Abstract
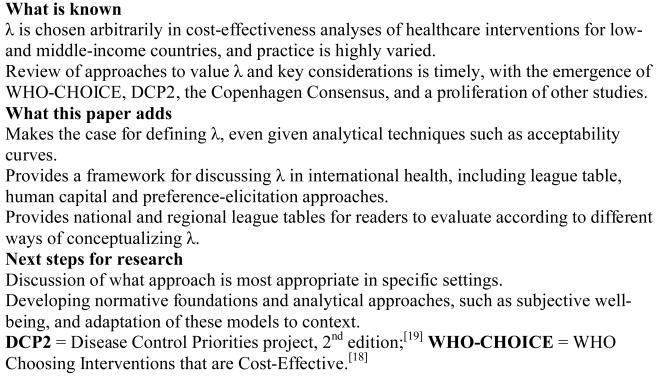
Cost-effectiveness analysis (CEA) is increasingly important in public health decision making, including in low- and middle-income countries. The decision makers' valuation of a unit of health gain, or ceiling ratio (λ), is important in CEA as the relative value against which acceptability is defined, although values are usually chosen arbitrarily in practice. Reference case estimates for λ are useful to promote consistency, facilitate new developments in decision analysis, compare estimates against benefit-cost ratios from other economic sectors, and explicitly inform decisions about equity in global health budgets.
The aim of this article is to discuss values for λ used in practice, including derivation based on affordability expectations (such as $US150 per disability-adjusted life-year [DALY]), some multiple of gross national income or gross domestic product, and preference-elicitation methods, and explore the implications associated with each approach. The background to the debate is introduced, the theoretical bases of current values are reviewed, and examples are given of their application in practice. Advantages and disadvantages of each method for defining λ are outlined, followed by an exploration of methodological and policy implications.
Cost-effectiveness analysis (CEA) is increasingly considered in public health decision making in low- and middle-income countries (LMICs), as reflected in the growing number of published studies.[1-15] It has been used in several prioritization exercises, such as the World Bank Health Sector Priorities Review (HSPR),[16,17] the WHO Choosing Interventions that are Cost-Effective (WHO-CHOICE) initiative,[18] the second edition of the Disease Control Priorities Project (DCP2)[19] and the Copenhagen Consensus.[20] The ceiling ratio (λ), or decision rule, is an important component of CEA, representing a decision maker's valuation of a unit of health gain, or the relative value against which the acceptability of incremental cost-effectiveness ratios (ICERs) is judged. The value of λ that is appropriate may be heavily contingent upon epidemiological, medical, political, ethical, cultural, budgetary and other factors, and therefore is likely to vary across time and space, but is usually chosen arbitrarily in practice. In addition, λ is not a strict decision-making criterion, and trade-offs between cost-effectiveness and other important decision-making factors are usually relevant.[21-23]
Cost-effectiveness acceptability curves (CEACs) have been developed as a technical approach that absolves analysts from committing to a fixed value for λ.[24,25] Nevertheless, reference case estimates for λ are often useful for political and analytical reasons. Decision makers may wish to be consistent with other administrative bodies or their own former choices, and an explicit and transparent normative definition may reduce the risk of repercussions from unpopular decisions.[26,27] More broadly, estimates for λ allow decision makers to convert outcomes to a metric that can be compared across economic sectors, as in the Copenhagen Consensus.[28] Technically, a reference case estimate for λ is necessary for some applications of decision analysis, such as expected value of perfect information (EVPI) analysis,[29,30] or cost-effectiveness probability planes that evaluate uncertainty in several dimensions.[31] Explicit definitions of λ are also useful for normative budgeting processes and debates about equity, which can promote public confidence in decision-making bodies.[32] Stimulation of public debate can lead to better hinformed and more rational policies about what the threshold should be (figure 1).[26]
Figure I.
Main messages
In evaluations of interventions affecting LMICs, selection of λ has been left largely to the discretion of the analyst, resulting in relatively arbitrary applications. In early studies, many analysts presented results simply in terms of cost per life saved or per unit of health gain, usually arguing for the cost-effectiveness of the intervention and thus inferring an implicit value for λ.[4] Others compared ICERs with that of an intervention representative of the least-cost alternative to save a life,[33] or to ICERs from other representative interventions to argue for cost-effectiveness.[4] In several analyses, $US150 per disability-adjusted life-year (DALY) has been used as a rough benchmark for λ.[34-43] Recent studies have used some multiple of per capita gross national income (GNI), stimulated by the approach of the Commission on Macroeconomics and Health (CMH),[44-48] or some multiple of gross domestic product (GDP), as applied by WHO-CHOICE.[5-15] However, it can be argued that people value life in dimensions that extend beyond income. For example, Jeffrey Sachs[44] argued in the CMH report that the costs of HIV/AIDS go well beyond income losses given the high and rapidly expanding burden of disease, affecting especially people in the prime of life. Willingness to pay (WTP) for health gain, and willingness to accept (WTA) increased risk of death, are more holistic approaches to valuing health improvements, and underlie the ‘full income’ estimates advocated by Jamison et al. in DCP2.[19] We are not aware of any LMIC CEAs that evaluate results according to WTP/WTA-based λ values, although some cost-benefit analyses (CBA) have valued health outcomes using contingent valuation.[4]
The aim of this article is to discuss different definitions of λ, including derivation from an expected budget, some multiple of GNI or GDP, and preference-elicitation methods, and to explore their implications. Values used in the WHO-CHOICE initiative, DCP2, 2004 Copenhagen Consensus, and in literature found through PubMed and Internet searches between June-October 2006, and bibliographies from other published papers are reviewed. Search terms included ‘cost-effectiveness thresholds’, ‘ceiling ratio’, ‘lambda’ and ‘cost-effectiveness’, ‘value of a statistical life’ ‘valuation of life’ and other search terms. Examples are given of λ applications in practice and advantages and disadvantages of each method for defining λ are outlined, followed by a discussion of methodological and policy implications and priorities for further research. Except for where indicated, values are reported as 2008 US$.
Approaches Used to Define λ
The definition of λ is simply the marginal cost or benefit to society of saving a healthy year of life. The value of λ can be defined normatively, or according to a predefined budget. A simplified framework has been used to illustrate prioritization decisions through these two converse approaches.[49] These approaches rely on ‘league tables’, which order all interventions under consideration according to their ICERs (tables I and II).[51-53] The budget may be defined first and then distributed across programmes with increasing (less cost-effective) values until funds are exhausted. In this case, λ is revealed as the cost-effectiveness of the last intervention approved. Alternatively, λ may be based on a normative value, with all interventions meeting or falling below this level being accepted. In this scenario, budgetary requirements are revealed from the collective cost of the approved interventions at the scale at which they are applied. Graphically, the relationship between λ and available budget can be represented on the cost-effectiveness plane, also showing the effects of budget increases on λ and interventions accepted.[55] Two main classes of normative definitions for λ are reviewed in this article. The human capital approach values life according to what a person contributes to society, often measured in terms of per capita GNI. Preference-elicitation approaches reveal valuations according to actual or hypothetical choices people make in relation to increased risks of death.
