DEBATE
The integration of continuous subcutaneous insulin infusion (CSII) (insulin pump therapy) and continuous interstitial glucose monitoring (CGM) appears to be an excellent solution for obtaining the desirable metabolic control for most insulin-treated subjects (1–4). Several studies have suggested that CGM with readings in real-time (CGM-RT) further improves blood glucose control (5–9). The introduction of CGM and CSII into clinical practice has generated an inevitable increase in the amount of data to be managed and interpreted. Telemedicine facilitates data management and preprocessing to optimize therapy. Among other potential benefits, telemedicine improves communication among patients and health care providers, improves quantity and quality of data collection, and eases decision-making and therapy adjustment (10–12). DIABTel, a web-based telemedicine system, is a good example for a solution designed to supply these needs (13).
PARIS (Páncreas Artificial Telemédico Inteligente) is a coordinated research project to develop and validate a telemedical artificial pancreas (TAP), a multi-access telemedicine system that integrates CGM-RT, insulin pump, a smart assistant (SA), and close-loop control algorithms. SA is a personal intelligent assistant based on a handheld digital device to provide both personal and remote loop strategies, using CGM, CSII, and mobile general packet radio service (GPRS) communication with a telemedicine central server (TMCS).
This review summarizes acquired experiences with TAP, integrating these new technologies with the objective to improve glycemic control of type 1 diabetic patients.
RESEARCH DESIGN AND METHODS
Description of the DIABTel telemedicine system
The telemedicine architecture consists of two components: the medical unit (a telemedical central server) and the patient unit (a smart assistant).
The TMCS at the diabetes center of the hospital continuously runs, receiving and processing patients' monitoring data, messages, and requests for professional advice. A previous publication already reported the benefits of DIABTel, allowing the implementation of an easy-to-use, user-tailored telemedicine system with a technological platform allowing tight integration between multi-access modalities (web, phone, palmtop) for diabetes management (14).
DIABTel provides the information for patient management and support for decision-making through the facilities of four main services: telemonitoring of main parameters of diabetes care (blood glucose, diet, insulin doses, physical activity, severe hypoglycemia, ketonuria, sick days), telecare (consultation and supervision), remote information access, and knowledge management tools. In previous experiences, DIABTel was effective, improving patient-doctor interaction, data display, and patient's confidence in self-management by constant professional supervision (15,16).
The SA supports both personal and remote-control strategies supervised by health care professionals through the TMCS. The transfer of information can be activated by the patient at any time through the mobile patient unit, a GPRS-based SA that supports personal and remote control strategies for patients, supervised by physicians through the telemedicine system. The SA architecture includes functionalities for data management: electronic logbook, rule-based reasoning methodology in decision support (17,18), advice generation by relying on a diabetic patient simulator, e-mail facility, and visualization. The blood glucose measurement edition includes specific time of measurement and time intervals between measurements. Monitoring data stored at the TMCS can be downloaded to the SA database through the synchronization process and vice versa. The multiparametric graphic scenario displays a quick overview of the patient's metabolic status, providing information of interest and supporting the decision-making process; variables such as blood glucose, diet, and administered doses of insulin can be shown.
SA may also allow communication with different medical devices (glucose sensing, insulin pump) for automatic download.
Operation of TAP
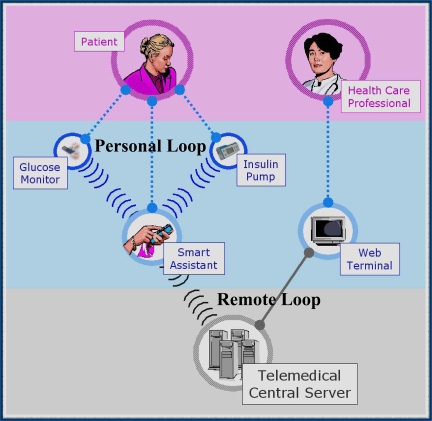
TAP is built in two interlinked loops. The “personal loop” allows wireless communication between the SA, the insulin pump, and the CGM device. The “remote loop” connects the diabetic subject to the health care professional via the SA and its wireless connection to the TMCS. The SA platform consists of several systems (user interface, data access, communication devices, model predictive control, and TCMS modules) (Fig. 1). The model predictive control module calculates the modification of the continuous insulin infusion rate provided by the pump, following the physiological model of Hovorka (19) The platform implies two control modes: 1) the patient decides changes in the insulin pump program by using the information coming from the glucosensor (free mode), and 2) the patient gets advice, through the SA, on the insulin bolus before each meal (advisory mode). The patient uses the SA to register and transfer data related to timing and pre- and postprandial glucose levels, amount of ingested carbohydrates, and additional relevant information (e.g., previous physical exercise). From this information, the algorithm computes corresponding insulin dose, which has to be approved by the physician through the Web interface, before it is shown to the patient. The analysis and design is based on the MOSAIK-M (modeling, simulation, and animation of information and communication systems in medicine) system model (20). The patient uses the SA to get results of the proposed insulin bolus and decides to follow it or not.
