Type 2 diabetes is a chronic disease characterized by coexisting insulin deficiency and insulin resistance, with the resultant hyperglycemia leading to micro- and macrovascular complications. A large number of intervention trials demonstrated that improving glycemic control achieves considerable reductions of such complications (1–7).
It has been estimated using the homeostasis multiple assessment (HOMA) that, at the time of diagnosis, ∼50% of pancreatic β-cell function has been lost, with almost 4% further loss of function expected per year thereafter (8,9). Therefore, type 2 diabetes is a chronic progressive disease characterized by worsening hyperglycemia and escalating deterioration in the function of pancreatic β-cells and loss of β-cell mass (10). Because of the progressive nature of the disease, an evolving treatment strategy is therefore necessary to maintain both fasting and postprandial glycemic control. Recently, an American Diabetes Association (ADA) and European Association for the Study of Diabetes (EASD) Consensus recommended a target of A1C <7% for good glucose control in clinical practice (11). Insulin therapy is required when dietary restrictions and lifestyle modifications combined with oral hypoglycemic agents (OHAs) failed to provide acceptable metabolic control (12). One major lesson learned from the milestone U.K. Prospective Diabetes Study (UKPDS) is the increasing requirement for multiple therapies in patients with type 2 diabetes to achieve blood glucose (BG) target control (13).
The augmentation of insulin to OHAs contributed to several beneficial metabolic effects, as recently reviewed (14). However, there is ongoing debate as to whether it is more rewarding to target postprandial BG concentrations with meal-related insulin, or to target fasting BG concentrations with basal insulin. Monnier et al. (15,16) provided data to explain the relative contribution of fasting and postprandial BG to A1C in patients with mild-to-moderate hyperglycemia (A1C <7.3%) than in those with more poorly controlled blood glucose.
The APOLLO trial (A Parallel design comparing an Oral antidiabetic drug combination therapy with either Lantus once daily or Lispro at mealtime in type 2 diabetic patients failing Oral treatment), a multicenter randomized prospective study, addressed the issue of targeting either prandial or fasting BG concentrations (17).
HOW TO INITIATE BASAL OR PRANDIAL INSULIN THERAPY: THE APOLLO TRIAL
In the 44-week parallel open study that was performed in 69 study sites across Europe and Australia, 418 individuals with type 2 diabetes inadequately controlled by OHAs (excluding α-glucosidase inhibitors) were randomly assigned to either basal insulin glargine (Lantus; sanofi-aventis, Frankfurt, Germany) once daily, at the same time every day, or to mealtime insulin lispro (Humalog; Eli Lilly, Bad Homburg, Germany) administered thrice daily in addition to the OHAs. The primary objective was to compare the change in A1C from baseline to end point (week 44) between the two regimens. In addition, secondary objectives included the percentage of participants who achieved A1C of 6.5 or 7.0% or less, respectively, the number of hypoglycemic events, the change in body weight in both treatment arms, and treatment satisfaction.
Male and female patients were eligible for enrollment if they were aged between 18 and 75 years. Additional inclusion criteria: type 2 diabetes for ≥1 year with an A1C concentration between 7.5 and 10.5%, OHA treatment for at least 6 months with stable doses for ≥3 months before study entry, fasting BG concentrations of ≥6.5 mmol/l, and BMI of ≤35 kg/m2. All participants were willing to perform self-monitoring of BG, and all provided written informed consent for their participation before study entry.
Of 412 patients in the intention-to-treat population, a total of 35 patients were excluded because of major protocol deviations during the study. Thus, the per-protocol population comprised 377 patients (186 in the insulin glargine and 191 in the insulin lispro groups) who were included in our analyses. After randomization, most patients received metformin therapy throughout the study (156 [76%] and 153 [74%]) in the insulin glargine and insulin lispro treatment groups, respectively). Most patients in both groups were prescribed glimepiride, with only 11 (6%) patients assigned to insulin glargine, and 14 (7%) to insulin lispro, without glimepiride. Patient demographics (mean age, 59.7 years in both arms; BMI: 29.2/29.3 kg/m2; duration of OHA treatment: 6.8/6.3 years, glycemic control: A1C: 8.73/8.67%, and fasting BG: 10.4/9.8 mmol/l, in both groups, respectively) were similar at baseline.