Table I.
| Disease group and intervention | Cost per person ($US) |
Cost per year of life saved ($US) |
|---|---|---|
| Treat pneumonia in children | 3 | 4 |
| Rehydration for mild diarrhoea in children | 4 | 9 |
| Treat pneumonia, malaria and diarrhoea in children |
5 | 10 |
| AIDS education via media | 0.01 | 15 |
| Short-course treatment for TB at health centre | 77 | 15 |
| Treat malaria in children | 4 | 17 |
| Caesarean section for obstructed delivery | 55 | 23 |
| Vaccinate children | 22 | 32 |
| Treat severe pneumonia in children | 89 | 40 |
| Surgery for appendicitis | 86 | 46 |
| Treat severe malnutrition in children | 91 | 54 |
| Distribute impregnated bed nets | 4 | 55 |
| Short-course treatment for TB at hospital | 299 | 55 |
| Distribute/promote condoms among bar ladies |
55 | 61 |
| Treat complicated measles | 52 | 61 |
| Deworming and vitamin A/iodine supplements |
3 | 86 |
| Treat rheumatic fever | 41 | 88 |
| Treat sexually transmitted diseases | 15 | 93 |
| Treat severe diarrhoea in children | 58 | 95 |
| Surgery for hernia | 68 | 95 |
| Anti-tobacco legislation and warnings | 0.01 | 98 |
| Legislation/fines regarding seat belts for injury prevention |
0.01 | 102 |
| Treat severe malaria in children | 58 | 111 |
| Screen blood for transfusion | 29 | 137 |
| Educate mothers on childhood pneumonia | 0.26 | 138 |
| Integrated family planning, prenatal and delivery |
42 | 139 |
| Provide prenatal and delivery care at hospital | 35 | 162 |
| Provide prenatal and delivery care at health centre |
32 | 170 |
| Treat pneumonia in adults | 4 | 171 |
| Treat severe pneumonia in adults | 83 | 272 |
| Distribute condoms among general public | 17 | 294 |
| Aspirin for pre-existing heart disease | 23 | 329 |
| Treat severe injury | 298 | 355 |
| Outreach family planning services | 97 | 362 |
| Treat stroke or heart attack | 201 | 366 |
| Construct pit latrines and provide safe water | 35 | 439 |
| Monitor growth, counsel mother on nutrition and pneumonia |
22 | 767 |
| Treat mild malnutrition in children | 20 | 996 |
| Treat AIDS | 182 | 1680 |
| Treat hypertension | 84 | 2916 |
Jha et al.[50] used cost-effectiveness estimates from the 1993 Disease Control Priorities project combined with expert opinion to construct this league table of interventions applicable to Guinea. This league table is particularly useful at the national level because it provides an estimate of cost per capita, which can help planners allocate the available budget across programmes, thus revealing a cost-effectiveness threshold.
Figures have been inflated from their published values to $US, year 2008 values.
TB = tuberculosis.
Table II.
Regional league table for sub-Saharan Africaa,b,c(reproduced from Laxminarayan et al.[54] with permission)
| Intervention | Cost | Cost-effectiveness estimate ($US) | |
|---|---|---|---|
|
| |||
| Low | High | ||
| Childhood immunization | Low | 1.10 | 5.52 |
| Penalties and speed bumps to prevent traffic accidents |
Low | 2.21 | 13.24 |
| Malaria prevention | Low | 2.21 | 26.48 |
| Surgical services and emergency care | Low | 7.72 | 237.26 |
| Childhood illness interventions | Low | 9.93 | 240.57 |
| Cardiovascular disease management | Low | 9.93 | 301.26 |
| HIV/AIDS prevention and diagnosis | Low | 6.62 | 416.03 |
| Maternal and neonatal care interventions | Low | 90.49 | 451.34 |
| Diarrhoeal diseases: ORT and rotavirus immunization |
High | 551.76 | 1829.65 |
| HIV/AIDS treatment | High | 742.67 | 1648.67 |
| Traffic accidents: breath tests and seatbelts | High | 1073.73 | 2368.17 |
| High blood pressure and cholesterol treatment | High | 2118.77 | Not assessed |
| Lifestyle diseases: legislation to improve diet | High | 1948.83 | 2599.91 |
| Stroke management and prevention | High | 1416.93 | 3244.37 |
| Tuberculosis treatment | High | 4556.46 | 6076.01 |
| Cardiovascular disease prevention and management |
High | 699.64 | 29588.83 |
Shading added by authors.
Costs inflated to $US, year 2008 values according to US inflation rates.
The second edition of the Disease Control Priorities project updated and improved the cost-effectiveness estimates of the 1993 volume, and were summarized by Laxminarayan et al.[54] Interventions were clustered according to disease area, and classified as low or high cost. Low and high estimates of cost-effectiveness should not be interpreted as confidence intervals but best estimates of individual interventions. Estimates listed above the grey shaded area are cost-effective according to the criterion of $US208 per disability-adjusted life-year averted, those shaded grey are cost-effective according to twice gross national income, and those underneath are not cost-effective.
ORT = oral rehydration therapy.
League Table Approach – $US150 per Disability-Adjusted Life-Year (DALY)
The $US150 per DALY estimate derives from work by the World Bank[17] in 1993 to recommend a minimum care package (MCP) of services that should be provided by LMICs, and this threshold was reiterated in 1996 in an effort to define research priorities.[56] These committees specified $US150 per DALY as ‘attractive’ cost-effectiveness and $US25 per DALY as ‘highly attractive’ cost-effectiveness for low-income countries, with $US500 and $US100 per DALY, respectively, specified for middle-income countries. In these prioritization processes, λ was established based on prior assumptions about budgetary resources and other criteria.[57] Countries were advised to tailor these global recommendations to their own budgetary constraints, epidemiological profile, demographic profile, existing health infrastructure and other health system considerations.
However, $US150 per DALY has limitations in its usefulness in economic evaluation. While evaluations included in the league table were methodologically comparable in health outcome measures and discount rate, comparators were not applicable to all contexts.[16] The interventions considered did not represent a complete list of interventions available,[51] and countries would have needed to either conduct additional evaluations or restrict their scope to those with comparable methodology.[53] The cost-effectiveness of interventions can vary when implemented at different scales,[58] and other contextual factors affect cost-effectiveness in different settings.[59] In addition, choosing the most cost-effective interventions according to a specific budget does not always maximize utility, since interventions do not have perfect divisibility.[58,60]
The main functional drawback to applying $US150 per DALY is that, despite being the lowest explicitly defined value for λ in the literature, resulting recommendations were still difficult for some LMIC health sectors to afford. For example, Uganda's attempt to implement the MCP was made with a budget of $US9.00 per person – much lower than the required $US31.49. As a result, Uganda was forced to prioritize within the MCP,[61] which led to some decisions being made on an ad hoc basis, reflecting professional opinions, political expediency or public hysteria rather than considered evidence. Without systematic tools, these types of factors may have disproportionate impact on decisions, and the status quo is often preserved.[62]
Twice Per Capita Gross National Income Approach
In accordance with the converse method for establishing λ, a classic paper argues for a normative threshold. In this paper, Garber and Phelps[63] derive twice per capita GNI for λ, using a standard von Neumann-Morgenstern utility framework to model returns to investment in the health sector relative to those in other sectors. We argue that by defining a person's life according to the monetary value they produce or receive for their contribution to society, a human capital approach is implied.
Besides the theoretical foundation of twice per capita GNI, a positive economic argument exists for using a human capital approach – it is consistent with accepted practice for economic evaluation in several high-income countries. The $US50 000 per QALY (year 1982 values) threshold commonly used in the US is similar to GNI ($US46 040);[64-66] if $US50 000 is inflated to year 2008 values, it becomes roughly twice per capita GNI ($US101 295 per QALY). Likewise, if the range of values proposed in Canada ($Can20 000–100 000; year 1990 values) is inflated to $US, year 2008 values, they become $US23 476–117 378,[67] with two times GNI falling within that range ($US79 300).[64] In the UK, £30 000 per QALY is commonly used in economic evaluation as the ceiling ratio, which can be inflated from its 2002 values to $US52 718,[27] and statistical evaluation has shown it to be even higher in practice.[68] Two times UK GNI is comparable to this valuation ($US81 320).[64] In addition, the Institute for Medical Technology Assessment in the Netherlands has announced a threshold that is 2.8 times national GNI.[69]
Defining λ according to economic activity of individuals is gaining recognition in economic evaluations of LMIC healthcare. The Commission for Macroeconomics and Health applied per capita income[44] and the WHO-CHOICE initiative applied GDP[18] as their thresholds for ‘very cost-effective’, and three times this level for ‘cost-effective’. A regional breakdown of GDP values used by WHO-CHOICE is given in table III. A human capital approach was also applied in the communicable disease analysis of the 2004 Copenhagen Consensus (GNI),[70] and the priority-setting initiative recently undertaken by the Mexican health system (GDP).[71]
Table III.
| WHO region | Threshold value ($I)b | |
|---|---|---|
| GDP per capitac | 3 × GDP per capitac | |
| AFRO D | 1695 | 5086 |
| AFRO E | 2154 | 6461 |
| AMRO A | 39950 | 119849 |
| AMRO B | 9790 | 29371 |
| AMRO D | 4608 | 13823 |
| EMRO B | 10208 | 30624 |
| EMRO D | 2769 | 8306 |
| EURO A | 30439 | 91318 |
| EURO B | 7945 | 23836 |
| EURO C | 9972 | 29915 |
| SEARO B | 4959 | 14876 |
| SEARO D | 1990 | 5971 |
| WPRO A | 30708 | 92123 |
| WPRO B | 6948 | 20845 |
The WHO Choosing Interventions that are Cost-Effective (WHO-CHOICE) initiative has generated a league table of over 700 interventions relevant to low- and middle-income countries.[18] The thresholds used are based on the normative recommendations of the Commission on Macroeconomics and Health (CMH).[44] Note that while traditional league tables seek to inform decisions concerning additional investment, the WHO-CHOICE also considers the cost-effectiveness of all interventions, existing and proposed, relative to the null comparator – the natural history of disease.
