Abstract
ALI (acute lung injury) and its more severe form ARDS (acute respiratory distress syndrome) are inflammatory diseases of the lung characterized by hypoxaemia and diffuse bilateral infiltrates. Disruption of epithelial integrity and injury to endothelium are contributing factors of the development of ALI/ARDS, and alveolar damage is the most pronounced feature of ALI/ARDS. The resulting increase in lung microvascular permeability promotes influx of inflammatory cells to the alveolar spaces. Oedema fluid contains pro-nflammatory mediators and plasma proteins, including Igs (immunoglobulins). Moreover, several reports describe the presence of autoantibodies and immune complexes [anti-IL-8 (interleukin-8) autoantibody/IL-8 complexes] in lung fluids (oedema and bronchoalveolar lavage fluids) from patients with ALI/ARDS. These immune complexes associate with FcγRIIa (Fcγ IIa receptor) in lungs of patients with ARDS. Furthermore, the expression of FcγRIIa is substantially elevated in lungs of these patients. FcγRIIa appears on virtually all myeloid cells, platelets and endothelial cells. It is a low-affinity receptor for IgG that preferentially binds aggregated immunoglobulins and immune complexes. FcγRs regulate phagocytosis and cell-mediated cytotoxicity, and initiate the release of inflammatory mediators. It should be noted that immune complexes formed between either anti-neutrophil autoantibodies and their specific antigens or anti-HLA (human leucocyte antigen) antibodies and target antigens are implicated in the pathogenesis of TRALI (transfusion-related acute lung injury), and importantly, animal studies indicate that FcγRs are essential for these complexes to cause damage to the lungs. Therefore, we hypothesize that FcγRs such as FcγRIIa could contribute to the pathogenesis of ALI/ARDS.
Keywords: acute lung injury, FcγRIIa, IgG receptor, lung, signal transduction
Abbreviations: ALI, acute lung injury; ARDS, acute respiratory distress syndrome; FcγR, Fcγ receptor; IL, interleukin; ITAM, immunoreceptor tyrosine-based activation motif; ITIM, immunoreceptor tyrosine-based inhibitory motif; KC, keratinocyte-derived chemokine; LIX, lipopolysaccharide-induced CXC chemokine; LPS, lipopolysaccharide; MIP-2, macrophage inflammatory protein 2; TLR4, Toll-like receptor 4; TRALI, transfusion-related acute lung injury
ALI (ACUTE LUNG INJURY)/ARDS (ACUTE RESPIRATORY DISTRESS SYNDROME)
ALI and the ARDS were first described in 1967 and represent a severe form of diffuse lung disease. Alternations of lung function in these pathological entities include rapid onset of dyspnoea, hypoxaemia and respiratory failure. The alveolar-capillary barrier becomes disrupted allowing massive influx of oedema fluid and inflammatory cells. The formation of pulmonary oedema is a consequence of both endothelial injury and increased vascular permeability. In accordance with the recommendations of the American–European Consensus Conference Committee (the consensus definition of 1994), patients are classified as having ALI when characteristic changes in lung compliance and residual capacity of the lungs are found. Diagnosis of ALI is given when an individual rapidly (in less than 7 days) develops severe hypoxaemia [a ratio of the partial pressure of arterial oxygen to the fraction of inspired oxygen (PaO2/FiO2) is 300 or less], and the frontal radiograph is abnormal (visible infiltrate). In fact, the presence of diffuse bilateral infiltrates on chest radiograph is indicative of pulmonary oedema in patients with ALI. More severe hypoxaemia (PaO2/FiO2 of 200 or less) warrants diagnosis of ARDS [1–4].
Clinical disorders associated with the progression to ALI/ARDS can be divided into two groups, i.e. diseases directly affecting the lungs such as pneumonia or gastric aspiration and conditions that can indirectly lead to lung injury such as sepsis or severe trauma [1,3]. Significantly, the highest risk of developing ALI/ARDS is attributed to sepsis [1,4]. There are also additional factors that can predispose individuals for development of ALI/ARDS, as for example, alcoholism or polymorphism of certain genes [1,3]. Nevertheless, the disease course is similar between pulmonary and extrapulmonary ALI/ARDS [3].
INCIDENCE OF AND THERAPY FOR ALI/ARDS
The incidence of ALI and ARDS in the United States is 79 cases and 59 cases per 100000 persons per year respectively. Because of lack of effective treatment modalities for ALI/ARDS, the mortality remains at about 40% [1,4].
Therapies available for ALI/ARDS are nonspecific and generally supportive, including mechanical ventilation [1–3]. Since hyperactive inflammation is one well-recognized feature of ALI/ARDS [5,6] (see below), several trials of steroid effectiveness in patients with ALI/ARDS have been conducted. Prolonged treatment with low doses of corticosteroids has been shown to improve both lung function and survival of patients with ALI/ARDS [7]. These findings are consistent with a causal role for the host inflammatory response in the early stages of the disease that ultimately drives activation of the coagulation cascade and inhibition of fibrinolysis. However, therapies to restore homeostasis in the coagulation or fibrinolytic systems are either partially effective or not effective at all and are associated with serious complications [8,9].
