The endothelium, once considered a mere selectively permeable barrier between the bloodstream and the outer vascular wall, is now recognized to be a crucial homeostatic organ, fundamental for the regulation of the vascular tone and structure. Indeed, endothelial cells are able to synthesize and secrete a broad spectrum of anti-atherosclerotic substances, the most characterized of which is nitric oxide (NO), a gas that is generated from the metabolism of l-arginine by endothelial NO synthase (eNOS), constitutively expressed in endothelial cells (1). Under physiologic conditions, endothelial stimulation induces the production and release of NO, which diffuses to surrounding tissue and cells and exerts its cardiovascular protective role by relaxing media-smooth muscle cells, preventing leukocyte adhesion and migration into the arterial wall, muscle cell proliferation, platelet adhesion and aggregation, and adhesion molecule expression (1,2). In disease conditions, including the presence of cardiovascular risk factors, the endothelium undergoes functional and structural alterations, thus losing its protective role and becoming a proatherosclerotic structure (1). In the earliest stages, the principal endothelial alteration is merely functional and addressed as “endothelial dysfunction.” The fundamental feature of this condition is the impaired NO bioavailability. This can be the consequence of either a reduced production by eNOS or, more frequently, of an increased breakdown by reactive oxygen species (ROS) (1,2). In the presence of impaired NO bioavailability, the endothelium implements various physiological pathways in the attempt to compensate for NO deficiency. For instance, endothelium-dependent vasodilation is warranted, although impaired, also in the presence of cardiovascular risk factors by the production and release of endothelium-derived vasodilators other than NO, such as prostanoids and other endothelium-derived hyperpolarizing factors. Along with NO deficiency, a dysfunctioning endothelium also becomes the source of other substances and mediators that are detrimental to the arterial wall, including endothelin-1, tromboxane A2, prostaglandin H2, and ROS (2). The presence of endothelial dysfunction, whether primary or after cardiovascular risk factors, has been implicated in the pathogenesis of atherosclerosis and thrombosis, both for the loss of its protective capability and for the induction of proatherothrombotic mechanisms (2,3).
The regulation of the endothelial processes is largely vascular district–specific, thus producing different results in various organs and tissues. Within the same vascular district, it varies largely in relation to vessel size, i.e., large arteries (macrocirculation) versus arterioles (microcirculation). For this reason, the use of systemic circulating markers of endothelial function is unreliable. Moreover, NO is a volatile substance, with a very short half-life, and therefore its moment-by-moment quantification in a specific vascular area is almost impossible. Therefore, its bioavailability is usually evaluated in humans by measuring the downstream effects, namely the vasodilation induced by the local stimulation of NO production by specific external mechanical and pharmacological stimuli, i.e., through vascular reactivity tests (4). In particular, endothelium-dependent relaxation has been evaluated by the use of either receptor-operated (acetylcholine, bradykinin, substance P), mechanical (increase in shear stress), or mixed (dynamic exercise and cold pressor test) stimuli and in different vascular beds (4,5). At the coronary level, endothelial function can be assessed in the macrocirculation by quantitative angiography, evaluating the change in coronary artery diameter after local infusion of agonists (e.g., acetylcholine), and in the microcirculation as changes in flow by intravascular ultrasound (4). This central approach is potentially the one with the highest clinical value, since it explores the vascular bed more often involved by the atherosclerotic process and is responsible for cardiac events. However, its invasiveness highly limits its applicability (4). Therefore, several other techniques have been developed to assess peripheral circulation endothelial function. In particular, peripheral microcirculation can be contemplatedly studied by venous plethysmography to evaluate forearm blood flow changes to intra-arterial infusion of various substances. This approach is useful, since it facilitates the study of mechanisms underlying endothelial dysfunction by administering endothelial agonists and antagonists (4). However, again, forearm blood flow is still invasive and requires brachial artery cannulation. For this reason, in the last decade, flow-mediated dilation (FMD) of the brachial artery has been widely used among researchers. Indeed, although its reproducibility is limited, FMD has the advantage of being completely noninvasive since it uses ultrasound analysis of brachial artery diameter after a local increase in shear stress, induced by a 5-min forearm ischemia (4). However, it is noteworthy that vascular responses obtained in different vascular areas/districts and using different stimuli and techniques are poorly related (6). Considering this aspect and the autocrine-paracrine nature of endothelial physiology, extreme caution should be taken in interpreting experimental studies and mostly in considering data obtained in a vascular region as indicative of endothelial function in other areas.
MECHANISMS UNDERLYING DIABETES-RELATED ENDOTHELIAL DYSFUNCTION
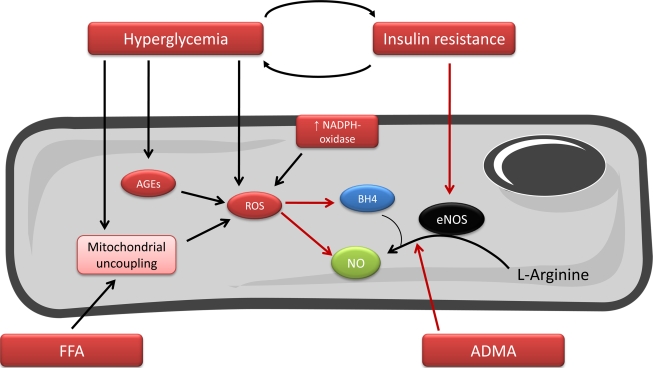
Patients with diabetes invariably show an impairment of endothelium-dependent vasodilation. This is partly due to the frequent association of the disease with other cardiovascular risk factors, including hypertension, obesity, and dyslipidemia. Moreover diabetic as well as obese patients usually consume a high-calorie diet rich in macronutrients that per se is able to induce vascular abnormalities. Indeed, protein (7), lipid (7), and glucose (8) loads are associated with a marked production in ROS, and high-fat meals are associated with an impaired endothelial-dependent vasodilation (9). A crucial negative effect is particularly attributable to high levels of circulating free fatty acids, which are able to induce ROS production and impair endothelial function (10). Mechanisms of endothelial damage in diabetes, independently from other cardiovascular risk factors, include insulin resistance, hyperglycemia, and low-grade systemic inflammation (11) (Fig. 1).
