Abstract
Although physicians’ communication style and perceptions affect outcomes, few studies have examined how these perceptions relate to the way physicians communicate with patients. Moreover, while any number of factors may affect the communication process, few studies have analyzed these effects collectively in order to identify the most powerful influences on physician communication and perceptions. Adopting an ecological approach, this investigation examined: (a) the relationships of physicians’ patient-centered communication (informative, supportive, partnership-building) and affect (positive, contentious) on their perceptions of the patient, and (b) the degree to which communication and perceptions were affected by the physicians’ characteristics, patients’ demographic characteristics, physician-patient concordance, and the patient’s communication. Physicians (N = 29) and patients (N = 207) from 10 outpatient settings in the United States participated in the study. From audio-recordings of these visits, coders rated the physicians’ communication and affect as well as the patients’ participation and affect. Doctors were more patient-centered with patients they perceived as better communicators, more satisfied, and more likely to adhere. Physicians displayed more patient-centered communication and more favorably perceived patients who expressed positive affect, were more involved, and who were less contentious. Physicians were more contentious with black patients, whom they also perceived as less effective communicators and less satisfied. Finally, physicians who reported a patient-centered orientation to the doctor-patient relationship also were more patient-centered in their communication. The results suggest that reciprocity and mutual influence have a strong effect on these interactions in that more positive (or negative) communication from one participant leads to similar responses from the other. Physicians’ encounters with black patients revealed communicative difficulties that may lower quality of care for these patients.
Keywords: USA, physician-patient communication, physician perceptions, racial inequalities, patient participation
Introduction
The quality of care a patient receives depends in part on the physician’s communication skills. Physicians who are informative, show support and respect for the patient, and facilitate patient participation in care generally have patients who are more satisfied, more committed to treatment regimens, and who experience better health following the consultation (Henman, Butow, Brown, Boyle & Tattersall, 2002; Jahng, Martin, Golin & DiMatteo, 2005; Kaplan, Greenfield & Ware, Jr., 1989; Ong, de Haes, Hoos & Lammes, 1995; Stewart, Brown, Donner, McWhinney, Oates, Weston et al. 2000; Street, Piziak, Carpentier, Herzog, Hejl, Skinner et al. 1993; Trummer, Mueller, Nowak, Stidl & Pelikan, 2006). Quality of care may also be affected by physicians’ perceptions of patients. For example, physicians’ liking for their patients has been associated with patients’ ratings of satisfaction with care and more positive evaluations of the physician’s behavior (Hall, Epstein, DeCiantis & McNeil, 1993; Hall, Horgan, Stein & Roter, 2002). Moreover, physicians’ communication and perceptions of patients appear to be interconnected. Physicians have provided more information, expressed more empathy, and showed more positive affect toward patients they respected and viewed favorably (Beach, Roter, Wang, Duggan & Cooper, 2006; Levinson & Roter, 1995).
Because physicians’ communication and perceptions are related to outcomes, it is critically important to account for variability in physicians’ behavior as well as understand why different doctors talk and perceive different patients differently. With such an understanding, researchers and educators will be better positioned to effectively examine relationships between communication and outcomes as well as design interventions for improving the quality of health care.
Conceptual Framework: An Ecological Approach
To examine these issues, we adopted an ecological approach (Aita, McIlvain, Backer, McVea & Crabtree, 2005; Street, 2003) that takes into account the interplay of multiple physician, patient, and contextual factors that collectively influence physician-patient interactions. An ecological approach is unique to traditional approaches to the study of communication in medical encounters. For example, some studies take a ‘single factor’ approach by examining the influence of one variable such as gender (Hall & Roter, 1998) or age (Greene, Adelman, Charon & Friedmann, 1989) on physician-patient encounters. However, the influence of any one variable (e.g., ethnicity) may vary depending on the presence of other factors (e.g., the patient’s level of education, the physicians’ communication style). While some studies have examined multiple variables (Cooper, Roter, Johnson, Ford, Steinwachs & Powe, 2003; Siminoff, Graham & Gordon, 2006), little attention has been given to the processes by which these factors may have influence. In contrast, an ecological approach recognizes that within the context of any medical encounter, a number of processes affect the way physicians and patients communicate and perceive one another. In this study, we focus on four sources of potential influence—the physician’s communication style, the patients’ characteristics, physician-patient demographic concordance, and the patient’s communication (see Figure 1).
Figure 1.
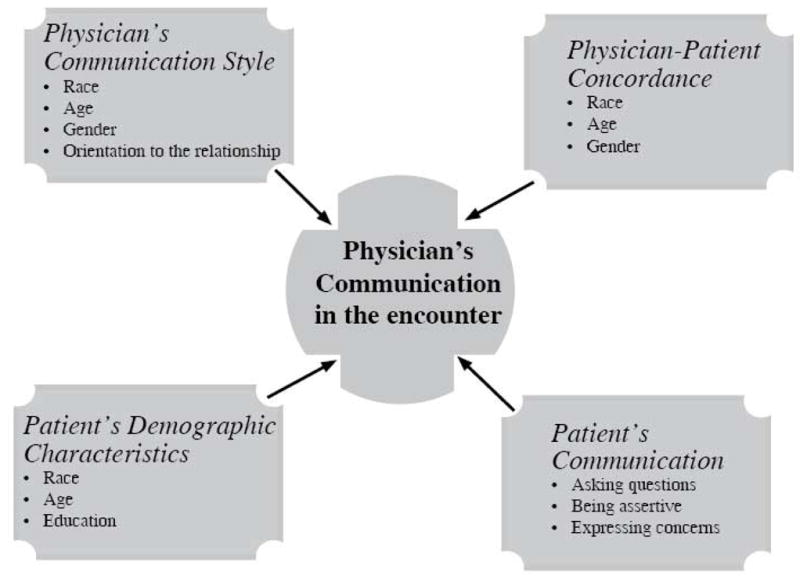
Potential influences on physicians’ communication
First, how a physician communicates with and views a patient may simply depend on the doctor’s style. Some physicians as a matter of routine provide more information, use more partnership-building, are more supportive, and are more willing to talk about psychosocial topics than are other doctors (Roter, Stewart, Putnam, Lipkin, Stiles & Inui, 1997; Street, 1991a; Street, 1992b; Zandbelt, Smets, Oort, Godfried & de Haes, 2006). A physician’s style of communicating with patients may have evolved from repeated experiences with certain kinds of patients, his or her philosophy of care (Krupat, Rosenkranz, Yeager, Barnard, Putnam & Inui, 2000; Levinson & Roter, 1995), or socialization related to gender (Bertakis, Helms, Callahan, Azari & Robbins, 1995; Hall & Roter, 1998), culture (Waitzkin, 1985), and medical training (Bertakis, Callahan, Helms, Azari, Robbins & Miller, 1998; Bertakis, Helms, Azari, Callahan, Robbins & Miller, 1999; Paasche-Orlow & Roter, 2003). In this investigation, we were particularly interested in whether physicians’ communication and perceptions were related to their orientations to the provider-patient relationship (Haidet, Dains, Paterniti, Hechtel, Chang, Tseng et al. 2002; Krupat, Bell, Kravitz, Thom & Azari, 2001; Krupat, Hiam, Fleming & Freeman, 1999). That is, do physicians who report a stronger belief in sharing control and understanding the patient’s perspective (i.e., a more patient-centered orientation) use more forms of patient-centered communication (e.g., clear explanations, partnership-building, support) and view their patients more favorably than do physicians oriented more toward biomedical issues and doctor control?
