Abstract
Background
Patients after Fontan are at risk for suboptimal functional health status, and associations with laboratory measures are important for planning interventions and outcome measures for clinical trials.
Methods and Results
Parents completed the generic Child Health Questionnaire (CHQ) for 511 Fontan Cross-Sectional Study patients aged 6–18 years (61% male). Associations of CHQ Physical and Psychosocial Functioning Summary Scores (FSS) with standardized measurements from prospective exercise testing, echocardiography, magnetic resonance imaging (MRI), and measurement of brain natriuretic peptide (BNP) were determined by regression analyses. For exercise variables for maximal effort patients only, the final model showed higher Physical FSS was associated only with higher maximum work rate, accounting for 9% of variation in Physical FSS. For echocardiography, lower Tei index (particularly for patients with extracardiac lateral tunnel connections), lower indexed end-systolic volume, and the absence of atrioventricular valve regurgitation for patients having Fontan at age <2 years were associated with higher Physical FSS, accounting for 14% of variation in Physical FSS. For MRI, lower mass to end-diastolic volume ratio, and mid-quartiles of indexed end-systolic volume (non-linear) were associated with higher Physical FSS, accounting for 11% of variation. Lower BNP was significantly but weakly associated with higher Physical FSS (1% of variation). Significant associations for Psychosocial FSS with laboratory measures were fewer and weaker than for Physical FSS.
Conclusions
In relatively healthy Fontan patients, laboratory measures account for a small proportion of the variation in functional health status and, therefore, may not be optimal surrogate endpoints for trials of therapeutic interventions.
Keywords: Fontan procedure, heart defects, congenital, pediatrics
INTRODUCTION
A long term concern for patients after the Fontan procedure for palliation of functional single ventricle is the preservation and improvement of suboptimal functional health status. Important cardiac morbidities, including arrhythmia, ventricular dysfunction, protein-losing enteropathy and thrombosis, remain difficult to predict, prevent and treat.1 Changes in the specific venous anastomoses performed during the Fontan procedure have improved exercise capacity and decreased arrhythmias.2, 3 Strategies aimed at preventing thrombosis have been proposed which are only partially effective and not evidence-based.4 Strategies to preserve ventricular function, such as the use of angiotensin converting enzyme (ACE) inhibitors, have not shown benefit in limited study.5 Improved exercise capacity has been noted with exercise training programs, but the impact on functional health status and activity levels is not known.6, 7 A rationale for intervention strategies is incomplete, since associations between laboratory measures and functional health status are not well characterized, making it difficult to plan clinical trials likely to answer important management questions.
The Fontan Cross-Sectional Study was designed by the Pediatric Heart Network (PHN) to identify a quantifiable measure of cardiovascular performance that is associated with clinical outcome assessed by a validated functional health status instrument in children and adolescents after Fontan procedure.8 The study enrolled Fontan patients age 6 to 18 years and included assessment of patient characteristics and medical history, functional health status, and standardized assessment with cardiopulmonary exercise testing, echocardiography, magnetic resonance imaging (MRI) and measurement of brain natiuretic peptide (BNP).8, 9 The purpose of the current analysis was to determine associations between laboratory measures and functional health status in children and adolescents after the Fontan procedure, as well as interactions with a pre-specified set of patient characteristics.
METHODS
Study Design
The Fontan Cross-Sectional Study was performed by the PHN, consisting of 7 pediatric cardiac centers in the United States and Canada, a data coordinating center at the New England Research Institutes, a PHN chair and staff from the National Heart, Lung and Blood Institute of the National Institutes of Health.10 The design and methods of the study have been previously described.8 Institutional ethical review and approval was obtained from each participating institution, and written informed consent or assent was obtained for all study participants or their legal guardian.
Study Subjects
Study subjects were eligible if they were age 6 to 18 years at enrollment, had a Fontan procedure at least 6 months before initial testing, and agreed to complete the functional health status questionnaire and undergo study laboratory testing within 3 months of enrollment. Patients with important non-cardiac or psychiatric conditions precluding or influencing testing, pregnancy or planned pregnancy, current or planned participation in another conflicting research study, or whose primary caregiver lacked reading fluency in English or Spanish were deemed not eligible. A detailed medical record review for eligible and consenting participants was performed.
Functional Health Status Questionnaire
Functional health status was assessed by having a parent complete the parent report version of the Child Health Questionnaire (CHQ-PF50).11 The CHQ assesses functional health status in twelve domains of physical, behavioral, social and emotional well-being, and has been validated for use in children aged 5 to 18 years. Domain scores contribute to a Physical and a Psychosocial Functioning Summary Score (FSS), which were used for analysis in the current report.
Laboratory Testing
Details of the laboratory testing procedures have been reported elsewhere.8 Resting serum BNP concentration was determined in a single laboratory using standardized methods. Echocardiography and MRI were performed according to standardized protocols, and transmitted to core reading laboratories for central measurement, interpretation and data completion. Maximal cardiopulmonary exercise testing was performed using cycle ergometry and a standardized protocol. Measurements from exercise testing were made locally and transmitted to the Data Coordinating Center.
