Abstract
Background
Traditional research approaches frequently fail to yield representative numbers of people of color in research. Community-based participatory research (CBPR) may be an important strategy for partnering with and reaching populations who bear a greater burden of illness but have been historically difficult to engage. A Community Action Board of 20 East Harlem residents, leaders and advocates used CBPR to compare the effectiveness of different strategies in recruiting and enrolling adults with prediabetes into a peer-led diabetes prevention intervention.
Methods
The Board created five different recruitment strategies: recruiting through clinicians, at large public events like farmers markets, organizing special local recruitment events, recruiting at local organizations, and a partner-led approach in which community partners developed and managed the recruitment efforts at their sites.
Results
In 3 months, 555 local adults were approached; 249 were appropriate candidates for further evaluation (overweight, nonpregnant, East Harlem residents without known diabetes); 179 consented and returned fasting for 1/2 day of prediabetes testing; and 99 had prediabetes and enrolled in a pilot randomized trial. The partner-led approach was most successful, recruiting 68% of people enrolled. This was also the most efficient strategy; 34% of those approached through partners were ultimately enrolled, versus 0%–17% through the other four strategies. Participants were predominantly low-income, uninsured, undereducated Spanish-speaking women.
Conclusions
This CBPR approach highlights the value of a partner-led recruitment to identify, reach out and motivate a vulnerable population into research, using techniques that may be unfamiliar to researchers, but are nevertheless rigorous and effective.
Populations who bear the greatest burden from chronic illnesses have historically been the least represented and most difficult to engage in research.1–3 The good intentions of researchers and their desire to mitigate the health disparities that disproportionately affect people of color have not been enough to garner support and collaboration in activities designed to seek solutions.
Diabetes is escalating across the U.S.4 Lifestyle change is the most effective strategy to mitigate its rise and has been shown to eliminate racial and ethnic disparities in diabetes incidence.5–8 Unfortunately, interventions have not been sustained even at the very institutions which demonstrated their efficacy. Failing to translate such research into routine practice is particularly problematic for the minority communities hardest hit by diabetes and its devastating consequences.
Developing practical, sustainable, programs that prevent or delay diabetes will require substantial participation of people of color in research. The barriers to their participation include distrust of researchers and research, fear among undocumented immigrants that participation might lead to deportation, and beliefs about health and illness that may cause some individuals to question the value of research.9 In addition, people from minority groups may not be well informed of, or appropriately invited to enroll in research programs.10,11 Lack of participation may also be fueled by the transient nature of research. Successful interventions often disappear with cessation of funding used to document their effectiveness. As a result, people of color may view researchers as interested primarily in data collection to advance their careers, in portraying their communities in an unfavorable light rather than to address community health problems, and in lacking commitment to give back to the community.2
CBPR is an approach that may address the barriers for partnering with and reaching populations who bear a greater burden of illness but have been historically difficult to engage.12 The East Harlem Partnership for Diabetes Prevention, a community–academic partnership, employed CBPR to design and implement a pilot intervention to reduce diabetes among adults in East Harlem. Also known as El Barrio, East Harlem, is the northeast corner of Manhattan. Her residents, 50% of whom are Latino and 40% black, are predominantly low-income, have among the highest obesity and diabetes prevalence, and the highest diabetes mortality rate in NYC.13–15
The Partnership’s Community Action Board, consisting of 20 local residents, activists, and leaders (15 of whom live in East Harlem), formed in 2005 to write a grant to address health disparities. The Partnership (of community and academic partners), conducted community assessments, chose to focus on diabetes, narrowed the focus to prevention, and built a pilot diabetes prevention intervention. As part of the trial, the Board chose to develop and test the effectiveness of five different community-led recruitment strategies to attract local residents, rigorously test them for prediabetes, and if eligible, enroll them into a community-based, peer-led, diabetes prevention RCT. This article describes the effectiveness of these recruitment and enrollment strategies.