Figure 1.
PARIS Research Project. TAP integrates an SA based on a handheld personal digital assistant (PDA) to provide patients with closed-loop control strategies (personal and remote loop), based on real-time CGM, CSII (insulin pump), and a mobile GPRS-based telecommunication. The patient decides on the changes in the insulin pump programming, using the information coming from a glucose sensor. The physician suggests changes in the insulin program, using the information provided by the CGM and from the CSII, coming from the personal smart assistant (PSA) through the TMCS. Close-loop algorithms implemented in the PSA provide a real-time control of the insulin pump based on glucose sensor data.
The TAP has been evaluated by a research consortium funded by the European Commission: The Intelligent Control Assistant for Diabetes (INCA Project), introducing the concept, design, and preliminary evaluation of a mobile close-loop system for diabetes management. A feasibility pilot was carried out in a group of type 1 pump-treated diabetic patients investigated at the Institut für Diabetesforschung (München, Germany), with satisfactory outcomes in ambulatory scenarios (21).
CLINICAL EVALUATION OF TAP
Various clinical experiences have been designed to investigate the clinical impact of the telemedical artificial pancreas in “real life.” So far, two randomized crossover ambulatory clinical studies have been carried out. Clinical study 1 focused to evaluate the results of the original web-based telemedicine system. Clinical study 2 evaluated the impact of CGM-RT, together with a telemedicine system.
Clinical study 1: Evaluation of a telemedicine system that includes an SA
A comprehensive full description of the trial is available (22).
Design and methods.
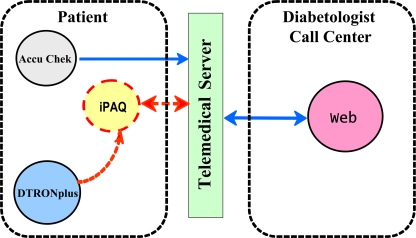
The local ethical committee approved the protocol and patients signed the informed consent. Ten insulin pump–treated (for more than 1 year) type 1 diabetic subjects (five women), mean age 40.6 years (range 21–62 years), diabetes duration 14.7 years (3–52), C-peptide negative, and A1C <10%, were randomized into intervention versus control groups and crossed over to alternate arm after 4 weeks. During the intervention phase, patients were assisted by telemedicine (DIABTel System). All subjects were instructed in the use of the DIABTel web service, the management of the SA (a commercial handheld digital assistant; iPAQHP2210 pocket PC, Palo Alto, CA) provided with wireless communication facilities, such as infrared, Bluetooth, and GPRS. Patients were requested to submit blood glucose levels directly from a conventional glucose monitor (Accu-Chek, Accutrend, and Acculink modem; Roche Diagnostics, Basel, Switzerland) and insulin treatment data at least twice a week. In the control phase, patients only used the conventional glucose monitor plus modem for sending data, without any feedback from the diabetes center. In the intervention phase, patients were assisted by telemedicine (DIABTel System) (Fig. 2). Confidentiality was guaranteed through data encryption, using the Secure Locket Layer protocol; patients' names were coded when interacting with the website. The system notified doctors with predefined alarm messages for out-of-range glucose values. After analyzing data sent by patients, modifications of insulin basal rate and boluses were advised when necessary by heath care professionals; all exchanged messages were automatically registered by the DIABTel System. A1C was measured by ion-exchange high-pressure liquid chromatography (Bio-Rad VARIANT II; Bio-Rad laboratories, München, Germany), with a reference range of 4.2–5.7%. Fructosamine was measured by a colorimetric assay system (nitroblue tetrazolium method), provided by BioSystems (Barcelona, Spain); the reference range was 205–285 μmol/l (interassay coefficient of variation 3% at 281 μmol/l and 4% at 531 μmol/l). In the last 72 h of each phase, CGM was performed (CGMS; Minimed Medtronic, Northridge, CA). A group of variables were compared (mean glucose, SD, percentage of time >180 mg/dl, and area under the curve >180 mg/dl) using data provided by the software CGM Sensor 3.0 (Minimed, Medtronic). SPSS 14 package for Windows (SPSS, Chicago, IL) was used for the comparison between groups (Student's t for Gaussian distribution, Mann-Whitney's U test for non-Gaussian distribution, for quantitative data; χ2 for qualitative variables). For comparisons within a group, Student's t paired or Wilcoxon's test were used. Bivariate correlations between continuous data were carried out by Spearman's ρ.