PATHOBIOLOGY OF ALI/ARDS
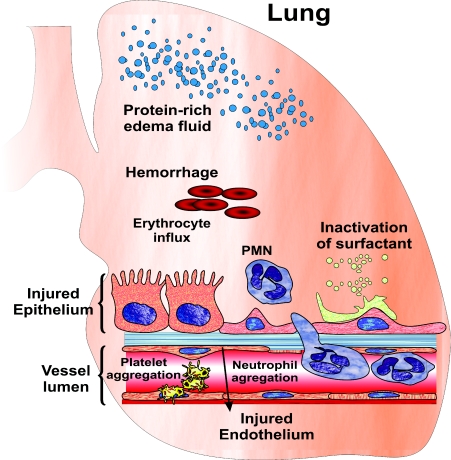
Early stage of ALI/ARDS (exudative phase) is associated with diffuse alveolar damage, neutrophil infiltrate, haemorrhage and the accumulation of a protein-rich pulmonary oedema (Figure 1). Other histopathological changes that are characteristic of the exudative phase include disruption of the epithelial barrier and injury to the capillary endothelium. Some patients with ALI/ARDS progress to a fibroproliferative phase, during which chronic inflammation, fibrosis and neovascularization take place. The final stage of ALI/ARDS, in surviving patients, is the recovery phase that results in a variable degree of restoration of lung function in these patients [1–3]. During the exudative phase, cytokines and other pro-nflammatory molecules initiate, amplify and perpetuate inflammatory responses in the lungs. Increased oxidative stress and the appearance of proteolytic enzymes in the alveolar spaces and interstitium results in a substantial decrease in the surfactant level in the lungs and thereby promotes atelectasis. Elastolytic proteases disrupt the structural framework of the lung. In addition, damage to the epithelial barrier contributes to and exacerbates the alveolar flooding, and also delays recovery by impairing fluid clearance. Finally, capillary thrombosis is most probably brought about by an impairment in the balance between pro-/anti-coagulant and pro-/anti-fibrinolytic proteins [2,3].
Figure 1. Events characterizing early stage of lung damage in patients with ALI/ARDS.
See text for details.
The increase in lung microvascular permeability and the resultant formation of pulmonary oedema are causative of alveolar flooding. Lung fluids from patients with ALI/ARDS contain an abundance of plasma proteins and inflammatory mediators. Studies from several laboratories have described the presence of various autoantibodies in these fluids [10–13]. Our findings indicate that autoantibodies directed against IL-8 (interleukin-8) form immune complexes (anti-IL-8 autoantibody/IL-8 immune complexes) in lung fluids from patients with ALI/ARDS [10,11]. Furthermore, anti-IL-8 autoantibody/IL-8 immune complexes are found in association with FcγRIIa (Fcγ receptor IIa) in pulmonary tissues from these patients [14].
IgG/IMMUNE COMPLEX RECEPTORS (FcγRs)
FcγRs interact with the Fc portion of IgG. To date, three different classes of FcγRs have been identified in humans, i.e. FcγRI, FcγRII and FcγRIII. The FcγRI family contains four different isoforms (Ia, Ib1, Ib2 and Ic), the FcγRII group comprises six proteins (IIa1, IIa2, IIb1, IIb2, IIb3 and IIc), and the FcγRIII group two (IIIa and IIIb). FcγRs consist of two (FcγRII and FcγRIII) or three (FcγRI) N-terminal extracellular immunoglobulin-like domains (ligand binding domains), a transmembrane region and an intracellular tail with a C terminus. FcγRI exhibits high affinity for monomeric IgG, whereas FcγRII and FcγRIII bind immune complexes more efficiently than uncomplexed IgG. The binding affinities of FcγRs are influenced additionally by variations in glycosylation patterns of both the receptors and IgG [15,16].
DIVERSE FUNCTIONS OF FcγRs
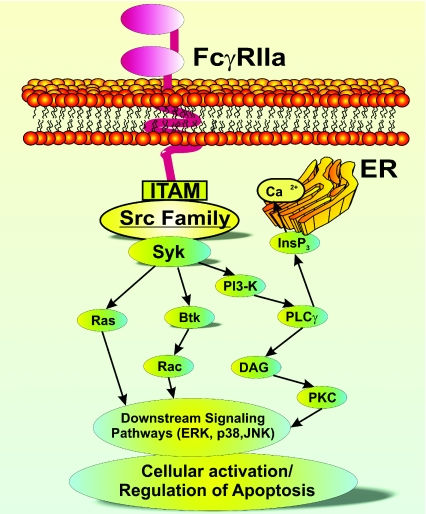
Functionally, FcγRs can be divided into two categories: activating and inhibitory receptors. Activating FcγRs contain ITAM (immunoreceptor tyrosine-based activation motif), while inhibitory FcγRs contain ITIM (immunoreceptor tyrosine-based inhibitory motif). Cross-linking of the former receptors is followed by phosphorylation of tyrosine residues within the ITAM by kinases of the Src [v-src sarcoma (Schmidt-Ruppin A-2) viral oncogene homologue] family. This in turn initiates the FcγR signalling cascade [15,16] (Figure 2).
Figure 2. FcγRIIa signalling cascade.
Activation of the Src kinases leads to the recruitment of a kinase from the Syk family followed by phosphorylation of a series of downstream proteins such as phosphoinositide 3-kinase (PI3-K). Subsequent events include production of PtdIns(3,4,5)P3 and recruitment of Bruton's tyrosine kinase (BtK) and phospholipase Cγ (PLCγ). This leads to increased calcium mobilization and also triggers additional downstream signalling events as activation of the Ras/Raf/MAPK (mitogen-activated protein kinase) pathways [15,16]. DAG, diacylglycerol; ERK, extracellular-signal-regulated kinase; InsP3, Ins(1,4,5)P3; JNK, c-Jun N-terminal kinase; PKC, protein kinase C.
