409–13. doi: 10.1093/gerona/60.11.1409. [DOI] [PubMed] [Google Scholar]
- 39.Jeune B, Brønnum-Hansen H. Trends in health expectancy at age 65 for various health indicators, 1987–2005, Denmark. Eur J Ageing. 2008;5:279–85. doi: 10.1007/s10433-008-0100-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Crimmins EM, Saito Y. Change in the prevalence of diseases among older Americans: 1984–1994. Demogr Res. 2000;3:9. [Google Scholar]
- 41.Freedman VA, Martin LG. Contribution of chronic conditions to aggregate changes in old-age functioning. J Am Public Health Assoc. 2000;90:1755–60. doi: 10.2105/ajph.90.11.1755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lafortune G, Balestat G. Trends in severe disability among elderly people: assessing the evidence in 12 OECD countries and the future implications (OECD health working paper, No 26) Paris: Organisation for Economic Co-operation and Development; 2007. [Google Scholar]
- 43.Rosen M, Haglund B. From healthy survivors to sick survivors—implications for the twenty-first century. Scand J Public Health. 33:151–55. doi: 10.1080/14034940510032121. [DOI] [PubMed] [Google Scholar]
- 44.Fors S, Lennartsson C, Lundberg O. Health inequalities among older adults in Sweden 1991–2002. Eur J Public Health. 2008;18:138–43. doi: 10.1093/eurpub/ckm097. [DOI] [PubMed] [Google Scholar]
- 45.Meinow B, Parker M, Kåreholt I, Thorslund M. Complex health problems in the oldest old in Sweden 1992–2002. Eur J Ageing. 2006;3:98–106. doi: 10.1007/s10433-006-0027-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Karim-Kos HE, de Vries E, Soerjomataram I, Lemmens V, Siesling S, Coebergh JWW. Recent trends of cancer in Europe: a combined approach of incidence, survival and mortality for 17 cancer sites since the 1990s. Eur J Cancer. 2008;44:1345–89. doi: 10.1016/j.ejca.2007.12.015. [DOI] [PubMed] [Google Scholar]
- 47.Jagger C, Matthews R, Matthews F, et al. Cohort differences in disease and disability in the young-old: findings from the MRC Cognitive Function and Ageing Study (MRC-CFAS) BMC Public Health. 2007;7:156. doi: 10.1186/1471-2458-7-156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bhattacharya J, Choudhry K, Lakdawalla D. Chronic disease and trends in severe disability in working age populations. Med Care. 2008;46:92–100. doi: 10.1097/MLR.0b013e3181484335. [DOI] [PubMed] [Google Scholar]
- 49.Martin LG, Freedman VA, Schoeni RF, Andreski PM. Health and functioning among baby boomers approaching 60. J Gerontol B Psychol Sci Soc Sci. 2009;64:369–77. doi: 10.1093/geronb/gbn040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Paul SL, Srikanth VK, Thrift AG. The large and growing burden of stroke. Curr Drug Targets. 2007;8:786–93. doi: 10.2174/138945007781077418. [DOI] [PubMed] [Google Scholar]
- 51.Lakdawalla DN, Bhattacharya J, Goldman DP. Are the young becoming more disabled? Health A3. 2004;23:168–76. doi: 10.1377/hlthaff.23.1.168. [DOI] [PubMed] [Google Scholar]
- 52.Peeters A, Barendregt JJ, Willekens F, Mackenbach JP, Mamun AA, Bonneux L. Obesity in adulthood and its consequences for life expectancy: a life-table analysis. Ann Intern Med. 2003;138:24–32. doi: 10.7326/0003-4819-138-1-200301070-00008. [DOI] [PubMed] [Google Scholar]
- 53.Sturm R, Ringel JS, Andreyeva T. Increasing obesity rates and disability trends. Health A3. 2004;23:199–205. doi: 10.1377/hlthaff.23.2.199. [DOI] [PubMed] [Google Scholar]
- 54.Olshansky SJ, Passaro DJ, Hershow RC, et al. A potential decline in life expectancy in the United States in the 21th century. N Engl J Med. 2005;352:1138–45. doi: 10.1056/NEJMsr043743. [DOI] [PubMed] [Google Scholar]