Figure 2.
PARIS clinical study 1. The main objective of the study was to evaluate clinical utilities of the telemedicine system (DIABTel) that includes an SA (iPAQ), provided with wireless communication facilities. In the control phase, type 1 diabetic patients directly submitted blood glucose levels from a conventional glucose monitor (Accuchek, Acculink modem) and insulin data to the diabetes center without any feedback. In the experimental phase, patients were assisted by telemedicine (DiabTel) System.
Main results.
During the intervention phase, fructosamine decreased from 393 ± 32 to 366 ± 25 μmol/l (P < 0.05), whereas no change was observed during the control phase. A1C tended to decrease after the active phase (from 8.0 ± 0.6 to 7.78 ± 0.6%; P < 0.073) but did not change during the control phase. The number of treatment modifications prescribed by the physician and carried out by the patients correlated with the change observed in A1C during the telecare phase (r = −0.729, P = 0.017). Eight of ten patients reduced the percentage of home blood glucose values >180 mg/dl during the intervention phase, with the total group mean reduction being 16.6%. The percentage of blood glucose values <65 mg/dl was reduced in 29.6%.
Clinical study 2: Evaluation of the clinical impact of CGM-RT with a telemedicine system
A comprehensive full description of the trial is available (23). The aim of the study was to evaluate the impact of the use of real-time CGM together with a telemedicine system in A1C and glucose variability in insulin pump–treated type 1 diabetic patients.
Design and methods.
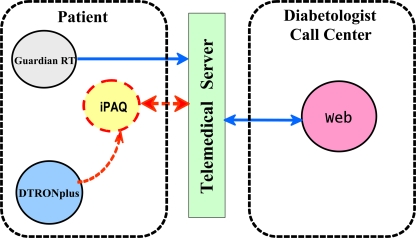
Ten insulin pump–treated (D-tron plus; Disetronic, Burgdorf, Switzerland) type 1 diabetic patients (five women), mean age 41.2 years (range 21–62), duration of diabetes 14.9 years (3–52), were randomized in a crossover study with two phases of 4 weeks' duration each, with an interim washout period of 6 weeks. Interaction between patients and health care professionals was supported by the DIABTel System. Real-time CGM data (Guardian RT, Medtronic Minimed) was used 3 days per week during the experimental phase. A 72-h masked CGM registry (CGM System Gold, Medtronic Minimed, Northridge, CA) was carried out at the end of the control phase. Monitoring data were retrieved directly from the pump, and the Accutrend glucose monitor (Boehringer Mannheim, Germany) and Acculink modem (Roche Diagnostics, Basel, Switzerland) were available on the web and the patient SA (iPAQ HP2210 pocket PC), which communicates with the DIABTel server (mobile GPRS Wide Area Network) (Fig. 3). Within the 24-h period after data reception, physicians analyzed patients' data and advised treatment changes, when necessary. A1C was measured by ion-exchange high-performance liquid chromatography (VARIANT II, Bio-Rad), with a reference range of 4.2–5.7%. Statistical analyses were performed using SPSS v 14.0. Comparisons were made using nonparametric tests for paired data (Wilcoxon's test). The study had been previously approved by the local ethics committee, and all patients signed the informed consent form. To assess glucose variability, glucose risk index was calculated to assess glucose variability (24–27).