Methods
In keeping with CBPR principles, Board members chose all strategies, codeveloped the intervention and its evaluation, and directed the researchers to provide the tools, support, expertise and staffing necessary to meet study goals.16 The study had five phases. First, the Partnership needed to find people with prediabetes range glucoses. Partners identified adults who were overweight (BMI ≥ 25) and obtained informed consent so these individuals could return fasting to determine if they had prediabetes. Returning individuals underwent 1/2 day of testing, including an oral glucose tolerance test and a survey. Eligible people (with prediabetes) had fasting finger-stick glucoses of 100–125 mg/dl or postprandial glucoses of 140–199 mg/dl.17 This group also had hemoglobin A1c (average glucose), lipids, blood pressure and waist circumference measured. The Board, interested in maximizing the information gained from the study, asked participants to bank an additional tube of blood for future studies about prediabetes. Basic scientists interested in accessing these samples would need to formally present their ideas to the Board, who would review and approve or deny the requests. People with prediabetes were randomized to intervention, versus delayed intervention in 1 year.
The Partnership accomplished most if its work through subcommittees. The Board’s Intervention Subcommittee developed an 8 session peer-led program, tailored from a Chronic Disease Self-Management Program, to focus on lifestyle change.18 The goal was 5%–7% weight loss, the amount shown to prevent or delay diabetes in large randomized trials.5–8,19 Classes were offered in English or Spanish at community locations such as churches and senior centers. The Latino Education Subcommittee independently developed or reviewed all study materials and the intervention to ensure they were linguistically and culturally appropriate for the Latinos from the Caribbean, and from North, Central, and South America who live in East Harlem.
The Community Engagement Subcommittee was charged with developing a sensitive, culturally appropriate, noncoercive recruitment and enrollment process. The goals were to create an atmosphere of inclusion and a feeling of importance from taking part, address common barriers to enrolling minority people in research, provide education about prediabetes, and explain the results of the screening. Based on literature review and local knowledge and experiences, the subcommittee developed a Spanish/English training manual and offered a 2-day, hands-on training for all staff and community representatives participating in the project.
Training included information about maintaining confidentiality, mock interviews and suggestions for addressing participants’ resistance, including fear of experimentation, mistrust of the medical system, claiming being too busy, and misunderstanding the research protocol.20–25 Staff provided verbal and written assurance that the research team would use no experimental drugs, that personal health data would be kept confidential and stressed that the participants’ primary clinician, if applicable, would remain in charge of their care. Leaders held weekly meetings to discuss recruitment progress, highlight successful techniques, and brainstorm ways to handle difficult situations that had arisen. All people screened received $50 gift certificates to local stores, study gifts such as tee shirts, pens, and a healthy box lunch. The Partnership sponsored numerous screening events, including on weekends, at various community locations.
The Community Engagement Subcommittee also developed five different strategies to recruit and enroll participants in the diabetes prevention trial. The first was clinician referral, educating local clinicians about prediabetes. The Clinician Subcommittee created a toolkit, including a laminated pocket reference, information about prediabetes and the study, and referral cards so clinicians could easily refer patients. They disseminated the kit to all internal medicine clinicians (physicians and nurse practitioners) practicing in East Harlem and followed up with all through phone calls, visits and educational sessions. The second was holding Board-sponsored recruitment special events, such as —Stop Diabetes Day, advertised in local newspapers, flyers, e-mail blasts and at local businesses and housing developments. These included live music, dancing, healthy foods and giveaways specifically tailored to identifying potential enrollees. The third approach was presenting information about prediabetes and diabetes prevention to local community-based organizations (CBO’s) and garnering their support in approaching their clients about the study. Fourth, Partners recruited at public events such as health fairs, street fairs and farmer’s markets. Partners set up tables with banners, giveaways and community members, who were greeters, encouraged their neighbors to learn about the project. Finally, the Subcommittee developed a community partner-led recruitment strategy. Community advocates spearheaded these efforts and voiced their needs to make recruitment work at their organizations. They explained and championed the study to their own constituents and invited researchers into the process once people understood the study and showed interest in taking part. In this process, they also told the research staff what would be needed to make recruitment work, including appropriate timing of events, staffing, refreshments, incentives, and taught research staff how to interact with clients.