During the treatment phase, insulin doses were adjusted by a forced titration regimen to a target fasting BG <5.5 mmol/l in the insulin glargine group, and a preprandial BG <5.5 mmol/l and a postprandial BG <7.5 mmol/l in the insulin lispro group, in accordance with the insulin titration algorithms proposed by the European Diabetes Policy Group in 1999 (18). Insulin dose titration algorithms and monitoring are presented in Tables 1 and 2. At the start of screening, at week 20, and at week 44 (study end point), a validated diabetes treatment satisfaction questionnaire was distributed among the patients (19).
Table 1.
Insulin glargine dose titration algorithm and monitoring
| Starting dose: 10 IU/day | ||
|---|---|---|
| Titration monitoring | Direct investigator contact. Fasting BG and insulin dose submitted to coordinating center by electronic data capture. Additional weekly calls to adjust insulin dose if A1C >7% | |
| Insulin dose titration | ||
| algorithm | If self-monitored fasting BG for 2 consecutive days with no severe hypoglycemia: | |
| >8.9 mmol/l (>160 mg/dl) | Add 8 IU/day | |
| >7.8 to ≤8.9 mmol/l (>140 to ≤160 mg/dl) | Add 6 IU/day | |
| >6.7 to ≤7.8 mmol/l (>120 to ≤140 mg/dl) | Add 4 IU/day | |
| >5.5 to ≤6.7 mmol/l (>100 to ≤120 mg/dl) | Add 2 IU/day | |
| 5.5 mmol/l (≤100 mg/dl) | No further titration |
Table 2.
Insulin lispro dose titration algorithm and monitoring
| Starting dose: 4 IU/meal | ||
|---|---|---|
| Titration | ||
| monitoring | Direct investigator contact. Fasting BG and insulin dose submitted to coordinating center by electronic data capture. Additional weekly calls to adjust insulin dose if A1C >7% | |
| Preprandial BG | ||
| Insulin dose titration | ||
| algorithm | >10.3 mmol/l (>185 mg/dl) | Add 3 IU before main meal |
| >8.3 to ≤11.1 mmol/l (>150 to ≤200 mg/dl) | Add 2 IU before main meal | |
| >5.5 to ≤8.3 mmol/l (>100 to ≤150 mg/dl) | No further titration | |
| Postprandial BG | ||
| Insulin dose titration | ||
| algorithm | >10.3 mmol/l (>185 mg/dl) | Add 2 IU before main meal |
| >7.5 to ≤10.3 mmol/l (>135 to ≤185 mg/dl) | Add 1 IU before main meal | |
| ≤7.5 mmol/l (≤135 mg/dl) | No further titration |
Hypoglycemia was defined as an event with or without symptoms consistent with hypoglycemia, not requiring the assistance of another person, and associated with BG concentration of <3.3 mmol/l. Severe hypoglycemia was defined as an event with symptoms consistent with hypoglycemia, necessitating assistance, associated with a BG concentration of <2.0 mmol/l, or recovery after oral carbohydrate, intravenous glucose, or glucagon administration. Nocturnal hypoglycemia was defined as hypoglycemia, occurring while the individual was asleep and before arising in the morning. Whenever participants awoke during the night and experienced symptoms of hypoglycemia, self-monitoring of BG was performed and documented in the patients' diary.
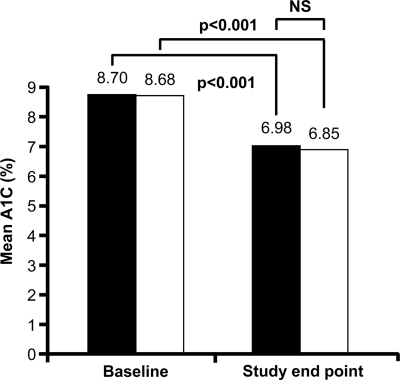
Both treatment regimens were equally effective in lowering A1C concentrations to target (≤7%) at study end, with similar differences between the adjusted means (−1.71 vs. −1.87%), which was within the predefined 0.4% limit for parity for the differences of A1C between the groups (Fig. 1).
Figure 1.
Improvement in A1C with insulin glargine plus OHAs (■) versus insulin lispro plus OHAs (□) from baseline to end point (44 weeks) in the per-protocol population. Change from baseline not significantly different between both groups.