Figures are presented in terms of International dollars ($I), which have the value of $US1 spent in the US; year 2005 values.
<GDP per capita is considered very cost-effective; 1–3 × GDP per capita is considered cost-effective; >3 × GDP per capita is considered not cost-effective.
AFRO = African region; AMRO = Americas region; EMRO = Eastern Mediterranean region; EURO = European region; SEARO = South-East Asia region; WPRO = Western Pacific region.
Drawbacks to using multiples of per capita GNI include equity, affordability and neglect of the multidimensional nature of welfare. In terms of equity, using an estimate based on GNI values life differently in real economic terms across countries with different economic environments, and using a state-dependent ceiling ratio may reinforce wide global inequities in health and wealth. Between the world's richest countries and poorest countries, GNI in terms of International dollars ($I; i.e. adjusted for purchasing power parity [PPP]) differs by two orders of magnitude.[64] The per capita GNI in high-income Organisation for Economic Cooperation and Development (OECD) countries in terms of current $US is $US39 158 (×2 = $US78 316). The per capita GNI for low-income countries is $US574 (×2 = $US1148). Furthermore, exceptional circumstances such as war, natural disaster and other negative economic shocks lower average wages selectively, causing further international inequities between affected areas and the rest of the world.
In terms of affordability, using per capita GNI may lead to total budgetary costs that are currently not sustainable, far exceeding the documented affordability problems with the much lower figure of $US150 per DALY discussed in section 1.1.[61] Predicating decisions on normative arguments for λ instead of budgets can lead to high potential expenditure, and health sector budgets in LMICs are already severely constrained. Two interventions may have similar cost-effectiveness, but one may apply to a much larger population than another (e.g. insecticide-treated bed nets for malaria compared with intermittent presumptive treatment of pregnant women),[35] leading to much higher budgetary requirements. More effective but expensive interventions may also be recommended to replace affordable inferior goods,[55] which may limit the number of people to whom services can be provided.
However, investment in the health of LMIC populations is reaching levels unprecedented in global history,[44,72] and with some of this investment subsidizing patient costs, affordability concerns for both providers and patients can be relaxed to some degree. In addition, projections of funding from private sources may be considered alongside government budgets when considering the affordability of interventions, as many developing country health systems accept out-of-pocket payments for additional services (private out-of-pocket expenditures are 25% of total health expenditures in Africa and 65% in Southeast Asia).[73] Funds from donor organizations may also be accounted for where they are channeled through the public health system. Bobadilla and Saxenian[74] reported that countries considered in the design of the 1993 MCP were spending $US9.00 per capita in public funds on healthcare (year 2008 values); however, $US31.49 per person was being spent when private sources were taken into account.
As a final critique of the GNI approach, valuing health according to income ignores the other dimensions of life that can be argued to have utility. Addison[75] makes this case, stating that the human capital approach is not valid as it ‘puts a value on livelihood rather than life’. In other words, it suggests indifference between a life-saving intervention, and one that increases an individual's projected discounted productivity by a percentage that offsets the intervention cost.[76] While the argument exists that the human capital approach reflects the value that an individual contributes to society, Behrman et al.[77] argue that it does not remove consumption (what the individual takes from society) from the equation. With consumption netted out, the lives of many individuals would have no value if the balance between their production and consumption is equal.[78] Also, average GNI is not a measure of the marginal impact of losing 1 year of life, which may be very low in populations with high unemployment and underemployment.
Preference-Elicitation Approach
“To value life as the individual herself would value it” was proposed by Nancy Stokey[79] of the 2004 Copenhagen Consensus expert panel to guide normative discussions about the value of λ. This criterion links λ to its root in individual preferences, maintaining consistency with utility theory and welfare economics.[80] Eliciting preferences can take two perspectives – WTP for incremental improvements in health,[81-85] or the amount of money people are WTA as compensation to agree to take life-threatening risks.[86,87] Methodological approaches for preference elicitation can evaluate real-world decisions (revealed preference) or hypothetical scenarios (stated preference), focus on valuation of healthy life-years or medical interventions, and can sample from patients or policy makers. WTA estimates are higher than those taken from a WTP perspective; people require more compensation for a loss than the amount they would pay for an equivalent gain.[88,89] This implies that λ should be different for investing in new services and disinvesting from existing ones, and evidence from the UK indicates that this is true in practice.[68]
The WTA approach has been found empirically to produce estimates for λ that are much higher than those discussed to this point, and is the approach used to value health gains through the ‘full income’ measure reviewed by Jamison.[90] Addison[75] argues that individuals in high-income countries value their lives at roughly five times GNI. Viscusi and Aldy[87] reviewed more than 60 studies from ten countries, which revealed that individuals' willingness to risk death in exchange for higher salaries was 100–200 times annual GDP.[87] Based on this evidence, Evans[91] calculated that λ would be 1.4–2.8 times GDP with a 70-year life span, or 3.4–6.9 times GDP if this life span is discounted by 3%. Hirth et al.[66] standardized results from 42 published articles and revealed λ estimates of 3–20 times GNI of high-income countries for individuals in North America and Western Europe.
The WTP approach often uses hypothetical testing methods such as contingent valuation,[92] or structured bidding methods.[93] As an example of the latter, a study measuring WTP for neurosurgery in the US derived estimates of $US14 356–36 918 per QALY,[82] lower than the average GNI of $US46 040, or the commonly cited figure of $US101 295 (inflated from $US50 000).[67] To our knowledge, this approach has not been used to derive estimates for λ in LMICs. As an example of what would be possible: in the Central African Republic (CAR), the median WTP for malaria treatment determined by contingent valuation was $US10.37.[81] With a probability of death between 0.1% and 0.75%, and a discounted life expectancy of 24.83–27.47 years,[31] the value of λ can be calculated to be $US0.26–2.14. Similar calculations can be conducted for other interventions with appropriate data, such as estimates for WTP for a malaria vaccine in Ethiopia.[94]
Dolan et al. (2008)[95] identified four factors that theoretically should be relevant influences on values derived through preference elicitation, including baseline and background risk, wealth, age and latency of the risk. Except for latency, they found that valuations were insensitive to all of these factors. They also identified four influences that should be theoretically irrelevant, including differences between WTA and WTP, size of change in risk, type of death, and irrelevant methodological cues; and found that valuations were sensitive to all of them. Their review provides thorough discussion of all of these factors; we discuss two that are particularly relevant to resource-poor settings: ability to pay and psychological factors.
To some extent, less wealthy individuals are less willing and able to afford health services, and several studies exist to support this.[83-85,94,96-99] However, other evidence suggests that poverty has less of an impact on WTP for health interventions than might be expected, especially for characteristics of high-quality care that people view as essential.[100,101] Extensive evidence demonstrates that people will pay catastrophic amounts for the healthcare of loved ones,[102] and a family may be willing to pay more than their annual income if they anticipate future income or are willing to liquidate resources.[85] Dolan et al.[95] conclude that, while WTP for health increases with wealth, it does not do so proportionally.
Psychological factors that affect decision-making processes have been identified. The formation of preferences is complex, being adaptable over time and in environments with different levels of uncertainty.[103] In addition, psychological research indicates that individuals' valuations of health states are affected substantially by their emotional state,[104] and health valuations are positively correlated with the quality of current health.[105] Conversely, having a family member previously affected may motivate coping mechanisms and lead to a lower WTP.[85,106] It is less clear if health education has an impact on WTP,[84,85] and social, cultural and financing factors that influence decisions between biomedical and traditional medicine may also have an influence.[107] From a policy-maker's perspective, bias in WTP is likely to be upwards in decisions about whether to fund an intervention, and downwards if deciding how much to charge.[108] Attention should be paid to ensuring that preference-elicitation estimates are derived from the context in which prioritization decisions will be made (e.g. regional, national or sub-national).