Study personnel were trained to collect data about the number of people approached through each strategy, the number who consented and returned for prediabetes testing, and the number who had prediabetes and were enrolled in the trial. Each person would report to a welcome desk, where Partners or staff captured the data on the number of people who were approached and who declined further participation before they could be screened for eligibility. At that point, staff used a computerized data management system to collect data on the flow of each person through the study. All people approached for the study received a gift after this information was obtained. The study analyst used chi-square statistics to determine the most effective enrollment strategy and differences between those enrolled and the overall East Harlem population.
RESULTS
Between April and July 2007, Partners implemented the 5 recruitment strategies to identify and enroll community residents with prediabetes. This included mailing the clinician education and study referral toolkit and following up with all 295 general adult medical clinicians in East Harlem: 118 hospital or clinic-based providers, 143 residents, 8 nurse practitioners, and 26 private local physicians.
Partners approached 555 people through the five strategies, of whom 249 (45%) were appropriate candidates to be screened for prediabetes and the study (adults ≥18 years, East Harlem residents, BMI ≥25, English or Spanish Speaking, not pregnant or on hypoglycemic medications). The other 305 people were ineligible (281) or declined to take part (25). The 249 who were candidates signed an IRB-approved consent to return fasting for prediabetes testing, and most (178/249, or 71%), did return for prediabetes testing. Of these 178 tested, 99 (56%) had prediabetes and were enrolled in project HEED, Help Educate to Eliminate Diabetes. No person with prediabetes range glucoses refused enrollment.
Three aspects of the success of recruitment efforts were evaluated: volume (number of people approached), efficiency (number enrolled of those approached) and representativeness of the community they came from (Table 1).
Table 1.
Recruitment and Enrollment Results
| # approached | # Consented and tested for prediabetes | % Screened of Approached | # enrolled | % enrolled of approached | |
|---|---|---|---|---|---|
| Total | 555 | 178 | 32 | 99 | 18 |
| Strategy: | |||||
| Clinician referral | 0 | 0 | 0 | 0 | 0 |
| Special events | 46 | 9 | 20 | 8 | 17 |
| Community orgs | 106 | 17 | 16 | 10 | 9 |
| Public events | 201 | 27 | 13 | 13 | 6 |
| Partner-led | 201 | 125 | 62 | 68 | 34 |
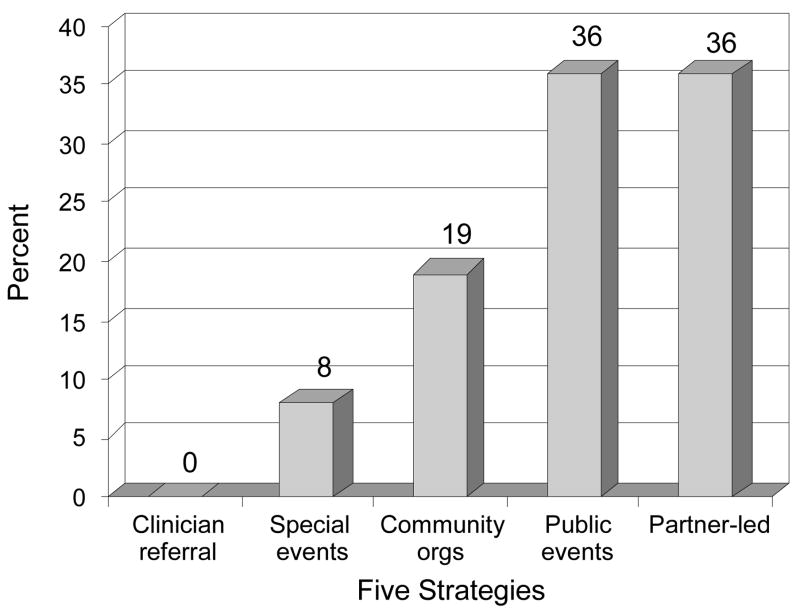
In terms of volume, Partners approached 36% of people via community partner-led approaches, 36% via public events such as health fairs and 19% through CBO’s (Figure 1). Only 8% were approached through specially produced events. Clinicians referred no participants to the study. Partners enrolled more participants through the partner-led strategy (implemented at one family service agency and two churches) than any other approach. Fully 68% (68/99) came through partner-led efforts, whereas between 0% and 13% enrolled came through the other four strategies (p<0.01).