ITAM-bearing FcγRs mediate a pleiotropy of functions in various cell types. These functions include facilitating phagocytosis of diverse pathogens, induction of antibody dependent cytotoxicity, modulation of cell activation, regulation of apoptosis and triggering of the release of pro-inflammatory mediators [15,16].
FcγRIIb, an ITIM-containing receptor, is the only inhibitory FcγR. It is expressed on B cells, mast cells, macrophages, monocytes and neutrophils, and inhibits pro-inflammatory functions of these cells [15,16].
POLYMORPHISM OF FcγRs
Two allelic forms of FcγRIIa have been described in humans: FcγRIIa-R131 and FcγRIIa-H131. FcγRIIa-R131 has an arginine (R) residue, while FcγRIIa-H131 has a histidine (H) residue at position 131. The first allotype binds all human IgG subclasses, particularly IgG2, with low affinity, whereas the second one binds IgG2 and IgG3 with higher affinity. Only one variant of the FcγRIIb gene exists, in which isoleucine (I) at position 232 is replaced by a threonine (T) residue. FcγRIIb-T232 displays enhanced ability to inhibit B-cell receptor signalling compared with FcγRIIb-I232 [15].
FcγRIIIa was shown to have two allelic forms, i.e. FcγRIIIa-V158, which has a valine (V) residue at position 158, and FcγRIIIa-F158 that has a phenylalanine (F) residue in that position. The former allelic variant of FcγRIIIa binds IgG1, IgG3 and IgG4 with higher affinity than the FcγRIIIa-F158 variant. Three alleles of the FcγRIIIb gene are known (NA1, NA2 and SH). The NA1 type mediates phagocytosis of IgG1- and IgG3-opsonized particles more efficiently than the NA2 variant [15].
Polymorphisms in FcγR genes influence susceptibility of individuals to the development of many autoimmune diseases and to acquiring of various infections. Patient responses to treatment with intravenous immunoglobulins and monoclonal antibodies are also affected [15].
HYPOTHESIS: FcγRs IN ALI/ARDS
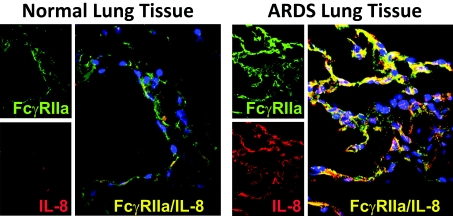
Our hypothesis is that immune and inflammatory responses triggered in the host during the development of ALI/ARDS lead to an increase in expression and functionality of FcγRs, specifically FcγRIIa, in the lung. In support of this hypothesis, we have shown that the level of FcγRIIa is higher in lung tissues from patients with ARDS than in normal lung tissues [14] (Figure 3). Moreover, Hietbrink et al. [17] and Kanters et al. [18] reported that lung fluid neutrophils from three patients with ALI were in a highly primed state characterized by elevated expression of an epitope that the authors later classified as ‘activated’ FcγRIIa.
Figure 3. Expression of FcγRIIa and association of IL-8 in anti-IL-8 autoantibody/IL-8 immune complexes with FcγRIIa in normal lung tissues and tissues from ARDS patients.
Left panels from the top: FcγRIIa (green)/IL-8 (red) x60. Big left panel: co-localization (yellow) of FcγRIIa (green) and IL-8 (red). Nuclei are stained blue. Right panels from the top: FcγRIIa (green)/IL-8 (red) ×60. Big right panel: co-localization (yellow) of FcγRIIa (green) and IL-8 (red). Nuclei are stained blue. Acquisition settings for the images were UV/567/647, and specific parameters for the fluorophores were Cy3 (red) excitation at 567 nm and emission at 600 nm, Alexa 647 (pseudo-colour green) excitation at 647 nm and emission at 700 nm. The sections were evaluated using a PerkinElmer Ultra VIEW LCI confocal imaging system with a Nikon TE2000-S fluorescence microscope and a PlanApo'60 immersion oil objective. Ultra VIEW Imaging Suite software (version 5.5.0.4) was used for image processing.
Additional indirect supportive data for our hypothesis comes from two recently published studies [19,20]. In the first one, Endeman et al. described the presence of the association between the FcγRIIa-R131 genotype and severe sepsis in community-acquired pneumonia [19]. The authors of the second manuscript summarized the results of multiple clinical trials of patients with sepsis, severe sepsis or septic shock who received polyclonal intravenous immunoglobulin therapy. They concluded that there was a survival benefit of this therapy in patients with sepsis [20]. This finding indicates that FcγRs could contribute to the pathogenesis of sepsis (see below), which constitutes the major risk factor for development of ALI/ARDS [1,4].
LIGANDS FOR FcγRs IN PATIENTS WITH ALI/ARDS
A considerable subpopulation of FcγRIIa in lungs of patients with ALI/ARDS associate with anti-IL-8 autoantibody/IL-8 immune complexes [14,21]. At present, it is not known what the pathophysiological significance of this observation is. However, our group reported that anti-IL-8 autoantibody/IL-8 immune complexes in lung fluids from patients with ALI/ARDS are important prognostic indicators for the development and ultimate outcome of ALI/ARDS [10,11,22]. Presence of elevated concentrations of these complexes was associated with poor outcome in patients with ALI/ARDS [11]. We also detected anti-IL-8/IL-8 complexes (at increased levels) in lung fluids of patients at risk of ALI/ARDS who later developed ALI/ARDS. These patients were evaluated immediately after admission to intensive care before influx of neutrophils and lung injury occurred, indicating that the complexes are formed locally in the lung prior to the development of ALI/ARDS [22].