Figure 1.
Principal mechanisms responsible for endothelial dysfunction in diabetes. NO is the principal anti-atherosclerotic endothelium-derived mediator. It is formed from l-arginine by eNOS, being tetrahydrobiopterin (BH4), a crucial cofactor for the reaction. Endothelial dysfunction is defined by the presence of a reduced NO bioavailability. In the presence of diabetes, characterized by the existence of insulin resistance and hyperglycemia, endothelial dysfunction is due to both reduced production (increased circulating levels of the eNOS endogenous inhibitor asymmetric dimethylarginine [ADMA], decreased cellular levels of BH4 and decreased eNOS activation) and to an increased breakdown of NO by ROS. AGEs, advanced aging end products; FFA, free fatty acids.
A large amount of literature has been published on the interaction between insulin and NO system. It was shown that, in normal subjects, insulin is able to induce a dose-dependent increase in lower limb blood flow by reducing vascular resistance in skeletal muscle (12), mainly vasodilating the microcirculation (13). This observed vasodilatory effect of insulin is, at least partly, mediated by the enhanced production of NO both through the activation of the insulin receptor substrate-1/phosphoinositol 3-kinase/Akt pathway (14) and increased expression of eNOS (15). Interestingly, studies on lower limb circulation showed that the magnitude of vasodilation to insulin appears to be linked to the rate of insulin-mediated glucose metabolism (16). However, some controversies exist on this topic, with other groups, including ours (17), failing to detect a net direct effect of insulin in inducing vasodilation. The reasons for this could be related to the use of different methodology used and different analyzed vascular districts. Indeed, we previously showed no net direct effect of insulin on forearm microcirculation, but a potentiating effect of insulin on acetylcholine-mediated vasodilation at this level, possibly through a hyperpolarizing effect on the endothelium (17).
However, insulin downstream pathways, whether through a direct interaction with the eNOS/NO system or other intracellular systems are implicated in the regulation of vascular tone and reactivity, since the presence of insulin resistance is associated with the presence of endothelial dysfunction, not only in diabetes and obesity, but also in more clean models of insulin resistance, such as polycystic ovary syndrome (18).
ENDOTHELIAL FUNCTION AND OTHER CARDIOVASCULAR RISK FACTORS
Endothelial dysfunction, detected as the presence of reduced vasodilating response to endothelial stimuli, has been observed to be associated with major cardiovascular risk factors, such as aging, hyperhomocysteinemia, postmenopause state, smoking, diabetes, hypercholesterolemia, and hypertension (3).
The presence of multiple risk factors, each contributing to the development of impaired NO bioavailability by different mechanisms, may be able to determine a progressive worsening of endothelial function. Accordingly, endothelial function in the coronary circulation was found to be inversely associated with the number of risk factors (19) and therefore with the global cardiovascular risk. This was also confirmed in the Framingham population, in which an escalating inverse relationship between endothelium-dependent relaxation, estimated by FMD, and the cardiovascular risk score, evaluated according to tables from “Framingham risk score,” was demonstrated (9).
Moreover, the relationship between endothelial dysfunction and the presence of cardiovascular risk factors may be two-way. Indeed, recent data in postmenopausal women suggest that endothelial dysfunction may be a predisposing factor, or an anticipating marker for the development of hypertension (20) and diabetes (21), thus being not only a consequence or a collateral feature of risk factors, but also a possible pathogenetic mechanism for their onset.
ENDOTHELIAL FUNCTION AND TARGET ORGAN DAMAGE
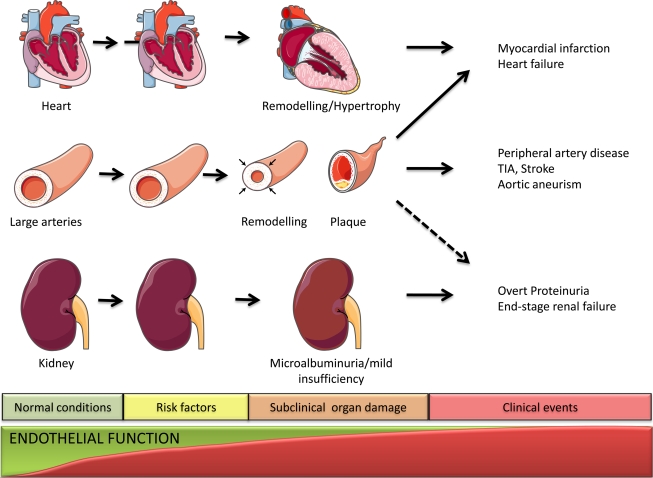
Another important aspect concerns the role of endothelial function in the progression of atherosclerotic lesions (Fig. 2). The importance of subclinical and clinical target organ damage is widely recognized and considered to profoundly influence patients' prognosis, as emphasized recently by the 2007 European Hypertension Guidelines, representing an intermediate stage in the continuum of vascular disease eventually leading to clinical events. The main relevant organ damage includes vascular atherosclerosis, detected by ultrasound scanning; left ventricular hypertrophy, assessed by electrocardiography or by echocardiography; and renal damage, on the basis of a reduced renal function and/or the detection of elevated urinary albumin excretion. These structural alterations have been linked by experimental evidence to the extent of endothelial dysfunction. In particular, increased intima-media thickness of the common carotid artery, which is a noninvasive marker of atherosclerosis and a predictor of coronary and cerebrovascular disease, was demonstrated to be directly related to the impairment of endothelial dysfunction in the forearm microcirculation of hypertensive patients (22) and in the brachial macrocirculation of patients with coronary atherosclerosis (23). The results of these small studies have also been confirmed in the large cohort of the Cardiovascular Risk in Young Finns Study. Indeed, the authors found that brachial artery FMD was inversely associated with intima-media thickness, also after adjusting for age, sex, brachial vessel size, and several risk variables (24). Finally, Rundek et al. (25) reported that endothelial dysfunction of the conduit artery, measured as brachial FMD, was independently associated to carotid plaque in a multi-ethnic population of elderly men and women (25). Apart from large cerebro-afferent arteries, intracerebral microcirculatory endothelial dysfunction, through the impairment of the blood-brain barrier, cerebral autoregulation, and prothrombotic changes, may also play a role in the genesis of brain infarct and in particular for the lacunar subtype. This type of lesion is particularly frequent in diabetic and hypertensive patients and represents a risk for the development of cognitive impairment and dementia. To date, no specific study evaluating the relationship between peripheral endothelial function and brain lesions has been performed. However, available data showed increased circulating markers of endothelial activation and damage, such as intercellular adhesion molecule-1, thrombomodulin, tissue factor, and tissue factor pathway inhibitor in patients with cerebral small vessel disease (26).