Figure 1.
Adults approached through the Five Strategies (n=555)
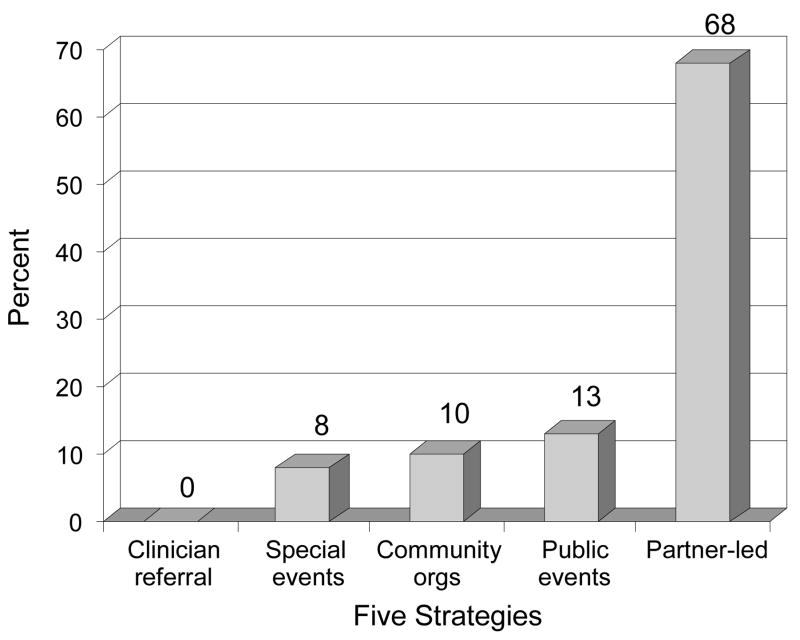
Partner-led strategies were the most efficient form of recruiting people who were ultimately eligible and enrolled (Figure 2). Nearly 2/3 of those approached using this strategy returned fasting for screening, versus 20% or less for the other four approaches. And, fully 34% of those approached through partner-led strategies were eligible and enrolled, versus 0%–17% using any of the other four strategies (p<0.0001).
Figure 2.
Adults enrolled through the Five Strategies (n=99)
Regarding the representativeness of those enrolled, table 2 reveals that the population enrolled was generally low-income, uninsured, undereducated, unemployed and non–English speaking. Enrollees were 89% Latino, 9% black, 1% Asian, and 1% Native American, and 25% were food insufficient (skip meals or do not eat enough because of money). Only 11% reported their health as very good or excellent, and 50% reported depressive symptoms. Compared to the overall East Harlem population, the enrolled population was significantly more female, Latina, unemployed, uninsured, unemployed, obese, and had poorer self-reported health, although they had similar education attainment and yearly income.
Table 2.