Figure 3.
PARIS clinical study 2. The study evaluated the clinical impact of the combined use of real-time CGM (Guardian RT) together with telemedicine in insulin pump–treated (DTRON plus) type 1 diabetic subjects, integrated in the TAP. Insulin data were retrieved directly from the DTRON, plus insulin pump real-time CGM was used 3 days per week during the experimental phase. SMBG was used at all other times during both control and experimental phases. Data were available on the web and the patient's SA (iPAQ), which communicated with the DiabTel server.
Results.
The local ethical committee approved the protocol and patients signed the informed consent; all patients completed the study. At the end of the intervention phase, A1C decreased in 9 of 10 patients, with a mean decrease of 0.8% (8.1 ± 1.1 vs. 7.3 ± 0.8%; P = 0.007); no change was observed during the control phase. The change in A1C observed during the intervention phase was higher than in the control phase (P = 0.017). Data from real-time CGM depicted that the percentage of glucose values between 70 and 180 mg/dl was higher during the intervention phase (62 vs. 52%; P < 0.05), without differences in the percentage of values below 70 mg/dl. The glucose risk index obtained from the CGM was higher during the control phase than that obtained by aggregation of the four monitoring sessions performed during the intervention phase (9.6 vs. 6.25; P < 0.05), which suggests an improvement in glucose stability. The number of insulin bolus doses per day was higher on those days patients wore the continuous glucose monitor (5.64 ± 1.7 vs. 4.90 ± 0.96). The DIABTel System was more frequently used during the experimental phase, particularly logbook visualization (19.5 ± 9.4 vs. 8.5 ± 4.8 times per patient per week; P < 0.01).
CONCLUSIONS
Self-monitoring of blood glucose (SMBG) is considered a standard of care in diabetes management (28). As previously demonstrated for type 1 diabetes (29–32), the clinical benefit of SMBG in type 2 diabetes is widely accepted, with independence from the recommended type of antidiabetic treatment (33–37). Responsible use of SMBG requires adequate training and skill performance by the patient (38). A1C, SMBG, mean blood glucose, and glucose variability measurements should be considered together, complementing the information on good and bad control, as well as the risk for hypoglycemia. Experiences including subjects with normal glucose tolerance, glucose intolerance, and diabetes, using SMBG in conjunction with CGM, investigated for up to 75 days, showed the same correlations with A1C and glucose level variability (after adding the SD to the model). Nevertheless, glucose profiles generated from either SMBG or CGM showed that identical A1C at different stratified levels produced different and unpredictable diurnal patterns. Although CGM still remains experimental, it permits recognition of the diurnal modal profile in ambulatory observation for extended periods, which may be linked to diabetes complications (39).
CGM is still a clinically experimental, invasive (although minimally), rather cumbersome alternative to SMBG, requiring the periodic change of the indwelling sensor (40). A dynamic picture of the glucose profile is provided by the CGM, as well as the direction and speed of its movement (41). Fasting glucose levels correlate better with A1C, and it is not a good indicator of diurnal glucose changes. In the specific group of women with gestational diabetes, in whom postprandial glucose is critical regarding fetal complications, the experience has suggested advantages of CGM in detecting abnormal postprandial glucose levels (42).
A recently published multicenter clinical trial has shown that CGM is associated with improved glycemic control in adults (25 years of age or older) with type 1 diabetes, being the primary outcome of the change in A1C level at 26 weeks (43). The same trial, as well as a systematic review and meta-analysis, confirmed that CGM is not better than SMBG with regard to improvement of metabolic control among type 1 diabetic children (44). A plausible explanation for these findings may relay in the observation that among the subjects using CGM, those in the 15- to 24-year-old group were less adherent to sensor use than were older or younger patients (43). Rates of hypoglycemia were similar with CGM and SMBG in all age-groups.