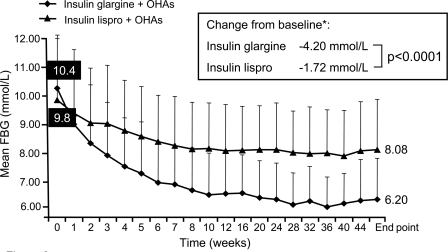
Figure 2 illustrates reductions of fasting BG concentrations over the 44-week trial period as well as the difference in the degree of change from baseline to end point between the groups (P < 0.0001). Insulin glargine achieved a reduction in the fasting glucose level from 10.4 to 6.2 mmol/l (Fig. 2). In comparison, a much smaller reduction in fasting glucose level from 9.8 to 8.08 mmol/l was seen in the insulin lispro group (Fig. 2).
Figure 2.
Reduction in fasting blood glucose (FBG) with insulin glargine plus OHAs versus insulin lispro plus OHAs from baseline to end point (44 weeks) in the per-protocol population. Change from baseline significantly greater in the glargine group.
Compared with baseline, 106 (57%) patients in the insulin glargine group and 131 (69%) patients in the insulin lispro group achieved the A1C target of ≤7% (Table 3). Significantly more patients in the insulin glargine group reached the fasting BG target of ≤5.5 mmol/l than with insulin lispro at study end point (71 [38%]) versus 11 [6%]) (Table 3). Conversely, a significantly greater reduction of the 2-h postprandial BG was achieved with insulin lispro than insulin glargine after breakfast: −4.6 vs. 4.2 mmol/l (P = 0.0421); lunch: −4.3 vs. −3.1 mmol/l (P < 0.0001); and dinner: −5.0 vs. −3.2 mmol/l (P < 0.0001), respectively. Both insulin preparations were also effective beyond the targets of their titration algorithms. Insulin glargine resulted in a highly significant (P < 0.0001) absolute reduction of mean daytime glucose level from baseline to end point: 9.9 ± 2.0 to 6.9 ± 1.5 mmol/l, which corresponds to −3.0 ± 2.1 mmol/l. The insulin lispro group showed an absolute reduction from baseline to end point of 9.7 ± 2.9 to 7.1 ± 1.8 mmol/l corresponding to −1.8 ± 2.3 mmol/l, which was also highly significant (P < 0.0001).
Table 3.
Main outcomes in the APOLLO trial and the 4-T study
| APOLLO |
4-T |
|||
|---|---|---|---|---|
| Target A1C ≤7% at 44 weeks |
Target A1C ≤7% at 52 weeks |
|||
| Basal* | Prandial† | Basal* | Prandial† | |
| A1C (%) | ||||
| At baseline | 8.73 | 8.67 | 8.40 | 8.60 |
| At endpoint | 6.98 | 6.80 | 7.60 | 7.20 |
| Δ (baseline vs. endpoint) | −1.75 | −1.87 | −1.40 | |
| Responder rate (% patients achieving A1C target) | ||||
| ≤7.0% | 57 | 69 | 28 | 49 |
| ≤6.5% | 30 | 38 | 8 | 24 |
| Responder rate (% patients achieving FBG target) | 38 | 6 | ||
| Insulin dose (IU/day) at end point | 42 | 45 | 42 | 56 |
| Treatment satisfaction score‡ (Δ change from baseline) | +6.23 | +2.74 | ±0 | −0.02 |
| Number of overall hypoglycemic events per patient-year | 5.2 | 24.0 (×4.6) | 2.3 | 12.0 (×5.2) |
| Change in body weight (Δ kg from baseline) | +3.0 | +3.5 | +1.9 | +5.7 |
*Basal insulin: insulin glargine for APOLLO trial, insulin detemir for 4-T study.
†Prandial insulin: insulin lispro for APOLLO trial, insulin aspart for 4-T study.
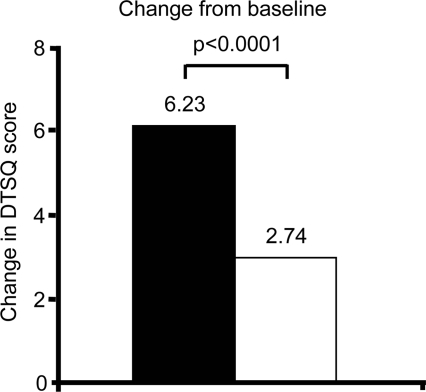
The mean score for treatment satisfaction improved in both groups from baseline to end point, but the magnitude of change was significantly greater with insulin glargine than with insulin lispro (difference of the magnitude of change 3.49; P < 0.0001) (Fig. 3).
Figure 3.