Ethical Criteria
It is important to consider the ethical criteria that inevitably underlie prioritization decisions. Examples of these criteria include equity in health status, equity of access, differential provision according to need, ‘rule of rescue’, prioritization according to importance to society, equity in opportunity for health and health maximization.[109-112] λ thresholds as they are currently defined may imply that health status should be maximized across individuals; however, evidence exists that people do not hold this objective for healthcare expenditures. Several studies have found that people are willing to accept a lower overall societal standard of health in order to make health states across individuals more equal,[113-115] and efforts have been made to quantify this trade-off.[116-118]
The trade-off between equity and efficiency in public decision making has theoretical foundations in welfare economics,[110,116,119] and clear examples show this conflict in terms of both horizontal and vertical equity.[21] However, it is recognized that many of the most cost-effective interventions available benefit the poor, since they die younger, have the most potential for health improvement and are disproportionately affected by infectious diseases with inexpensive cures.[21] A main message from the 2006 DCP2 is that massive gains in equity can be obtained in international health even without explicitly adding equity considerations to cost-effectiveness estimates.[19]
Methodological and Policy Implications
With unprecedented levels of interest, research and investment in LMIC health, considered examination is warranted of the methods used to value health improvement, and the issues surrounding them. By making these practices explicit, scrutiny by decision makers and the international community becomes possible, and the selection process for λ becomes less arbitrary. A standard cross-country threshold of $US150 per DALY was recommended in the past, largely due to budgetary concerns, and may be used to make results comparable to already published CEAs. More recently, multiples of national GNI and GDP have been applied, possibly to accommodate recent increases in public health budgets and more expensive but highly valued therapies such as antiretroviral treatment for AIDS. However, this method was strongly criticized by some in the 2004 Copenhagen Consensus, with the two health-related papers using different approaches,[70,77] while Nancy Stokey[79] advocated preference elicitation. Only a few disease-specific WTP studies exist; evidence suggests that estimates vary widely according to methodology,[66] and more research is needed to define protocols for aggregating results.[120]
Each approach to defining λ has its strengths and weaknesses. However, we would argue that, for given programmes and national governments, it is most appropriate to reveal values for λ by prioritizing within a league table according to context-specific budget, making trade-offs between other decision-making factors within that constraint. Emphasizing budget would reduce the likelihood of inefficiencies such as those described in Uganda due to recommendations exceeding available resources, the need for a second round of prioritization, and the potential for unplanned and unfavorable distributions of health services.[61] While the problems faced in Uganda may not be intrinsic or inevitable, maintaining recommendations within national budgetary limits would create conditions for political promises to be kept, and maintain focus on sound delivery of interventions with the best cost-effectiveness.
When using CEA to determine regional or international priorities upstream in the process, we would argue that more influence from normative criteria is appropriate, and that equity should be explicitly considered in the distribution of budgets. While budget constraints maintain relevance at this level,[121] and larger numbers of programmes and interventions are considered, international bodies may have more influence on how budgets are defined,[122] and can make efforts to approve intervention mixes that are consistent with normative ideals. For decision-making bodies allocating resources across different countries, results should be presented in terms of $I to address variations in PPP.[77,123]
The league tables shown in tables I and II serve as simplified examples of how λ can be conceptualized. Table I is specific to Guinea, and could be used to prioritize interventions according to a specified budget, cost per person, and coverage levels, thus revealing the λ threshold.[50] Table II is an example of how prioritization can be conducted at the regional level, using a threshold that can subsequently be used to define budget allocations. Evidence for sub-Saharan Africa is taken from the recent DCP2, and interventions are clustered according to the health area and overall programme costs.[54] If these estimates are compared with the $US150 per DALY threshold ($US208 in 2008 values), interventions deemed cost-effective are childhood immunization, traffic penalties and speed bumps, and malaria prevention, as well as many from the other low-cost intervention clusters. If the threshold is moved to twice GNI in sub-Saharan Africa ($US1902),[64] all low-cost interventions and some from three high-cost clusters qualify according to cost-effectiveness. It is important to note that the cost-effectiveness of some estimates for HIV/AIDS treatment differs from evidence generated earlier this decade when the cost of antiretroviral therapy was higher than it is today.[124]
Importantly, cost-effectiveness should be considered alongside other decision-making factors such as the intervention being a public good, externalities, catastrophic costs, preferential benefit to the poor, vertical and horizontal equity and potential to save lives.[21] Burden of disease and the size of programmes will have important implications for the budget. Patient demand will have strong influence on whether projected health gains are realized. How this evidence is presented to decision makers should be tailored to the political environment, as prioritization is necessarily a long, complex process involving many people with different preferences, both for outcome and process. One option is to accompany cost-effectiveness evidence with qualitative information for decision makers to consider according to their own mechanisms. Mathematically, a multi-criteria league table approach has been applied in hypothetical studies in Ghana and Nepal,[125,126] which estimates the probability that interventions are approved through a regression framework.[127] For determining the scale at which different interventions should be implemented, several mathematical modeling approaches are available to facilitate calculations.[58]
Notably, the evidence from Nepal suggested that cost-effectiveness was not the primary factor for policy approval,[126] which is consistent with the real-world policy decision to implement universal coverage of antiretroviral therapy in Thailand.[128] Other research, from Tanzania, suggests that evidence does affect the way health planners rank alternative interventions, with cost-effectiveness being their dominant consideration in a hypothetical exercise.[129] Indeed, the true impact of CEA may be to increase investment in the target health system,[130] or the number of interventions approved. Research is underway to improve the use of evidence in priority setting in LMICs through considering contextual factors.[131]
Several alternative approaches to defining λ are not explored in this paper. Behrman et al.[77] advocated comparing the value of postponing mortality through one intervention to the resource cost of the most effective alternative means of postponing mortality. Birch and Gafni[58] advocated investment in a new programme only if its health gains exceeded those from ones that they could replace at equal or lower cost. Another alternative is to base λ on the value of tax revenues lost through avoidable mortality.[123] Questions left by these approaches include how to guide decisions for allocating new resources, and how to consider normative perspectives that are inevitably relevant. As a solution to the problems of assessing preferences associated with current approaches, Dolan et al.[95] advocated deriving λ values thorough the ratio of coefficients for household income and health state in estimating subjective well-being (SWB) through a regression framework.
The empirical research behind the SWB approach suggests that it may not be desirable for public bodies to have a uniform value for λ across people, populations or health states.[95] Indeed, the health economics community focused on LMICs recognizes differential valuation of life by including the option to use age weighting in DALY calculations.[132] In addition to adjustments to DALY calculations, λ thresholds might be conceptualized as a distribution, which accounts in its variance for the influence of factors beyond cost-effectiveness in previous decisions. Deriving λ values thorough the SWB framework for different global areas, as outlined by Dolan et al.,[95] should be a priority area for research. Valuing life before birth is a burgeoning area of study, which will be of relevance to economic evaluations of maternal and neonatal health interventions.[133,134]
Despite their limitations and methodological weaknesses, cost-effectiveness thresholds will remain important criteria for health sector prioritization decisions in LMICs. However, as budgets, contexts, normative arguments, equity criteria and relevant interventions change, values for λ should incrementally evolve. Analysts should accommodate these changes through time by accompanying reference case results with acceptability curves. Health and life spans have improved substantially in much of the world in the last century,[90] and evidence indicates that improvements in health make substantial contributions to increases in GNI.[135,136] This finding suggests that values for λ defined by the human capital approach can be expected to increase with economic growth. In addition, the infusion of new investment in LMIC health implies increases in values for λ revealed through budget allocations. Finally, as people enjoy better standards of living, they will be better able to ‘manage to desire’ improvements in health,[137] and values elicited according to WTP/WTA may be expected to increase.
Conclusions
Approaches to defining λ in economic evaluation of interventions relevant to LMICs have evolved from ad hoc comparisons to $US150 per DALY to valuations based on GNI or GDP. Preference elicitation methods are also available, and each method has advantages and disadvantages. Being explicit about λ promotes consistency in decision making, encourages informed debate about health state valuations, and enhances the potential to perform more advanced applications of decision science. Consistency with previous studies, empirical validity, the objectives of decision making bodies, and the need to accommodate evolving preferences should all be considered when choosing a ceiling ratio. Key areas for further research include the estimation of subjective well-being, discussing differential valuations of life for different groups, and discussion of which vaulation approach is most appropriate in different settings.