Our work strongly suggests that the intermittent use (42% of the time) of GCM, with the support of telemedicine, achieves reduction of A1C and improvement of glucose stability in type 1 diabetic patients. Furthermore, for the first time, real-time CGM, in conjunction with telemedical support, has been successfully assessed. CGM, together with SMBG and insulin pump, generate a tremendous amount of data, which makes processing by patients and physicians quite troublesome; thanks to DIABTel, the analysis is facilitated by data aggregation, statistics, and graphic registries in an easily integrated and user-friendly manner.
Improved accuracy of real-time CGM facilitates the development of close-loop systems, with the greatest potential for the near future and the support of the Juvenile Diabetes Research Artificial Pancreas Project (45).
In conclusion, the PARIS Research Project has shown that a Telemedicine System incorporating an SA improves glucose control in adult type 1 diabetic subjects. The investigation has also proven that the use of real-time CGM in conjunction with telemedical assistance improves glucose control and glucose stability in adult type 1 diabetic patients, treated with an insulin pump. Because of the small size of the recruited samples, these results need to be reproduced in larger groups of type 1 diabetic patients in the coming future. The Telemedical Artificial Pancreas solution, proposed in the PARIS Research Project, integrates a personal loop that allows wireless communication between the SA, insulin pump, and CGM device, with a remote loop that connects the diabetic patient to the health care professional via the SA and its wireless communication with a telemedicine central server. The TAP offers four control strategies, each of them supported by a special function of the smart assistant. In strategy 1, the patient decides changes in the insulin program by using the information provided by the glucose sensor. In strategy 2, the physician prescribes changes in insulin treatment, using the information provided by CGM and CSII, reaching the TMCS from the SA. In strategy 3, the SA is remotely programmed by automatic procedure, under the physician supervision (remote loop control algorithm). Finally, in strategy 4, the SA provides a real-time control of the insulin pump based on the information offered by the CGM (personal loop control algorithm). The selection of a specific strategy or combination of strategies depends on the different circumstances of the patient (for example, an automatic personal loop control algorithm could be active at night and a control mode could be used during the day). Close-loop systems may generate a revolution in diabetes management; nevertheless, their introduction must be gradual and progressive, in parallel to advance of knowledge, increasing experience, accuracy of the systems, and overall, the patient's safety.
Acknowledgments
The PARIS Research Project was funded by Spanish Grants CICYT SAF98-0170, Fundació Marató TV3 (OPTIDIAB), ISCIII (PIO 42466/PIO 42372; PIO 61067/PIO 60437, CIBER-BBN), and FUNDACIÓ DIABEM and also by European Union Grants EU-TIDDM HC 1047 and EU-Consortium INCA (IST-2001-37632).
We thank Medtronic (Madrid, Spain) and Roche-Disetronic Medical System (Burgdorf, Switzerland) for technical and instrumental support.
No potential conflicts of interest relevant to this article were reported.
Other coauthors from EDUAB-HSP include M. Rigla, I. Capel, E. Brugués, B. Pons, L. Erdozain, A. Prados, and R. Corcoy. Other coauthors from GBT-UPM include E.J. Gómez, G. García-Sáez, I. Martínez-Sarriegui, A. Rodríguez-Herrero, C. Pérez-Gandía, and F. del Pozo.
Footnotes
The publication of this supplement was made possible in part by unrestricted educational grants from Eli Lilly, Ethicon Endo-Surgery, Generex Biotechnology, Hoffmann-La Roche, Johnson & Johnson, LifeScan, Medtronic, MSD, Novo Nordisk, Pfizer, sanofi-aventis, and WorldWIDE.