Figure 2.
Schematic representation of the cardiovascular continuum from normal physiologic condition (left) to the presence of cardiovascular risk factors, subclinical organ damage, and eventually cardiovascular, cerebrovascular, and renal events (right). The earliest vascular abnormality is represented by endothelial dysfunction, which potentially precedes established cardiovascular risk factors, and tends to worsen in parallel with aggravation of organ damage. TIA, transient ischemic attack.
A significant relationship between endothelial function and coronary atherosclerosis is also present. In patients with coronary artery stenosis, a selective impairment of endothelium-dependent vasodilation in coronary arteries was demonstrated, not only in diseased vessels, but also in nondiseased prestenotic arterial segments or vessels, and in the coronary microcirculation (3). In addition, in these patients, the endothelial dysfunction is not only present centrally, but also in the peripheral macro- and microcirculation (27). Notably, in patients without angiographic evidence of coronary atherosclerosis, the vasodilation to intracoronary acetylcholine, index of endothelial function, was found to be inversely related to the presence of intramural plaques, as detected by Brunner et al. (3). Moreover, in patients with coronary artery disease, the presence of a reduced coronary flow reserve is associated with a more pronounced impairment in microvascular endothelial function (28). These data are supported also by longitudinal studies. In a group of patients with heart transplants, the presence of coronary endothelial dysfunction at baseline was associated with a significant augmented risk of developing arteriolosclerosis at the 1-year follow-up, as well as atherosclerotic lesions (29). Overall, these results support the existence of a link between endothelial dysfunction and the probability of developing structural changes in the coronary and carotid circulation.
It is well known that the increase in left ventricular mass is able to independently predict an increased risk for cardiovascular disease, and regression of left ventricular hypertrophy has a positive prognostic impact (30). Available data suggest that left ventricular hypertrophy is associated with the presence of endothelial dysfunction, particularly if a concentric geometry is present, and a direct relationship between left ventricular mass and the vasodilation to intrabrachial acetylcholine was also described (21).
Target organ damage, other than large arteries and heart, also includes impairment in renal function. In particular, the loss of albumin in urine is considered a marker of impaired glomerular permeability for plasma proteins and represents an integrated marker of subclinical organ damage, both in hypertension and in diabetes. Accordingly, existing data show that the presence of microalbuminuria is an independent predictor of renal events, as well as cardiovascular mortality and morbidity after adjustment for other conventional cardiovascular risk factors (31). Interestingly, in the LIFE trial, the levels of albumin excretion at baseline were independent predictors of cardiovascular outcome also in nondiabetic hypertensive patients with left ventricular hypertrophy, as well as for range of albuminuria below the threshold to define microalbuminuria (32). The presence of reduced endothelial function has been demonstrated in diabetic patients with albuminuria compared with normoalbuminuric diabetic patients, or healthy subjects, and the level of albumin excretion is inversely related to endothelium-dependent response in several diabetic and nondiabetic populations (32). Both microalbuminuria and endothelial dysfunction are expressions of an endothelial pathology; however, it is still uncertain whether they are interrelated, or if the two phenomena are caused in parallel by the cardiovascular risk burden. Moreover, it is of note that some studies failed to demonstrate a relationship between microalbuminuria and endothelial dysfunction in hypertensive patients, either in the peripheral macrocirculation (33) and microcirculation (34). Taken together, these data seem to suggest either that no direct connection between systemic endothelial function and albumin excretion exists or that impaired endothelial function precedes the development of microalbuminuria.
Another important renal parameter is represented by reduced renal filtration. In the presence of profoundly impaired renal function, the high prevalence of traditional cardiovascular risk factors, as well as the activation of other several mechanisms reducing NO availability (35), leads to marked endothelial dysfunction (36), which is considered to be involved in the accelerated atherosclerotic process, and cardiovascular morbidity and mortality, which characterize patients with renal disease. Although, as noted, in advanced renal disease, endothelial dysfunction is constantly present and its degree is correlated to the degree of glomerular filtration rate decrease (36), the association between endothelial and renal function is still uncertain in the presence of mild renal insufficiency. Some scientific data support the concept that hypertension-related endothelial dysfunction, as detected also in the peripheral microcirculation, may independently favor the progressive reduction in glomerular filtration rate (37), although this association was not confirmed in patients with severe coronary atherosclerosis (38).