Data Analysis
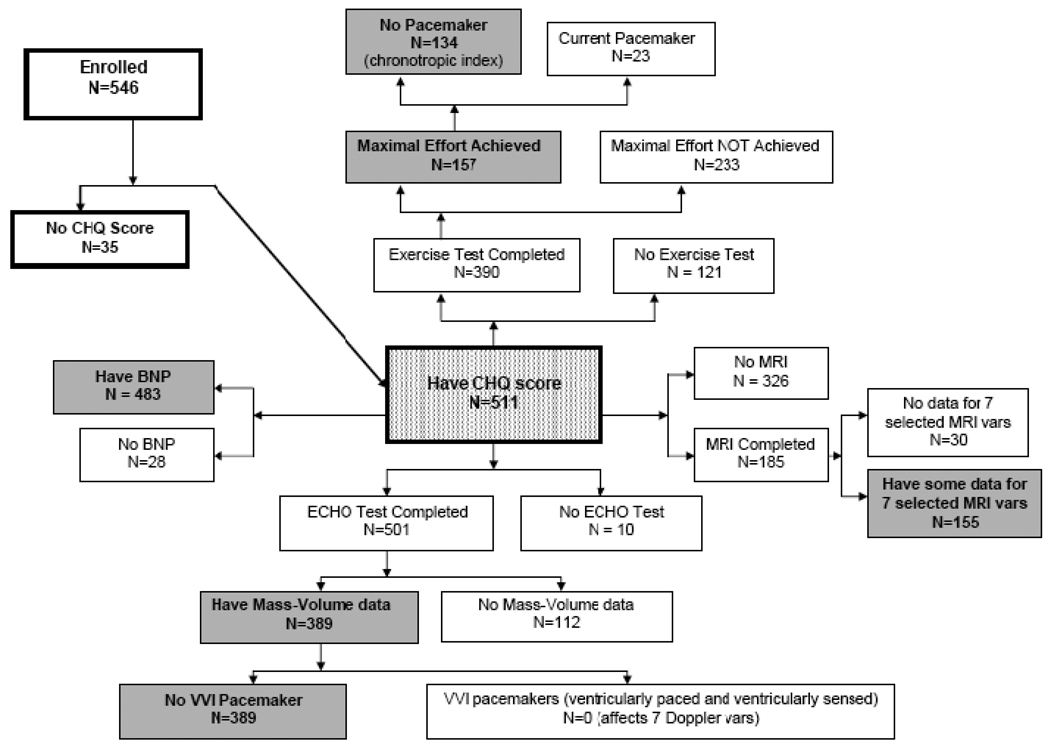
Data are described as frequencies, medians with 25th and 75th percentile values, and means with standard deviations as appropriate. Given the skewed distribution of BNP values, a normalizing logarithmic transformation was performed. The study population used for analysis was restricted to those patients with both Physical Psychosocial FSS from the parent-completed CHQ. Since all tests were not performed in all patients (Figure 1), analyses were restricted to individual test datasets, and no overall analysis incorporating all tests was performed.
Figure 1. Level of Participation of PHN Fontan Cross-Sectional Study Enrolled Subjects.
BNP, brain natriuretic peptide; CHQ, Child Health Questionnaire; ECHO, echocardiography; MRI, magnetic resonance imaging; PHN, Pediatric Heart Network; vars, variables
Since data derived from exercise testing performed with submaximal effort are of questionable validity and without normative values, analysis of associations with cardiopulmonary exercise variables was restricted to those patients who had a maximal effort, defined as a respiratory exchange ratio ≥1.1. Furthermore, analysis of chronotropic index was also restricted to those patients without a pacemaker. Analyses of echocardiographic and MRI variables were restricted to those tests for which suitable ventricular mass and volume data were obtained. MRI variables for ventricular end systolic and diastolic volume and mass were indexed to body surface area1.3 (BSA1.3), and echocardiographic quantitative variables were converted to Z scores based on BSA using published normal values and methods.12 Separate analyses were performed for the Physical and the Psychosocial FSS. Univariable associations between the Scores and each testing variable were first performed without any imputation of missing values. BNP values demonstrated a non-normal distribution, and a normalizing logarithmic transformation was performed (logBNP), and associations determined with this variable. Missing values were minimal for the exercise testing and MRI datasets, but were more frequent in the echocardiography dataset. Mean imputation of the missing values in the echocardiography dataset was performed before multivariable regression analyses. Multivariable linear regression analysis of each testing dataset was performed initially with all testing variables included, to determine overall R2 adjusted for the number of included variables. Stepwise multivariable regression was performed for both Scores, with further testing for non-linear associations. Variable selection for final models was also guided by bootstrap bagging (1000 random sample datasets) to assess reliability (percentage of random sample datasets for which the variable was selected) for inclusion. Interactions with testing variables were sought only for six pre-specified categorical patient characteristics, which included gender, dominant ventricular morphology, staging with a cavopulmonary anastomosis, age at Fontan, type of Fontan connection and age at enrollment. Given the large number of potential interaction terms, only interactions with p≤0.01 were considered significant for inclusion in final regression models. Data analyses were performed using SAS statistical software version 9.1 (SAS Institute Inc., Cary, NC).
The authors had full access to the data and take full responsibility for its integrity. All authors have read and agree to the manuscript as written.
RESULTS
Study Participation
Medical records were screened for 1078 patients, with 831 potentially eligible for participation. After being contacted, 637 patients were fully eligible, and consent was obtained for 546 (86%). Of these, 511 had a fully completed parent-report CHQ and were included in the current analysis. Only 118 patients (23%) completed all laboratory tests, while 275 (54%) completed all tests except MRI. The number of patients who underwent each type of test is shown in Figure 1.
Patient Characteristics
Patient and medical characteristics together with their associations with parent-completed CHQ Physical and Psychosocial FSS have been reported previously.13 Selected characteristics of the 511 subjects included in the present analysis are shown in Supplemental Table 1, as well as results from the CHQ and laboratory testing. Mean Physical and Psychosocial FSS were 45±12 and 47±11, respectively.
Associations with CHQ Summary Scores
BNP
BNP concentration was measured in 483 of the 511 study subjects. Higher logBNP was significantly but weakly related to lower CHQ Physical FSS (parameter estimate = −1.50; p=0.009; R2=0.01; parameter estimates represent the degree of change in the summary score associated with a one integer unit change in the laboratory testing variable). There were no significant interactions with the six pre-specified patient characteristic variables. BNP was not significantly associated with CHQ Psychosocial FSS, and there were no significant interactions with the six pre-specified patient characteristic variables.
Cardiopulmonary Exercise Testing
Of the 511 study subjects, 390 had cardiopulmonary exercise testing. Of these, only 157 (40%) achieved a maximal effort as indicated by a respiratory exchange ratio >1.1. The number of missing values was very small on the maximal effort subset (only 4 missing values for all the variables under consideration), so imputation of missing values was not performed. Chronotropic index was not considered for 23 patients who had a pacemaker at testing.