References
- 1. Hovorka R: Continuous glucose monitoring and closed-loop systems. Diabet Med 2005; 23: 1– 12 [DOI] [PubMed] [Google Scholar]
- 2. Baquette BV: A critical assessment of algorithms and challenges in the development of a close-loop artificial pancreas. Diabetes Technol Ther 2005; 7: 28– 47 [DOI] [PubMed] [Google Scholar]
- 3. Owens C, Zisser H, Jovanovic L, Srinivasan B, Bonvin D, Doyle J, III: Run-to-run control of blood glucose concentration for people with type 1 diabetes mellitus. IEEE Trans Inf Technol Biomed 2006; 6: 996– 1005 [DOI] [PubMed] [Google Scholar]
- 4. Hovorka R, Chassin LJ, Wilinska ME, Canonico V, Akwi JA, Federici MO, Massi-Benedetti M, Hutzli I, Zaugg C: Closing the loop: the Adicol experience. Diabetes Technol Ther 2004; 6: 307– 318 [DOI] [PubMed] [Google Scholar]
- 5. Bailey TS, Zisser HC, Garg SK: Reduction in hemoglobin A1c with real-time continuous glucose monitoring: results from a 12-week observational study. Diabetes Technol Ther 2007; 9: 203– 210 [DOI] [PubMed] [Google Scholar]
- 6. Garg S, Zisser HC, Schwartz S, Bailey T, Kaplan R, Ellis S, Jovanovic L: Improvement in glycemic excursions with a transcutaneous, real-time continuous glucose sensor. Diabetes Care 2006; 29: 44– 50 [DOI] [PubMed] [Google Scholar]
- 7. Garg S, Jovanovic L: Relationship of fasting and hourly blood glucose levels to HbA1c values: safety, accuracy, and improvements in glucose profiles obtained using a 7-day continuous glucose sensor. Diabetes Care 2006; 29: 2644– 2649 [DOI] [PubMed] [Google Scholar]
- 8. Halvorson M, Carpenter S, Kaiserman K, Kaufman FR: A pilot trial in pediatrics with sensor-augmented pump: combining real time continuous glucose monitoring with the insulin-pump. J Pediatr 2007; 150: 103– 105 [DOI] [PubMed] [Google Scholar]
- 9. Deiss D, Bolinder J, Riveline J-P, Battelino T, Boli E, Tubiana-Rufi N, Kerr D, Phillip M: Improved glycemic control in poorly controlled patients with type 1 diabetes using real-time continuous glucose monitoring. Diabetes Care 2006; 12: 2730– 2734 [DOI] [PubMed] [Google Scholar]
- 10. Gómez EJ, Hernando ME, García A, del Pozo F, Corcoy R, Brugués E, Cermeño J, de Leiva A: Telemedicine as a tool for intensive management of diabetes: the DIABTel experience. Comput Meth Prog Biomed 2002; 69: 163– 177 [DOI] [PubMed] [Google Scholar]
- 11. Wojcicki J, Ladyzynski P, Krzymien J, Jozwicka E, Blachowicz J, Janczewska E, Czajkowski K, Karnafel W: What can we really expect from telemedicine in intensive diabetes treatment: results from 3-year study on type 1 pregnant women. Diabetes Technol Ther 2001; 3: 581– 589 [DOI] [PubMed] [Google Scholar]
- 12. Bellazzi R, Larizza C, Montani S, Riva A, Stefanelli M, D'Annunzio G, Lorini R, Gómez EJ, Hernando ME, Brugués E, Cermeño J, Corcoy R, de Leiva A, Cobelli C, Nucci G, del Prato S, Maran A, Kilkki E, Tuominen J: A telemedicine support for diabetes management: the T-IDDM project. Comput Meth Prog Biomed 2002; 69: 147– 161 [DOI] [PubMed] [Google Scholar]
- 13. Gómez EJ, del Pozo F, Hernando ME: Telemedicine for diabetes care: the DIABTel approach towards diabetes telecare. Med Inform 1996; 21: 283– 295 [DOI] [PubMed] [Google Scholar]
- 14. Bellazzi R, Arcelloni M, Bensa G, Blankenfeld H, Brugués E, Carson E, Cobelli C, Cramp D, d'Annunzio G, de Cata P, de Leiva A, Deutsch T, Fratino P, Gazzaruso C, García A, Gergely T, Gómez E, Harvey F, Ferrari P, Hernando E, Boulos MK, Larizza C, Ludekke H, Maran A, Nuccci G, Pennati C, Ramat S, Roudsari A, Rigla M, Stefanelli M: Design, methods, and evaluation directions of a multi-access service for the management of diabetes mellitus patients. Diabetes Technol Ther 2003; 5: 621– 629 [DOI] [PubMed] [Google Scholar]