- 55.Doblhammer G, Hoffmann R, Muth E, Westphal C, Kruse A. A systematic literature review of studies analyzing the effect of sex, age, education, marital status, obesity, and smoking on health transitions. Demogr Res. 2009;20:37–64. [Google Scholar]
- 56.Reynolds SL, Saito Y, Crimmins EM. The impact of obesity on active life expectancy in older American men and women. Gerontologist. 2005;45:438–44. doi: 10.1093/geront/45.4.438. [DOI] [PubMed] [Google Scholar]
- 57.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27:1047–53. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 58.Zamboni M, Mazzali G, Zoico E, et al. Health consequences of obesity in the elderly: a review of four unresolved questions. Int J Obes. 2005;29:1011–29. doi: 10.1038/sj.ijo.0803005. [DOI] [PubMed] [Google Scholar]
- 59.Ong KL, Cheung BMY, Man YB, Lau CP, Lam KSL. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999–2004. Hypertension. 2007;49:69–75. doi: 10.1161/01.HYP.0000252676.46043.18. [DOI] [PubMed] [Google Scholar]
- 60.Alley DE, Chang VW, Doshi J. The shape of things to come: obesity, aging, and disability. LDI Issue Brief. 2008;13:1. [PubMed] [Google Scholar]
- 61.Alley DE, Chang VW. The changing relationship of obesity and disability, 1988–2004. JAMA. 2007;298:2020–27. doi: 10.1001/jama.298.17.2020. [DOI] [PubMed] [Google Scholar]
- 62.Ostchega Y, Dillon CF, Hughes JP, Carroll M, Yoon S. Trends in hypertension prevalence, awareness, treatment, and control in older US adults: data from the National Health and Nutrition Examination Survey 1988 to 2004. J Am Geriatr Soc. 2007;55:1056. doi: 10.1111/j.1532-5415.2007.01215.x. [DOI] [PubMed] [Google Scholar]
- 63.Qureshi AI, Suri MFK, Kirmani JF, Divani AA. Prevalence and trends of prehypertension and hypertension in United States: National Health and Nutrition Examination Surveys 1976 to 2000. Med Sci Monit. 2005;11:CR403–09. [PubMed] [Google Scholar]
- 64.Rodgers WL, Ofstedal MB, Herzog AR. Trends in scores on tests of cognitive ability in the elderly U.S. population, 1993–2000. J Gerontol B Psychol Sci Soc Sci. 2003;58:S338–46. doi: 10.1093/geronb/58.6.s338. [DOI] [PubMed] [Google Scholar]
- 65.Manton KG, Lamb VL. Mortality and disability trajectories above age 90 in the U.S. 1982–2004. International Union for the Scientific Study of Population, XXV International Population Conference; Tours, France. July 18–23, 2005. [Google Scholar]
- 66.Langa KM, Larson EB, Karlawish JH, et al. Trends in the prevalence and mortality of cognitive impairment in the United States: is there evidence of a compression of cognitive morbidity? Alzheimers Dement. 2008;4:134–44. doi: 10.1016/j.jalz.2008.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sagardui-Villamor J, Guallar-Castillon P, Garcia-Ferruelo M, Banegas JR, Rodriguez-Artalejo F. Trends in disability and disability-free life expectancy among elderly people in Spain: 1986–1999. J Gerontol A Biol Sci Med Sci. 2005;60:1028–34. doi: 10.1093/gerona/60.8.1028. [DOI] [PubMed] [Google Scholar]
- 68.Zunzunegui MV, Nunez O, Durban M, García de Yébenes M-J, Otero Á. Decreasing prevalence of disability in activities of daily living, functional limitations and poor self-rated health: a 6-year follow-up study in Spain. Aging Clin Exp Res. 2006;18:352–58. doi: 10.1007/BF03324830. [DOI] [PubMed] [Google Scholar]