For CHQ Physical FSS, when all six exercise testing variables were included in a multivariable model, the R2 was 0.094 (R2 adjusted=0.049) with p=0.06 (n=130). In univariable analyses, higher CHQ Physical FSS was significantly associated with higher percent predicted maximum work rate, higher percent predicted VO2 at peak exercise, higher percent predicted VO2 at anaerobic threshold, and higher percent predicted maximum oxygen pulse. The relationship between Score and percent predicted VO2 at anaerobic threshold appeared to be non-linear, but various transformations did not improve the model fit. In multivariable analysis, only higher percent predicted maximum work rate was significant, with a model R2 of 0.086 and p<0.001 (Table 1). There were no significant interactions between the six pre-specified patient characteristic variables and any of the exercise testing variables.
Table 1.
Association between CHQ Physical Functioning Summary Score and Cardiopulmonary Exercise Testing*
| Univariable | Multivariable** | ||||
|---|---|---|---|---|---|
| Variable | PE | p | PE | p | Reliability*** |
| Percent predicted maximum work rate (%) | 0.216 | <0.001 | 0.216 | <0.001 | 79% |
| Percent predicted VO2 at peak exercise (%) | 0.198 | <0.001 | |||
| Percent predicted VO2 at anaerobic threshold (%) | 0.108 | 0.003 | |||
| Percent predicted maximum oxygen pulse (%) | 0.079 | 0.03 | |||
| Resting oxygen saturation (%) | 0.134 | 0.49 | |||
| Chronotropic index | 1.699 | 0.77 | |||
PE, parameter estimate; VO2, oxygen consumption
Parameter estimates represent the degree of change in the Summary Score associated with a one integer unit change in the laboratory testing variable.
Analysis limited to 157 subjects with maximal effort indicated by a respiratory exchange ratio >1.1. Additionally, analysis of chronotropic index was further limited to those 134 subjects who did not have a current pacemaker.
R2=0.086 (R2 adjusted=0.079), p<0.001, n=157
From bootstrap bagging (presented for the variables included in the multivariable model)
For CHQ Psychosocial FSS, when all six exercise testing variables were included in a multivariable model, the R2 was 0.05 (R2 adjusted=0.01) with p=0.31 (n=130). In univariable analyses, there were no significant linear or non-linear associations. A stepwise multivariable analysis showed higher CHQ Psychosocial FSS was significantly associated with higher percent predicted maximum work rate (p<0.05), but the inclusion in the data set of chronotropic index restricted the analysis to 130 patients with available data, with no significant univariable association noted over the full exercise testing data set (p=0.40). Exploration for interactions with the six pre-specified patient characteristics showed a significant interaction between gender and resting oxygen saturation (p=0.007). Higher CHQ Psychosocial FSS was associated with higher resting oxygen saturation for females (parameter estimate 0.825; p=0.006) and no association for males (parameter estimate −0.271; p=0.32) (model R2=0.06, adjusted R2=0.04, p<0.001, n=156).
Echocardiography
Of the 511 study subjects with CHQ summary scores, 501 underwent echocardiography, with 389 subjects having suitable mass-volume data available. None of the patients with pacemakers were being paced in VVI mode at testing, and thus diastolic function parameters were considered valid.
For CHQ Physical FSS, when all sixteen echocardiography variables were included in a multivariable model (n=63), the model R2 was 0.29 (R2 adjusted=0.04) with p=0.49. With mean imputation of missing values, the multivariable model R2 was 0.07 (R2 adjusted=0.03) with p=0.12 (n=388). In univariable analyses without mean imputation, higher CHQ Physical FSS was significantly associated with lower end-systolic and end-diastolic volume Z scores, lower ventricular mass Z score, and lower atrioventricular valve peak late diastolic velocity. In multivariable analysis with imputation of missing values, only lower end-systolic volume Z score and lower Tei index were significantly and independently related to higher Score, with a model R2=0.03 (adjusted R2=0.02) and p=0.005 (n=389) from a data set with mean imputation of missing values (Table 2). Tei index was included in the final model despite borderline statistical significance as it was more reliable than other variables in bootstrapping. When Tei index was excluded from the model, only end-systolic volume Z score was selected for inclusion in a final model.
Table 2.
Association between CHQ Physical Functioning Summary Score and Echocardiography*
| Univariable | Multivariable** | ||||
|---|---|---|---|---|---|
| Variable | PE | p | PE | p | Reliability*** |
| Overall AV valve regurgitation | 0.27 | ||||
| None | reference | ||||
| Mild | 1.214 | ||||
| Moderate or severe | −1.448 | ||||
| Semilunar valve regurgitation | 0.77 | ||||
| None | reference | ||||
| Mild | 0.615 | ||||
| Moderate | 1.910 | ||||
| End-systolic volume Z score | −0.718 | 0.005 | −0.689 | 0.007 | 43% |
| End-diastolic volume Z score | −0.810 | 0.02 | |||
| Total stroke volume Z score | −0.488 | 0.16 | |||
| Total ejection fraction Z score | 0.423 | 0.17 | |||
| Total ventricular mass Z score | −0.700 | 0.02 | |||
| Total mass:end-diastolic volume ratio | 0.225 | 0.89 | |||
| Tei index | −7.160 | 0.08 | −6.422 | 0.10 | 48% |
| dP/dt (mm Hg/sec) | 0.000 | 0.63 | |||
| AVV peak late diastolic velocity (m/sec) | −11.02 | <0.05 | |||
| Early:late AVV diastolic velocity (E/A) | 1.580 | 0.23 | |||
| Duration of AVV late diastolic inflow (msec) | −0.026 | 0.33 | |||
| Absolute systemic ventricular flow propagation rate (cm/sec) | 0.040 | 0.40 | |||
| Ratio of AV to tissue Doppler early diastolic flow velocity | −0.158 | 0.41 | |||
| Tissue Doppler peak early diastolic flow velocity (cm/sec) | −0.122 | 0.56 | |||
PE, parameter estimate
Parameter estimates represent the degree of change in the Summary Score associated with a one integer unit change in the laboratory testing variable.
Analysis limited to 389 subjects. Of those with a current pacemaker, none were being paced in a VVI mode. Missing values were not imputed for univariable analyses, and were imputed for multivariable analyses.