We have purified anti-IL-8 autoantibodies from lung fluids of ALI/ARDS patients. These autoantibodies bind IL-8 with high affinity (about 10−12 M) and inhibit the activity of IL-8 in vitro when experiments are performed using a mixture of IL-8 and autoantibodies (in excess) [10]. However, complexes between these antibodies and IL-8 purified from lung fluids of ALI/ARDS patients display pro-inflammatory activity via FcγRIIa [21,23–25]. Moreover, blocking of FcγRIIa suppresses the biological effects of these complexes in vitro [21,23–25].
Our studies were the first to show that purified anti-IL-8 autoantibody/IL-8 immune complexes trigger chemotaxis of human blood neutrophils, induce neutrophil activation and modulate survival of these cells. Anti-IL-8/IL-8 complexes also have the ability to damage human epithelial cells, promoting cell dysfunction and loss of integrity. Moreover, these complexes display pro-inflammatory activity towards human endothelial cells. Finally, FcγRIIa are the principal receptors that mediate the biological activities of the anti-IL-8/IL-8 complexes in vitro [21,23–25].
Although whether anti-IL-8/IL-8 complexes are causative of disease progression in vivo remains to be established, autoantibodies/immune complexes can trigger the development of ALI/ARDS in humans. Patients with the ‘catastrophic’ variant of the antiphospholipid syndrome can succumb to ALI/ARDS as do patients receiving blood transfusions. TRALI (transfusion-related acute lung injury) is believed to be a result of stimulatory activity of immune complexes formed between either anti-neutrophil autoantibodies and their specific antigens or anti-HLA (human leucocyte antigen) antibodies and target antigens [26–28]. In addition, animal studies indicate that FcγRs are essential for the latter complexes to cause damage to the lungs [29].
ADDITIONAL EVIDENCE: ANIMAL MODELS OF LUNG INJURY AND FcγRs
There is a substantial body of literature describing regulation of lung inflammation in animal models of immune complex-induced lung injury. Most of these models rely on the reverse passive Arthus reaction, a localized alveolitis triggered by deposition of heterologous immune complexes. The local formation of heterologous immune complexes is achieved by intratracheal administration of IgG antibody against a foreign antigen, such as BSA, followed by the intravenous injection of this antigen [30]. We have developed a mouse model of ALI triggered by anti-KC (keratinocyte-derived chemokine) autoantibody/KC immune complexes and concluded that these complexes are injurious for lungs based on our investigations in mice [31]. Murine KC (CXCL1/KC) is a functional homologue of IL-8 [32], so this model provides excellent means for studying the mode of action of immune complexes containing autoantibodies to chemokines [31]. Other murine CXC chemokines that promote neutrophil migration include MIP-2 (macrophage inflammatory protein 2) (CXCL2), LIX (lipopolysaccharide-induced CXC chemokine) (CXCL5) and lungkine (CXCL15) [33–35]. KC, however, shares more common properties with human IL-8 than MIP-2, LIX or lungkine. KC is an early response chemokine and is responsible for the initial influx of neutrophils to the alveolar compartment [36]. Since platelet–neutrophil interactions have been shown to contribute to lung injury in murine models of acid-induced ALI, sepsis-associated ALI and TRALI, and since FcγRIIa is expressed by both platelets and neutrophils, it is very likely that this receptor facilitates neutrophil capture by circulating platelets [15,16,37,38].
Furthermore, mice deficient in all FcγRs or FcγRI are protected from lung injury [30,31,39]. Importantly, the same holds true for mice lacking FcγRIII, a murine homologue of human FcγRIIa [16,30,39].
Perhaps even more relevant are findings of attenuated inflammatory response in the lungs of LPS (lipopolysaccharide)-treated mice or rats in the absence of FcγRs [31,40]. Moreover, studies from our laboratory as well as those of others indicate that there is cross-talk between FcγRs, including FcγRIIa and TLR4 (toll-like receptor 4) in human neutrophils [41] and in mouse models of LPS-induced lung injury [42,43]. Finally, there are reports suggesting a regulatory role of FcγRs in Escherichia coli sepsis and Pseudomonas aeruginosa pneumonia in mice [44,45].
It should be noted that anti-IL-8/IL-8 complexes consist of one IgG and one IL-8 molecule [10] and are capable of triggering complement activation (A. Krupa and A.K. Kurdowska, unpublished work). However, our in vitro experiments are performed in the absence of serum or other sources of complement, and in such conditions, complement activation cannot occur. This is different from the situation in vivo where complement activation plays an important role. It has been demonstrated, for example, that blocking of complement activation protects against lung injury triggered by the administration of heterologous immune complexes. Furthermore, C5a mediates activity of immune complexes by regulating expression of FcγRs [30,39]. Therefore, both complement and the FcγR cascade are likely to be involved in orchestrating the inflammatory events in ALI/ARDS.
TESTING OF THE HYPOTHESIS
The published data supporting our hypothesis is primarily indirect evidence (‘by association’), predominantly from in vitro studies and animal models of ALI. Despite the inquisitory value of this observation, more studies utilizing specimens from patients with ALI/ARDS are certainly needed. Lung tissues from these patients should be rigorously analysed for the presence of different types of FcγRs. The levels and expression patterns of FcγRs should also be evaluated. Our studies, for example, indicate that FcγRIIa is expressed in injured lungs and is present on endothelial cells in patients with ARDS [14,21]. Inflammatory cells in lung fluids of patients with ALI/ARDS should be similarly tested. Moreover, it would be useful to know which proteins from the FcγRIIa-signalling cascade are up- or down-regulated in the lungs of these patients. Whether FcγRIIa is the only or the most abundant FcγR in lungs in ALI/ARDS is at present not known. Because of the limited availability of clinical samples, fluorescence-based methods, such as laser confocal microscopy or fluorescence resonance energy transfer, are preferable.