Second, variability in physicians’ communication and perceptions may be related to the patients’ demographic characteristics. Even the most well-meaning and egalitarian physicians may have stereotypes or biases based on a patient’s demographic status (Burgess, Fu & Van Ryn, 2004; Van Ryn, Burgess, Malat & Griffin, 2006). Racial bias, in particular, has been implicated in research showing that some physicians associate more negative attributes (e.g., non-compliant, less intelligent, more likely to abuse drugs and alcohol) to minority and less educated patients (Van Ryn & Burke, 2000), perceptions that in turn may affect physicians’ informativeness (Amir, 1987) and medical decision-making (Krupat, Irish, Kasten, Freund, Burns, Moskowitz et al. 1999; Schulman, Berlin, Harless, Kerner, Sistrunk, Gersh et al. 1999). Such findings have led some to explore whether demographic concordance between physician and patient may facilitate better relationships and more positive health care interactions because the physician and patient have some element of shared identity. Some evidence supports this claim, particularly with regard to racial concordance (Cooper et al., 2003; Cooper-Patrick, Gallo, Gonzales, Vu, Powe, Nelson et al. 1999; LaVeist & Nuru-Jeter, 2002; Saha, Komaromy, Koepsell & Bindman, 1999). Although there is little evidence indicating that physicians provide better care to patients similar in age or gender, we nevertheless examined whether differences in physicians’ communication and perceptions are uniquely related to physician-patient concordance with respect to race, age, and gender (see Figure 1).
Finally, the patient’s communication style can have a powerful effect on physician behavior and beliefs. The medical encounter, like other forms of social interaction, requires that the participants cooperate and coordinate their talk. Thus, any one interactant can exert considerable influence over the other (Street, 2001; Street & Millay, 2001). For example, physicians typically are more informative, accommodating, and supportive when patients ask questions, make requests, offer opinions, and express their fears and concerns (Gordon, Street, Sharf & Souchek, 2006; Heszen-Klemens & Lapinska, 1984; Kravitz, Epstein, Feldman, Franz, Azari, Wilkes et al. 2005; Street, 1991a; Street, 1992a; Street, Krupat, Bell, Kravitz & Haidet, 2003). Physicians generally are more responsive to the actively involved patient in part because they have a better understanding of the patient’s needs and concerns and in part because of conversational norms (e.g., ‘answers’ should follow ‘questions’, utterances should be topically connected) (Street, 2001). Moreover, any analysis of variability in physician communication should take into account the patient’s communication because it is often confounded with patients’ demographic characteristics. For example, black patients in some studies have been less active communicators than were white patients (Gordon et al., 2006; Johnson, Roter, Powe & Cooper, 2004; Siminoff et al., 2006; Wiltshire, Cronin, Sarto & Brown, 2006), women are more likely to discuss their feelings and emotions than are men (Hall & Roter, 1995; Street, Gordon, Ward, Krupat & Kravitz, 2005; Street, et al. 1993), and college educated patients are often more assertive and inquisitive than patients with a high school education or less (Siminoff et al., 2006; Street, Jr., Voigt, Geyer, Jr., Manning & Swanson, 1995).
In summary, physicians’ communication and perceptions of patients may be a function of various factors emerging from different aspects of communication processes. The importance of taking into account the collective influence of these factors can be demonstrated by contrasting two investigations. Siminoff et al. (Siminoff et al., 2006) reported that physician-patient communication in cancer consultations varied across several patient demographic characteristics. Physicians gave more information, used more partnership-building, and had more emotional talk with younger, better educated, and white patients. Yet, these same patients also tended to ask more questions and volunteer more information. Are these differences in physicians’ communication a function of patient demographics per se or of the patient’s communication? In contrast, a recent study of lung cancer consultations takes a more ecological approach (Gordon et al., 2006). This study found that physicians gave less information to black patients than to their white counterparts. This finding alone might suggest physician bias. However, the race effect on physician information-giving vanished once the patients’ communication was entered into the model. That is, black patients received less information than whites because they asked fewer questions and were less assertive; behaviors that elicited more information from physicians. Thus, our investigation examines the independent effects of various factors in order to identify the more powerful influences on physicians’ communication and perceptions.
METHODS
Research Setting, Participants, and Procedures
These data were collected as part of project CONNECT (Haidet & Street, 2006), a multi-faceted, cross-sectional study of communication and illness perceptions among patients and physicians of varying races. The setting for project CONNECT was 10 public and private primary care clinics in Houston, Texas. Twenty-nine primary care physicians (family practice, general internal medicine) were recruited to participate in the study. For each physician, we recruited one patient per half-day clinic session by sequentially approaching potential subjects as they arrived for their regularly scheduled visits. Patients were eligible to participate if they spoke English and were over 18 years of age. We recruited 6–10 patients per physician. A total of 270 patients agreed to participate. The study received IRB approval and informed consent was obtained from all patients and physicians.
Patients completed surveys prior to and after the consultation. These surveys included measures of patients’ demographics, including an estimate of the number of previous visits with the physician. At study entry, physicians completed the Patient-Provider Orientation Scale (PPOS) (Haidet et al., 2002; Krupat et al., 2000; Krupat, Yeager & Putnam, 2000), a measure that uses two subscales, Caring (importance of understanding patients’ perspectives) and Sharing (importance of sharing control with the patient), to measure physicians’ orientations to the physician-patient relationship along a doctor-centered/patient-centered continuum. Following visits with patients, physicians completed measures of their perceptions of the patient. We attempted to audiotape all the consultations. Due to audio-recording malfunctions, missed taping, and missing data on physician surveys, the total number of consultations included in the study was 207. The number of patients per physician ranged from 3 to 11 with a median of 7.
Measures of Physician and Patient Communication
Two coders rated the physician’s and patient’s communication on three sets of measures. First, a measure initially developed by Arntson and colleagues (Arntson, Makoul, Pendleton & Schofield, 1989) and later adapted by others (Street, 1991b; Street et al., 1995) was used to assess on 5-point Likert scales the extent to which the physician: a) was informative b) used supportive communication, and c) engaged in partnership-building (see Table 1). Because correlations among ratings of physicians’ informativeness, supportiveness, and partnership-building, were very high (> .71) and because each of these scales were measured with the same number of items (n = 4), they were summed to create a single measure, patient-centered communication.