R2=0.03 (R2 adjusted=0.02), p=0.005
From bootstrap bagging (presented for the variables included in the multivariable model)
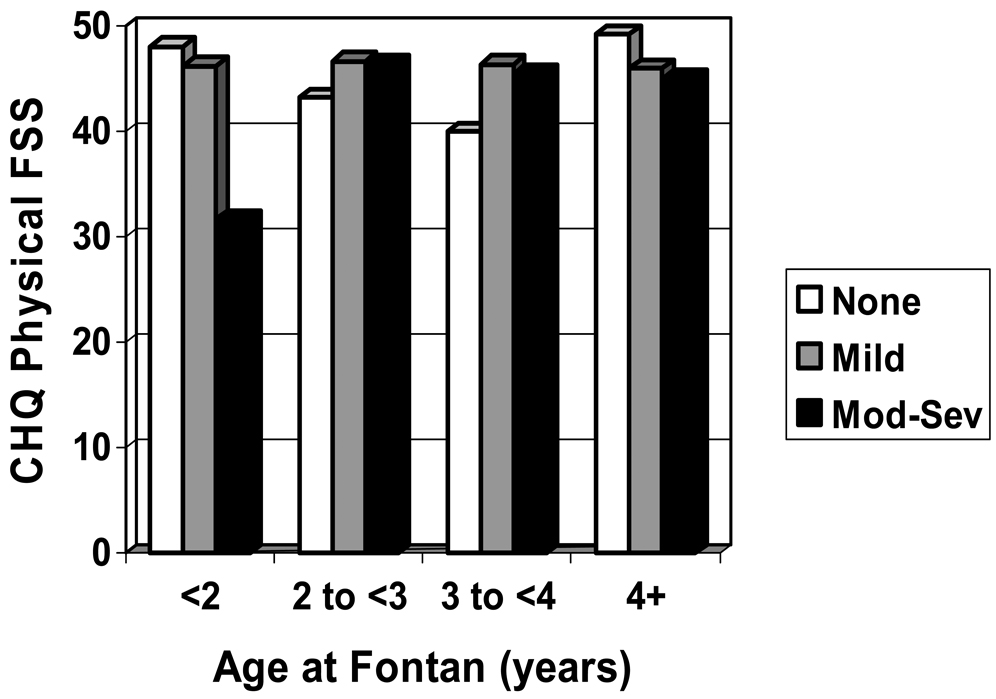
Interactions with the six pre-specified patient characteristics were explored with mean imputation of missing values. There was a significant interaction between Tei index and type of Fontan connection (p=0.001). The negative relationship between a lower Tei index and higher Score was largest and most significant for patients with an extracardiac lateral tunnel connection versus all other connection types. In addition, there was a significant interaction between the presence of moderate or severe atrioventricular valve regurgitation and age at Fontan (p=0.005). The presence of moderate or severe regurgitation appeared to have a particularly detrimental effect on Physical FSS only for patients who had their Fontan procedure at age <2 years (Figure 2). When these two interactions were included in the final multivariable model, the R2 increased to 0.15 (R2 adjusted=0.14) with p<0.001 (n=388).
Figure 2. Interaction of Subjective Grade of Atrioventricular Valvar Regurgitation from Echocardiography with Age at Fontan and the Association with Physical Functioning Summary Score.
The detrimental impact of moderate or severe atrioventricular valve regurgitation appears to be limited to patients who had Fontan at <2 years of age.
CHQ, Child Health Questionnaire; FSS, Functioning Summary Score; Mod-Sev, moderate to severe
For CHQ Psychosocial FSS, when all sixteen echardiography variables were included in a multivariable model, the model R2 was 0.12 (R2 adjusted <0.01) with p>0.99 (n=63). With mean imputation of missing values, the multivariable model R2 was 0.07 (R2 adjusted=0.03) with p=0.11 (n=388). In univariable analyses, higher CHQ Psychosocial FSS was significantly associated with higher Tei index and lower total ventricular mass Z score. A stepwise multivariable regression analysis from a data set with mean imputation included both of these variables in a final model, with a parameter estimate for Tei index of 8.83 per integer unit increment (p=0.01) and for total ventricular mass Z score of −0.57 (p=0.02), with a model R2 of 0.03 (adjusted R2=0.02) (p=0.004). When interactions with the six pre-specified patient characteristics were explored, the only significant interaction was between dominant ventricular morphology and ratio of early to late atrioventricular valve diastolic velocities (E/A ratio) (p=0.006). It appeared that the positive relationship between increasing Psychosocial FSS and increasing E/A ratio was restricted to those patients with non-LV morphology. When this interaction term was included in the final multivariable model, the model R2 increased to 0.07 (R2 adjusted=0.06) with p<0.001.