Studies using well-established animal models of ALI/ARDS and mice transgenic for FcγRIIa would also be very valuable. Such mice have been generated by other investigators [46,47]. When considering a model of ALI/ARDS, one should take into account the complexity of the disease in ALI/ARDS. Therefore, two hit models are probably the most appropriate [48]. Nevertheless, to study the role of FcγRIIa in the pathogenesis of ALI/ARDS, a model of immune-complex-triggered lung injury should be used initially [30,31,39], then, perhaps treatment with LPS could be added to create a two-hit model [31,40]. Contribution of human autoantibodies/immune complexes such as anti-IL-8/IL-8 complexes to the pathogenesis of lung injury could also be studied using FcγR-deficient mice that are transgenic for FcγRIIa. These mice should be treated with the immune complexes formed between IL-8 and fully human anti-IL-8 monoclonal antibodies [49]. To study the role of FcγRIIa in different populations of cells, adaptive transfer experiments could be performed. Cells from mice lacking murine FcγRs and expressing human FcγRIIa could be injected into FcγR-knockout mice [47]. In addition, other common models of ALI/ARDS, including ventilator-induced lung injury and hyperoxia, ought to be evaluated using mice deficient in FcγRs that are transgenic for human FcγRIIa [48]. Moreover, FcγRIIa may be inhibited in the above-described mouse models employing specific FcγRIIa blockers [50–52]. Finally, the role of FcγR signalling could be explored in these models taking advantage of the availability of small inhibitors of signalling proteins and silencing RNAs targeting these proteins [53–55].
CONCLUSIONS
Studies with animal models of ALI/ARDS and FcγRIII (homologue of human FcγRIIa)-deficient mice support our hypothesis [30,31,39,40,43–45]. Our findings of increased levels of FcγRIIa and its association with anti-IL-8/IL-8 immune complexes in lungs of patients with ARDS provide direct evidence of expression of functional FcγRIIa in the lungs of these patients [14,21]. The relevance of these observations is substantiated by the several facts described by us and other researchers. First of all, concentrations of anti-IL-8/IL-8 immune complexes in lung fluids from patients with ALI/ARDS were predictive of disease progression and the eventual outcome of ALI/ARDS [10,11,22]. Secondly, purified complexes exhibit pro-inflammatory activities in vitro [21,23–25]. Thirdly, other autoantibodies have been detected in patients with ALI/ARDS, and also could be correlated with disease activity [12,13]. Finally, autoantibodies/immune complexes at large are known to induce ALI/ARDS in humans [26–28].
At present, involvement of FcγRIIa in the pathophysiology of ALI/ARDS is not understood, but the many basic and clinical studies place this receptor at the ‘heart’ of the inflammatory milieu in the lung. It is certainly conceivable that FcγRIIa could contribute to the pathogenesis of ALI/ARDS. Keeping in mind the association of FcγRIIa polymorphism with the development of sepsis (a major risk factor for ALI/ARDS) in community-acquired pneumonia, one can envision that this receptor could play an important regulatory role during the course of this illness, as evident from animal models of sepsis and pneumonia [19,44,45].
Comprehensive research into the function and molecular mechanisms of FcγRIIa activity could lead to development of novel and more effective therapies for ALI/ARDS. It is important to note that specific inhibitory molecules, i.e. FcγRIIa blockers, have already been tested in animal models of inflammation [50–52]. Signalling proteins from the FcγRIIa cascade could serve as therapeutic targets as well. The progress made in the fields of designing and utilizing small inhibitors of signalling proteins and pulmonary delivery of inhibitory entities makes this possibility very attractive [53–55].
FUNDING
This work was supported by the National Institutes of Health [grant number HLO73245].