- 15. Hernando ME, Gómez EJ, Corcoy R, del Pozo F: Evaluation of DIABNET, a decision support system for therapy planning in gestational diabetes. Comput Methods Prog Biomed 2000; 62: 235– 248 [DOI] [PubMed] [Google Scholar]
- 16. Gómez EJ, del Pozo F, Ortiz E, Malpica N, Rahms H: A broad multimedia collaborative system for advanced teleradiology and medical diagnosis. IEEE Trans Inf Technol Biomed 1998; 2: 146– 156 [DOI] [PubMed] [Google Scholar]
- 17. Montani S, Bellazzi R, Larizza C, Riva A, d'Annunzio G, Fiochi S, Lorini R, Stefanelli M: Protocol-based reasoning in diabetic patient management. Int J Med Inf 1999; 53: 61– 77 [DOI] [PubMed] [Google Scholar]
- 18. Hovorka R, Svacina S, Carson ER, Williams CD, Sönsken PH: A consultation system for insulin therapy. Comput Methods Prog Biomed 1996; 32: 303– 310 [DOI] [PubMed] [Google Scholar]
- 19. Hovorka R, Shojaee-Moradie F, Carroll PV, Chassin J, Gowrie IJ, Jackson NC, Tudor RS, Umpleby AM, Jones RH: Partitioning glucose distribution/transport, disposal, and endogenous production during IVGTT. Am J Physiol Endocrinol Metab 2002; 282: E992– E1007 [DOI] [PubMed] [Google Scholar]
- 20. Bott OJ, Bergmann J, Hoffmann I, Vering T, Gómez EJ, Hernando ME, Pretschner DP: Analysis and specification of telemedical systems using modelling and simulation: the MOSAIK-M approach. Stud Health Technol Inform 2005; 116: 503– 508 [PubMed] [Google Scholar]
- 21. Gómez EJ, Hernando ME, Vering T, Rigla M, Bott O, García-Sáez G, Pretschner P, Brugués E, Schnell O, Patte C, Bergmann J, Dudde R, de Leiva A: The INCA system: a further step towards a telemedical artificial pancreas. IEEE Trans Inf Technol Biomed 2008; 12: 470– 479 [DOI] [PubMed] [Google Scholar]
- 22. Rigla M, Hernando ME, Gómez EJ, Brugués E, García-Sáez G, Torralba V, Prados A, Erdozain L, Vilaverde J, de Leiva A: A telemedicine system that includes a personal assistant improves glycemic control in pump-treated patients with type 1 diabetes. J Diabetes Sci Technol 2007; 1: 505– 510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Rigla M, Hernando ME, Gómez EJ, Brugués E, García-Sáez G, Capel I, Pons B, de Leiva A: Real-time continuous glucose monitoring together with telemedical assistance improves glycemic control and glucose stability in pump-treated patients. Diabetes Technol Ther 2008; 10: 194– 199 [DOI] [PubMed] [Google Scholar]
- 24. Kovatchev BP, Clarke WL, Breton M, Brayman K, McCall AL: Quantifying temporal glucose monitoring: mathematical methods and clinical application. Diabetes Technol Ther 2005; 7: 849– 862 [DOI] [PubMed] [Google Scholar]
- 25. McCall AL, Cox DJ, Crean J, Gloster M, Kovatchev BP: A novel analytical method for assessing glucose variability: using CGMS in type 1 diabetes mellitus. Diabetes Technol Ther 2006; 8: 644– 653 [DOI] [PubMed] [Google Scholar]
- 26. Kovatchev BP, Otto E, Cox D, Gonder-Frederick L, Clarke W: Evaluation of a new measure of blood glucose variability in diabetes. Diabetes Care 2006; 29: 2433– 2438 [DOI] [PubMed] [Google Scholar]
- 27. Bolli GB: Glucose variability and complications. Diabetes Care 2006; 29: 1707– 1709 [DOI] [PubMed] [Google Scholar]
- 28. International Diabetes Federation. Global Guidelines for Type 2 Diabetes. Brussels, Belgium, IDF, 2005 [Google Scholar]