Characteristics of Enrolled Participants and the East Harlem Population
| Enrolled (n=99) | East Harlem residents (n=108,000) | p | |
|---|---|---|---|
| Age (M, SD) | 48 (16.5) | NA | |
| Women (%) | 85 | 53 | <0.0001 |
| African American (%) | 9 | 33 | <0.0001 |
| Latino (%) | 89 | 55 | <0.0001 |
| Mexican | 54 | ||
| Puerto Rican | 24 | ||
| Ecuadorian | 11 | ||
| Dominican | 9 | ||
| Other | 2 | ||
| Spanish speaking only (%) | 77 | NA | |
| Education (%) | |||
| Did not complete junior high school | 25 | 21 | 0.3226 |
| Did not complete high school | 58 | 56 | 0.7626 |
| Not working (%) | 70 | 52 | 0.0004 |
| Yearly household income <$15,000 (%) | 45 | 38 | 0.1466 |
| Uninsured (%) | 49 | 11 | <0.0001 |
| Food insufficient (%) | 25 | NA | |
| Self-rated health as fair or poor | 68 | 30 | <0.0001 |
| BMI (%) | 0.0264 | ||
| Overweight (BMI 25.0 to 29.9) | 38 | 31 | |
| Obese (BMI ≥30) | 62 | 31 |
Discussion
Using a CBPR approach, partners evaluated the effectiveness of different recruitment and enrollment strategies. This was a demanding recruitment. Participants were asked to come fasting, drink an oral glucose solution, stay for nearly 1/2 day of testing and, have repeated finger-sticks and a blood draw. Yet in just 3 months, Partners recruited and enrolled 99 people from a vulnerable cohort that many would consider quite challenging to reach and engage in research. Clinician referrals, a commonly used recruitment strategy,32 yielded no participants. In contrast, a community partner-driven strategy approached, screened and enrolled the largest proportion of participants in this trial.
While partner-based strategies resulted in a high volume of enrolled people in an efficient manner and in a relatively short time, this population was not truly representative of East Harlem. Most participants are Latina, as the first organizations the Board partnered with served mainly this group. The planned pilot sample size was reached so quickly working with these organizations that the Board group did not go further. In addition, the Board aimed to engage people often under-represented in research, including non–English speaking, low-income, uninsured, undereducated people and sought out organizations with connections to these groups. As a measure of this success, these individuals may have been over represented in the study. Many approaches have been cited as effective in recruiting and retaining people of color in research, including the use of culturally tailored, community-based approaches. These include collaborating with community partners and community boards to develop recruitment materials, conduct outreach, build trust and rapport, include flexibility in schedules, and working with gatekeepers—individuals trusted and sought after for advice by residents.1–3,20,26–36 Yet, Partners found no references to researchers relinquishing control of community-based recruitment. For the current study, allowing community partners to lead the recruitment efforts facilitated identification of potential subjects who are ultimately both eligible AND enrolled in an intervention with sufficient relevance that community members were enthusiastic, rather than reluctant participants.
In analyzing these data during a Board retreat, community leaders attributed this success to the enthusiastic commitment of both community and academic partners to each other and to the research. On one hand, this required a tight timeline and rigorous methods. On the other hand, this demanded that the project resonate with and provide direct benefit to the community. Community partners understood and advocated for local needs and approaches and insisted clients’ needs be met as a condition of their participation. Their longstanding trusting relationships and history of service likely broke down barriers to participation and engendered trust in the project via their dual role as research partners and advocates. The Partnership developed an evidence-based intervention the community actually wanted, and that was created for and by community members who know them well.
The road was not always smooth. For example, outreach workers at one partner site became frustrated that researchers were too rigid and were not fully including their recommendations in recruitment efforts. Instead of leaving the partnership, their relationship with researchers prompted them to negotiate a way to restructure the protocol, which did not compromise research integrity. Partnering with organizations that work at a grass-roots level may be optimal when recruiting in communities of color. Lessons learned will inform next steps, as Partners begin a larger randomized trial to prevent or delay diabetes. The Board has committed to continuing to create alliances that facilitate this approach.
Success must be balanced with limitations. This was a small study at relatively few sites in one urban community. Furthermore, it would not have been possible to randomize people to the five different strategies, and this may have led to selection bias. People more amenable to research may have been more amenable to joining or receiving services from organizations that have strong, trusted leaders, i.e., those who ran partner-led recruitment for the pilot. These sites may be more cohesive, and include people who are “joiners” by nature.