ENDOTHELIAL FUNCTION AND CLINICAL EVENTS
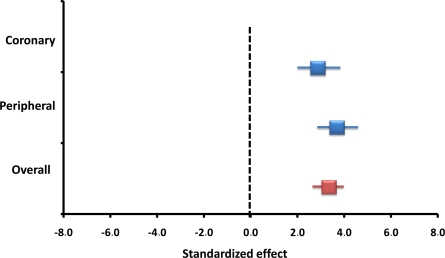
In recent years, a large body of evidence has been accumulating to support the hypothesis that the presence of endothelial dysfunction represents a major promoter for atherosclerosis and thrombosis and is an independent prognostic predictor for the risk of future cardiovascular events in several groups of patients (29,39) (Fig. 3). It is important to note that the vasodilating responses in different vascular zones of the same subject are poorly related (6), partly due to the different techniques and stimuli used and partially because of the highly specific regional regulation endothelial physiology. Despite this, the presence of endothelial dysfunction is almost invariably an independent predictor of clinical events wherever detected. Indeed, this prognostic role has been demonstrated in peripheral and central circulation, in microcirculation and large arteries, and independently from the used endothelial stimulus (3,29,39). It should, however, be emphasized that the total number of clinical events so far investigated is limited and does not allow definition of the presence of endothelial dysfunction as an independent risk factor for cardiovascular events, since it could potentially represent an integrated marker for global risk. Finally, some conflicting studies should be remembered: In a high-risk population, the presence of reduced FMD showed an association to the risk of cardiovascular events at follow-up, which was, however, not independent of major cardiovascular risk factors (40), and the coronary vasodilating response to acetylcholine may lose its predicting role in patients referring for a coronary angiogram (41).
Figure 3.
Meta-analysis of studies evaluating the association between coronary or peripheral endothelial function and cardiovascular events. Adapted from Lerman and Zeiher (39).
IS ENDOTHELIAL DYSFUNCTION RESOLVABLE?
Several nonpharmacological and pharmacological approaches have been demonstrated to improve or reverse endothelial dysfunction, although their effect is never selective and usually also target one or more traditional cardiovascular risk factors. Considering that oxidative stress is the main pathophysiologic mechanism leading to impaired NO bioavailability and endothelial dysfunction, immense attention has been drawn by antioxidant substances. Although in acute studies the use of high-dose antioxidant vitamins is extremely effective in restoring normal endothelial function, interventional studies using oral administration of these substances (i.e., vitamin C and E) failed to provide consistent data (42). However, recently, other antioxidant compounds, such as the flavonoids contained in red wine and chocolate, have been found to ameliorate endothelial function in peripheral large arteries (43), although it is difficult to evaluate the importance of their direct effect on the endothelium from the beneficial effect on blood pressure and lipid profile (43).
Among cardiovascular drugs, there is a large variability as far as their effect on endothelial function is concerned, depending on their mechanism of action and investigated vascular size and location (29). In particular, classic antihypertensive β-blockers and diuretics are invariably found to have little or no effect on endothelium-dependent vasodilation (29). An exception to this is represented by newer β-blockers. Nebivolol, indeed, is able to induce vasodilation by a direct effect on NO synthase and by its antioxidant effect (29), and carvedilol was found to suppress ROS generation and improve endothelial dysfunction (44). However, in general, newer drug classes are more effective in the protection of the endothelium. Specifically, calcium-channel blockers have been consistently shown to reverse impaired endothelium-dependent vasodilation, mainly in the microcirculation, with conflicting results in the brachial artery FMD (29). It is important to note that the beneficial effect of this class of drug is strictly related to its well-demonstrated antioxidant activity, which improves NO bioavailability and goes beyond its antihypertensive effect. Indeed, calcium-channel blockers are able to improve endothelial function in normotensive hypercholesterolemic patients as well, without affecting blood pressure or lipid levels (29). An entirely different scenario characterizes the renin-angiotensin system modulating drugs. In fact, both ACE inhibitors and angiotensin receptor blockers are characterized by several pleiotropic effects, including antioxidant and anti-inflammatory activities (45). Several mechanisms inducing endothelial dysfunction are certainly attributable to angiotensin II, such as superoxide and vasoconstricting prostanoid production and release of endothelin-1 (45). Accordingly, ACE inhibitors and angiotensin receptor blockers have been shown to ameliorate endothelium-dependent vasodilation in several experimental settings, exploring both coronary and peripheral large arteries (29,45), but conflicting results have been obtained in the microcirculation (29).
Statins represent another important cardiovascular drug class with proven beneficial effect in the primary and secondary prevention of cardiovascular events, independently of their lipid-lowering effect. Several ancillary properties of statins have been proposed to explain their beneficial excess, including their endothelium-protective action. The improvement of endothelial function by statin treatment is related to its ability to reduce LDL cholesterol levels and to partially increase HDL cholesterol (46). However, statins are able to improve endothelial function, even in the absence of any effect on lipid profile (47), and in populations with normal cholesterol levels, but distinguished by endothelial dysfunction, including smokers, hypertensive, and diabetic patients. This beneficial action on endothelial function may result as a consequence of various mechanisms, including the upregulation of eNOS expression, the enhanced NO release, their antioxidant activity, and the reduced expression and synthesis of endothelin-1 (46).
Also, glitazones (insulin-sensitizing agents used to treat patients with type 2 diabetes) have been found to have a protective and restoring effect on endothelial function. In randomized studies performed in diabetic patients, both rosiglitazone (48) and pioglitazone (49) were able to improve endothelial function compared with standard antidiabetic drugs. Similar results were obtained also in obese nondiabetic patients (50). These beneficial effects are the results of several pleiotropic actions of glitazones, including the ability to reduce levels of asymmetric dimethylarginine (51), a competitive inhibitor of eNOS, to decrease ROS production and inhibit vascular inflammation (52).