Acknowledgements
No specific sources of funding were used to assist in the preparation of this review. Samuel Shillcutt is supported by the WHO Child Health Epidemiology Reference Group (CHERG), Damian Walker is supported by the UK Department for International Development (DFID)-funded Future Health Systems Consortium, and Catherine Goodman is a member of the KEMRI/Wellcome Trust Research Programme, which is supported by a grant from the Wellcome Trust (#077092). The authors have no conflicts of interest that are directly relevant to the content of this review.
References
- 1.Warner KE, Hutton RC. Cost-benefit and cost-effectiveness analysis in health care: growth and composition of the literature. Med Care. 1980;18(11):1069–84. doi: 10.1097/00005650-198011000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Elixhauser A, Luce BR, Taylor WR, et al. Health care CBA/CEA: an update on the growth and composition of the literature. Med Care. 1993;31(Suppl. 7):JS1–11. doi: 10.1097/00005650-199307001-00001. JS8-149. [DOI] [PubMed] [Google Scholar]
- 3.Elixhauser A, Halpern M, Schmier J, et al. Health care CBA and CEA from 1991 to 1996: an updated bibliography. Med Care. 1998;36(Suppl. 5):MS1–9. doi: 10.1097/00005650-199805001-00001. MS18-147. [DOI] [PubMed] [Google Scholar]
- 4.Walker D, Fox-Rushby JA. Economic evaluation of communicable disease interventions in developing countries: a critical review of the published literature. Health Econ. 2000;9(8):681–98. doi: 10.1002/1099-1050(200012)9:8<681::aid-hec545>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 5.Adam T, Lim SS, Mehta S, et al. Cost effectiveness analysis of strategies for maternal and neonatal health in developing countries. BMJ. 2005;331(7525) doi: 10.1136/bmj.331.7525.1107. doi:10.1136/bmj.331.7525.1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mulligan JA, Walker D, Fox-Rushby JA. Economic evaluations of non-communicable disease interventions in developing countries: a critical review of the evidence base. BMC Cost-Effectiveness Resource Allocation. 2006;4(7) doi: 10.1186/1478-7547-4-7. doi:10.1186/1478-7547-4-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baltussen R, Floyd K, Dye C. Cost effectiveness analysis of strategies for tuberculosis control in developing countries. BMJ. 2005;331(7529) doi: 10.1136/bmj.38645.660093.68. doi:10.1136/bmj.38645.660093.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chisholm D. Cost-effectiveness of first-line antiepileptic drug treatments in the developing world: a population-level analysis. Epilepsia. 2005;46(5):751–9. doi: 10.1111/j.1528-1167.2005.52704.x. [DOI] [PubMed] [Google Scholar]
- 9.Chisholm D, Rehm J, Van Ommeren M, et al. Reducing the global burden of hazardous alcohol use: a comparative cost-effectiveness analysis. J Stud Alcohol. 2004;65(6):782–94. doi: 10.15288/jsa.2004.65.782. [DOI] [PubMed] [Google Scholar]
- 10.Chisholm D. Choosing cost-effective interventions in psychiatry: results from the CHOICE programme of the World Health Organization. World Psychiatry. 2005;4(1):37–44. [PMC free article] [PubMed] [Google Scholar]
- 11.Chisholm D, van Ommeren M, Ayuso-Mateos JL, et al. Cost-effectiveness of clinical interventions for reducing the global burden of bipolar disorder. Br J Psychiatry. 2005;187(6):559–67. doi: 10.1192/bjp.187.6.559. [DOI] [PubMed] [Google Scholar]
- 12.Tan-Torres Edejer T, Baltussen R, Adam T, et al. WHO guide to cost-effectiveness analysis. World Health Organization; Geneva: 2003. [Google Scholar]
- 13.Hogan DR, Baltussen R, Hayashi C, et al. Cost effectiveness analysis of strategies to combat HIV/AIDS in developing countries. BMJ. 2005;331(7530):1431–7. doi: 10.1136/bmj.38643.368692.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morel CM, Lauer JA, Evans DB. Cost effectiveness analysis of strategies to combat malaria in developing countries [published erratum appears in BMJ 2006; 332 (7534): 151 and BMJ 2006; 333 (7558): 86] BMJ. 2005;331(7528) doi: 10.1136/bmj.38639.702384.AE. doi:10.1136/bmj.38639.702384.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shibuya K, Ciecierski C, Guindon E, et al. WHO Framework Convention on Tobacco Control: development of an evidence based global public health treaty. BMJ. 2003;327(7407):154–7. doi: 10.1136/bmj.327.7407.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jamison DT, Mosley WH, Measham AR, et al. Disease control priorities in developing countries. Oxford University Press; Oxford: 1993. [Google Scholar]
- 17.World Bank . World development report. World Bank; Washington, DC: 1993. [Google Scholar]
- 18.WHO-CHOICE. Choosing interventions that are cost-effective [online] Available from URL: http://www.who.int/choice/en [Accessed 2006 Jun 30]
- 19.Jamison D, Breman J, Measham A, et al. Disease control priorities in developing countries. 2nd ed. The World Bank and Oxford University Press; Washington, DC: 2006. [PubMed] [Google Scholar]
- 20.Lomborg B. Copenhagen Consensus [online] Available from URL: http://www.copenhagenconsensus.com/Default.aspx?ID=788 [Accessed 2009 Jan 13]
- 21.Musgrove P. Public spending on health care: how are different criteria related? Health Policy. 1999;47:207–23. doi: 10.1016/s0168-8510(99)00024-x. [DOI] [PubMed] [Google Scholar]
- 22.Musgrove P. A critical review of ‘a critical review’: the methodology of the 1993 World Development Report, ‘Investing in Health’. Health Policy Plan. 2000;15(1):110–5. doi: 10.1093/heapol/15.1.110. [DOI] [PubMed] [Google Scholar]
- 23.Musgrove P, Fox-Rushby J. Cost-effectiveness analysis. In: Jamison D, Breman J, Measham A, et al., editors. Disease control priorities in developing countries. 2nd ed. The World Bank and Oxford University Press; Washington, DC: 2006. [Google Scholar]
- 24.Briggs AH. Handling uncertainty in economic evaluation and presenting the results. In: Drummond MF, McGuire A, editors. Economic evaluation in health care: merging theory with practice. Oxford University Press; Oxford: 2001. pp. 172–214. [Google Scholar]
- 25.Fenwick E, O'Brien BJ, Briggs A. Cost-effectiveness acceptability curves: facts, fallacies and frequently asked questions. Health Econ. 2004;13(5):405–15. doi: 10.1002/hec.903. [DOI] [PubMed] [Google Scholar]
- 26.Coast J. Who wants to know if their care is rationed? Views of citizens and service informants. Health Expect. 2001;4:243–52. doi: 10.1046/j.1369-6513.2001.00147.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Towse A, Pritchard C, Devlin N. Cost-effectiveness thresholds. Office of Health Economics; London: 2002. [Google Scholar]
- 28.Lomborg B. Global crises, global solutions. Cambridge University Press; Cambridge: 2004. [Google Scholar]
- 29.Claxton K, Posnett J. An economic approach to clinical trial design and research priority-setting. Health Econ. 1996;5(6):513–24. doi: 10.1002/(SICI)1099-1050(199611)5:6<513::AID-HEC237>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 30.Fenwick E, Claxton K, Sculpher MJ, et al. Improving the efficiency and relevance of health technology assessment: the role of iterative decision analytic modelling. University of York; York: 2000. [Google Scholar]