Change in treatment satisfaction in both groups as analyzed by the Diabetes Treatment Satisfaction Questionnaire (DTSQ [19]). Change from baseline significantly greater in the glargine group. ■, Insulin glargine + OHAs; □, insulin lispro + OHAs.
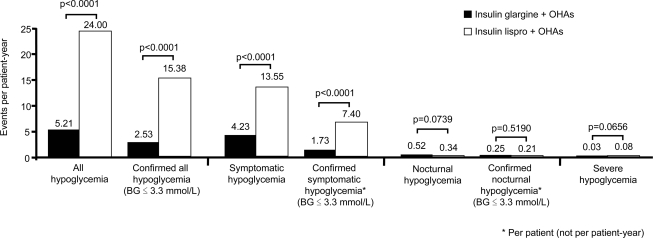
As can be seen in Fig. 4, the rates of all, including confirmed all (BG ≤3.3 mmol/l), symptomatic, and confirmed symptomatic hypoglycemic episodes (BG ≤3.3 mmol/l), were significantly lower with insulin glargine than with insulin lispro (all P < 0.0001). However, the rates of nocturnal, confirmed nocturnal, and severe hypoglycemic episodes were comparable in both groups (Fig. 4).
Figure 4.
Rates of hypoglycemia in participants receiving at least one dose of insulin (safety analysis population).
Weight gain was recorded between baseline and end point in both the insulin glargine (3.01 ± 4.33 kg) and insulin lispro (3.54 ± 4.48 kg) groups, although the difference did not reach significance (P = 0.23). There was no significant variation in the rates of adverse and severe adverse events between the two treatment groups.
A similar study, the Treating to Target in Type 2 Diabetes Trial (4-T study), recently published the 1-year interim analysis (20). In their basal insulin treatment group, insulin detemir (Novo Nordisk, Bagsvaerd, Denmark) was used once or twice daily and insulin aspart (Novo Nordisk) administered premeal thrice daily, representing the prandial insulin treatment group. Data on an additional group of patients who received premixed insulin twice daily is not discussed here. Excluding the latter, the study design and overall baseline characteristics were analogous to those in the APOLLO trial.
The reduction of A1C in both (basal and prandial) treatment groups was lower in the 4-T study than in the APOLLO trial (Table 3). Furthermore, twice as many patients in the basal insulin cohort achieved target A1C <7% in the APOLLO trial compared with the 4-T study, despite apparently equivalent insulin doses administered in both studies, and despite the twice-daily dose of basal insulin detemir that was required in 34% of the patients in the 4-T study (Table 3). In the APOLLO trial, the quality-of-life assessment improved in both groups with significant (P < 0.0001) advantage of basal insulin treatment over the prandial regimen, using a different quality-of-life assessment score (21). In the 4-T study, there was no significant difference between the groups (Table 3).
Both studies also noted a significantly lower risk of hypoglycemia with basal compared with prandial insulin treatment (Table 3). The patients of the 4-T study on insulin detemir reported on 50% less incidences of hypoglycemia per patient year compared with those on insulin glargine in the APOLLO trial. This effect may be explained by the lower magnitude of A1C reduction in the 4-T study group compared with baseline (Δ baseline versus end point −1.75 in the APOLLO trial and −0.80 in the 4-T study).Weight gain after 1 year was significantly lower in the basal insulin detemir group compared with the prandial insulin aspart group in the 4-T study, whereas weight gain after 44 weeks was only slightly less in the basal insulin glargine group, but the difference with prandial insulin lispro did not reach statistical significance in the APOLLO trial.
SHOULD NPH INSULIN OR INSULIN GLARGINE BE USED FOR BASAL INSULIN THERAPY?
It has been shown that the supplementation of basal insulin reduces the entire 24-h fasting BG profile (22). This improvement results predominantly from suppression of overnight hepatic glucose production, both via direct effects on the liver and indirect effects through suppression of free fatty acid release from adipose tissue. Furthermore, targeting fasting BG levels reduce the overall glucose load and may improve pancreatic β-cell insulin secretion to a certain extent (23). Therefore, basal insulin as a first-line insulin initiation therapy is now recommended in a joint consensus guideline by the ADA and EASD (11).