IS THE CORRECTION OF ENDOTHELIAL FUNCTION CLINICALLY RELEVANT?
Given these data, it is conceivable that the therapeutic correction of endothelial dysfunction may lead to an improvement of prognosis in patients with cardiovascular risk factors or cardiovascular disease. However, scant data are available on this topic, and most of the conclusions that can be drawn are highly speculative. There is, therefore, virtually no available substance able to specifically target the endothelium; moreover, the results of interventional studies evaluating the effect of cardiovascular drugs on endothelial function vary, depending on the investigated vascular zone and technique and stimulus used.
To date, only one study (53) evaluated the correctional effect of endothelial dysfunction in terms of cardiovascular risk events. A group of postmenopausal hypertensive women with impaired endothelial function, assessed by brachial artery FMD, was treated with antihypertensive drugs and followed up for >5 years. In the subgroup that experienced amelioration of endothelial function within 6 months from the onset of treatment, the long-term outcome was found significantly better compared with the subgroup without improvement in FMD, with a lower rate of cardiovascular events, despite similar reduction in blood pressure (53). These results support the concept that the amelioration of endothelial dysfunction is potentially a powerful tool to reduce cardiovascular risk. Moreover, it can be speculated that among cardiovascular drugs, the ones with the ancillary property of improving endothelial function are possibly preferable in the treatment of risk factors.
An argument against this may be a derivative of evidence arising from controlled clinical trials on the use of lipid-lowering agents (54). Antihypertensive drugs (55) have clearly demonstrated that the benefit is virtually entirely attributable to the magnitude of cholesterol and lowering of blood pressure, respectively. Moreover, a meta-analysis showed no difference among antihypertensive drugs in improving patient prognosis (56), suggesting the reduction in blood pressure as the only clinically important effect of these drugs. It should be considered, however, that the duration of controlled clinical trials is usually 4–5 years, and this may be insufficient to detect additional benefit of some drug classes, especially in low-risk patients. Another aspect to consider is that of the definition of endothelial function. The endothelium embodies several activities contributing to vascular protection beyond vasodilation, including inhibition of platelet aggregation, smooth muscle cell proliferation, and vascular inflammation. The use of “endothelial function” (which is defined only on vasoreactivity) as an ancillary target for therapy, may in this sense not be completely correct, since it is possible that drugs improving endothelium-dependent vasodilation may potentially increase platelet aggregation or inflammation, such as the case for exogenous estrogen (57–59).
CONCLUSIONS
There is no doubt that the structural and functional integrity of the endothelium is crucial to maintain vascular homeostasis and prevent atherosclerosis. This, as mentioned, is documented by the increased risk of developing target organ damage and cardiovascular events in the presence of endothelial dysfunction. So far, several cardiovascular drugs have been shown to improve compromised endothelial function through supposed pleiotropic and/or ancillary properties. However, it is difficult to highlight the direct effect on endothelium against the indirect effect of the specific drugs, such as the blood pressure–lowering, lipid-lowering, or insulin sensitivity–improving effect. Nonetheless, the endothelium is increasingly becoming a surrogate end point of the therapeutic approach to cardiovascular risk, as demonstrated by its inclusion among markers of organ damage in the latest European hypertension guidelines (55). Although it is possible that endothelial dysfunction is only a marker of cardiovascular risk, in the clinical practice, the development of a technique to easily and noninvasively explore endothelial function at a low cost will afford a reliable index of the effectiveness of patients' cardiovascular therapy.
Acknowledgments
No potential conflicts of interest relevant to this article were reported.
Footnotes
The publication of this supplement was made possible in part by unrestricted educational grants from Eli Lilly, Ethicon Endo-Surgery, Generex Biotechnology, Hoffmann-La Roche, Johnson & Johnson, LifeScan, Medtronic, MSD, Novo Nordisk, Pfizer, sanofi-aventis, and WorldWIDE.