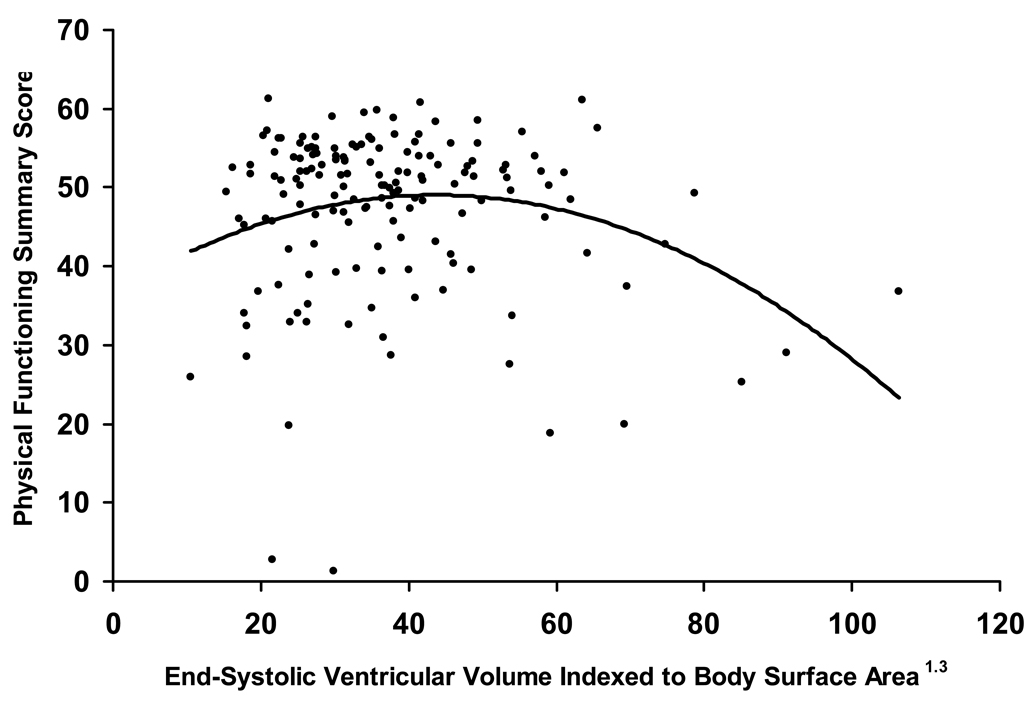
MRI
Of the 511 study subjects, 185 had MRI, with 155 having sufficient data for the 7 studied variables. Since there were only two missing values for these seven variables over 155 subjects, imputation was not performed. Subjects who underwent MRI were comparable to the remaining subjects regarding demographics and non-MRI study test results (data not shown; no significant differences). For Physical FSS, when all seven MRI variables were included in a multivariable model, the R2 was 0.13 (R2 adjusted=0.09) with p=0.004 (n=153). In univariable analyses, higher CHQ Physical FSS was significantly associated with lower mass:end-diastolic volume ratio and lower total ventricular mass indexed to BSA1.3. Total end-systolic volume indexed to BSA1.3 appeared to have a non-linear relationship to Score from non-parametric analysis, and several transformations were explored. The variable became significant when a quadratic term was included in addition to the linear term in the model (Figure 3). In multivariable analysis, lower mass:end-diastolic volume ratio and lower and higher total end-systolic volume indexed to BSA1.3 were significantly and independently related to higher Score, with a model R2=0.12 (adjusted R2=0.11) with p<0.001 (n=153) (Table 3). There were no significant interactions between the six pre-specified patient characteristic variables and any of the MRI variables.
Figure 3. Non-Linear Relationship Between MRI-Assessed End-Systolic Ventricular Volume Indexed to Body Surface Area (mL/m1.3) and Physical Functioning Summary Score.
Table 3.
Association between CHQ Physical Functioning Summary Score and MRI*
| Univariable | Multivariable** | ||||
|---|---|---|---|---|---|
| Variable | PE | p | PE | p | Reliability*** |
| Total ESV indexed to BSA1.3 (mL/m2) | −0.057 | 0.30 | 0.437 | 0.03 | 36% |
| (Total ESV/BSA1.3)2 | −0.006 | 0.004 | 56% | ||
| Total EDV indexed to BSA1.3 (mL/m2) | −0.006 | 0.87 | |||
| Total stroke volume (mL) | 0.045 | 0.19 | |||
| Total ejection fraction (per cent) | 0.075 | 0.43 | |||
| Cardiac output (L/min) | 0.326 | 0.52 | |||
| Total ventricular mass indexed to BSA1.3 (gm/m2) | −0.099 | 0.02 | |||
| Total mass/EDV ratio (gm/mL) | −7.068 | 0.02 | −8.366 | 0.004 | 56% |
BSA, body surface area; EDV, end-diastolic volume; ESV, end-systolic volume; gm, grams; L, litres; m, meters; mL, milliliters; min, minute; PE, parameter estimate.
Parameter estimates represent the degree of change in the Summary Score associated with a one integer unit change in the laboratory testing variable.
Analysis limited to 155 subjects with values for the 7 variables. Missing values were not imputed.
R2=0.12 (R2 adjusted=0.11), p<0.001 (n=153). Final multivariable model includes a significant quadratic term for total end-systolic volume indexed to BSA1.3, indicating a non-linear relationship.
From bootstrap bagging (presented for the variables included in the multivariable model)
For Psychosocial FSS, when all seven MRI variables were included in a multivariable model, the R2 was 0.02 (R2 adjusted < 0.01) with p=0.85 (n=153). In univariable analyses, CHQ Psychosocial FSS was not significantly associated with any of the MRI variables. For the six pre-specified patient characteristics, there was a significant interaction between total end-diastolic volume indexed to BSA1.3 and age at Fontan (p=0.005). A multivariable model with the interaction term and both variables had a model R2 of 0.12 (adjusted R2=0.10) with a p=0.02. The interaction showed that lower Psychosocial FSS was significantly related to higher total end-diastolic volume indexed to BSA1.3 for patients who had their Fontan at age <2 years (parameter estimate −0.19; p=0.02) and age of 4 years or more (parameter estimate −0.16; p<0.05), versus those at age 2 years (parameter estimate 0.01; p=0.83) or age 3 years (parameter estimate 0.13; p=0.08).
DISCUSSION
Summary
Summary score measures of both physical and psychosocial functional health status were only weakly associated with objective laboratory measures reflecting various physiologic and pathophysiologic parameters. Some associations are of interest. Higher Physical FSS was weakly associated with more optimal measures of exercise capacity, most significantly higher maximum work rate. A weak but statistically significant association was noted between lower BNP levels and higher Physical FSS. Physiologic assessment from imaging modalities showed weak but statistically significant associations of higher Physical FSS with more optimal ventricular size, mass, and indices of both systolic and diastolic function. Some of these associations were modified by other factors, such as age at Fontan and Fontan connection type. For example, the presence of moderate or severe grade of atrioventricular valvar regurgitation was associated with lower Physical FSS only for those having Fontan at <2 years of age. Psychosocial FSS was weakly associated with limited variables from laboratory testing, usually in relation to interactions with the six pre-specified categorical patient characteristics, and the possibility that these associations may be spurious cannot be excluded.