Clinical trials have demonstrated that type 2 diabetic patients treated with insulin glargine exhibited significant improvements in glycemic control, which are at least equivalent (24–27), or superior (28,29), to improvements associated with NPH insulin. Furthermore, a recent meta-analysis concluded that patients treated with insulin glargine are at lower risk of hypoglycemia, and in particular, nocturnal hypoglycemia, compared with NPH insulin-treated patients (30). To further clarify this issue of the overnight action profile of insulin glargine and NPH insulin, a randomized placebo-controlled double-blind three-way crossover clamp study in type 2 diabetic patients, comparing bedtime injections of either insulin glargine or NPH insulin, was conducted to investigate the rates of endogenous glucose production and glucose disposal during the night and in the morning (31). The study confirmed delayed onset of insulin glargine compared with NPH insulin in these patients (31). Insulin glargine was associated with a greater reduction of endogenous glucose production in the morning between 6:00 and 8:00 a.m. compared with NPH insulin, when the insulins were administered at bedtime. The joint actions of insulin glargine would therefore be expected to contribute to the reduced risk of nocturnal hypoglycemia and lower fasting BG compared with NPH insulin (31).
Insulin glargine has an additional advantage over NPH insulin. It can be administered once daily at the same time of day, owing to its relatively peakless and extended hypoglycemic profile in type 2 diabetic patients, whereas NPH insulin requires to be given twice daily in most cases (24,28,32).
SUMMARY AND CONCLUSIONS
The APOLLO trial, designed as a noninferiority study, clearly demonstrated that a single dose of basal insulin glargine is as effective as thrice-daily prandial insulin lispro in controlling glucose metabolism when used in combination with OHAs in individuals with type 2 diabetes. Moreover, the basal insulin regimen was associated with a significantly lower risk of hypoglycemia and a greater improvement in quality of life and treatment satisfaction compared with the prandial insulin regimen. Fewer insulin injections and less self-monitoring of BG required with basal insulin glargine therapy may have contributed to the greater treatment satisfaction experienced compared with a thrice-daily prandial insulin regimen.
A comparable study, the 4-T study, using different basal and prandial insulin analogs and different titration algorithms, documented a similar beneficial effect of the basal insulin approach with respect to hypoglycemic risk and body weight increase.
Overall, insulin glargine has proved superior to NPH insulin in basal insulin regimens for the management of type 2 diabetes. Recent results of a 5-year long-term study with insulin glargine versus NPH insulin have also demonstrated no harmful effects on diabetic retinopathy progression with insulin glargine over that expected by BG lowering, a lower incidence of hypoglycemic episodes, and less weight gain. These data were recently published (33).
The addition of insulin glargine to OHAs is a simple and well-tolerated intervention that may prove helpful in overcoming major barriers to timely insulin initiation in settings of both primary and secondary care (34). Furthermore, it has been demonstrated that the use of a simple self-administered titration algorithm is equally as effective at improving glycemic control as is titration management by staff at hospital-based diabetes centers (27,35). Results of a large observational study of daily practice in >10,000 individuals with type 2 diabetes inadequately controlled on OHAs confirmed the benefits from supplementation of basal insulin treatment with glargine, since the patients demonstrated improved glycemic control with little or no weight gain (36).
Finally, when basal insulin therapy in type 2 diabetes is insufficient to control daily BG profiles, a single injection of prandial insulin before the mealtime that induces the largest postprandial BG excursion (measured 2 h after the start of the meal) may be given (37). Over time and with progression of the disease, additional prandial boluses of insulin may be required to sustain daytime glycemic control. This strategy of basal insulin to control fasting BG first and, if needed, followed by an additional single prandial insulin injection (“basal plus” concept) offers a simple, stepwise approach in progressing from a basal insulin to a basal-bolus regimen (37,38).
In conclusion, evidence from the APOLLO trial suggests that the addition of basal insulin analog glargine to therapies with OHAs can be regarded as a first-line insulin initiation approach in inadequately controlled type 2 diabetes (39).
Acknowledgments
R.G.B. served as a consultant to or gave lectures organized by Bayer, Develogen, GlaxoSmithKline, Lilly, MSD, Novo Nordisk, and sanofi-aventis. M.E. gave lectures organized by Novo Nordisk and sanofi-aventis. W.L. is an employee of sanofi-aventis. D.R.O. served as a consultant for sanofi-aventis, MSD, Pfizer, Novo Nordisk, Roche, and Novartis, and gave lectures at various symposia sponsored by these companies. T.L. received an unrestricted research grant from sanofi-aventis.
No other potential conflicts of interest relevant to this article were reported.
The authors express their thanks to all the investigators and their teams who contributed to the success of this trial.
This article is dedicated to the patients with diabetes who volunteered for the APOLLO trial.