References
- 1.Ware L. B., Matthay M. A. The acute respiratory distress syndrome. N. Engl. J. Med. 2000;342:1334–1346. doi: 10.1056/NEJM200005043421806. [DOI] [PubMed] [Google Scholar]
- 2.Ware L. B., Pathophysiology of acute lung injury The acute respiratory distress syndrome. Semin. Respir. Crit. Care Med. 2006;27:337–349. doi: 10.1055/s-2006-948288. [DOI] [PubMed] [Google Scholar]
- 3.Wheeler A. P., Bernard G. R. Acute lung injury and the acute respiratory distress syndrome: a clinical review. Lancet. 2007;369:1553–1565. doi: 10.1016/S0140-6736(07)60604-7. [DOI] [PubMed] [Google Scholar]
- 4.Perl M., Lomas-Neira J., Chung C.-S., Ayala A. Epithelial cell apoptosis and neutrophil recruitment in acute lung injury: a unifying hypothesis?. What we have learned from small interfering RNAs. Mol. Med. 2008;14:465–475. doi: 10.2119/2008-00011.Perl. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meduri G. U., Kohler G., Headly S., Tolley E., Stentz F., Postlethwaite A. Inflammatory cytokines in the BAL of patients with ARDS. Persistent elevation over time predicts poor outcome. Chest. 1995;108:1303–1314. doi: 10.1378/chest.108.5.1303. [DOI] [PubMed] [Google Scholar]
- 6.Goodman R. G., Strieter R. M., Martin D. P., Steinberg K. P., Milberg J. A., Maunder R. J., Kunkel S. L., Walz A., Hudson L. D., Martin T. R. Inflammatory cytokines in patients with persistence of the acute respiratory distress syndrome. Am. J. Respir. Crit. Care Med. 1996;154:602–611. doi: 10.1164/ajrccm.154.3.8810593. [DOI] [PubMed] [Google Scholar]
- 7.Tang B. M. P., Craig J. C., Eslick G. D., Seppelt I., McLean A. S. Use of corticosteroids in acute lung injury and acute respiratory distress syndrome: a systematic review and meta-analysis. Crit. Care Med. 2009;37:1594–1603. doi: 10.1097/CCM.0b013e31819fb507. [DOI] [PubMed] [Google Scholar]
- 8.MacLaren R., Stringer K. A. Emerging role of anticoagulants and fibrinolytics in the treatment of acute respiratory distress syndrome. Pharmacotherapy. 2007;27:860–873. doi: 10.1592/phco.27.6.860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vincent J.-L., Artigas A., Petersen L. C., Meyer C. A multicenter, randomized, double-blind, placebo-controlled, dose-escalation trial assessing safety and efficacy of active site inactivated recombinant factor VIIa in subject with acute lung injury or acute respiratory distress syndrome. Crit. Care Med. 2009;37:1–7. doi: 10.1097/CCM.0b013e31819fff2c. [DOI] [PubMed] [Google Scholar]
- 10.Kurdowska A., Miller E. J., Noble J. M., Baughman R. P., Matthay M. A., Brelsford W. G., Cohen A. B. Anti-IL-8 autoantibodies in alveolar fluid from patients with the adult respiratory distress syndrome. J. Immunol. 1996;157:2699–2706. [PubMed] [Google Scholar]
- 11.Kurdowska A., Noble J. M., Steinberg K. P., Ruzinski J. T., Hudson L. D., Martin T. R. Anti-interleukin-8 autoantibody:interleukin-8 complexes in the acute respiratory distress syndrome. Relationship between the complexes and clinical disease activity. Am. J. Respir. Crit. Care Med. 2001;163:463–468. doi: 10.1164/ajrccm.163.2.2005109. [DOI] [PubMed] [Google Scholar]
- 12.Maneta-Peyret L., Kitsiouli E., Lekka M., Nakos G., Cassagne C. Autoantibodies to lipids in bronchoalveolar lavage fluid of patients with acute respiratory distress syndrome. Crit. Care Med. 2001;29:1–9. doi: 10.1097/00003246-200110000-00017. [DOI] [PubMed] [Google Scholar]
- 13.Thomson L., Christie J., Vadseth C., Lanken P. N., Fu X., Hazen S. L., Ischiropoulos H. Identification of immunoglobulins that recognize 3-nitrotyrosine in patients with acute lung injury after major trauma. Am. J. Respir. Cell. Mol. Biol. 2007;36:152–157. doi: 10.1165/rcmb.2006-0288SM. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Allen T. C., Fudala R., Nash S., Kurdowska A. Anti-interleukin-8 autoantibody:interleukin-8 immune complexes visualized by laser confocal microscopy in injured lung. Co-localization with FcγRIIa in lung tissues from patients with acute respiratory distress syndrome. Arch. Pathol. Lab. Med. 2007;131:452–456. doi: 10.5858/2007-131-452-AAICVB. [DOI] [PubMed] [Google Scholar]
- 15.Ivan E., Colovai A. I. Human Fc receptors: critical targets in the treatment of autoimmune diseases and transplant rejections. Hum. Immunol. 2006;67:479–491. doi: 10.1016/j.humimm.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 16.Nimmerjahn F., Ravetch J. V. Fcγ receptors as regulators of immune responses. Nature. 2008;8:34–47. doi: 10.1038/nri2206. [DOI] [PubMed] [Google Scholar]
- 17.Hietbrink F., Oudijk E.-J., Braams R., Koenderman L., Leenen L. Aberrant regulation of polymorphonuclear phagocyte responsiveness in multitrauma patients. Shock. 2006;26:558–564. doi: 10.1097/01.shk.0000233196.40989.78. [DOI] [PubMed] [Google Scholar]
- 18.Kanters D., ten Hove W., Luijk B., van Aalst C., Schweizer R. C., Lammers J. W., Leufkens H. G., Raaijmakers J. A., Bracke M., Koenderman L. Expression of activated FcγRII discriminates between multiple granulocyte-priming phenotypes in peripheral blood of allergic asthmatic subjects. J. Allergy Clin. Immunol. 2007;120:1073–1081. doi: 10.1016/j.jaci.2007.06.021. [DOI] [PubMed] [Google Scholar]