Table 1.
Physician and Patient Communication Measures
Items Used to Measure Physicians’ Informativeness (I), Supportiveness (S), and Partnership-Building (P)
|
Items Assessing Patients’ Communication
|
Second, the degree to which patients were active participants was measured with an adaptation of Lerman’s perceived involvement in care scale (PICS) (Brody, Miller, Lerman, Smith & Caputo, 1989; Lerman, Brody, Caputo, Smith, Lazaro & Wolfson, 1990). We modified this patient self-report measure to make it appropriate for observer coding. For example, the item, “I asked the doctor a lot of questions” was modified to “The patient asked the doctor a lot of questions” (see Table 1).
Third, the global affect scales of the Roter Interaction Analysis System (Roter & Larson, 2002) were used to assess physician and patient affective communication during the consultation. The items in this measure use a 5-point scale to assess the degree to which physician and patient separately showed anger-irritation, anxiety-nervousness, dominance-assertiveness, interest-concern, friendliness-warmth, and sympathy-empathy. The RIAS Global Affect measure also has two scales for patients only, depression and emotional distress. The two coders participated in a two hour training session prior to coding the audio-recorded consultations. Once training was completed, each coder rated each consultation independently.
We assessed communication using the rating scales described above because coding systems that rely on counts, frequencies, and proportions of certain types of utterances (e.g., information and socio-emotional behaviors; patient assertiveness and question-asking) are both labor-intensive and only provide quantitative information about the degree to which certain verbal acts were performed. However, as is the case with other observer rating systems (Mead & Bower, 2000), the measures used in this study tap into both the quantity as well as the quality of the physicians’ and patients’ communication.1
Measures of Physicians’ Perceptions
Based on our reading of the literature and discussion with other physicians, we generated a list of nine items that tap into important elements of physicians’ perceptions of the patient as a communicator— “good historian,” “fully explained symptoms,” “understood treatment options,” “fully discussed his/her concerns,” “stayed on topic,” “asked no questions” (reverse scored), “was hard to get the patient to answer questions completely” (reverse scored), and “fully discussed fears.” The items were presented as 7-point bipolar scales. We also asked physicians to complete 2 Likert scale items that, when summed, created a measure of their perceptions of how satisfied the patient was (“The patient was satisfied with the visit,” “The patient was pleased with the care he/she received”), and 4 items that, when summed, created a measure of their perceptions of how likely the patient would adhere to prescribed treatments (“I expect the patient to follow my suggestions exactly,” “The patient will have a hard time doing what I recommended” (reverse scored), “The patient will be unable to do what is necessary to follow my plan” (reverse scored), “It will be easy for the patient to do the things I suggested”).
Data Analysis
As has been done in similar studies (Ambady, Laplante, Nguyen, Rosenthal, Chaumeton & Levinson, 2002; Harrigan, Gramata, Lucic & Margolis, 1989), the coders’ global affect ratings were initially subjected to factor analyses to reduce the number of variables and create composite measures of physician and patient affective communication. The same was done to the items assessing physician perceptions of the patient as a communicator since we did not assume this was a unidimensional scale. To examine the first research question, correlations were computed to assess the relationship of physicians’ communication behaviors to their perceptions of the patient as a communicator and whether they thought the patient was satisfied and likely to adhere. To identify variables having the strongest influence on physicians’ communication and perceptions, mixed model multiple linear regression procedures were used with the individual doctor as a random effect to account for patients being nested within physicians. The predictor variables included the patients’ demographics (race, age, gender, education), demographic concordance (race, gender, and age—10 years apart or less), and patients’ communication behaviors. The models also controlled for the number of previous visits the patient had with the physician. Finally, for measures on which the random effect for individual physician was significant, follow-up analyses were conducted to examine whether physicians’ communication and perceptions were related to the doctors’ gender, race, age, and orientation to the physician-patient relationship.
RESULTS
Overview
As shown in Table 2, the sample was diverse with respect to physician and patient race, age, and gender. While racial concordance was relatively balanced for white and black patients, the demographics of the sample were such that all Asian physicians and all Hispanic patients had racially discordant encounters.
Table 2.
Characteristics of Survey Populations
| Characteristic | Physician Sample (N=29) | Patient Sample (N=207) | Percent Concordant |
|---|---|---|---|
| Mean Age in yrs (SD) Range |
40 (8.1) 29–57 |
55.7 (14.7) 19–84 |
48.8% (Within 10 years) |
| Ethnicity | 41.4% Asian 27.6% African American 31% White |
38.8% African American 11.1% Hispanic 50.1% White |
32.1% |
| Percent Female | 40% | 39.1% | 57.8% |
| Education | NA | 13.8% High school or less 29.5% High School 35.5% Some College 21.7% College Degree plus |
21.7%a |
| Mean Score on PPOS (SD) Range |
73.1 (10.2) 52.2–92.2 |
NA | NA |
All physicians have college medical school degrees. Thus, the percent concordant on education is the same percent as patients with college degrees.
Intraclass correlations (ICC) were used to assess reliability between the two coders’ ratings of the communication measures. All correlations were statistically significant and ranged from .52 to .79 for the individual measures. Thus, the coders’ ratings were averaged to create one score per measure.
The factor analysis for physician affect revealed a two dimensional solution, positive affect (“interest,’ “empathy,” “friendly”) and contentious (“dominant,” “angry”), that accounted for 37% and 17% of the item variance, respectively. For patient affect, factor analysis revealed a three factor solution that included the same two factors (positive affect, contentious) as physician affect along with a third factor, distressed communication, that consisted of the “depression” and “emotional distress” items. The patient positive affect, contentiousness, and distressed communication factors accounted for 18%, 17%, and 13% of the item variance, respectively.
Factor analysis also was conducted on the physicians’ perceptions of the patient as a communicator. A two dimensional solution emerged. One factor (39% of the variance in factor loadings) was labeled good communicator (“good historian,’ “stayed on topic,’ “explained symptoms,” “understood treatment options,” “hard to get patient to answer questions”). The other factor, active participant (“fully discussed fears,” “asked no questions,” “fully discussed concerns”), accounted for an additional 15% of the item variance. Items that had a primary loading on the individual factors were summed to create measures of physician and patient affect and of physicians’ perceptions of the patient as a communicator. For all composite measures, reliabilities (Cronbach’s alpha) ranged from .51 to .94 (see Table 3).
Table 3.