Footnotes
The publication of this supplement was made possible in part by unrestricted educational grants from Eli Lilly, Ethicon Endo-Surgery, Generex Biotechnology, Hoffmann-La Roche, Johnson & Johnson, LifeScan, Medtronic, MSD, Novo Nordisk, Pfizer, sanofi-aventis, and WorldWIDE.
References
- 1. Stratton M, Adler AI, Neil HA, Matthews DR, Manley SE, Cull CA, Hadden D, Turner RC, Holman RR: Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ 2000; 321: 405– 412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Action to Control Cardiovascular Risk in Diabetes Study Group. Gerstein HC, Miller ME, Byington RP, Goff DC, Jr, Bigger JT, Buse JB, Cushman WC, Genuth S, Ismail-Beigi F, Grimm RH, Jr, Probstfield JL, Simons-Morton DG, Friedewald WT: Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 2008; 358: 2545– 2559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. ADVANCE Collaborative Group. Patel A, MacMahon S, Chalmers J, Neal B, Billot L, Woodward M, Marre M, Cooper M, Glasziou P, Grobbee D, Hamet P, Harrap S, Heller S, Liu L, Mancia G, Mogensen CE, Pan C, Poulter N, Rodgers A, Williams B, Bompoint S, de Galan BE, Joshi R, Travert F: Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 2008; 358: 2560– 2572 [DOI] [PubMed] [Google Scholar]
- 4. Raz I, Wilson PW, Strojek K, Kowalska I, Bozikov V, Gitt AK, Jermendy G, Campaigne BN, Kerr L, Milicevic Z, Jacober SJ: Effects of prandial versus fasting glycemia on cardiovascular outcomes in type 2 diabetes: the HEART2D trial. Diabetes Care 2009; 32: 381– 386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Duckworth W, Abraira C, Moritz T, Reda D, Emanuele N, Reaven PD, Zieve FJ, Marks J, Davis SN, Hayward R, Warren SR, Goldman S, McCarren M, Vitek ME, Henderson WG, Huang GD: VADT Investigators. Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med 2009; 360: 129– 139 [DOI] [PubMed] [Google Scholar]
- 6. Stettler C, Allemann S, Jüni P, Cull CA, Holman RR, Egger M, Krähenbühl S, Diem P: Glycemic control and macrovascular disease in types 1 and 2 diabetes mellitus: meta-analysis of randomized trials. Am Heart J 2006; 152: 27– 38 [DOI] [PubMed] [Google Scholar]
- 7. Holman RR, Paul SK, Angelyn Bethel M, Matthews DR, Andrew H, Neil W: 10-Year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med 2008; 359: 1577– 1589 [DOI] [PubMed] [Google Scholar]
- 8. U.K. Prospective Diabetes Study Group U.K. Prospective Diabetes Study 16: overview of 6 years' therapy of type II diabetes: a progressive disease. Diabetes 1995; 44: 1249– 1258 [PubMed] [Google Scholar]
- 9. Holman RR: Assessing the potential for alpha-glucosidase inhibitors in prediabetic states. Diabetes Res Clin Pract 1998; 40 ( Suppl. 1): S21– S25 [DOI] [PubMed] [Google Scholar]
- 10. Butler AE, Janson J, Bonner-Weir S, Ritzel R, Rizza RA, Butler PC: Beta-cell deficit and increased beta-cell apoptosis in humans with type 2 diabetes. Diabetes 2003; 52: 102– 110 [DOI] [PubMed] [Google Scholar]
- 11. Nathan DM, Buse JB, Davidson MB, Heine RJ, Holman RR, Sherwin R, Zinman B: Management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 2006; 29: 1963– 1972 [DOI] [PubMed] [Google Scholar]
- 12. Brown AF, Gregg EW, Stevens MR, Karter AJ, Weinberger M, Safford MM, Gary TL, Caputo DA, Waitzfelder B, Kim C, Beckles GL: Race, ethnicity, socioeconomic position, and quality of care for adults with diabetes enrolled in managed care: the Translating Research Into Action for Diabetes (TRIAD) study. Diabetes Care 2005; 28: 2864– 2870 [DOI] [PubMed] [Google Scholar]