- 69.Murabito JM, Pencina MJ, Zhu L, Kelly-Hayes M, Shrader P, D’Agostino RB., Sr Temporal trends in self-reported functional limitations and physical disability among the community-dwelling elderly population: the Framingham Heart Study. Am J Public Health. 2008;98:1256–62. doi: 10.2105/AJPH.2007.128132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Schoeni B, Liang J, Bennett H, Sugisawa H, Fukaya T, Kobayash E. Trends in old-age functioning and disability in Japan 1993–2002. Popul Stud (Camb) 2006;60:39–54. doi: 10.1080/00324720500462280. [DOI] [PubMed] [Google Scholar]
- 71.Parker MG, Schön P, Lagergren M, Thorslund M. Functional ability in the elderly Swedish population from 1980 to 2005. Eur J Ageing. 2008;5:299–309. doi: 10.1007/s10433-008-0096-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Desai M, Pratt LA, Lentzner H, Robinson KN. Trends in vision and hearing among older Americans. Aging Trends. 2001;2:1–8. doi: 10.1037/e620682007-001. [DOI] [PubMed] [Google Scholar]
- 73.Freedman VA, Martin LG. Understanding trends in functional limitations among older Americans. Am J Public Health. 1998;88:1457–62. doi: 10.2105/ajph.88.10.1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Freedman VA, Schoeni RF, Martin LG, Cornman JC. Chronic conditions and the decline in late-life disability. Demography. 2007;44:459–77. doi: 10.1353/dem.2007.0026. [DOI] [PubMed] [Google Scholar]
- 75.Spalton D, Koch D. The constant evolution of cataract surgery. BMJ. 2000;321:1304. doi: 10.1136/bmj.321.7272.1304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sulander TT, Rahkonen OJ, Uutela AK. Functional ability in the elderly Finnish population: time period differences and associations, 1985–1999. Scand J Public Health. 2003;31:100–06. doi: 10.1080/14034940210133933. [DOI] [PubMed] [Google Scholar]
- 77.Äijänseppä S, Notkola I-L, Tijhuis M, van Staveren W, Kromhout D, Nissinen A. Physical functioning in elderly Europeans: 10 year changes in the north and south: the HALE project. J Epidemiol Community Health. 2005;59:413–19. doi: 10.1136/jech.2004.026302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ahacic K, Parker MG, Thorsland M. Mobility limitations 1974–1991: period changes explaining improvement in the population. Soc Sci Med. 2003;57:2411–22. doi: 10.1016/s0277-9536(03)00136-9. [DOI] [PubMed] [Google Scholar]
- 79.Engberg H, Christensen K, Andersen-Ranberg K, Vaupel JW, Jeune B. Improving activities of daily living in Danish centenarians—but only in women: a comparative study of two birth cohorts born in 1895 and 1905. J Gerontol A Biol Sci Med Sci. 2008;63:1186–92. doi: 10.1093/gerona/63.11.1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Sulander T, Martelin T, Sainio P, Rahkonen O, Nissinen A, Uutela A. Trends and educational disparities in functional capacity among people aged 65–84 years. Int J Epidemiol. 2006;35:1255–61. doi: 10.1093/ije/dyl183. [DOI] [PubMed] [Google Scholar]
- 81.Cambois E, Robine JM, Mormiche P. Did the prevalence of disability in France really fall sharply in the 1990s: a discussion of questions asked in the French Health Survey. Population. 2007;62:315–38. [Google Scholar]
- 82.Manton KG, Gu X, Lamb VL. Change in chronic disability 1982 to 2004/2005 as meaured by long-term changes in function and health in the US elderly population. Proc Natl Acad Sci USA. 2006;103:18374–79. doi: 10.1073/pnas.0608483103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Freedman VA, Crimmins E, Schoeni RF, et al. Resolving inconsistencies in trends in old-age disability: report from a technical working group. Demography. 2004;41:417–41. doi: 10.1353/dem.2004.0022. [DOI] [PubMed] [Google Scholar]
- 84.Martin LG, Schoeni RF, Freedman VA, Andreski P. Feeling better? Trends in general health status. J Gerontol B Psychol Sci Soc Sci. 2007;62:S11–21. doi: 10.1093/geronb/62.1.s11. [DOI] [PubMed] [Google Scholar]