References
- 1. Luscher TF, Vanhoutte PM: The Endothelium: Modulator of Cardiovascular Function. Boca Raton, FL, CRC Press, 1990 [Google Scholar]
- 2. Taddei S, Ghiadoni L, Virdis A, Versari D, Salvetti A: Mechanisms of endothelial dysfunction: clinical significance and preventive non-pharmacological therapeutic strategies. Curr Pharm Des 2003; 9: 2385– 2402 [DOI] [PubMed] [Google Scholar]
- 3. Brunner H, Cockcroft JR, Deanfield J, Donald A, Ferrannini E, Halcox J, Kiowski W, Luscher TF, Mancia G, Natali A, Oliver JJ, Pessina AC, Rizzoni D, Rossi GP, Salvetti A, Spieker LE, Taddei S, Webb DJ: Endothelial function and dysfunction. Part II: Association with cardiovascular risk factors and diseases: a statement by the Working Group on Endothelins and Endothelial Factors of the European Society of Hypertension. J Hypertens 2005; 23: 233– 246 [DOI] [PubMed] [Google Scholar]
- 4. Deanfield J, Donald A, Ferri C, Giannattasio C, Halcox J, Halligan S, Lerman A, Mancia G, Oliver JJ, Pessina AC, Rizzoni D, Rossi GP, Salvetti A, Schiffrin EL, Taddei S, Webb DJ: Endothelial function and dysfunction. Part I: Methodological issues for assessment in the different vascular beds: a statement by the Working Group on Endothelin and Endothelial Factors of the European Society of Hypertension. J Hypertens 2005; 23: 7– 17 [DOI] [PubMed] [Google Scholar]
- 5. John S, Schmieder RE: Impaired endothelial function in arterial hypertension and hypercholesterolemia: potential mechanisms and differences. J Hypertens 2000; 18: 363– 374 [DOI] [PubMed] [Google Scholar]
- 6. Anderson TJ, Uehata A, Gerhard MD, Meredith IT, Knab S, Delagrange D, Lieberman EH, Ganz P, Creager MA, Yeung AC, et al. : Close relation of endothelial function in the human coronary and peripheral circulations. J Am Coll Cardiol 1995; 26: 1235– 1241 [DOI] [PubMed] [Google Scholar]
- 7. Mohanty P, Ghanim H, Hamouda W, Aljada A, Garg R, Dandona P: Both lipid and protein intakes stimulate increased generation of reactive oxygen species by polymorphonuclear leukocytes and mononuclear cells. Am J Clin Nutr 2002; 75: 767– 772 [DOI] [PubMed] [Google Scholar]
- 8. Mohanty P, Hamouda W, Garg R, Aljada A, Ghanim H, Dandona P: Glucose challenge stimulates reactive oxygen species (ROS) generation by leucocytes. J Clin Endocrinol Metab 2000; 85: 2970– 2973 [DOI] [PubMed] [Google Scholar]
- 9. Vogel RA, Corretti MC, Plotnick GD: Effect of a single high-fat meal on endothelial function in healthy subjects. Am J Cardiol 1997; 79: 350– 354 [DOI] [PubMed] [Google Scholar]
- 10. Tripathy D, Mohanty P, Dhindsa S, Syed T, Ghanim H, Aljada A, Dandona P: Elevation of free fatty acids induces inflammation and impairs vascular reactivity in healthy subjects. Diabetes 2003; 52: 2882– 2887 [DOI] [PubMed] [Google Scholar]
- 11. Calles-Escandon J, Cipolla M: Diabetes and endothelial dysfunction: a clinical perspective. Endocr Rev 2001; 22: 36– 52 [DOI] [PubMed] [Google Scholar]
- 12. Baron AD, Brechtel G: Insulin differentially regulates systemic and skeletal muscle vascular resistance. Am J Physiol 1993; 265: E61– E67 [DOI] [PubMed] [Google Scholar]
- 13. Clerk LH, Vincent MA, Lindner JR, Clark MG, Rattigan S, Barrett EJ: The vasodilatory actions of insulin on resistance and terminal arterioles and their impact on muscle glucose uptake. Diabete Metab Res Rev 2004; 20: 3– 12 [DOI] [PubMed] [Google Scholar]
- 14. Muniyappa R, Iantorno M, Quon MJ: An integrated view of insulin resistance and endothelial dysfunction. Endocrinol Metab Clin North Am 2008; 37: 685– 711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Aljada A, Dandona P: Effect of insulin on human aortic endothelial nitric oxide synthase. Metabolism 2000; 49: 147– 150 [DOI] [PubMed] [Google Scholar]
- 16. Mather K, Laakso M, Edelman S, Hook G, Baron A: Evidence for physiological coupling of insulin-mediated glucose metabolism and limb blood flow. Am J Physiol Endocrinol Metab 2000; 279: E1264– E1270 [DOI] [PubMed] [Google Scholar]
- 17. Taddei S, Virdis A, Mattei P, Natali A, Ferrannini E, Salvetti A: Effect of insulin on acetylcholine-induced vasodilation in normotensive subjects and patients with essential hypertension. Circulation 1995; 92: 2911– 2918 [DOI] [PubMed] [Google Scholar]
- 18. Paradisi G, Steinberg HO, Hempfling A, Cronin J, Hook G, Shepard MK, Baron AD: Polycystic ovary syndrome is associated with endothelial dysfunction. Circulation 2001; 103: 1410– 1415 [DOI] [PubMed] [Google Scholar]
- 19. Vita JA, Treasure CB, Nabel EG, McLenachan JM, Fish RD, Yeung AC, Vekshtein VI, Selwyn AP, Ganz P: Coronary vasomotor response to acetylcholine relates to risk factors for coronary artery disease. Circulation 1990; 81: 491– 497 [DOI] [PubMed] [Google Scholar]
- 20. Rossi R, Chiurlia E, Nuzzo A, Cioni E, Origliani G, Modena MG: Flow-mediated vasodilation and the risk of developing hypertension in healthy postmenopausal women. J Am Coll Cardiol 2004; 44: 1636– 1640 [DOI] [PubMed] [Google Scholar]