- 29. Schiffrin A, Belmonte M: Multiple daily self-glucose monitoring: its essential role in long-term glucose control in insulin-dependent diabetic patients treated with pump and multiple subcutaneous injections. Diabetes Care 1982; 5: 479– 484 [DOI] [PubMed] [Google Scholar]
- 30. Diabetes Control and Complications Trial Research Group The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993; 329: 977– 986 [DOI] [PubMed] [Google Scholar]
- 31. Evans JMM, Newton RW, Ruta DA, MacDonald TM, Stevenson RJ, Morris AD: Frequency of blood glucose monitoring in relation to glycaemic control: observational study with diabetes database. BMJ 1999; 319: 83– 86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Karter AJ, Ackerson LM, Darbinian JA, D'Agostino RB, Jr, Ferrara A, Liu J, Selby JV: Self-monitoring of blood glucose levels and glycemic control: the Northern California Kaiser Permanent Diabetes Registry. Am J Med 2001; 111: 1– 9 [DOI] [PubMed] [Google Scholar]
- 33. Welschen LM, Bloemendal E, Nijpels G, Dekker JM, Heine RJ, Stalman WA, Bouter LM: Self-monitoring of blood glucose in patients with type 2 diabetes who are not using insulin: a systematic review. Diabetes Care 2005; 28: 1510– 1517 [DOI] [PubMed] [Google Scholar]
- 34. Sarol JN, Nicodemus NA, Tan KM, Grava MB: Self-monitoring of blood glucose as part of a multi-component therapy among non-insulin-requiring type 2 diabetic patients: a meta-analysis (1966–2004). Curr Med Res Opin 2005; 21: 173– 183 [DOI] [PubMed] [Google Scholar]
- 35. Jansen JP: Self-monitoring of blood glucose in type-2 diabetes mellitus: a Bayesian meta-analysis of direct and indirect comparisons. Curr Med Res Opin 2006; 22: 671– 681 [DOI] [PubMed] [Google Scholar]
- 36. Palmer AJ, Dinneen S, Gavin JR, Gray A, Herman WH, Karter AJ: Cost-utility analysis in a UK setting of self-monitoring of blood glucose in patients with type 2 diabetes. Curr Med Res Opin 2006; 22: 861– 872 [DOI] [PubMed] [Google Scholar]
- 37. McGeoch G, Moore RA: Self-monitoring of blood glucose in type-2 diabetes: what is the evidence? Diabete Metab Res Rev 2007; 23: 423– 440 [DOI] [PubMed] [Google Scholar]
- 38. Heinemann L, Koschinsky T: Clinical application and challenges of blood glucose measurement technology for self-monitoring. Diabetes Technol Ther 2008; 10 ( Suppl. 1): S27– S34 [Google Scholar]
- 39. Mazze R: The future of self-monitored blood glucose: mean blood glucose versus glycosylated haemoglobin. Diabetes Technol Ther 2008; 10 ( Suppl. 1): S93– S101 [Google Scholar]
- 40. Hönes J, Müller P, Surridge N: The technology behind glucose meters: test strips. Diabetes Technol Ther 2008; 10 ( Suppl. 1): S10– S26 [Google Scholar]
- 41. Laird T, Zisser H, Jovanovic L: Self-monitoring of blood glucose in pregnancy: past to present. Diabetes Technol Ther 2008; 10 ( Suppl. 1): S82– S87 [Google Scholar]
- 42. Ben-Haroush A, Yogel Y, Chen R, Rosenn B, Hod M, Langer O: The postprandial glucose profile in the diabetic pregnancy. Am J Obstet Gynecol 2004; 191: 576– 581 [DOI] [PubMed] [Google Scholar]
- 43. Juvenile Diabetes Res Foundation Continuous Glucose Monitoring Study Group Continuous glucose monitoring and intensive treatment of type 1 diabetes. N Engl J Med 2008; 359: 1464– 1476 [DOI] [PubMed] [Google Scholar]
- 44. Golicki DT, Golicka D, Groele L, Pankowska E: Continuous glucose monitoring system in children with type 1 diabetes mellitus: a systematic review and meta-analysis. Diabetologia 2008; 51: 233– 240 [DOI] [PubMed] [Google Scholar]
- 45. Hovorka R: The future of continuous glucose monitoring: closed loop. Current Diabetes Reviews 2008; 4: 269– 279 [DOI] [PubMed] [Google Scholar]