- 85.Freedman VA, Martin LG, Schoeni RF, Cornman JC. Declines in late-life disability: The role of early-and mid-life factors. Soc Sci Med. 2008;66:1588–602. doi: 10.1016/j.socscimed.2007.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Robine JM. A new health expectancy classification system. In: Murray CJL, Salomon JA, Mathers CD, Lopez AD, editors. Summary measures of population health. Geneva: World Health Organization; 2002. pp. 205–12. [Google Scholar]
- 87.Doblhammer G, Kytir J. Compression or expansion of morbidity? Trends in healthy-life expectancy the elderly Austrian population between 1978 and 1998. Soc Sci Med. 2001;52:385–91. doi: 10.1016/s0277-9536(00)00141-6. [DOI] [PubMed] [Google Scholar]
- 88.Van Oyen H. Living longer healthier lives, comments on the changes in life expectancy and disability free life expectancy in the European Union since 1995. In: Robine J-M, Jagger C, van Oyen H, et al., editors. Are we living longer healthier lifes in the EU? Disability-free life expectancy (DFLE) in EU countries from 1991 to 2003 based on the European Household Panel (ECHP) EHEMU Technical Report 2. Montpellier: EHEMU; 2005. pp. 1–29. [Google Scholar]
- 89.Jagger C, Gillies C, Moscone F, et al. the EHLEIS team. Inequalities in healthy life years in the 25 countries of the European Union in 2005: a cross-national meta-regression analysis. Lancet. 2008;372:2124–31. doi: 10.1016/S0140-6736(08)61594-9. [DOI] [PubMed] [Google Scholar]
- 90.Mathers CD, Sadana R, Salomon JA, Murray CJL, Lopez AD. Healthy life expectancy in 191 countries, 1999. Lancet. 2001;357:1685–91. doi: 10.1016/S0140-6736(00)04824-8. [DOI] [PubMed] [Google Scholar]
- 91.Robine JM. Trends in population health. Aging Clin Exp Res. 2006;18:349–51. doi: 10.1007/BF03324829. [DOI] [PubMed] [Google Scholar]
- 92.Van Oyen H, Cox B, Demarest S, Deboosere P, Lorant V. Trends in health expectancy indicators in the older adult population in Belgium between 1997 and 2004. Eur J Ageing. 2008;5:137–46. doi: 10.1007/s10433-008-0082-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Cambois E, Clavel A, Romieu I, Robine JM. Trends in disability-free life expectancy at age 65 in France: consistent and diverging patterns according to the underlying disability measure. Eur J Ageing. 2008;5:287–98. doi: 10.1007/s10433-008-0097-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Doblhammer G, Ziegler U. Alter(n) und Gesellschaft. Future elderly living conditions in Europe: demographic aspects. In: Baltes GM, Lasch V, Reimann K, editors. Gender, health and ageing European perspectives on life Course, health issues and social challenges. 2006. [Google Scholar]
- 95.Unger R. Trends in active life expectancy in Germany between 1984 and 2003—a cohort analysis with different health indicators. J Public Health. 2006;14:155–63. [Google Scholar]
- 96.Doblhammer G, Hoffmann R. Gender differences in trajectories of health limitations and subsequent mortality. A study based on the German socioeconomic panel 1995–2001 with a mortality follow-up 2002–2005. J Gerontol B Psychol Sci Soc Sci. 2009 doi: 10.1093/geronb/gbp051. published online June 29. [DOI] [PubMed] [Google Scholar]
- 97.Riley JC. Rising life expectancy: a global history. New York: Cambridge University Press; 2001. [Google Scholar]
- 98.Oksuzyan O, Juel K, Vaupel JW, Christensen K. Men: good health and high mortality. Sex differences in health and aging. Aging Clin Exp Res. 2008;20:91–102. doi: 10.1007/bf03324754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Perenboom RJM, Van Herten LM, Boshuizen HC, Van Den Bos GAM. Trends in disability-free life expectancy. Disabil Rehabil. 2004;26:377–86. doi: 10.1080/0963828032000174098. [DOI] [PubMed] [Google Scholar]