Descriptive Statistics for the Communication and Perception Measures
| Measure | Mean (SD) | Range | Reliability |
|---|---|---|---|
| Physicians’ | |||
| Patient-centered communication | 52.11 (8.13) | 23–60 | .91 |
| Positive affect | 9.46 (2.18) | 4–15 | .71 |
| Contentiousness | 3.96 (1.19) | 2–8.5 | .51 |
| Perception of patient as a communicator | 21.88 (4.43) | 9–28 | .87 |
| Perception of patients as active participant | 15.18 (3.20) | 6–21 | .61 |
| Perception of patient satisfaction | 10.99 (2.06) | 2–14 | .94 |
| Perception of patient adherence | 14.62 (2.63) | 4–20 | .78 |
| Patients’ | |||
| Active participation | 23.32 (5.46) | 11–35 | .90 |
| Positive affect | 8.71 (1.85) | 4–13 | .68 |
| Contentiousness | 3.25 (1.26) | 2–10 | .61 |
| Emotional distress | 2.51 (1.16) | 2–9.5 | .78 |
Relationships among Physicians’ Communication and Perceptions
As shown in Table 4, physicians’ communication was moderately, but significantly correlated with their perceptions of patients. Specifically, physicians exhibited more patient-centered communication, more positive affect, and were less contentious with patients they perceived as good communicators and believed were more satisfied. Positive affect and patient-centered communication also were associated with doctors’ perceptions of a more involved patient. Finally, physicians were more patient-centered and less contentious with patients they believed were more likely to adhere to recommendations.
Table 4.
Correlations among Physicians’ Perceptions and Communication (N = 207)
| Physician Perceptions | ||||
|---|---|---|---|---|
| Physician Behavior | Good Communicator | Active Participation | Patient Satisfaction | Patient Adherence |
| Patient-centered Communication | .14* | .25*** | .22*** | .15* |
| Positive affect | .18** | .17** | .27*** | .09 |
| Contentious | −.21** | −.13 | −.29*** | −.18** |
P < .05
P < .01
P < .001
Predictors of Physicians’ Communication
Table 5 presents regression analyses of variables predicting physicians’ communication. The strongest predictor of a physician’s communication was the patient’s communication. Physicians were more patient-centered with actively involved patients, showed more positive affect when patients also had positive affect, and were more contentious with more contentious patients. Physician communication varied little with respect to patient demographic and concordance variables with one exception. Doctors were more contentious with black patients compared to white and Hispanic patients.
Table 5.
Factors affecting physicians’ communication with patients
| Patient-centered communication (N=207) | Positive affect (N=207) | Contentious (N=207) | ||||
|---|---|---|---|---|---|---|
| Estimate (SE) | P | Estimate (SE) | P | Estimate (SE) | P | |
| Physicians’ Communication Style | ||||||
| Individual Dr. effect | 31.2 (9.67) | 0.001 | 1.41 (0.46) | 0.003 | 0.11 (0.07) | 0.12 |
| Patients’ Demographics | ||||||
| Patient race = black (ref = white) | 1.23 (0.86) | 0.16 | 0.24 (0.23) | ns | 0.43 (0.16) | 0.009 |
| Patient race = Hispanic (ref = white) | −1.14 (1.31) | ns | 0.35 (0.35) | ns | 0.17 (0.25) | ns |
| Patient age | 0.01 (0.04) | ns | 0.02 (0.01) | 0.07 | 0.00 (0.01) | ns |
| Patient gender (ref = female) | −0.67 (1.07) | ns | 0.04 (0.27) | ns | 0.10 (0.17) | ns |
| Patient education (HS or less, some college, college graduate plus) | 0.11 (0.40) | ns | 0.12 (0.11) | ns | −0.08 (0.08) | ns |
| Physician-Patient Concordance | ||||||
| Racial concordance | 0.90 (1.0) | ns | 0.30 (0.27) | ns | 0.13 (0.17) | ns |
| Gender concordance | −0.43 (1.09) | ns | −0.37 (0.28) | 0.19 | 0.24 (0.17) | 0.17 |
| Age concordance (equal to or less than 10 years difference) | −0.20 (0.95) | ns | 0.01 (0.25) | ns | 0.26 (0.18) | 0.14 |
| Patient’s Communication | ||||||
| Patients’ active participation | 0.47 (0.09) | 0.000 | 0.03 (0.02) | ns | −0.03 (0.02) | 0.089 |
| Patients’ positive affect | 0.50 (0.24) | 0.041 | 0.54 (0.06) | 0.000 | 0.02 (0.04) | ns |
| Patients’ contentiousness | −0.48 (0.31) | 0.13 | −0.11 (0.08) | 0.20 | 0.47 (0.06) | 0.000 |
| Patients’ distress | 0.21 (0.30) | ns | 0.30 (0.08) | 0.000 | 0.00 (0.06) | ns |
Individual physicians differed in their patient-centered communication and positive affect (see Table 5). To explore whether these differences were related to physician characteristics, each individual physician’s scores on patient-centered communication and positive affect were averaged across their consultations to create one score per behavior per physician. Analyses were then conducted to determine whether these scores differed as a function of physician gender, race (black vs. white vs. Asian), age, and relational orientation (more patient-centered vs. more doctor-centered based on a median spilt of physicians’ PPOS scores). These analyses indicated that physicians reporting a more patient-centered orientation to the relationship displayed significantly more (P < .04) patient-centered communication (mean = 54.72) and positive affect (mean = 10.15) than did physicians reporting a more doctor-centered orientation (means = 48.44 and 8.72, respectively). Also, physicians of Asian descent were rated as showing less positive affect than did black and white doctors.
Predictors of Physicians’ Perceptions of Patients
The patient’s communication also was strongly predictive of physicians’ perceptions (Table 6). When patients showed more positive affect and were less contentious, physicians perceived them as more effective communicators and more satisfied with care. Interestingly, the degree to which patients actively participated in the visit was related only to the physicians’ perceptions of patient involvement. Physicians’ perceptions of patient adherence were not related to any of the patient communication variables although there was a trend (P < .06) for physicians to expect more adherence from patients expressing more positive affect.
Table 6.