- 13. Turner RC, Cull CA, Frighi V, Holman RR: Glycemic control with diet, sulfonylurea, metformin, or insulin in patients with type 2 diabetes mellitus: progressive requirement for multiple therapies (UKPDS 49): UK Prospective Diabetes Study (UKPDS) Group. JAMA 1999; 281: 2005– 2012 [DOI] [PubMed] [Google Scholar]
- 14. Massi-Benedetti M, Orsini-Federici M: Treatment of type 2 diabetes with combined therapy: what are the pros and cons?. Diabetes Care 2008; 31 ( Suppl. 2): S131– S135 [DOI] [PubMed] [Google Scholar]
- 15. Monnier L, Lapinski H, Colette C: Contributions of fasting and postprandial plasma glucose increments to the overall diurnal hyperglycemia of type 2 diabetic patients: variations with increasing levels of HbA(1c). Diabetes Care 2003; 26: 881– 885 [DOI] [PubMed] [Google Scholar]
- 16. Monnier L, Colette C, Dunseath GJ, Owens DR: The loss of postprandial glycemic control precedes stepwise deterioration of fasting with worsening diabetes. Diabetes Care 2007; 30: 263– 269 [DOI] [PubMed] [Google Scholar]
- 17. Bretzel RG, Nuber U, Landgraf W, Owens DR, Bradley C, Linn T: Once-daily basal insulin glargine versus thrice-daily prandial insulin lispro in people with type 2 diabetes on oral hypoglycaemic agents (APOLLO): an open randomised controlled trial. Lancet 2008; 371: 1073– 1084 [DOI] [PubMed] [Google Scholar]
- 18. European Diabetes Policy Group. A desktop guide to type 2 diabetes mellitus. Diabet Med 1999; 16: 716– 730 [PubMed] [Google Scholar]
- 19. Bradley C, Lewis KS: Measures of psychological well-being and treatment satisfaction developed from responses of people with tablet-treated diabetes. Diabet Med 1990; 7: 445– 451 [DOI] [PubMed] [Google Scholar]
- 20. Holman RR, Thorne KI, Farmer AJ, Davies MJ, Keenan JF, Paul S, Levy JC: for the 4-T Study Group: Addition of biphasic, prandial, or basal insulin to oral therapy in type 2 diabetes. N Engl J Med 2007; 357: 1716– 1730 [DOI] [PubMed] [Google Scholar]
- 21. The EuroQol Group: EuroQol: a new facility for the measurement of health-related quality of life. Health Policy 1990; 16: 199– 208 [DOI] [PubMed] [Google Scholar]
- 22. Hirsch IB, Bergenstal RM, Parkin CG, Wright E, Jr, Buse JB: A real-world approach to insulin therapy in primary care practice. Clinical Diabetes 2005; 23: 78– 86 [Google Scholar]
- 23. Brunzell JD, Robertson RP, Lerner RL, Hazzard WR, Ensinck JW, Bierman EL, Porte D, Jr: Relationships between fasting plasma glucose levels and insulin secretion during intravenous glucose tolerance tests. J Clin Endocrinol Metab 1976; 42: 222– 229 [DOI] [PubMed] [Google Scholar]
- 24. Riddle MC, Rosenstock J, Gerich J: The treat-to-target trial: randomized addition of glargine or human NPH insulin to oral therapy of type 2 diabetic patients. Diabetes Care 2003; 26: 3080– 3086 [DOI] [PubMed] [Google Scholar]
- 25. Fonseca V, Bell DS, Berger S, Thomson S, Mecca TE: A comparison of bedtime insulin glargine with bedtime neutral protamine hagedorn insulin in patients with type 2 diabetes: subgroup analysis of patients taking once-daily insulin in a multicenter, randomized, parallel group study. Am J Med Sci 2004; 328: 274– 280 [DOI] [PubMed] [Google Scholar]
- 26. Eliaschewitz FG, Calvo C, Valbuena H, Ruiz M, Aschner P, Villena J, Ramirez LA, Jimenez J: HOE 901/4013 LA Study Group: Therapy in type 2 diabetes: insulin glargine vs. NPH insulin both in combination with glimepiride. Arch Med Res 2006; 37: 495– 501 [DOI] [PubMed] [Google Scholar]
- 27. Yki-Järvinen H, Kaupinnen-Mäkelin R, Tiikainen M, Vähätalo M, Virtamo H, Nikkilä K, Tulokas T, Hulme S, Hardy K, McNulty S, Hänninen J, Levänen H, Lahdenperä S, Lehtonen R, Ryysy L: Insulin glargine or NPH combined with metformin in type 2 diabetes: the LANMET study. Diabetologia 2006; 49: 442– 451 [DOI] [PubMed] [Google Scholar]