- 31.Shillcutt S, Morel C, Goodman C, et al. Cost-effectiveness of malaria diagnostic methods in sub-Saharan Africa in an era of combination therapy. Bull WHO. 2008;86(2):101–10. doi: 10.2471/BLT.07.042259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tyagi V, Singh SK, Sawhney A, et al. Using gross national product to calculate acceptable immunisation costs: deploying cost-effectiveness calculations in reverse. Pharmacoeconomics. 2003;21(7):497–9. doi: 10.2165/00019053-200321070-00004. [DOI] [PubMed] [Google Scholar]
- 33.Summers LH. Investing in the people. Pak Dev Rev. 1992;31(4):367–406. [PubMed] [Google Scholar]
- 34.Coleman PG, Goodman CA, Mills A. Rebound mortality and the cost-effectiveness of malaria control: potential impact of increased mortality in late childhood following the introduction of insecticide treated nets. Trop Med Int Health. 1999;4(3):175–86. doi: 10.1046/j.1365-3156.1999.43382.x. [DOI] [PubMed] [Google Scholar]
- 35.Goodman CA, Coleman PG, Mills AJ. Cost-effectiveness of malaria control in sub-Saharan Africa. Lancet. 1999;354(9176):378–85. doi: 10.1016/s0140-6736(99)02141-8. [DOI] [PubMed] [Google Scholar]
- 36.Goodman CA, Coleman PG, Mills AJ. Changing the first line drug for malaria treatment: cost-effectiveness analysis with highly uncertain inter-temporal trade-offs. Health Econ. 2001;10(8):731–49. doi: 10.1002/hec.621. [DOI] [PubMed] [Google Scholar]
- 37.Budke CM, Jiamin QIU, Qian W, et al. Economic effects of echinococcosis in a disease-endemic region of the Tibetan Plateau. Am J Trop Med Hyg. 2005;73(1):2–10. [PubMed] [Google Scholar]
- 38.Caincross S, Valdmanis V. Water supply, sanitation, and hygiene promotion. In: Jamison DT, Breman JG, Measham AR, et al., editors. Disease control priorities in developing countries. Oxford University Press and the World Bank; New York: 2006. [Google Scholar]
- 39.Walker D, Rheingans R. Cost-effectiveness of rotavirus vaccines. Exp Rev Pharmacoeconomics Outcomes Res. 2005;5(5):593–601. doi: 10.1586/14737167.5.5.593. [DOI] [PubMed] [Google Scholar]
- 40.Von Schirnding Y, Bruce N, Smith K, et al. Addressing the impact of household energy and indoor air pollution on the health of the poor: implications for policy action and intervention measures [working paper 12] World Health Organization Commission for Macroeconomics and Health, Working Group 5; Geneva: 2001. [Google Scholar]
- 41.Varley RC, Tarvid J, Chao DN. A reassessment of the cost-effectiveness of water and sanitation interventions in programmes for controlling childhood diarrhoea. Bull WHO. 1998;76(6):617–31. [PMC free article] [PubMed] [Google Scholar]
- 42.Guyatt HL, Snow RW, Evans DB. Malaria epidemiology and economics: the effect of delayed immune acquisition on the cost-effectiveness of insecticide-treated bednets. Phil Trans Roy Soc B: Biol Sci. 1999;354(1384):827–35. doi: 10.1098/rstb.1999.0434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Listorti J, Doumani F. Energy and environmental health: a literature review and recommendations. World Bank; Washington, DC: 2001. [Google Scholar]
- 44.Sachs J. Macroeconomics and health: investing in health for economic development. World Health Organization; Geneva: 2001. [Google Scholar]
- 45.Jha P, Mills A. Improving health outcomes of the poor: the report of working group 5 of the Commission on Macroeconomics and Health. World Health Organization; Geneva: 2002. [Google Scholar]
- 46.Simon J, Gray A, Duley L, Magpie Trial Collaborative Group Cost-effectiveness of prophylactic magnesium sulphate for 9996 women with pre-eclampsia from 33 countries: economic evaluation of the Magpie trial. BJOG. 2006;11:144–51. doi: 10.1111/j.1471-0528.2005.00785.x. [DOI] [PubMed] [Google Scholar]
- 47.Aggarwal R, Ghoshal UC, Naik SR. Treatment of chronic hepatitis B with interferon-alpha: cost-effectiveness in developing countries. Natl Med J India. 2002;15(6):320–7. [PubMed] [Google Scholar]
- 48.Dye C, Floyd K. Tuberculosis. In: Jamison DT, Breman JG, Measham AR, et al., editors. Disease control priorities in developing countries. Oxford University Press and the World Bank; New York: 2006. [PubMed] [Google Scholar]
- 49.Briggs AH, Gray AM. Handling uncertainty when performing economic evaluation of healthcare interventions. Health Technol Assess. 1999;3(2):1–134. [PubMed] [Google Scholar]
- 50.Jha P, Bangoura O, Ranson K. The cost-effectiveness of forty health interventions in Guinea. Health Pol Plan. 1998;13(3):249–62. doi: 10.1093/heapol/13.3.249. [DOI] [PubMed] [Google Scholar]
- 51.Gerard K, Mooney G. QALY league tables: handle with care. Health Econ. 1993;2(1):59–64. doi: 10.1002/hec.4730020108. [DOI] [PubMed] [Google Scholar]
- 52.Birch S, Gafni A. Cost-effectiveness ratios: in a league of their own. Health Policy. 1994;28(2):133–41. doi: 10.1016/0168-8510(94)90031-0. [DOI] [PubMed] [Google Scholar]
- 53.Drummond M, Torrance G, Mason J. Cost-effectiveness league tables: more harm than good? Soc Sci Med. 1993;37(1):33–40. doi: 10.1016/0277-9536(93)90315-u. [DOI] [PubMed] [Google Scholar]
- 54.Laxminarayan R, Mills AJ, Breman JG, et al. Advancement of global health: key messages from the Disease Control Priorities Project. Lancet. 2006;367(9517):1193–208. doi: 10.1016/S0140-6736(06)68440-7. [DOI] [PubMed] [Google Scholar]
- 55.Sendi PP, Briggs AH. Affordability and cost-effectiveness: decision-making on the cost-effectiveness plane. Health Econ. 2001;10(7):675–80. doi: 10.1002/hec.639. [DOI] [PubMed] [Google Scholar]
- 56.WHO Investing in Health Research and Development . Report of the Ad Hoc committee on health research relating to future intervention options. World Health Organization; Geneva: 1996. [Google Scholar]
- 57.Bobadilla JL, Cowley P, Musgrove P, et al. Design, content, and financing of an essential national package of health services. World Bank; Washington, DC: 1995. [PMC free article] [PubMed] [Google Scholar]
- 58.Birch S, Gafni A. Information created to evade reality (ICER): things we should not look to for answers. Pharmacoeconomics. 2006;24(11):1121–31. doi: 10.2165/00019053-200624110-00008. [DOI] [PubMed] [Google Scholar]
- 59.Birch S, Gafni A. Economics and the evaluation of health care programmes: generalisability of methods and implications for generalisability of results. Health Policy. 2003;64:207–19. doi: 10.1016/s0168-8510(02)00182-3. [DOI] [PubMed] [Google Scholar]
- 60.Cohen JP. Cost-effectiveness and resource allocation. JAMA. 2006;295(23):2723. doi: 10.1001/jama.295.23.2723-a. [DOI] [PubMed] [Google Scholar]
- 61.Ssengooba F. Uganda's minimum package for health care: rationing within the minimum? Health Policy Development J. 2003;2(1) [Google Scholar]
- 62.Devlin N, Ashton T, Cumming J. Rationing health care: how should the HFA proceed? N Z Med J. 1999;112(1097):369–70. [PubMed] [Google Scholar]
- 63.Garber AM, Phelps CE. Economic foundations of cost-effectiveness analysis. J Health Econ. 1997;16(1):1–31. doi: 10.1016/s0167-6296(96)00506-1. [DOI] [PubMed] [Google Scholar]
- 64.World Bank World development indicators data query [online] Available from URL: http://ddp-ext.worldbank.org/ext/DDPQQ/member.do?method=getMembers&userid=1&queryId=135 [Accessed 2008 Mar 9]
- 65.Weinstein MC. From cost-effectiveness ratios to resource allocation: where to draw the line? In: Sloan FA, editor. Valuing health care: costs, benefits, and effectiveness of pharmaceuticals and other medical technologies. Cambridge University Press; New York: 1995. [Google Scholar]
- 66.Hirth RA, Chernew ME, Miller E, et al. Willingness to pay for a quality-adjusted life year: in search of a standard. Med Dec Making. 2000;20(3):332–42. doi: 10.1177/0272989X0002000310. [DOI] [PubMed] [Google Scholar]