Factors affecting physicians’ perceptions of patients
| Patient as good communicator (N=207) | Patient as active participant (N=207) | Perceived patient satisfaction (N=207) | Likelihood patient will adhere (N=207) | |||||
|---|---|---|---|---|---|---|---|---|
| Estimate (SE) | P | Estimate (SE) | P | Estimate (SE) | P | Estimate (SE) | P | |
| Physicians’ Communication Style | ||||||||
| Individual Dr. effect | 3.73 (1.80) | 0.04 | 3.67 (1.33) | 0.006 | 1.36 (0.54) | 0.012 | 1.22 (0.61) | 0.047 |
| Patients’ Demographics | ||||||||
| Patient race = black (ref = white) | −1.53 (0.66) | 0.02 | −0.53 (0.42) | ns | −0.72 (0.29) | 0.02 | −0.65 (0.42) | 0.12 |
| Patient race = Hisp. (ref = white) | −0.86 (1.01) | ns | 0.22 (0.65) | ns | −0.26 (0.45) | ns | 0.27(0.65) | ns |
| Patient age | −0.04 (0.03) | 0.11 | −0.01 (0.02) | ns | 0.01 (0.01) | ns | 0.03 (0.02) | 0.12 |
| Patient gender (ref = female) | −0.86 (0.74) | ns | −0.86 (0.50) | 0.089 | 0.14 (0.34) | ns | −0.51 (0.47) | ns |
| Patient education (HS or less, some college, college graduate) | 0.28 (0.31) | ns | 0.17 (0.20) | ns | 0.14 (0.14) | ns | −0.04(0.20) | ns |
| Physician-Patient Concordance | ||||||||
| Racial concordance | 0.64 (0.71) | ns | −0.69 (0.48) | 0.16 | 0.41 (0.36) | ns | 0.12 (0.45) | ns |
| Gender concordance | 1.26 (0.74) | 0.09 | .31 (0.51) | ns | −0.17 (0.35) | ns | −0.49 (0.47) | ns |
| Age concordance (equal to or less than 10 years difference) | −0.78 (0.73) | ns | −0.24 (0.47) | ns | −0.31 (0.32) | ns | 0.03 (0.47) | ns |
| Patient’s Communication | ||||||||
| Patients’ active participation | 0.02 (0.07) | ns | 0.14 (0.04) | 0.002 | −0.03 (0.03) | ns | −0.04 (0.04) | ns |
| Patients’ positive affect | 0.55 (0.18) | 0.00 | 0.28 (0.12) | 0.02 | 0.20 (0.08) | 0.014 | 0.22 (0.12) | 0.057 |
| Patients’ contentiousness | −0.63 (0.24) | 0.01 | 0.07 (0.16) | ns | −0.48 (0.11) | 0.000 | −0.03 (0.15) | ns |
| Patients’ distress | 0.14 (0.23) | ns | 0.22 (0.15) | 0.13 | 0.01 (0.10) | ns | 0.07 (0.15) | ns |
The only demographic variable predicting physician perceptions was race, as physicians perceived black patients to be less effective communicators and less satisfied than white and Hispanic patients. Finally, there were individual doctor differences across all perceptions indicating that some physicians perceived their patients more favorably than did other doctors. However, these differences were not related to any of the physicians’ characteristics.
Secondary Analyses Related to Patient Race
We were concerned by the findings that physicians were more contentious with black patients and perceived these patients as less effective communicators and less satisfied with care. Although our sample size precluded the feasibility of studying interaction effects in the regression models, post hoc analyses were conducted to explore possible reasons for the race effects. Given the reciprocal relationships between physician and patient affect, one possibility is that black patients were more contentious and displayed less positive affect than white and Hispanic patients. Post hoc comparisons revealed no significant patient race effects on these measures. Second, perhaps the doctors’ race influenced their communication with and perceptions of black patients. There was some evidence of this. Specifically, Asian doctors perceived black patients (mean = 19.4) as significantly (P < .04) less effective communicators than did white (mean = 21.5) and black (mean = 21.7) physicians. Also, black physicians thought their black patients were more satisfied with care (mean = 11.1) than did Asian doctors (mean = 10.1, P < .03) though neither group differed from the white physicians’ perceptions of patient satisfaction (mean = 10.8).
DISCUSSION
The findings of this investigation indicated that not only were physicians’ communication behaviors linked to their perceptions of patients, both were influenced by a variety of factors, the most powerful being the patient’s communication, the patient’s ethnicity, and the physicians’ orientation to the doctor-patient relationship. These findings have important implications for future research and clinical practice.
First, physicians were more patient-centered, less contentious, and showed more positive affect to patients they judged to be better communicators, more satisfied with care, and more likely to adhere to treatment. This finding is consistent with a growing body of evidence indicating that how a physician perceives a patient (likeable, intelligent, adherent) is related to how that doctor treats the patient (Amir, 1987; Beach, Roter, Wang, Duggan & Cooper, 2006a; Gerbert, 1984; Hall et al., 1993; Hall et al., 2002; Van Ryn et al., 2006). However, to assume a causal pathway from perception to communication would be premature. As shown in Tables 5 and 6, other factors, such as the patient’s communication and the physician’s personal attributes, appeared to influence both physician perceptions and communication.
Second, patients’ expressions of positive affect consistently predicted more positive physician communication (patient-centeredness, positive affect) and judgments (patient as a good communicator, satisfied with care). Physicians also were more patient-centered with more involved patients. Conversely, physicians were more contentious with contentious patients whom they also viewed as less effective communicators and less satisfied. These results likely reflect the dynamics of communicative reciprocity and mutual influence in medical encounters. One person’s expression of positive affect typically elicits similar behavior from another thereby creating a mutually friendly, supportive interaction. Similarly, patients who ask questions, express concerns, and state preferences provide opportunities for physicians to provide information, offer support, and accommodate requests which, in turn, legitimize continued patient involvement. Yet, the reciprocity also may be negative in that contentiousness on the part of one interactant could breed contentiousness and negative perceptions from the other interactant, at least in some medical encounters.
Third, considerable variability in physicians’ communication was related to differences among individual doctors, particularly with respect to the physician’s orientation to the physician-patient relationship. Doctors who self-reported a patient-centered orientation were rated by coders as using a more informative, supportive, and facilitative communication style than did doctors holding a more doctor-centered orientation. Perhaps physicians who value the patient’s perspective and participation have an understanding of the patient that facilitates both the task (explaining medical issues, describing treatment options) and relationship (showing respect, encouraging patient participation) functions of communication. Because previous studies have demonstrated that students adopt progressively less patient-centered orientations in later years of medical school (Haidet et al., 2002; Haidet & Stein, 2006), our findings suggest that communication skill training must be an ongoing and sustained part of medical and continuing education.
Fourth, considered collectively, patient demographics and concordance had little effect on physician communication and perceptions with one disturbing exception—physicians were more contentious with black patients whom they also perceived as less effective communicators and less satisfied with care. Follow-up analyses indicated that the communication of black physicians with black patients was not significantly different from that of white and Asian doctors, although black and white physicians did perceive patients as better communicators than did Asian physicians. Several explanations could account for these findings. First, there could a subtle bias toward the communication of black patients. This would be consistent with other research indicating that, compared to white patients, black patients (a) are more likely to believe that a good self-presentation during the office visit is important to getting good medical care (Malat, Van Ryn & Purcell, 2006), (b) need to be more assertive to receive more thorough diagnostic testing (Krupat et al., 1999), and (c) are more likely to have negative attributes assigned to them by physicians (Van Ryn & Burke, 2000). Second, for cultural or other reasons, physicians may have more difficulty interacting with some black patients, thus leading to more contentious behavior and less positive impressions. In turn, some black patients may struggle in their communication with physicians given past experiences within the health care system (Matthews, Sellergren, Manfredi & Williams, 2002). Regardless of the reason, race and ethnicity continue to be associated with communicative difficulties in medical encounters in ways that affect quality of care and could contribute to health disparities (Ashton, Haidet, Paterniti, Collins, Gordon, O’Malley et al. 2003).