- 28. Fritsche A, Schweitzer MA, Häring HU: Glimepiride combined with morning insulin glargine, bedtime neutral protamine hagedorn insulin, or bedtime insulin glargine in patients with type 2 diabetes: a randomized, controlled trial. Ann Intern Med 2003; 138: 952– 959 [DOI] [PubMed] [Google Scholar]
- 29. Pan CY, Sinnassamy P, Chung KD, Kim KW: Insulin glargine versus NPH insulin therapy in Asian type 2 diabetes patients. Diabetes Res Clin Pract 2007; 76: 111– 118 [DOI] [PubMed] [Google Scholar]
- 30. Rosenstock J, Dailey G, Massi-Benedetti M, Fritsche A, Lin Z, Salzman A: Reduced hypoglycemia risk with insulin glargine: a meta-analysis comparing insulin glargine with human NPH insulin in type 2 diabetes. Diabetes Care 2005; 28: 950– 955 [DOI] [PubMed] [Google Scholar]
- 31. Linn T, Fischer B, Soydan N, Eckhard M, Ehl J, Kunz C, Bretzel RG: Nocturnal glucose metabolism after bedtime injection of insulin glargine or NPH insulin in patients with type 2 diabetes. J Clin Endocrinol Metab 2008; 93: 3839– 3846 [DOI] [PubMed] [Google Scholar]
- 32. Lepore M, Pampanelli S, Fanelli C, Porcellati F, Bartocci L, Di Vincenzo A, Cordoni C, Costa E, Brunetti P, Bolli GB: Pharmacokinetics and pharmacodynamics of subcutaneous injection of long-acting human insulin analog glargine, NPH insulin, and ultralente human insulin and continuous subcutaneous infusion of insulin lispro. Diabetes 2000; 49: 2142– 2148 [DOI] [PubMed] [Google Scholar]
- 33. Rosenstock J, Fonseca V, McGill JB, Riddle M, Hallé JP, Hramiak I, Johnston P, Davis M: Similar progression of diabetic retinopathy with insulin glargine and neutral protamine Hagedorn (NPH) insulin in patients with type 2 diabetes. Diabetologia. 13 June 2009. [ Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Peyrot M, Rubin RR, Lauritzen T, Skovlund SE, Snoek FJ, Matthews DR, Landgraf R, Kleinebreil L: The International DAWN Advisory Panel: Resistance to insulin therapy among patients and providers: results of the cross-national Diabetes Attitudes, Wishes, and Needs (DAWN) study. Diabetes Care 2005; 29: 952– 953 [DOI] [PubMed] [Google Scholar]
- 35. Davies M, Storms F, Shutler S, Bianchi-Biscay M, Gomis R: The ATLANTUS Study Group: Improvement of glycemic control in subjects with poorly controlled type 2 diabetes: comparison of two treatment algorithms using insulin glargine. Diabetes Care 2005; 28: 1282– 1288 [DOI] [PubMed] [Google Scholar]
- 36. Schreiber SA, Haak T: Insulin glargine benefits patients with type 2 diabetes inadequately controlled on oral antidiabetic treatment: an observational study of everyday practice in 12,216 patients. Diabet Obes Metab 2006; 9: 31– 38 [DOI] [PubMed] [Google Scholar]
- 37. Raccah D, Bretzel RG, Owens D, Riddle M: When basal insulin therapy in type 2 diabetes mellitus is not enough: what next? Diabete Metab Res Rev 2007; 23: 257– 264 [DOI] [PubMed] [Google Scholar]
- 38. Lankisch MR, Ferlinz KC, Leahy JL, Scherbaum WA: Orals Plus Apidra and LANTUS (OPAL) Study Group. Introducing a simplified approach to insulin therapy in type 2 diabetes: a comparison of two single-dose regimens of insulin glulisine plus insulin glargine and oral antidiabetic drugs. Diabetes Obes Metab 2008; 10: 1178– 1185 [DOI] [PubMed] [Google Scholar]
- 39. Nathan DM, Buse JB, Davidson MB, Ferrannini E, Holman RR, Sherwin R, Zinman B: American Diabetes Association, European Association for the Study of Diabetes Medical management of hyperglycemia in type 2 diabetes: a consensus algorithm or the initiation and adjustment of therapy: a consensus statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 2009; 32: 193– 203 [DOI] [PMC free article] [PubMed] [Google Scholar]