- 19.Endeman H., Cornips M. C. A., Grutters J. C., van den Bosch J. M., Ruven H. J., van Velzen-Blad H., Rijkers G. T., Biesma D. H. The Fcγ receptor IIA-R/R131 genotype is associated with severe sepsis in community acquired pneumonia. Clin. Vaccine Immunol. 2009;16:1087–1090. doi: 10.1128/CVI.00037-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Turgeon A. F., Hutton B., Fergusson D. A., McIntyre L., Tinmouth A. A., Cameron D. W., Hébert P. C. Meta-analysis: intravenous immunoglobulin in critically ill adult patients with sepsis. Ann. Intern. Med. 2007;146:193–203. doi: 10.7326/0003-4819-146-3-200702060-00009. [DOI] [PubMed] [Google Scholar]
- 21.Krupa A., Fudala R., Stankowska D., Loyd T., Allen T. C., Matthay M. A., Gryczynski Z., Gryczynski I., Mettikolla Y. V., Kurdowska A. K. Anti-chemokine autoantibody:chemokine immune complexes activate endothelial cells via IgG receptors. Am. J. Respir. Cell. Mol. Biol. 2009;41:155–169. doi: 10.1165/rcmb.2008-0183OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kurdowska A., Noble J. M., Grant I. S., Robertson C. R., Haslett C., Donnelly S. C. Anti-interleukin-8 autoantibodies in patients at risk for acute respiratory distress syndrome. Crit. Care Med. 2002;30:2335–2337. doi: 10.1097/00003246-200210000-00024. [DOI] [PubMed] [Google Scholar]
- 23.Krupa A., Kato H., Matthay M. A., Kurdowska A. K. Proinflammatory activity of anti-IL-8 autoantibody:IL-8 complexes in alveolar edema fluid from patients with acute lung injury. Am. J. Physiol. Lung Cell. Mol. Physiol. 2004;286:L1105–L1113. doi: 10.1152/ajplung.00277.2003. [DOI] [PubMed] [Google Scholar]
- 24.Fudala R., Krupa A., Matthay M. A., Allen T. C., Kurdowska A. Anti-IL-8 autoantibody:IL-8 immune complexes suppress spontaneous apoptosis of neutrophils. Am. J. Physiol. Lung Cell Mol. Physiol. 2007;293:L364–L374. doi: 10.1152/ajplung.00179.2006. [DOI] [PubMed] [Google Scholar]
- 25.Stankowska D., Fudala R., Kurdowska A. Mechanism of epithelial injury triggered by anti-IL-8:IL-8 immune complexes. PATS. 2008;5:365–366. [Google Scholar]
- 26.Bucciarelli S., Erkan D., Espinosa G. Catastrophic antiphospholipid syndrome: treatment, prognosis, and the risk of relapse. Clinic. Rev. Allerg. Immunol. 2009;36:80–84.. doi: 10.1007/s12016-008-8107-9. [DOI] [PubMed] [Google Scholar]
- 27.Bux J., Sachs U. J. The pathogenesis of transfusion-related acute lung injury. Br. J. Haematol. 2007;136:788–799. doi: 10.1111/j.1365-2141.2007.06492.x. [DOI] [PubMed] [Google Scholar]
- 28.Triulzi D. J. Transfusion-related acute lung injury: an update. Hematology Am. Soc. Hematol. Educ. Program. 2006;2006:497–501. doi: 10.1182/asheducation-2006.1.497. [DOI] [PubMed] [Google Scholar]
- 29.Looney M. R., Su X., van Ziffle J. A., Lowell C. A., Matthay M. A. Neutrophils and their Fc gamma receptors are essential in a mouse model of transfusionrelated acute lung injury. J. Clin. Invest. 2006;116:1615–1623. doi: 10.1172/JCI27238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gao H., Neff T., Ward P. A. Regulation of lung inflammation in the model of IgG immune-complex injury. Annu. Rev. Pathol. Mech. Dis. 2006;1:215–242. doi: 10.1146/annurev.pathol.1.110304.100155. [DOI] [PubMed] [Google Scholar]
- 31.Krupa A., Walencka M. J., Shrivastava V., Loyd T., Fudala R., Frevert C. W., Martin T. R., Kurdowska A. K. Anti-KC autoantibody:KC complexes cause severe lung inflammation in mice via IgG receptors. Am. J. Respir. Cell Mol. Biol. 2007;37:532–543. doi: 10.1165/rcmb.2006-0395OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bozic C. R., Kolakowski L. F., Jr, Gerard N. P., Garcia-Rodriguez C., von Uexkull-Guldenband C., Conklyn M. J., Breslow R., Showell H. J., Gerard C. Expression and biologic characterization of the murine chemokine KC. J. Immunol. 1995;154:6048–6057. [PubMed] [Google Scholar]
- 33.Rovai L. E., Herschman H. R, Smith J. B. The murine neutrophil-chemoattractant chemokines LIX, KC, and MIP-2 have distinct induction kinetics, tissue distributions, and tissue-specific sensitivities to glucocorticoid regulation in endotoxemia. J. Leukocyte Biol. 1998;64:494–502. doi: 10.1002/jlb.64.4.494. [DOI] [PubMed] [Google Scholar]
- 34.Starckx S., Wuyts A., Opsomer I., Van Coillie E., Proost P., Arnold B., Van Damme J., Opdenakker G. Recombinant mouse granulocyte chemotactic protein-2: production in bacteria, characterization, and systemic effects on leukocytes. J. Interferon Cytokine Res. 2002;22:965–974. doi: 10.1089/10799900260286678. [DOI] [PubMed] [Google Scholar]
- 35.Rossi D. L., Hurst S. D., Xu Y., Wang W., Menon S., Coffman R. L., Zlotnik A. Lungkine, a novel CXC chemokine, specifically expressed by lung bronchoepithelial cells. J. Immunol. 1999;162:5490–5497. [PubMed] [Google Scholar]
- 36.Tsai W. C., Strieter R. M., Wilkowski J. M., Bucknell K. A., Burdick M. D., Lira S. A., Standiford T. J. Lung-specific transgenic expression of KC enhances resistance to Klebsiella pneumoniae in mice. J. Immunol. 1998;161:2435–2440. [PubMed] [Google Scholar]