However, there may be similar pitfalls for those recruited through highly standardized clinical trials. For example, the Diabetes Prevention Program required people to come to several visits and keep detailed food diaries before enrolling, which may select for more literate people with better support to enable such intensive participation, and still be selecting for more motivated individuals.5 Thus, CBPR may motivate populations that are not drawn to more clinically based programs, but are still motivated to take action to improve their health. Future research should determine if this approach will be effective with more diverse populations and in more diverse settings. Nevertheless, this approach holds great promise for recruiting vulnerable and hard to reach populations. The team aims to continue recognizing and directly addressing the tensions between community and academic priorities that, instead of becoming barriers to working constructively, serve as critical elements in effective recruitment, and the glue that holds partnerships together.
Acknowledgments
We thank all members of the Community Action Board for their immense contributions, the community partners and organizations who work with us, and Crispin Goytia, Carlton Bailey, Anika Martin, Carlo Canepa, Ken Fernandez, Donna Bonn, Jose Moreno, and Judit Dieguez for their outreach and recruitment efforts.
The work was supported by grant number 5R24MD001691-03 from The National Center on Minority Health and Health Disparities and the Diabetes Prevention and Control Program of the New York State Department of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Carol R. Horowitz, Departments of Health Policy and Medicine, Mount Sinai School of Medicine, New York, New York.
Barbara L. Brenner, Community and Preventive Medicine, Mount Sinai School of Medicine, New York, New York.
Susanne Lachapelle, Little Sisters of the Assumption Family Health Service, Inc, New York, New York.
Duna A. Amara, Department of Pediatrics, Cornell University Medical College, New York, New York.
Guedy Arniella, Department of Community Outreach and Health Education, North General Hospital, New York, New York.
References
- 1.Levkoff S, Sanchez H. Lessons learned about minority recruitment and retention from the Centers on Minority Aging and Health Promotion. Gerontologist. 2003;43:18–26. doi: 10.1093/geront/43.1.18. [DOI] [PubMed] [Google Scholar]
- 2.Yancey AK, Ortega AN, Kumanyika SK. Effective recruitment and retention of minority research participants. Annu Rev Public Health. 2006;27:1–28. doi: 10.1146/annurev.publhealth.27.021405.102113. [DOI] [PubMed] [Google Scholar]
- 3.Dancy BL, Wilbur JE, Talashek M, Bonner G, Barnes-Boyd C. Community-based research: barriers to recruitment of African Americans. Nurs Outlook. 2004;52:234–40. doi: 10.1016/j.outlook.2004.04.012. [DOI] [PubMed] [Google Scholar]
- 4.Cowie CC, Rust KF, Byrd-Holt DD, Eberhardt MS, Flegal KM, Engelgau MM, Saydah S, Williams DE, Geiss LS. Prevalence of diabetes and impaired fasting glucose in adults in the U.S. population: National Health and Nutrition Survey 1999–2002. Diabetes Care. 2006;29:1263–1268. doi: 10.2337/dc06-0062. [DOI] [PubMed] [Google Scholar]
- 5.The Diabetes Prevention Program Research Group. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. The New England Journal of Medicine. 2001;344:1343–1350. doi: 10.1056/NEJM200105033441801. [DOI] [PubMed] [Google Scholar]
- 6.Hamman RF, Wing RR, Edelstein SL, Lackin JM, Bray GA, Delhanty L, Hoskin M, Kriska AM, Mayer-Davis EJ, Pi-sunyer X, Regensteiner J, Venditti B, Wylie-Rosett J. Effect of weight loss with lifestyle intervention on risk of diabetes. Diabetes Care. 2006;29:2102–2107. doi: 10.2337/dc06-0560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Franz MJ. The evidence is in: lifestyle interventions can prevent diabetes. American Journal of Lifestyle Medicine. 2007;1:113–121. [Google Scholar]