Functional health status and relationship to patient and medical characteristics
CHQ Summary Scores in this cohort were lower than published Scores from subjects with other types of chronic health conditions.13 A previous focused analysis showed that lower Physical FSS was significantly associated with higher patient weight at Fontan, no fenestration performed, other surgical procedures performed at Fontan, arrhythmias during follow-up and higher number of current medications.13 In addition, associated non-cardiac medical conditions, including asthma, non-asthma respiratory problems, and orthopedic problems, were independently associated with lower Scores. Psychosocial factors, including learning problems, lower family income, and parent not working because of patient’s health, were also independently associated with lower Scores. These factors accounted for 40% of the variation in Physical FSS, much more than any combination of laboratory variables in the present analysis. Lower Psychosocial FSS was associated only with psychosocial factors, including lower family income and problems with behavior, learning, anxiety, attention and depression, accounting for 34% of the variation in Scores. The current analysis showed limited and weak associations between Psychosocial FSS and laboratory variables. Current medical and psychosocial conditions appear to be more strongly associated with functional health status than Fontan specific factors, including those measured objectively.
Relationship to BNP
BNP level explained only 1% of the variation observed in Physical FSS, with patients having higher BNP having lower Physical FSS. Our findings are consistent with smaller single center reports using less specific health status indices. In patients evaluated in the outpatient setting a median of 9 years after Fontan, those in New York Heart Association (NYHA) class I (n=55) had lower BNP than those in class II (n=12).14 Similarly amino-terminal pro-brain natriuretic peptide (NT-pro-BNP) has been correlated with a higher index of heart failure using the New York University Pediatric Heart Failure Index in 59 children and adolescents at a median of 8 years after Fontan.15 Among adults after Fontan, higher BNP differentiated patients in NYHA class II from NYHA class III and IV.16 In a single center study of heterogeneous adult patients with a systemic right ventricle, BNP was elevated and was related to NYHA class but not to exercise capacity or echocardiography assessed function.17 The BNP values noted in our study were within an age-adjusted normal range in the majority of patients. This likely reflects the compensated state of the relatively healthy outpatient cohort that was enrolled. The relationship of BNP to functional health status may be stronger among symptomatic Fontan patients.
Relationship to exercise capacity
While patients who achieved maximal effort had diminished exercise capacity, exercise variables were not strongly associated with functional health status. A previous focused analysis of this cohort has shown that peak oxygen consumption was 65% of normal, with only 40% achieving maximal capacity.18 Oxygen consumption at ventilatory anaerobic threshold was better preserved, and associations with echocardiographic indices of ventricular function were weak. Better exercise capacity was associated with higher oxygen pulse at peak exercise, probably a surrogate for higher stroke volume.
The majority of subjects failed to achieve maximal aerobic capacity, and pulmonary, musculoskeletal deconditioning and motivational factors may be important determinants. Deconditioning may be related to poor levels of physical activity,19 possibly reflective of increased parental and patient anxiety and uncertainty around physical activity. Many patients in this cohort were reported to have asthma or non-asthma respiratory conditions, and abnormalities of pulmonary function have been previously reported.20 Pulmonary function abnormalities and musculoskeletal deconditioning may have at least as important an impact on perceived physical functioning in this population as aerobic capacity. The limited association (only 9% of the variation in Physical FSS explained) between the measures of aerobic capacity and functional health status in the current study population for those who achieved a maximal aerobic effort would support this notion. This would suggest that interventions designed to improve physical functioning should address these issues as well as aerobic capacity.
Rehabilitation through exercise training programs show improved exercise capacity7, 21 and muscle function.22 Although exercise training programs have shown modest improvements in aerobic capacity, these programs are resource intensive, and interventions aimed at improving physical activity levels may prove more feasible. Improved control of asthma or improved muscle strength may result in a more significant enhancement of physical functioning than attempts to improve aerobic capacity. Limited data are available regarding pharmacologic interventions. Sildenafil treatment has been shown to be associated with improvements in exercise capacity,23 while no effect has been noted with treatment with enalapril.5 Improvements in the surgical management of single ventricle patients have been associated with better exercise capacity, including earlier volume unloading surgery24 and avoidance of and conversion from atriopulmonary Fontan connection type.2 The role of fenestration closure is less clear.25 The development and study of interventions aimed at improving exercise capacity might include measures of functional health status.
Valvar function, ventricular size and performance and relationship to functional health status
Measures of valvar function, ventricular volumes, mass and mass/volume relationships were weakly associated with Physical FSS, accounting for only 14% of the variation in Scores (6% for Psychosocial FSS) in the final multivariable model for echocardiographic variables and 11% (10% for Psychosocial FSS) for MRI variables. Both systolic and diastolic functional abnormalities have been reported after the Fontan, with diastolic functional abnormalities of both compliance and relaxation reported to worsen with time.26, 27 Effective interventions to reduce ventricular volumes, preserve systolic function, manage diastolic dysfunction and prevent or treat inappropriate hypertrophy have not been developed or studied. There is some evidence that earlier volume unloading is beneficial.26 The relationship of neurohumoral activation to these abnormalities is unclear, although it is present and does not appear to be related to functional health status.16
Study limitations
The results of this study should be viewed in light of some limitations. The subjects represented a subgroup of available current survivors, although enrolled versus non-enrolled eligible subjects did not differ in important ways.8 The level of participation of enrolled subjects was not uniform for all laboratory tests, and may have been influenced by factors associated with functional health status. In addition, analysis of associations with cardiopulmonary exercise variables was restricted to those with maximal effort. These factors may have introduced some selection bias, although the focus of the current analysis was on determining associations. The study population was relatively well, and this may have contributed to the lack of strong associations noted. Many interventions proposed for study in Fontan patients have been aimed at primary prevention (preventing ventricular dysfunction, arrhythmias, thrombosis, exercise intolerance), and, thus, the population we studied would be the target population and the associations explored would be the ones of interest. Functional health status was determined from parent or proxy report, which may differ from that reported by the child or adolescent, although the age range of the subjects precluded uniform administration of the Child Report form of the CHQ. A few of the variables reported, such as subjective grade of valvar regurgitation, may have been less valid and reliable, although no gold standard currently exists for use in a heterogenous group of functional single ventricle patients. Given the large number of variables tested, we may have observed spurious associations arising from multiple comparisons. For this reason, only results from multivariable analyses are emphasized, and variable selection was confirmed with bootstrapping for reliability. Finally, the clinical meaning of the observed associations is unclear, given their relatively small magnitude.