- 67.Laupacis A, Feeny D, Detsky AS, et al. How attractive does a new technology have to be to warrant adoption and utilization? Tentative guidelines for using clinical and economic evaluations. Can Med Ass J. 1992;146(4):473–81. [PMC free article] [PubMed] [Google Scholar]
- 68.Devlin N, Parkin D. Does NICE have a cost-effectiveness threshold and what other factors influence its decisions? A binary choice analysis. Health Econ. 2004;13:437–52. doi: 10.1002/hec.864. [DOI] [PubMed] [Google Scholar]
- 69.IMTA . €80,000 per QALY is the limit. 1. Vol. 4. Institute of Medical Technology Assessment Newsletter; Netherlands: 2006. www.imta.nl/publications/imta_newsletter_4_1.pdf [Accessed 2006 Oct 30] [Google Scholar]
- 70.Mills AJ, Shillcutt SD. Communicable diseases. In: Lomborg B, editor. Global crises, global solutions. Cambridge University Press; Cambridge: 2004. pp. 62–111. [Google Scholar]
- 71.González-Pier E, Gutiérrez-Delgado C, Stevens G, et al. Health system reform in Mexico: priority setting for health interventions in Mexico's system of social protection in health. Lancet. 2006;368:1608–18. doi: 10.1016/S0140-6736(06)69567-6. [DOI] [PubMed] [Google Scholar]
- 72.Loomis C. Warren Buffett gives it away. Fortune. 2006;154(1):56–60. [PubMed] [Google Scholar]
- 73.WHO . National health accounts: country information. WHO [online]; Geneva: Available from URL: http://www.who.int/nha/country/en/ [Accessed 2009 Jan 20] [Google Scholar]
- 74.Bobadilla JL, Saxenian H. Designing an essential national health package. Finance Dev. 1993;30:10–3. [Google Scholar]
- 75.Addison T. Perspective paper 3.2. In: Lomborg B, editor. Global crises, global solutions. Cambridge University Press; Cambridge: 2004. pp. 165–74. [Google Scholar]
- 76.Appleton S. Perspective paper 7.2. In: Lomborg B, editor. Global crises, global solutions. Cambridge University Press; Cambridge: 2004. pp. 435–42. [Google Scholar]
- 77.Behrman JR, Alderman H, Hoddinott J. Malnutrition and hunger. In: Lomborg B, editor. Global crises, global solutions. Cambridge University Press; Cambridge: 2004. pp. 363–420. [Google Scholar]
- 78.Schelling TC. Expert panel ranking. In: Lomborg B, editor. Global crises, global solutions. Cambridge University Press; Cambridge: 2004. pp. 627–9. [Google Scholar]
- 79.Stokey N. Expert panel ranking. In: Lomborg B, editor. Global crises, global solutions. Cambridge University Press; Cambridge: 2004. pp. 639–44. [Google Scholar]
- 80.Johansson PO. An introduction to modern welfare economics. Cambridge University Press; Cambridge: 1991. [Google Scholar]
- 81.Weaver M, Ndamobissi R, Kornfield R, et al. Willingness to pay for child survival: results of a national survey in Central African Republic. Soc Sci Med. 1996;43(6):985–98. doi: 10.1016/0277-9536(96)00015-9. [DOI] [PubMed] [Google Scholar]
- 82.King JT, Jr, Tsevat J, Lave JR, et al. Willingness to pay for a quality-adjusted life year: implications for societal health care resource allocation. Med Dec Mak. 2005;25(6):605–6. doi: 10.1177/0272989X05282640. [DOI] [PubMed] [Google Scholar]
- 83.Cho-Min-Naing LS, Kamol-Ratanakul P, Saul AJ. Ex post and ex ante willingness to pay (WTP) for the ICT Malaria Pf/Pv test kit in Myanmar. Southeast Asian J Trop Med Public Health. 2000;31(1):104–11. [PubMed] [Google Scholar]
- 84.Dong H, Kouyate B, Cairns J, et al. Willingness-to-pay for community-based insurance in Burkina Faso. Health Econ. 2003;12:849–62. doi: 10.1002/hec.771. [DOI] [PubMed] [Google Scholar]
- 85.Rheingans RD, Haddix AC, Messonnier ML, et al. Willingness to pay for prevention and treatment of lymphatic filariasis in Leogane, Haiti. Filaria J. 2004;3(1) doi: 10.1186/1475-2883-3-2. doi: 10.1186/1475-2883-3-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Jones-Lee M. Safety and the saving of a life, the economics of safety and physical risk. In: Layard R, Glaister S, editors. Cost-benefit analysis. Cambridge University Press; Cambridge: 2006. pp. 290–318. [Google Scholar]
- 87.Viscusi WK, Aldy JE. The value of a statistical life: a critical review of market estimates throughout the world. J Risk Uncertain. 2003;27(1):5–76. [Google Scholar]
- 88.Guria J, Leung J, Jones-Lee M, et al. The willingness to accept value of statistical life relative to the willingness to pay value: evidence and policy implications. Environmental Res Econ. 2005;32(1):113–27. [Google Scholar]
- 89.Whynes DK, Sach TH. WTP and WTA: do people think differently? Soc Sci Med. 2007;65(5):946–57. doi: 10.1016/j.socscimed.2007.04.014. [DOI] [PubMed] [Google Scholar]
- 90.Jamison D. Investing in health. In: Jamison DT, Breman JG, Measham AR, et al., editors. Disease control priorities in developing countries. Oxford University Press and the World Bank; New York: 2006. [PubMed] [Google Scholar]
- 91.Evans DB. Perspective paper 2.1. In: Lomborg B, editor. Global crises, global solutions. Cambridge University Press; Cambridge: 2004. pp. 115–23. [Google Scholar]
- 92.Ryan M, Scott DA, Reeves C, et al. Eliciting public preferences for healthcare: a systematic review of techniques. Health Technol Assess. 2001;5(5):1–186. doi: 10.3310/hta5050. [DOI] [PubMed] [Google Scholar]
- 93.Onwujekwe O. Criterion and content validity of a novel structured haggling contingent valuation question format versus the bidding game and binary with follow-up format. Soc Sci Med. 2004;58(3):525–37. doi: 10.1016/s0277-9536(03)00214-4. [DOI] [PubMed] [Google Scholar]
- 94.Cropper ML, Lampietti JA, Haile M, et al. The value of preventing malaria in Tembien, Ethiopia [World Bank Policy Research working paper No 2273] World Bank; Washington, DC: 2001. [Google Scholar]
- 95.Dolan P, Metcalfe R, Munro V, et al. Valuing lives and life years: anomalies, implications, and an alternative. Health Econ Pol Law. 2008;3:277–300. doi: 10.1017/S1744133108004507. [DOI] [PubMed] [Google Scholar]
- 96.Whittington D, Matsui-Santana O, Freiberger JJ, et al. Private demand for a HIV/AIDS vaccine: evidence from Guadalajara, Mexico. Vaccine. 2002;20(19-20):2585–91. doi: 10.1016/s0264-410x(02)00152-4. [DOI] [PubMed] [Google Scholar]
- 97.Mathiyazhagan K. Willingness to pay for rural health insurance through community participation in India. Int J Health Plann Mgmt. 1998;13:47–67. doi: 10.1002/(SICI)1099-1751(199801/03)13:1<47::AID-HPM495>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- 98.Dong H, Kouyate B, Cairns J, et al. Inequality in willingness-to-pay for community-based health insurance. Health Policy. 2005;72(2):149–56. doi: 10.1016/j.healthpol.2004.02.014. [DOI] [PubMed] [Google Scholar]
- 99.Bonu S, Rani M, Bishai D. Using willingness to pay to investigate regressiveness of user fees in health facilities in Tanzania. Health Policy Plan. 2003;18(4):370–82. doi: 10.1093/heapol/czg045. [DOI] [PubMed] [Google Scholar]
- 100.Habbani K, Groot W, Jelovac I. Household health-seeking behaviour in Khartoum, Sudan: the willingness to pay for public health services if these services are of good quality. Health Policy. 2006;75(2):140–58. doi: 10.1016/j.healthpol.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 101.Mataria A, Giacaman R, Khatib R, et al. Impoverishment and patients' ‘willingness’ and ‘ability’ to pay for improving the quality of health care in Palestine: an assessment using the contingent valuation method. Health Policy. 2006;75(3):312–28. doi: 10.1016/j.healthpol.2005.03.014. [DOI] [PubMed] [Google Scholar]