- 8.Pan XR, Li GW, Hu YH, Wang JX, Yang WY, An ZX, Hu ZX, Lin J, Xiao JZ, Cao HB, Liu PA, Jiang XG, Jiang YY, Wang JP, Zheng H, Zhang H, Bennett PH, Howard BV. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance: the Da Qing IGT and Diabetes Study. Diabetes Care. 1997;20:537–544. doi: 10.2337/diacare.20.4.537. [DOI] [PubMed] [Google Scholar]
- 9.Shavers VL, Lynch CF, Burmeister LF. Racial differences in factors that influence the willingness to participate in medical research studies. Annals of Epidemiology. 2002;12:248–256. doi: 10.1016/s1047-2797(01)00265-4. [DOI] [PubMed] [Google Scholar]
- 10.Sullivan PS, McNaghten AD, Begley E, Huchinson A, Cargill VA. Enrollment of racial/ethnic minorities and women with HIV in clinical research studies of HIV medicines. J Natl Med Assoc. 2007;99(3):242–50. [PMC free article] [PubMed] [Google Scholar]
- 11.Corbie-Smith G, Thomas SB, St George DMM. Distrust, race and research. Arch Intern Med. 2002;162:2458–2463. doi: 10.1001/archinte.162.21.2458. [DOI] [PubMed] [Google Scholar]
- 12.Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: Assessing partnership approaches to improve public health. Annual Review of Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- 13.Karpati A, Lu X, Mostashari F, Thorpe L, Frieden TR. The Health of East Harlem. New York City Community Health Profiles. 2003;1:1–12. [Google Scholar]
- 14.U.S. Census Bureau. Census 2000 Summary File 1 Census of Population and Housing. 2000 September; [Google Scholar]
- 15.United Hospital Fund Staff. New York City Community Health Atlas, 2002. New York: United Hospital Fund; 2002. [Google Scholar]
- 16.Horowitz C, Robinson M, Seifer S. Community-Based Participatory Research’s Journey From Margins to Mainstream: Are Researchers Prepared? Circulation. 2009;119:2633–2642. doi: 10.1161/CIRCULATIONAHA.107.729863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nathan DM, Davidson MB, DeFronzo RA, Heine RJ, Henry RR. Impaired fasting glucose and impaired glucose tolerance-implications for care. Diabetes Care. 2007;30:753–759. doi: 10.2337/dc07-9920. [DOI] [PubMed] [Google Scholar]
- 18.Lorig KR, Ritter P, Stewart AL, et al. Chronic disease self-management program: 2-year health status and health care utilization outcomes. Med Care. 2001 Nov;39(11):1217–23. doi: 10.1097/00005650-200111000-00008. [DOI] [PubMed] [Google Scholar]
- 19.American Diabetes Association. Nutrition recommendation and Interventions for Diabetes: A Position statement of the American Diabetes Association. Diabetes Care. 2007;30:s48–s65. doi: 10.2337/dc07-S048. [DOI] [PubMed] [Google Scholar]
- 20.Sisk JE, Horowitz CR, Wang JJ, Hebert PL, McLaughlin MA, Tuzzio L. The success of recruiting minorities, women, and elderly into a randomized controlled effectiveness trial. Mt Sinai Journal of Medicine. 2008;75:37–43. doi: 10.1002/msj.20014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Corbie-Smith G, Thomas S, Williams M, Moody-Ayers S. Attitudes and beliefs of African-Americans toward participation in medical research. J Gen Intern Med. 1999;14:537–546. doi: 10.1046/j.1525-1497.1999.07048.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gorelick PB, Harris Y, Burnett M, Bonecutter FJ. The recruitment triangle: reasons why African Americans enroll, refuse to enroll, or voluntarily withdraw from a clinical trial: an interim report from the African-American antiplatelet stroke prevention study. J Natl Med Assoc. 1998;90:141–145. [PMC free article] [PubMed] [Google Scholar]