- 100.Cutler DM, Landrum MB, Stewart K. NBER Working Paper No 12184. New York: National Bureau of Economic Research; 2006. Intensive medical care and cardiovascular disease disability reductions. [Google Scholar]
- 101.Engberg H, Christensen K, Andersen-Ranberg K, Jeune B. Cohort changes in cognitive function among Danish centenarians. A comparative study of 2 birth cohorts born in 1895 and 1905. Dement Geriatr Cogn Disord. 2008;26:153–60. doi: 10.1159/000149819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Manton KG, Corder L, Stallard E. Chronic disability trends in elderly United States populations: 1982–1994. Proc Natl Acad Sci USA. 1997;94:2593–98. doi: 10.1073/pnas.94.6.2593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Manton KG, Gu X. Changes in the prevalence of chronic disability in the United States black and nonblack population above age 65 from 1982 to 1999. Proc Natl Acad Sci USA. 2001;98:6354–59. doi: 10.1073/pnas.111152298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Suzuki M, Akisaka M, Ashitomi I, Higa K, Nozaki H. Chronological study concerning ADL among Okinawan centenarians. Nippon Ronen Igakkai Zasshi. 1995;32:416. doi: 10.3143/geriatrics.32.416. [DOI] [PubMed] [Google Scholar]
- 105.Wang Z, Zeng Y, Jeune B, Vaupel JW. A demographic and health profile of centenarians in China. In: Robine JM, Vaupel JW, Jeune B, Allard M, editors. Longevity: to the limits and beyond. New York: Springer; 1997. pp. 91–104. [Google Scholar]
- 106.Baltes PB, Smith J. New frontiers in the future of aging: from successful aging of the young old to the dilemmas of the fourth age. Gerontology. 2003;49:123–35. doi: 10.1159/000067946. [DOI] [PubMed] [Google Scholar]
- 107.Gruenberg EM. The failures of success. Milbank Mem Fund Q Health Soc. 1997;55:3–24. [PubMed] [Google Scholar]
- 108.Waidmann T, Bound J, Schoenbaum M. The illusion of failure: trends in the self-reported health of the US elderly. Milbank Q. 1995;73:253–87. [PubMed] [Google Scholar]
- 109.Hayflick L. Living forever and dying in the attempt. Exp Gerontol. 2003;38:1231–41. doi: 10.1016/j.exger.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 110.Hayflick L. Entropy explains aging, genetic determinism explains longevity, and undefined terminology explains misunderstanding both. PLoS Genet. 2007;3:e220. doi: 10.1371/journal.pgen.0030220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Schoenhofen EA, Wyszynski DF, Andersen S, et al. Characteristics of 32 supercentenarians. J Am Geriatr Soc. 2006;54:1237–40. doi: 10.1111/j.1532-5415.2006.00826.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Lubitz J, Cai L, Kramarow E, Lentzner H. Health, life expectancy, and health care spending among the elderly. N Engl J Med. 2003;349:1048–55. doi: 10.1056/NEJMsa020614. [DOI] [PubMed] [Google Scholar]
- 113.Vaupel JW, Loichinger E. Redistributing work in aging Europe. Science. 2006;312:1911–13. doi: 10.1126/science.1127487. [DOI] [PubMed] [Google Scholar]
- 114.Agree EM, Freedman VA, Cornman JC, Wolf DA, Marcotte JE. Reconsidering substitution in long-term care: when does assistive technology take the place of personal care? J Gerontol B Psychol Sci Soc Sci. 2005;60:S272–80. doi: 10.1093/geronb/60.5.s272. [DOI] [PubMed] [Google Scholar]
- 115.Freedman VA, Agree EM, Martin LG, Cornman JC. Trends in the use of assistive technology and personal care for late-life disability, 1992–2001. Gerontologist. 2006;46:124–27. doi: 10.1093/geront/46.1.124. [DOI] [PubMed] [Google Scholar]