- 21. Rossi R, Cioni E, Nuzzo A, Origliani G, Modena MG: Endothelial-dependent vasodilation and incidence of type 2 diabetes in a population of healthy postmenopausal women. Diabetes Care 2005; 28: 702– 707 [DOI] [PubMed] [Google Scholar]
- 22. Ghiadoni L, Taddei S, Virdis A, Sudano I, Di Legge V, Meola M, Di Venanzio L, Salvetti A: Endothelial function and common carotid artery wall thickening in patients with essential hypertension. Hypertension 1998; 32: 25– 32 [DOI] [PubMed] [Google Scholar]
- 23. Hashimoto M, Eto M, Akishita M, Kozaki K, Ako J, Iijima K, Kim S, Toba K, Yoshizumi M, Ouchi Y: Correlation between flow-mediated vasodilatation of the brachial artery and intima-media thickness in the carotid artery in men. Arterioscler Thromb Vasc Biol 1999; 19: 2795– 2800 [DOI] [PubMed] [Google Scholar]
- 24. Juonala M, Viikari JS, Laitinen T, Marniemi J, Helenius H, Ronnemaa T, Raitakari OT: Interrelations between brachial endothelial function and carotid intima-media thickness in young adults: the cardiovascular risk in young Finns study. Circulation 2004; 110: 2918– 2923 [DOI] [PubMed] [Google Scholar]
- 25. Rundek T, Hundle R, Ratchford E, Ramas R, Sciacca R, Di Tullio MR, Boden-Albala B, Miyake Y, Elkind MS, Sacco RL, Homma S: Endothelial dysfunction is associated with carotid plaque: a cross-sectional study from the population based Northern Manhattan Study. BMC Cardiovasc Disord 2006; 6: 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hassan A, Markus HS: Genetics and ischaemic stroke. Brain 2000; 123: 1784– 1812 [DOI] [PubMed] [Google Scholar]
- 27. Behrendt D, Ganz P: Endothelial function: from vascular biology to clinical applications. Am J Cardiol 2002; 90: 40L– 48L [DOI] [PubMed] [Google Scholar]
- 28. Zeiher AM, Krause T, Schachinger V, Minners J, Moser E: Impaired endothelium-dependent vasodilation of coronary resistance vessels is associated with exercise-induced myocardial ischemia. Circulation 1995; 91: 2345– 2352 [DOI] [PubMed] [Google Scholar]
- 29. Taddei S, Virdis A, Ghiadoni L, Sudano I, Salvetti A: Effects of antihypertensive drugs on endothelial dysfunction: clinical implications. Drugs 2002; 62: 265– 284 [DOI] [PubMed] [Google Scholar]
- 30. Verdecchia P, Angeli F, Borgioni C, Gattobigio R, de Simone G, Devereux RB, Porcellati C: Changes in cardiovascular risk by reduction of left ventricular mass in hypertension: a meta-analysis. Am J Hypertens 2003; 16: 895– 899 [DOI] [PubMed] [Google Scholar]
- 31. Ochodnicky P, Henning RH, van Dokkum RP, de Zeeuw D: Microalbuminuria and endothelial dysfunction: emerging targets for primary prevention of end-organ damage. J Cardiovasc Pharmacol 2006; 47 ( Suppl. 2): S151– S162 [DOI] [PubMed] [Google Scholar]
- 32. Wachtell K, Ibsen H, Olsen MH, Borch-Johnsen K, Lindholm LH, Mogensen CE, Dahlof B, Devereux RB, Beevers G, de Faire U, Fyhrquist F, Julius S, Kjeldsen SE, Kristianson K, Lederballe-Pedersen O, Nieminen MS, Okin PM, Omvik P, Oparil S, Wedel H, Snapinn SM, Aurup P: Albuminuria and cardiovascular risk in hypertensive patients with left ventricular hypertrophy: the LIFE study. Ann Intern Med 2003; 139: 901– 906 [DOI] [PubMed] [Google Scholar]
- 33. Diercks GF, Stroes ES, van Boven AJ, van Roon AM, Hillege HL, de Jong PE, Smit AJ, Gans RO, Crijns HJ, Rabelink TJ, van Gilst WH: Urinary albumin excretion is related to cardiovascular risk indicators, not to flow-mediated vasodilation, in apparently healthy subjects. Atherosclerosis 2002; 163: 121– 126 [DOI] [PubMed] [Google Scholar]
- 34. Taddei S, Virdis A, Mattei P, Ghiadoni L, Sudano I, Arrighi P, Salvetti A: Lack of correlation between microalbuminuria and endothelial function in essential hypertensive patients. J Hypertens 1995; 13: 1003– 1008 [DOI] [PubMed] [Google Scholar]
- 35. Schiffrin EL, Lipman ML, Mann JF: Chronic kidney disease: effects on the cardiovascular system. Circulation 2007; 116: 85– 97 [DOI] [PubMed] [Google Scholar]
- 36. Ghiadoni L, Cupisti A, Huang Y, Mattei P, Cardinal H, Favilla S, Rindi P, Barsotti G, Taddei S, Salvetti A: Endothelial dysfunction and oxidative stress in chronic renal failure. J Nephrol 2004; 17: 512– 519 [PubMed] [Google Scholar]
- 37. Perticone F, Maio R, Tripepi G, Zoccali C: Endothelial dysfunction and mild renal insufficiency in essential hypertension. Circulation 2004; 110: 821– 825 [DOI] [PubMed] [Google Scholar]
- 38. van der Harst P, Smilde TD, Buikema H, Voors AA, Navis G, van Veldhuisen DJ, van Gilst WH: Vascular function and mild renal impairment in stable coronary artery disease. Arterioscler Thromb Vasc Biol 2006; 26: 379– 384 [DOI] [PubMed] [Google Scholar]
- 39. Lerman A, Zeiher AM: Endothelial function: cardiac events. Circulation 2005; 111: 363– 368 [DOI] [PubMed] [Google Scholar]
- 40. Fathi R, Haluska B, Isbel N, Short L, Marwick TH: The relative importance of vascular structure and function in predicting cardiovascular events. J Am Coll Cardiol 2004; 43: 616– 623 [DOI] [PubMed] [Google Scholar]
- 41. Asselbergs FW, Monnink SH, Jessurun GA, van Boven AJ, Veeger NJ, Zijlstra F, van Gilst WH, Tio RA: Assessing the prognostic value of coronary endothelial function in patients referred for a first coronary angiogram. Am J Cardiol 2004; 94: 1063– 1067 [DOI] [PubMed] [Google Scholar]