Limitations
The study had several limitations. First, our sample size of just over 200 interactions from clinics within a large southern US city was perhaps too small and localized to generalize to other settings. Second, while our findings likely reflect mutual influence between physician and patient communication behavior, we did not examine how these cycles of positive and negative communication get started. For example, were patients more active participants because of the physicians’ patient-centered communication, or were physicians more informative and supportive because patients were asking questions, expressing concerns, and stating preferences? Third, we acknowledge that physician-patient communication and outcomes can be affected by other variables not examined in this study including the patient’s health status, physician specialty, reason for the visit, and type of health care facility.
Fourth, findings related to the patient’s ethnicity are important, but tell us nothing of why they occurred. More attention to cognitive and affective processes (attitudes, stereotypes) that account for these race-related communicative disparities is needed. As moderators of communication process and outcome relationships, demographic characteristics are difficult to change, but affective-cognitive processes underlying these effects may be amenable to interventions for improved communication. Finally, while we found little evidence of concordance effects, more research needs examine concordance in relation to measures of the quality of the relationship (e.g., trust, perceived similarity, rapport), the latter being the likely mediator of concordance effects on patient outcomes.
Acknowledgments
This research was supported in part by Career Development Awards to Drs. XXX and XXX from the Office of Research and Development, Health Services Research and Development Service, Department of Veterans Affairs (VA) and by grant number P01 HS10876 from the Agency for Healthcare Research and Quality. The authors also acknowledge the helpful suggestions offered by the Editor and four anonymous reviewers.
Footnotes
To establish convergent validity for using this approach of having coders rate the physicians’ communication, we had two different coders (not involved in this study) code the audiotapes using Street’s (Street, Jr. & Millay, 2001) patient-participation and physician facilitation coding scheme, a system that categorizes the frequency with which patients use active communication behaviors (ask questions, acts of assertiveness, expressions of concerns) and with which doctors use partnership-building and supportive communication (e.g., reassurance, empathy, encouragement). Ratings of the physicians’ supportiveness were significantly correlated with the frequency with which physicians used supportive statements (r = .25, P < .001) and ratings of partnership-building were correlated with the frequency with which doctors used partnering statements (r = .33, P < .001). Ratings of patient active participation also were significantly correlated with the frequency of patient question asking, expressions of concerns, and acts of assertiveness) (r = .46, P < .001). While we did not code the frequency of information-giving acts, these data support the validity for the measures used in this study.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aita V, McIlvain H, Backer E, McVea K, Crabtree B. Patient-centered care and communication in primary care practice: what is involved? Patient Education and Counseling. 2005;58(3):296–304. doi: 10.1016/j.pec.2004.12.008. [DOI] [PubMed] [Google Scholar]
- Ambady N, Laplante D, Nguyen T, Rosenthal R, Chaumeton N, Levinson W. Surgeons’ tone of voice: a clue to malpractice history. Surgery. 2002;132(1):5–9. doi: 10.1067/msy.2002.124733. [DOI] [PubMed] [Google Scholar]
- Amir M. Considerations guiding physicians when informing cancer patients. Social Science & Medicine. 1987;24(9):741–748. doi: 10.1016/0277-9536(87)90111-0. [DOI] [PubMed] [Google Scholar]
- Arntson P, Makoul G, Pendleton D, Schofield T. Patient perceptions of medical encounters in Great Britain: Variation with health loci of control and socidemographic factors. Health Communication. 1989;1(2):75–95. [Google Scholar]
- Ashton CM, Haidet P, Paterniti DA, Collins TC, Gordon HS, O’Malley K, Petersen LA, Sharf BF, Suarez-Almazor ME, Wray NP, Street RL., Jr Racial and ethnic disparities in the use of health services: bias, preferences, or poor communication? Journal of General Internal Medicine. 2003;18(2):146–152. doi: 10.1046/j.1525-1497.2003.20532.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beach MC, Roter DL, Wang NY, Duggan PS, Cooper LA. Are physicians’ attitudes of respect accurately perceived by patients and associated with more positive communication behaviors? Patient Education and Counseling. 2006;62(3):347–354. doi: 10.1016/j.pec.2006.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertakis KD, Callahan EJ, Helms LJ, Azari R, Robbins JA, Miller J. Physician practice styles and patient outcomes: differences between family practice and general internal medicine. Medical Care. 1998;36(6):879–891. doi: 10.1097/00005650-199806000-00011. [DOI] [PubMed] [Google Scholar]
- Bertakis KD, Helms LJ, Azari R, Callahan EJ, Robbins JA, Miller J. Differences between family physicians’ and general internists’ medical charges. Medical Care. 1999;37(1):78–82. doi: 10.1097/00005650-199901000-00011. [DOI] [PubMed] [Google Scholar]
- Bertakis KD, Helms LJ, Callahan EJ, Azari R, Robbins JA. The influence of gender on physician practice style. Medical Care. 1995;33(4):407–416. doi: 10.1097/00005650-199504000-00007. [DOI] [PubMed] [Google Scholar]
- Brody DS, Miller SM, Lerman CE, Smith DG, Caputo GC. Patient perception of involvement in medical care: relationship to illness attitudes and outcomes. Journal of General Internal Medicine. 1989;4(6):506–511. doi: 10.1007/BF02599549. [DOI] [PubMed] [Google Scholar]
- Burgess DJ, Fu SS, Van Ryn M. Why do providers contribute to disparities and what can be done about it? Journal of General Internal Medicine. 2004;19(11):1154–1159. doi: 10.1111/j.1525-1497.2004.30227.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper LA, Roter DL, Johnson RL, Ford DE, Steinwachs DM, Powe NR. Patient-centered communication, ratings of care, and concordance of patient and physician race. Annals of Internal Medicine. 2003;139(11):907–915. doi: 10.7326/0003-4819-139-11-200312020-00009. [DOI] [PubMed] [Google Scholar]