- 37.Zarbock A., Singbartl K., Ley K. Complete reversal of acid-induced acute lung injury by blocking of platelet-neutrophil aggregation. J. Clin. Invest. 2006;116:3211–3219. doi: 10.1172/JCI29499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hidalgo A., Chang J., Jang J.-E., Peired A. J., Chiang E. J., Frenette P. S. Heterotypic interactions enabled by polarized neutrophil microdomains mediate thromboinflammatory injury. Nat. Med. 2009;15:384–391. doi: 10.1038/nm.1939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Baumann U., Schmidt R. E., Gessner J. E. New insights into the pathophysiology and in vivo function of IgG Fc receptors through gene deletion studies. Arch. Immunol. Ther. Exp. 2003;51:399–406. [PubMed] [Google Scholar]
- 40.Wu C. L., Lin L. Y., Yeh H. M., Chan M. C., Yang C. H., Hsueh C. M. Delay of LPS-induced acute lung injury resolution by soluble immune complexes is neutrophil dependent. Shock. 2009;32:276–285. doi: 10.1097/SHK.0b013e31819962b2. [DOI] [PubMed] [Google Scholar]
- 41.Fudala R., Stankowska D., Krupa A., Kurdowska A. K. Cooperation between IgG receptors (FcγRIIa) and TLR4 in human neutrophils. FASEB J. 2008;22:710.4. [Google Scholar]
- 42.Krupa A., Fudala R., Stankowska D., Kurdowska A. K. Critical role of IgG receptors (FcγRs) in LPS-induced severe lung inflammation. FASEB J. 2008;22:672.48. [Google Scholar]
- 43.Rittirsch D., Flierl M. A., Day D., Nadeau B. A., Zetoune F. S., Sarma J. V., Werner C. M., Wanner G. A., Simmen H. P., Huber-Lang M. S., Ward P. A. Cross-talk between TLR4 and Fcγ receptor III (CD16) pathways. PLoS Pathog. 2009;5:e1000464. doi: 10.1371/journal.ppat.1000464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pinheiro da Siva F., Aloulou M., Skurnik D., Benhamou M., Andremont A., Velasco I. T., Chiamolera M., Verbeek J. S., Launay P., Monteiro R. C. CD16 promotes Escherichia coli sepsis through an FcRγ inhibitory pathway that prevents phagocytosis and facilitates inflammation. Nat. Med. 2007;13:1368–1374. doi: 10.1038/nm1665. [DOI] [PubMed] [Google Scholar]
- 45.Rhein L. M., Perkins M., Gerard N. P., Gerard C. FcγRIII is protective against Pseudomonas aeruginosa pneumonia. Am. J. Respir. Cell. Mol. Biol. 2008;38:401–406. doi: 10.1165/rcmb.2007-0309OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.McKenzie S. E., Reilly M. P. Heparin-induced thrombocytopenia and other immune thrombocytopenias: lessons from mouse models. Semin. Thromb. Hemostasis. 2004;30:559–568. doi: 10.1055/s-2004-835676. [DOI] [PubMed] [Google Scholar]
- 47.Tsuboi N., Asano K., Lauterbach M., Mayadas T. N. Human neutrophil Fcgamma receptors initiate and play specialized nonredundant roles in antibodymediated inflammatory diseases. Immunity. 2008;28:833–846. doi: 10.1016/j.immuni.2008.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bastarache J. A., Blackwell T. S. Development of animal models for the acute respiratory distress syndrome. Dis. Model. Mech. 2009;2:218–223. doi: 10.1242/dmm.001677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yang X. D., Corvalan J. R., Wang P., Roy C. M., Davis C. G. Fully human anti-interleukin-8 monoclonal antibodies: potential therapeutics for the treatment of inflammatory disease states. J. Leukocyte Biol. 1999;66:401–410. doi: 10.1002/jlb.66.3.401. [DOI] [PubMed] [Google Scholar]
- 50.Shashidharamurthy R., Hennigar R. A., Fuchs S., Palaniswami P., Sherman M., Selvaraj P. Extravasations and emigration of neutrophils to the inflammatory site depend on the interaction of immune-complex with Fcγ receptors and can be effectively blocked by decoy Fcγ receptors. Blood. 2008;111:894–904. doi: 10.1182/blood-2007-04-085944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pietersz G. A., Mottram P. L., van de Velde N. C., Sardjono C. T., Esparon S., Ramsland P A., Moloney G., Baell J. B., McCarthy T. D., Matthews B. R., et al. Inhibition of destructive autoimmune arthritis in FcγRIIa transgenic mice by small chemical entities. Immunol. Cell Biol. 2009;87:3–12. doi: 10.1038/icb.2008.82. [DOI] [PubMed] [Google Scholar]
- 52.Masuda A., Yoshida M., Shiomi H., Morita Y., Kutsumi H., Inokuchi H., Mizuno S., Nakamura A., Takai T., Blumberg R. S., Azuma T. Role of Fc receptors as a therapeutic target. Inflamm. Allergy Drug Targets. 2009;8:80–86. doi: 10.2174/187152809787582525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Grant S. K. Therapeutic protein kinase inhibitors. Cell. Mol. Life Sci. 2009;66:1163–1177. doi: 10.1007/s00018-008-8539-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gaestel M., Kotlyarov A., Kracht M. Targeting innate immunity protein kinase signaling in inflammation. Nat. Rev. Drug Discov. 2009;8:480–499. doi: 10.1038/nrd2829. [DOI] [PubMed] [Google Scholar]
- 55.Lomas-Neira J., Chung C.-S., Ayala A. RNA interference as a potential therapeutic treatment for inflammation associated lung injury. Int. J. Clin. Exp. Med. 2008;1:154–160. [PMC free article] [PubMed] [Google Scholar]