Conclusions
In a spectrum of Fontan patients, variation in exercise capacity and ventricular characteristics and performance explains only a small proportion of the variation in functional health status. Laboratory measures may not be optimal surrogate endpoints in trials of therapeutic interventions aimed at improving functional health status for Fontan patients, and functional health status assessment should be included. Our supposition is that patients would be more likely to benefit from interventions aimed at psychosocial and behavioral factors in terms of improving functional health status. Preventive medical interventions have not been shown to be of benefit, and treatment interventions might be effective once the patient passes a certain pathophysiologic threshold. Potential strategies and initiatives suggested by the PHN Fontan Cross-Sectional Study that may influence suboptimal functional health status and its assessment for Fontan patients and that might be the topic of further study include:
Coordinated and effective management of non-cardiac medical conditions.13
Coordinated and effective prevention, identification and management of learning, behavior and emotional problems.13
Specific targeting of interventions for patients from low income households.13
Development and evaluation of cardiovascular rehabilitation programs.
Development of a disease-specific assessment tool for functional health status that is responsive to laboratory measures.
Ongoing study regarding laboratory abnormalities and their association with functional health status, particularly longitudinal changes into adulthood.
Clinical Summary
As mortality has declined dramatically for repair of even the most complex congenital heart disease patients, clinical care will increasingly focus on preventing and treating morbidities, and improving functional health status. Patients with functional single ventricle who have had Fontan procedure are at high risk for suboptimal functional health status. Determination of associations of functional health status with laboratory measures, which may suggest pathophysiologic mechanisms, are important for planning interventions and outcome measures for clinical trials. We performed a cross-sectional assessment of patients aged 6 to 18 years who had undergone the Fontan procedure. Our results showed that laboratory measures of exercise capacity and ventricular characteristics and function, as assessed objectively by brain natiuretic peptide levels, exercise testing, echocardiography and magnetic resonance imaging, were only weakly associated with results from a validated questionnaire measure of physical and psychosocial functional health status. This suggests that strategies aimed at preserving indices of ventricular form and function as assessed by laboratory testing may have little effect on current functional health status. The impact of treatment strategies targeted towards those with important laboratory abnormalities in the pathologic range may influence functional health status to an unknown degree, but should be an important component of future studies. Strategies targeting functional health status and its non-cardiac determinants directly, such as through rehabilitation programs and addressing psychosocial morbidities, may have a greater impact on health-related quality of life. Such programs should be developed and evaluated for these high risk and complex patients.
Supplementary Material
Acknowledgments
FUNDING SOURCES
Supported by U01 grants from the NIH, National Heart, Lung, and Blood Institute (HL068269, HL068270, HL068279, HL068281, HL068285, HL068292, HL068290, HL068288)
Footnotes
DISCLOSURES
None
REFERENCES
- 1.Freedom RM, Hamilton R, Yoo SJ, Mikailian H, Benson L, McCrindle B, Justino H, Williams WG. The Fontan procedure: analysis of cohorts and late complications. Cardiol Young. 2000;10:307–331. doi: 10.1017/s1047951100009616. [DOI] [PubMed] [Google Scholar]
- 2.Giardini A, Napoleone CP, Specchia S, Donti A, Formigari R, Oppido G, Gargiulo G, Picchio FM. Conversion of atriopulmonary Fontan to extracardiac total cavopulmonary connection improves cardiopulmonary function. Int J Cardiol. 2006;113:341–344. doi: 10.1016/j.ijcard.2005.11.046. [DOI] [PubMed] [Google Scholar]
- 3.Azakie A, McCrindle BW, Van Arsdell G, Benson LN, Coles J, Hamilton R, Freedom RM, Williams WG. Extracardiac conduit versus lateral tunnel cavopulmonary connections at a single institution: impact on outcomes. J Thorac Cardiovasc Surg. 2001;122:1219–1228. doi: 10.1067/mtc.2001.116947. [DOI] [PubMed] [Google Scholar]
- 4.Monagle P, Cochrane A, McCrindle B, Benson L, Williams W, Andrew M. Thromboembolic complications after fontan procedures--the role of prophylactic anticoagulation. J Thorac Cardiovasc Surg. 1998;115:493–498. doi: 10.1016/s0022-5223(98)70310-1. [DOI] [PubMed] [Google Scholar]
- 5.Kouatli AA, Garcia JA, Zellers TM, Weinstein EM, Mahony L. Enalapril does not enhance exercise capacity in patients after Fontan procedure. Circulation. 1997;96:1507–1512. doi: 10.1161/01.cir.96.5.1507. [DOI] [PubMed] [Google Scholar]
- 6.Brassard P, Bedard E, Jobin J, Rodes-Cabau J, Poirier P. Exercise capacity and impact of exercise training in patients after a Fontan procedure: a review. Can J Cardiol. 2006;22:489–495. doi: 10.1016/s0828-282x(06)70266-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rhodes J, Curran TJ, Camil L, Rabideau N, Fulton DR, Gauthier NS, Gauvreau K, Jenkins KJ. Impact of cardiac rehabilitation on the exercise function of children with serious congenital heart disease. Pediatrics. 2005;116:1339–1345. doi: 10.1542/peds.2004-2697. [DOI] [PubMed] [Google Scholar]