- 42. Virdis A, Ghiadoni L, Salvetti G, Versari D, Taddei S, Salvetti A: Endothelial dysfunction, vascular damage and clinical events: role of antioxidant therapy. High Blood Press Cardiovasc Prev 2004; 11: 15– 27 [Google Scholar]
- 43. Grassi D, Necozione S, Lippi C, Croce G, Valeri L, Pasqualetti P, Desideri G, Blumberg JB, Ferri C: Cocoa reduces blood pressure and insulin resistance and improves endothelium-dependent vasodilation in hypertensives. Hypertension 2005; 46: 398– 405 [DOI] [PubMed] [Google Scholar]
- 44. Matsuda Y, Akita H, Terashima M, Shiga N, Kanazawa K, Yokoyama M: Carvedilol improves endothelium-dependent dilatation in patients with coronary artery disease. Am Heart J 2000; 140: 753– 759 [DOI] [PubMed] [Google Scholar]
- 45. Bohm M: Angiotensin receptor blockers versus angiotensin-converting enzyme inhibitors: where do we stand now? Am J Cardiol 2007; 100: 38J– 44J [DOI] [PubMed] [Google Scholar]
- 46. Beckman JA, Creager MA: The nonlipid effects of statins on endothelial function. Trends Cardiovasc Med 2006; 16: 156– 162 [DOI] [PubMed] [Google Scholar]
- 47. Beckman JA, Liao JK, Hurley S, Garrett LA, Chui D, Mitra D, Creager MA: Atorvastatin restores endothelial function in normocholesterolemic smokers independent of changes in low-density lipoprotein. Circ Res 2004; 95: 217– 223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Natali A, Baldeweg S, Toschi E, Capaldo B, Barbaro D, Gastaldelli A, Yudkin JS, Ferrannini E: Vascular effects of improving metabolic control with metformin or rosiglitazone in type 2 diabetes. Diabetes Care 2004; 27: 1349– 1357 [DOI] [PubMed] [Google Scholar]
- 49. Papathanassiou K, Naka KK, Kazakos N, Kanioglou C, Makriyiannis D, Pappas K, Katsouras CS, Liveris K, Kolettis T, Tsatsoulis A, Michalis LK: Pioglitazone vs glimepiride: differential effects on vascular endothelial function in patients with type 2 diabetes. Atherosclerosis 2009; 205: 221– 226 [DOI] [PubMed] [Google Scholar]
- 50. Garg R, Kumbkarni Y, Aljada A, Mohanty P, Ghanim H, Hamouda W, Dandona P: Troglitazone reduces reactive oxygen species generation by leukocytes and lipid peroxidation and improves flow-mediated vasodilatation in obese subjects. Hypertension 2000; 36: 430– 435 [DOI] [PubMed] [Google Scholar]
- 51. Stuhlinger MC, Abbasi F, Chu JW, Lamendola C, McLaughlin TL, Cooke JP, Reaven GM, Tsao PS: Relationship between insulin resistance and an endogenous nitric oxide synthase inhibitor. JAMA 2002; 287: 1420– 1426 [DOI] [PubMed] [Google Scholar]
- 52. Ceriello A: Thiazolidinediones as anti-inflammatory and anti-atherogenic agents. Diabete Metab Res Rev 2008; 24: 14– 26 [DOI] [PubMed] [Google Scholar]
- 53. Modena MG, Bonetti L, Coppi F, Bursi F, Rossi R: Prognostic role of reversible endothelial dysfunction in hypertensive postmenopausal women. J Am Coll Cardiol 2002; 40: 505– 510 [DOI] [PubMed] [Google Scholar]
- 54. Baigent C, Keech A, Kearney PM, Blackwell L, Buck G, Pollicino C, Kirby A, Sourjina T, Peto R, Collins R, Simes R: Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet 2005; 366: 1267– 1278 [DOI] [PubMed] [Google Scholar]
- 55. Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, Grassi G, Heagerty AM, Kjeldsen SE, Laurent S, Narkiewicz K, Ruilope L, Rynkiewicz A, Schmieder RE, Boudier HA, Zanchetti A, Vahanian A, Camm J, De Caterina R, Dean V, Dickstein K, Filippatos G, Funck-Brentano C, Hellemans I, Kristensen SD, McGregor K, Sechtem U, Silber S, Tendera M, Widimsky P, Zamorano JL, Erdine S, Kiowski W, Agabiti-Rosei E, Ambrosioni E, Lindholm LH, Viigimaa M, Adamopoulos S, Agabiti-Rosei E, Ambrosioni E, Bertomeu V, Clement D, Erdine S, Farsang C, Gaita D, Lip G, Mallion JM, Manolis AJ, Nilsson PM, O'Brien E, Ponikowski P, Redon J, Ruschitzka F, Tamargo J, van Zwieten P, Waeber B, Williams B: 2007 Guidelines for the Management of Arterial Hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2007; 25: 1105– 1187 [DOI] [PubMed] [Google Scholar]
- 56. Turnbull F: Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet 2003; 362: 1527– 1535 [DOI] [PubMed] [Google Scholar]
- 57. Virdis A, Ghiadoni L, Pinto S, Lombardo M, Petraglia F, Gennazzani A, Buralli S, Taddei S, Salvetti A: Mechanisms responsible for endothelial dysfunction associated with acute estrogen deprivation in normotensive women. Circulation 2000; 101: 2258– 2263 [DOI] [PubMed] [Google Scholar]
- 58. Maeso R, Navarro-Cid J, Munoz-Garcia R, Rodrigo E, Ruilope LM, Lahera V, Cachofeiro V: Losartan reduces phenylephrine constrictor response in aortic rings from spontaneously hypertensive rats: role of nitric oxide and angiotensin II type 2 receptors. Hypertension 1996; 28: 967– 972 [DOI] [PubMed] [Google Scholar]
- 59. Caine YG, Bauer KA, Barzegar S, ten Cate H, Sacks FM, Walsh BW, Schiff I, Rosenberg RD: Coagulation activation following estrogen administration to postmenopausal women. Thromb Haemost 1992; 68: 392– 395 [PubMed] [Google Scholar]