- Cooper-Patrick L, Gallo JJ, Gonzales JJ, Vu HT, Powe NR, Nelson C, Ford DE. Race, gender, and partnership in the patient-physician relationship. Journal of the American Medical Association. 1999;282(6):583–589. doi: 10.1001/jama.282.6.583. [DOI] [PubMed] [Google Scholar]
- Gerbert B. Perceived likeability and competence of simulated patients: influence on physicians’ management plans. Social Science & Medicine. 1984;18(12):1053–1059. doi: 10.1016/0277-9536(84)90164-3. [DOI] [PubMed] [Google Scholar]
- Gordon HS, Street RL, Jr, Sharf BF, Souchek J. Racial differences in doctors’ information-giving and patients’ participation. Cancer. 2006;107(6):1313–1320. doi: 10.1002/cncr.22122. [DOI] [PubMed] [Google Scholar]
- Greene MG, Adelman RD, Charon R, Friedmann E. Concordance between physicians and their older and younger patients in the primary care medical encounter. Gerontologist. 1989;29(6):808–813. doi: 10.1093/geront/29.6.808. [DOI] [PubMed] [Google Scholar]
- Haidet P, Dains JE, Paterniti DA, Hechtel L, Chang T, Tseng E, Rogers JC. Medical student attitudes toward the doctor-patient relationship. Medical Education. 2002;36(6):568–574. doi: 10.1046/j.1365-2923.2002.01233.x. [DOI] [PubMed] [Google Scholar]
- Haidet P, Stein HF. The role of the student-teacher relationship in the formation of physicians. The hidden curriculum as process. Journal of General Internal Medicine. 2006;21(Suppl 1):S16–S20. doi: 10.1111/j.1525-1497.2006.00304.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haidet P, Street RL., Jr Project CONNECT. Medical Encounter. 2006;20(3):33–34. [Google Scholar]
- Hall JA, Epstein AM, DeCiantis ML, McNeil BJ. Physicians’ liking for their patients: more evidence for the role of affect in medical care. Health Psychology. 1993;12(2):140–146. doi: 10.1037//0278-6133.12.2.140. [DOI] [PubMed] [Google Scholar]
- Hall JA, Horgan TG, Stein TS, Roter DL. Liking in the physician--patient relationship. Patient Education and Counseling. 2002;48(1):69–77. doi: 10.1016/s0738-3991(02)00071-x. [DOI] [PubMed] [Google Scholar]
- Hall JA, Roter DL. Patient gender and communication with physicians: results of a community-based study. Women’s Health. 1995;1(1):77–95. [PubMed] [Google Scholar]
- Hall JA, Roter DL. Medical communication and gender: a summary of research. Journal Gender Specific Medicine. 1998;1(2):39–42. [PubMed] [Google Scholar]
- Harrigan JA, Gramata JF, Lucic KS, Margolis C. It’s how you say it: physicians’ vocal behavior. Social Science & Medicine. 1989;28(1):87–92. doi: 10.1016/0277-9536(89)90310-9. [DOI] [PubMed] [Google Scholar]
- Henman MJ, Butow PN, Brown RF, Boyle F, Tattersall MH. Lay constructions of decision-making in cancer. Psycho-oncology. 2002;11(4):295–306. doi: 10.1002/pon.566. [DOI] [PubMed] [Google Scholar]
- Heszen-Klemens I, Lapinska E. Doctor-patient interaction, patients’ health behavior and effects of treatment. Social Science & Medicine. 1984;19(1):9–18. doi: 10.1016/0277-9536(84)90132-1. [DOI] [PubMed] [Google Scholar]
- Jahng KH, Martin LR, Golin CE, DiMatteo MR. Preferences for medical collaboration: patient-physician congruence and patient outcomes. Patient Education and Counseling. 2005;57(3):308–314. doi: 10.1016/j.pec.2004.08.006. [DOI] [PubMed] [Google Scholar]
- Johnson RL, Roter D, Powe NR, Cooper LA. Patient race/ethnicity and quality of patient-physician communication during medical visits. American Journal of Public Health. 2004;94(12):2084–2090. doi: 10.2105/ajph.94.12.2084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan SH, Greenfield S, Ware JE., Jr Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Medical Care. 1989;27(3 Suppl):S110–S127. doi: 10.1097/00005650-198903001-00010. [DOI] [PubMed] [Google Scholar]
- Koehn PH, Swick HM. Medical education for a changing world: moving beyond cultural competence into transnational competence. Academic Medicine. 2006;81(6):548–556. doi: 10.1097/01.ACM.0000225217.15207.d4. [DOI] [PubMed] [Google Scholar]
- Kravitz RL, Epstein RM, Feldman MD, Franz CE, Azari R, Wilkes MS, Hinton L, Franks P. Influence of patients’ requests for direct-to-consumer advertised antidepressants: a randomized controlled trial. Journal of the American Medical Association. 2005;293(16):1995–2002. doi: 10.1001/jama.293.16.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krupat E, Bell RA, Kravitz RL, Thom D, Azari R. When physicians and patients think alike: patient-centered beliefs and their impact on satisfaction and trust. Journal of Family Practice. 2001;50(12):1057–1062. [PubMed] [Google Scholar]
- Krupat E, Hiam CM, Fleming MZ, Freeman P. Patient-centeredness and its correlates among first year medical students. International Journal of Psychiatry in Medicine. 1999;29(3):347–356. doi: 10.2190/DVCQ-4LC8-NT7H-KE0L. [DOI] [PubMed] [Google Scholar]
- Krupat E, Irish JT, Kasten LE, Freund KM, Burns RB, Moskowitz MA, McKinlay JB. Patient assertiveness and physician decision-making among older breast cancer patients. Social Science & Medicine. 1999;49(4):449–457. doi: 10.1016/s0277-9536(99)00106-9. [DOI] [PubMed] [Google Scholar]
- Krupat E, Rosenkranz SL, Yeager CM, Barnard K, Putnam SM, Inui TS. The practice orientations of physicians and patients: the effect of doctor-patient congruence on satisfaction. Patient Education and Counseling. 2000;39(1):49–59. doi: 10.1016/s0738-3991(99)00090-7. [DOI] [PubMed] [Google Scholar]
- Krupat E, Yeager CM, Putnam S. Patient role orientations, doctor-patient fit, and visit satisfaction. Psychology and Health. 2000;15:707–719. [Google Scholar]
- LaVeist TA, Nuru-Jeter A. Is doctor-patient race concordance associated with greater satisfaction with care? Journal of Health and Social Behavior. 2002;43(3):296–306. [PubMed] [Google Scholar]
- Lerman CE, Brody DS, Caputo GC, Smith DG, Lazaro CG, Wolfson HG. Patients’ Perceived Involvement in Care Scale: relationship to attitudes about illness and medical care. Journal of General Internal Medicine. 1990;5(1):29–33. doi: 10.1007/BF02602306. [DOI] [PubMed] [Google Scholar]
- Levinson W, Roter D. Physicians’ psychosocial beliefs correlate with their patient communication skills. Journal of General Internal Medicine. 1995;10(7):375–379. doi: 10.1007/BF02599834. [DOI] [PubMed] [Google Scholar]
- Malat JR, Van Ryn M, Purcell D. Race, socioeconomic status, and the perceived importance of positive self-presentation in health care. Social Science & Medicine. 2006;62(10):2479–2488. doi: 10.1016/j.socscimed.2005.11.014. [DOI] [PubMed] [Google Scholar]