- 8.Sleeper LA, Anderson P, Hsu DT, Mahony L, McCrindle BW, Roth SJ, Saul JP, Williams RV, Geva T, Colan SD, Clark BJ. Design of a large cross-sectional study to facilitate future clinical trials in children with the Fontan palliation. Am Heart J. 2006;152:427–433. doi: 10.1016/j.ahj.2006.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anderson PA, Sleeper LA, Mahony L, Colan SD, Atz AM, Breitbart RE, Gersony WM, Gallagher D, Geva T, Margossian R, McCrindle BW, Paridon S, Schwartz M, Stylianou M, Williams RV, Clark BJ., 3rd Contemporary outcomes after the Fontan procedure: a Pediatric Heart Network multicenter study. J Am Coll Cardiol. 2008;52:85–98. doi: 10.1016/j.jacc.2008.01.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mahony L, Sleeper LA, Anderson PA, Gersony WM, McCrindle BW, Minich LL, Newburger JW, Saul JP, Vetter VL, Pearson GD. The Pediatric Heart Network: a primer for the conduct of multicenter studies in children with congenital and acquired heart disease. Pediatr Cardiol. 2006;27:191–198. doi: 10.1007/s00246-005-1151-9. [DOI] [PubMed] [Google Scholar]
- 11.Landgraf JM, Abetz L, Ware JE. The Child Health Questionnaire (CHQ) User's Manual, 2nd printing. Boston, MA: HealthAct; 1999. [Google Scholar]
- 12.Sluysmans T, Colan SD. Theoretical and empirical derivation of cardiovascular allometric relationships in children. J Appl Physiol. 2005;99:445–457. doi: 10.1152/japplphysiol.01144.2004. [DOI] [PubMed] [Google Scholar]
- 13.McCrindle BW, Williams RV, Mitchell PD, Hsu DT, Paridon SM, Atz AM, Li JS, Newburger JW. Relationship of patient and medical characteristics to health status in children and adolescents after the Fontan procedure. Circulation. 2006;113:1123–1129. doi: 10.1161/CIRCULATIONAHA.105.576660. [DOI] [PubMed] [Google Scholar]
- 14.Koch AM, Zink S, Singer H, Dittrich S. B-type natriuretic peptide levels in patients with functionally univentricular hearts after total cavopulmonary connection. Eur J Heart Fail. 2008;10:60–62. doi: 10.1016/j.ejheart.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 15.Lechner E, Gitter R, Mair R, Pinter M, Schreier-Lechner E, Vondrys D, Tulzer G. Aminoterminal brain natriuretic peptide levels in children and adolescents after Fontan operation correlate with congestive heart failure. Pediatr Cardiol. 2008;29:901–905. doi: 10.1007/s00246-008-9225-0. [DOI] [PubMed] [Google Scholar]
- 16.Ohuchi H, Takasugi H, Ohashi H, Yamada O, Watanabe K, Yagihara T, Echigo S. Abnormalities of neurohormonal and cardiac autonomic nervous activities relate poorly to functional status in fontan patients. Circulation. 2004;110:2601–2608. doi: 10.1161/01.CIR.0000145545.83564.51. [DOI] [PubMed] [Google Scholar]
- 17.Larsson DA, Meurling CJ, Holmqvist F, Waktare JE, Thilen UJ. The diagnostic and prognostic value of brain natriuretic peptides in adults with a systemic morphologically right ventricle or Fontan-type circulation. Int J Cardiol. 2007;114:345–351. doi: 10.1016/j.ijcard.2006.01.023. [DOI] [PubMed] [Google Scholar]
- 18.Paridon SM, Mitchell PD, Colan SD, Williams RV, Blaufox A, Li JS, Margossian R, Mital S, Russell J, Rhodes J. A cross-sectional study of exercise performance during the first 2 decades of life after the Fontan operation. J Am Coll Cardiol. 2008;52:99–107. doi: 10.1016/j.jacc.2008.02.081. [DOI] [PubMed] [Google Scholar]
- 19.McCrindle BW, Williams RV, Mital S, Clark BJ, Russell JL, Klein G, Eisenmann JC. Physical activity levels in children and adolescents are reduced after the Fontan procedure, independent of exercise capacity, and are associated with lower perceived general health. Arch Dis Child. 2007;92:509–514. doi: 10.1136/adc.2006.105239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Larsson ES, Eriksson BO, Sixt R. Decreased lung function and exercise capacity in Fontan patients. A long-term follow-up. Scand Cardiovasc J. 2003;37:58–63. doi: 10.1080/14017430310007045. [DOI] [PubMed] [Google Scholar]
- 21.Singh TP, Curran TJ, Rhodes J. Cardiac rehabilitation improves heart rate recovery following peak exercise in children with repaired congenital heart disease. Pediatr Cardiol. 2007;28:276–279. doi: 10.1007/s00246-006-0114-0. [DOI] [PubMed] [Google Scholar]
- 22.Brassard P, Poirier P, Martin J, Noel M, Nadreau E, Houde C, Cloutier A, Perron J, Jobin J. Impact of exercise training on muscle function and ergoreflex in Fontan patients: a pilot study. Int J Cardiol. 2006;107:85–94. doi: 10.1016/j.ijcard.2005.02.038. [DOI] [PubMed] [Google Scholar]
- 23.Giardini A, Balducci A, Specchia S, Gargiulo G, Bonvicini M, Picchio FM. Effect of sildenafil on haemodynamic response to exercise and exercise capacity in Fontan patients. Eur Heart J. 2008;29:1681–1687. doi: 10.1093/eurheartj/ehn215. [DOI] [PubMed] [Google Scholar]
- 24.Mahle WT, Wernovsky G, Bridges ND, Linton AB, Paridon SM. Impact of early ventricular unloading on exercise performance in preadolescents with single ventricle Fontan physiology. J Am Coll Cardiol. 1999;34:1637–1643. doi: 10.1016/s0735-1097(99)00392-7. [DOI] [PubMed] [Google Scholar]
- 25.Meadows J, Lang P, Marx G, Rhodes J. Fontan fenestration closure has no acute effect on exercise capacity but improves ventilatory response to exercise. J Am Coll Cardiol. 2008;52:108–113. doi: 10.1016/j.jacc.2007.12.063. [DOI] [PubMed] [Google Scholar]
- 26.Milanesi O, Stellin G, Colan SD, Facchin P, Crepaz R, Biffanti R, Zacchello F. Systolic and diastolic performance late after the Fontan procedure for a single ventricle and comparison of those undergoing operation at <12 months of age and at >12 months of age. Am J Cardiol. 2002;89:276–280. doi: 10.1016/s0002-9149(01)02227-5. [DOI] [PubMed] [Google Scholar]
- 27.Cheung YF, Penny DJ, Redington AN. Serial assessment of left ventricular diastolic function after Fontan procedure. Heart. 2000;83:420–424. doi: 10.1136/heart.83.4.420. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.