- 23.Roberson NL. Clinical trial participation: viewpoints from racial/ethnic groups. Cancer. 1994;74 (suppl 9):2687–2691. doi: 10.1002/1097-0142(19941101)74:9+<2687::aid-cncr2820741817>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 24.Shavers-Hornaday VL, Lynch CF, Burmeister LF, Torner JC. Why are African Americans under-represented in medical research studies? Impediments to participation Ethn Health. 1997;2:31–45. doi: 10.1080/13557858.1997.9961813. [DOI] [PubMed] [Google Scholar]
- 25.Swanson GM, Ward AJ. Recruiting minorities into clinical trials: toward a participant-friendly system. J Natl Cancer Inst. 1995;87:1747–1759. doi: 10.1093/jnci/87.23.1747. [DOI] [PubMed] [Google Scholar]
- 26.Ashing-Giwa KT, Padilla GV, Tejero JS, Kim J. Breast cancer survivorship in a multiethnic sample: challenges in recruitment and measurement. Cancer. 2004;101:450–65. doi: 10.1002/cncr.20370. [DOI] [PubMed] [Google Scholar]
- 27.Corbie-Smith G, Ammerman AS, Katz ML, St George DM, Bluementhal C, Washington C, Weathers B, Keyserlinig TC, Switzer B. Trust, benefit, satisfaction, and burden: a randomized controlled trial to reduce cancer risk through African-American churches. J Gen Intern Med. 2003;18:531–41. doi: 10.1046/j.1525-1497.2003.21061.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wyatt SB, Diekelmann N, Henderson F, Andrew ME, Billingsley G, Felder SH, Fuqua S, Jackson PB. A community-driven model of research participation: the Jackson Heart Study Participant Recruitment and Retention Study. Ethn Dis. 2003;13:438–55. [PubMed] [Google Scholar]
- 29.Corbie-Smith G, Williams IC, Blumenthal C, Dorrance J, Estroff SE, Henderson G. Relationships and communication in minority participation in research: multidimensional and multidirectional. J Natl Med Assoc. 2007;99:489–98. [PMC free article] [PubMed] [Google Scholar]
- 30.Adams A, Miller-Korth N, Brown D. Learning to work together: developing academic and community research partnerships. WMJ. 2004;103:15–9. [PubMed] [Google Scholar]
- 31.Saunders SD, Greaney ML, Lees FD, Clark PH. Achieving recruitment goals through community partnerships: The SENIOR Project. Fam Community Health. 2003;26:194–202. doi: 10.1097/00003727-200307000-00004. [DOI] [PubMed] [Google Scholar]
- 32.Wisdom K, Neighbors K, Williams VH, Havstad SL, Tilley BC. Recruitment of African Americans with Type 2 diabetes to a randomized controlled trial using three sources. Ethnicity and Health. 2002;7:267–278. doi: 10.1080/1355785022000060727. [DOI] [PubMed] [Google Scholar]
- 33.Burns D, Soward AC, Skelly AH, Leeman J, Carlson J. Effective recruitment and retention strategies for older members of rural minorities. The Diabetes Educator. 2008;34:1045–1052. doi: 10.1177/0145721708325764. [DOI] [PubMed] [Google Scholar]
- 34.Merriam PA, Tellez TL, Rosal MC, et al. Methodology of a diabetes prevention translation research project utilizing a community–academic partnership for implementation in an underserved Latino community. BMC Medical Research Methodology. 2009;9:20–29. doi: 10.1186/1471-2288-9-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Derose KP, Hawes-Dawson J, Fox SA, Maldonado N, Tatum A, Kington R. Dealing with diversity: Recruiting churches and women for a randomized trial of mammography promotion. Health Education & Behavior. 2000;27:632–648. doi: 10.1177/109019810002700508. [DOI] [PubMed] [Google Scholar]
- 36.Russel KN, Maraj MS, Wilson LR, Shedd-Steele R, Champion VL. Barriers to recruiting urban African American women into research studies in community settings. Applied Nursing Research. 2008;21:90–97. doi: 10.1016/j.apnr.2006.05.001. [DOI] [PubMed] [Google Scholar]