- Matthews AK, Sellergren SA, Manfredi C, Williams M. Factors influencing medical information seeking among African American cancer patients. Journal of health Communication. 2002;7(3):205–219. doi: 10.1080/10810730290088094. [DOI] [PubMed] [Google Scholar]
- Mead N, Bower P. Measuring patient-centredness: a comparison of three observation-based instruments. Patient Education and Counseling. 2000;39(1):71–80. doi: 10.1016/s0738-3991(99)00092-0. [DOI] [PubMed] [Google Scholar]
- Ong LM, de Haes JC, Hoos AM, Lammes FB. Doctor-patient communication: a review of the literature. Social Science & Medicine. 1995;40(7):903–918. doi: 10.1016/0277-9536(94)00155-m. [DOI] [PubMed] [Google Scholar]
- Paasche-Orlow M, Roter D. The communication patterns of internal medicine and family practice physicians. Journal of the American Board of Family Practice. 2003;16(6):485–493. doi: 10.3122/jabfm.16.6.485. [DOI] [PubMed] [Google Scholar]
- Roter D, Larson S. The Roter interaction analysis system (RIAS): utility and flexibility for analysis of medical interactions. Patient Education and Counseling. 2002;46(4):243–251. doi: 10.1016/s0738-3991(02)00012-5. [DOI] [PubMed] [Google Scholar]
- Roter DL, Stewart M, Putnam SM, Lipkin M, Jr, Stiles W, Inui TS. Communication patterns of primary care physicians. Journal of the American Medical Association. 1997;277(4):350–356. [PubMed] [Google Scholar]
- Saha S, Komaromy M, Koepsell TD, Bindman AB. Patient-physician racial concordance and the perceived quality and use of health care. Archives of Internal Medicine. 1999;159(9):997–1004. doi: 10.1001/archinte.159.9.997. [DOI] [PubMed] [Google Scholar]
- Schulman KA, Berlin JA, Harless W, Kerner JF, Sistrunk S, Gersh BJ, Dube R, Taleghani CK, Burke JE, Williams S, Eisenberg JM, Escarce JJ. The effect of race and sex on physicians’ recommendations for cardiac catheterization. New England Journal of Medicine. 1999;340(8):618–626. doi: 10.1056/NEJM199902253400806. [DOI] [PubMed] [Google Scholar]
- Siminoff LA, Graham GC, Gordon NH. Cancer communication patterns and the influence of patient characteristics: Disparities in information-giving and affective behaviors. Patient Education and Counseling. 2006;62(3):355–360. doi: 10.1016/j.pec.2006.06.011. [DOI] [PubMed] [Google Scholar]
- Stewart M, Brown JB, Donner A, McWhinney IR, Oates J, Weston WW, Jordan J. The impact of patient-centered care on outcomes. Journal of Family Practice. 2000;49(9):796–804. [PubMed] [Google Scholar]
- Street RL., Jr Information-giving in medical consultations: the influence of patients’ communicative styles and personal characteristics. Social Science & Medicine. 1991a;32(5):541–8. doi: 10.1016/0277-9536(91)90288-n. [DOI] [PubMed] [Google Scholar]
- Street RL., Jr Physicians’ communication and parents’ evaluations of pediatric consultations. Medical Care. 1991b;29(11):1146–1152. doi: 10.1097/00005650-199111000-00006. [DOI] [PubMed] [Google Scholar]
- Street RL., Jr Communicative styles and adaptations in physician-parent consultations. Social Science & Medicine. 1992a;34(10):1155–1163. doi: 10.1016/0277-9536(92)90289-3. [DOI] [PubMed] [Google Scholar]
- Street RL., Jr Communicative styles and adaptations in physician-parent consultations. Social Science & Medicine. 1992b;34(10):1155–1163. doi: 10.1016/0277-9536(92)90289-3. [DOI] [PubMed] [Google Scholar]
- Street RL., Jr . Active patients as powerful communicators. In: Robinson WP, Giles H, editors. The new handbook of language and social psychology. New York: John Wiley & Sons; 2001. pp. 541–560. [Google Scholar]
- Street RL., Jr . Communication in medical encounters: An ecological perspective. In: Thompson T, Dorsey A, Miller K, Parrott R, editors. The handbook of health communication. Mahwah, NJ: Erlbaum; 2003. pp. 63–89. [Google Scholar]
- Street RL, Jr, Gordon HS, Ward MM, Krupat E, Kravitz RL. Patient participation in medical consultations: why some patients are more involved than others. Medical Care. 2005;43(10):960–969. doi: 10.1097/01.mlr.0000178172.40344.70. [DOI] [PubMed] [Google Scholar]
- Street RL, Jr, Krupat E, Bell RA, Kravitz RL, Haidet P. Beliefs about control in the physician-patient relationship: effect on communication in medical encounters. Journal of General Internal Medicine. 2003;18(8):609–616. doi: 10.1046/j.1525-1497.2003.20749.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Street RL, Jr, Millay B. Analyzing patient participation in medical encounters. Health Communication. 2001;13(1):61–73. doi: 10.1207/S15327027HC1301_06. [DOI] [PubMed] [Google Scholar]
- Street RL, Jr, Piziak VK, Carpentier WS, Herzog J, Hejl J, Skinner G, McLellan L. Provider-patient communication and metabolic control. Diabetes Care. 1993;16(5):714–721. doi: 10.2337/diacare.16.5.714. [DOI] [PubMed] [Google Scholar]
- Street RL, Jr, Voigt B, Geyer C, Jr, Manning T, Swanson GP. Increasing patient involvement in choosing treatment for early breast cancer. Cancer. 1995;76(11):2275–2285. doi: 10.1002/1097-0142(19951201)76:11<2275::aid-cncr2820761115>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- Trummer UF, Mueller UO, Nowak P, Stidl T, Pelikan JM. Does physician-patient communication that aims at empowering patients improve clinical outcome? A case study. Patient Education and Counseling. 2006;61(2):299–306. doi: 10.1016/j.pec.2005.04.009. [DOI] [PubMed] [Google Scholar]
- Van Ryn M, Burgess D, Malat J, Griffin J. Physicians’ perceptions of patients’ social and behavioral characteristics and race disparities in treatment recommendations for men with coronary artery disease. American Journal of Public Health. 2006;96(2):351–357. doi: 10.2105/AJPH.2004.041806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Ryn M, Burke J. The effect of patient race and socio-economic status on physicians’ perceptions of patients. Social Science & Medicine. 2000;50(6):813–828. doi: 10.1016/s0277-9536(99)00338-x. [DOI] [PubMed] [Google Scholar]
- Waitzkin H. Information giving in medical care. Journal of Health and Social Behavior. 1985;26(2):81–101. [PubMed] [Google Scholar]
- Wiltshire J, Cronin K, Sarto GE, Brown R. Self-advocacy during the medical encounter: use of health information and racial/ethnic differences. Medical Care. 2006;44(2):100–109. doi: 10.1097/01.mlr.0000196975.52557.b7. [DOI] [PubMed] [Google Scholar]
- Zandbelt LC, Smets EM, Oort FJ, Godfried MH, de Haes HC. Determinants of physicians’ patient-centred behaviour in the medical specialist encounter. Social Science & Medicine. 2006;63(4):899–910. doi: 10.1016/j.socscimed.2006.01.024. [DOI] [PubMed] [Google Scholar]