- 102.Xu K, Evans DB, Kawabata K, et al. Household catastrophic health expenditure: a multicountry analysis. Lancet. 2003;362(9378):111–7. doi: 10.1016/S0140-6736(03)13861-5. [DOI] [PubMed] [Google Scholar]
- 103.Cookson R. QALYs and the capability approach. Health Econ. 2005;14(8):817–29. doi: 10.1002/hec.975. [DOI] [PubMed] [Google Scholar]
- 104.Loomes G. (How) can we value health, safety and the environment? J Econ Psychol. 2006;27(6):713–36. [Google Scholar]
- 105.King JT, Jr, Tsevat J, Roberts MS. Positive association between current health and health values for hypothetical disease states. Med Decision Making. 2004;24(4):367–78. doi: 10.1177/0272989X04267692. [DOI] [PubMed] [Google Scholar]
- 106.Sloan FA, Viscusi KW, Chesson HW, et al. Alternative approaches to valuing intangible health losses: the evidence for multiple sclerosis. J Health Econ. 1998;17(4):475–97. doi: 10.1016/s0167-6296(97)00025-8. [DOI] [PubMed] [Google Scholar]
- 107.Muela SH, Mushi AK, Ribera JM. The paradox of the cost and affordability of traditional and government health services in Tanzania. Health Policy Plan. 2000;15(3):296–302. doi: 10.1093/heapol/15.3.296. [DOI] [PubMed] [Google Scholar]
- 108.Smith RD. The reliability of willingness to pay for changes in health status. Appl Health Econ Health Policy. 2004;3(1):35–8. doi: 10.2165/00148365-200403010-00007. [DOI] [PubMed] [Google Scholar]
- 109.Huack K, Smith PC, Goddard M. The economics of priority setting for health care: a literature review. International Bank for Reconstruction and Development, World Bank; Washington, DC: 2003. [Google Scholar]
- 110.Sassi F, Archard L, Le Grand J. Equity and the economic evaluation of healthcare. Health Technol Assess. 2001;5(3):1–138. doi: 10.3310/hta5030. [DOI] [PubMed] [Google Scholar]
- 111.Ottersen T, Mbilinyi D, Maestad O, et al. Distribution matters: equity considerations among health planners in Tanzania. Health Policy. 2008;85(2):218–27. doi: 10.1016/j.healthpol.2007.07.012. [DOI] [PubMed] [Google Scholar]
- 112.Le Grand J. Equity, health, and health care. Soc Justice Res. 1987;1(3):257–74. [Google Scholar]
- 113.Nord E. The relevance of health state after treatment in prioritizing between different patients. J Med Ethics. 1993;19:37–42. doi: 10.1136/jme.19.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Nord E, Street A, Richardson J, et al. The significance of age and duration of effect in social evaluation of health care. Health Care Anal. 1996;4(2):103–11. doi: 10.1007/BF02251210. [DOI] [PubMed] [Google Scholar]
- 115.Ubel PA, DeKay ML, Baron J, et al. Cost-effectiveness analysis in a setting of budget constraints: is it equitable? N Eng J Med. 1996;334(18):1174–7. doi: 10.1056/NEJM199605023341807. [DOI] [PubMed] [Google Scholar]
- 116.Dolan P. The measurement of individual utility and social welfare. J Health Econ. 1998;17:39–52. doi: 10.1016/s0167-6296(97)00022-2. [DOI] [PubMed] [Google Scholar]
- 117.Johannesson M, Gerdtham U. A note on the estimation of the equity efficiency trade-off for QALYs. J Health Econ. 1996;15:359–68. doi: 10.1016/0167-6296(96)00005-7. [DOI] [PubMed] [Google Scholar]
- 118.Andersson F, Lyttkens C. Preferences for equity in health behind a veil of ignorance. Health Econ. 1999;8:369–78. doi: 10.1002/(sici)1099-1050(199908)8:5<369::aid-hec456>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 119.Wagstaff A. QALYs and the equity-efficiency tradeoff. J Health Econ. 1991;10:21–41. doi: 10.1016/0167-6296(91)90015-f. [DOI] [PubMed] [Google Scholar]
- 120.Borghi J. Aggregation rules for cost–benefit analysis: a health economics perspective. Health Econ. 2008;17(7):863–75. doi: 10.1002/hec.1304. [DOI] [PubMed] [Google Scholar]
- 121.Musgrove P. Cost-effectiveness as a criterion for public spending: a reply to William Jack's ‘second opinion’. Health Policy. 2000;54:229–33. doi: 10.1016/s0168-8510(00)00115-9. [DOI] [PubMed] [Google Scholar]
- 122.Jack W. Public spending on health care: how are different criteria related? A second opinion. Health Policy. 2000;53:61–7. doi: 10.1016/s0168-8510(00)00093-2. [DOI] [PubMed] [Google Scholar]
- 123.Robinson JS, Barth ACM, Feltes CH, et al. Economic impact model for the development of a statewide trauma system in Georgia. J Med Assoc Ga. 2007;96(3):10–3. [PubMed] [Google Scholar]
- 124.Creese A, Floyd K, Alban A, et al. Cost-effectiveness of HIV/AIDS interventions in Africa: a systematic review of the evidence. Lancet. 2002;359(9318):1635–42. doi: 10.1016/S0140-6736(02)08595-1. [DOI] [PubMed] [Google Scholar]
- 125.Baltussen R. Priority setting of public spending in developing countries: do not try to do everything for everybody. Health Policy. 2006;78(2-3):149–56. doi: 10.1016/j.healthpol.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 126.Baltussen R, ten Asbroek AHA, Koolman X, et al. Priority setting using multiple criteria: should a lung health programme be implemented in Nepal? Health Policy Plan. 2007;22:178–85. doi: 10.1093/heapol/czm010. [DOI] [PubMed] [Google Scholar]
- 127.Baltussen R, Niessen L. Priority setting of health interventions: the need for multi-criteria decision analysis. Cost Eff Resour Alloc. 2006;4(14):1–9. doi: 10.1186/1478-7547-4-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Tantivess S, Walt G. Using cost-effectiveness analyses to inform policy: the case of antiretroviral therapy in Thailand. Cost Eff Resour Alloc. 2006;4 doi: 10.1186/1478-7547-4-21. doi:10.1186/1478-7547-4-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Makundi E, Kapiriri L, Norheim OF. Combining evidence and values in priority setting: testing the balance sheet method in a low-income country. BMC Health Serv Res. 2007;7 doi: 10.1186/1472-6963-7-152. doi:10.1186/1472-6963-7-152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Birch S, Gafni A. The biggest bang for the buck or bigger bucks for the bang: the fallacy of the cost-effectiveness threshold. J Health Serv Res Policy. 2006;11(1):46–51. doi: 10.1258/135581906775094235. [DOI] [PubMed] [Google Scholar]
- 131.Kapiriri L, Martin DK. A strategy to improve priority setting in developing countries. Health Care Anal. 2007;15:159–67. doi: 10.1007/s10728-006-0037-1. [DOI] [PubMed] [Google Scholar]
- 132.Fox-Rushby JA, Hanson K. Calculating and presenting disability adjusted life years (DALYs) in cost-effectiveness analysis. Health Policy Plan. 2001;16(3):326–31. doi: 10.1093/heapol/16.3.326. [DOI] [PubMed] [Google Scholar]
- 133.Jamison DT, Shahid-Salles SA, Jamison J, et al. Incorporating deaths near the time of birth into estimates of the global burden of disease. In: Lopez AD, editor. Global burden of disease and risk factors. World Bank Publications; New York: 2006. [PubMed] [Google Scholar]
- 134.Simon J, Petrou S, Gray A. The valuation of prenatal life in economic evaluations of perinatal interventions. Health Econ. 2009;18(4):487–94. doi: 10.1002/hec.1375. [DOI] [PubMed] [Google Scholar]
- 135.Bloom DE, Canning D, Jamison DT. Health, wealth and welfare. Finance Dev. 2004;41:10–4. [Google Scholar]
- 136.Lopez-Casanovas G, Rivera B, Currais L. Health and economic growth: findings and policy implications. MIT Press; Cambridge (MA): 2005. [Google Scholar]
- 137.Sen A. Inequality re-examined. Harvard University Press; Cambridge (MA): 1992. [Google Scholar]