In 2003, the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC VII) published its ultimate guidelines for hypertension prevention and management (1). One of the key messages was the definition of a new category of blood pressure (BP) levels, i.e., prehypertension, that included individuals with a systolic BP of 120–139 mmHg or a diastolic BP of 80–89 mmHg. Patients with prehypertension were considered at increased risk for progression to hypertension and individuals in the 130/80 to 139/89 mmHg range were at twice the risk of developing hypertension than subjects with lower values (2). In the same year, the European Society of Hypertension and the European Society of Cardiology (ESH-ESC) published their guidelines for the management of arterial hypertension and, for the same range of BP, two different categories of BP were defined: normal BP (systolic BP of 120–129 mmHg, or diastolic BP of 80–84 mmHg) and high-normal BP (systolic BP of 130–139 mmHg, or diastolic BP of 85–89 mmHg) (3).
In 2007, the ESH-ESC committee decided against using the term “prehypertension” for several reasons (4). First, even in the Framingham study, the risk of developing hypertension was definitely higher in subjects with high-normal BP than in patients with normal BP (2,5), and therefore there is little reason to combine the two groups. Second, given the ominous significance of the word “hypertension” for the layman, the term “prehypertension” may, in many subjects, create anxiety and a request for unnecessary medical visits and examinations. Finally, although lifestyle changes recommended by the 2003 JNC VII guidelines for all prehypertensive individuals may be a valuable population strategy (1), in practice, this category is a highly differentiated one, with the extremes consisting of subjects with no need of any intervention (e.g., an elderly individual with a BP of 120/80 mmHg), as well as of those with a very high or high cardiovascular risk profile (e.g., after stroke or with diabetes), in whom drug treatment is required.
Because the evidence of BP-lowering benefits in patients with high-normal BP were limited to subjects with stroke (6), coronary artery disease (7), and diabetes (8), antihypertensive treatment within this BP range was only recommended for patients at high risk (3). In 2007, the updated ESH-ESC guidelines recognized patients presenting with diabetes or metabolic syndrome as high or very-high-risk patients (4). The present review will focus on the benefits of antihypertensive therapy in patients with diabetes, or metabolic syndrome and high-normal BP.
HIGH-NORMAL BP AND CARDIOVASCULAR RISK
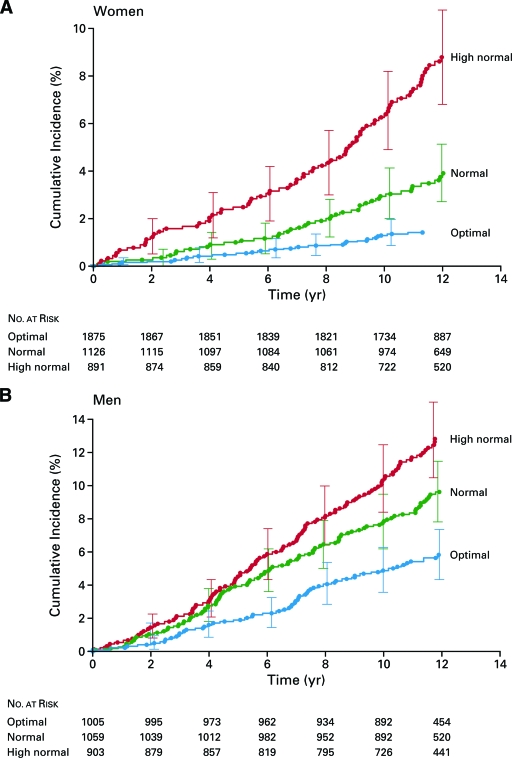
Several epidemiologic studies have demonstrated that systolic and diastolic BP values have a strong continuous graded and etiologically significant positive association with cardiovascular disease (CVD) outcomes (9). Although subjects with high-normal BP are likely to have an elevated risk of CVD (given the continuum of risk), there was a paucity of information regarding the absolute and relative risks of CVD in these individuals. Vasan et al. (5) published a prospective examination of the risk of CVD in men and women with high-normal BP, intended to investigate the association between BP category at baseline, and the incidence of CVD on follow-up among 6,859 participants in the Framingham Heart Study. During a mean follow-up of 11.1 years, 397 study subjects had a first cardiovascular event, including 72 deaths from CVD, 190 recognized myocardial infarctions, 85 strokes, and 50 cases of congestive heart failure. Cardiovascular event rates increased in a stepwise manner across the three BP categories (optimal, normal, and high-normal BP) (5) (Fig. 1). Compared with optimal BP, high-normal BP was associated with a risk factor adjusted hazard ratio (HR) for CVD of 2.5 (95% CI 1.6–4.1) among women and 1.6 (1.1–2.2) among men (5).
Figure 1.
Cumulative incidence of cardiovascular events in women (A) and men (B) according to BP category. From Vasan et al. (5).
Moreover, among subjects with no previous vascular disease, the usual BP values are positively related to the risks of death from vascular disease, not only among hypertensive patients or subjects with high-normal BP, but also among those who would usually be considered normotensive (at least down to usual BP levels of 115/75 mmHg) (10). Given the continuous relationship observed between BP and risk of death from vascular disease, the absolute benefits of a lower BP level are likely to be greatest for those at maximum absolute risk of vascular disease (10). At ages 40–69 years, each difference of 20 mmHg usual systolic BP (or approximately equivalent to 10 mmHg usual diastolic BP) is associated with more than a twofold difference in stroke death rate and with twofold differences in the death rates from ischemic heart disease and other vascular causes. All these proportional differences in vascular mortality are about half as extreme at ages 80–89 years than at ages 40–49 years, but the annual absolute differences in risk are greater in old age (10).
Although the relationship between BP categories and cardiovascular risk is firmly established, there is scarce evidence concerning the risk of cardiovascular events in subjects with progressive BP increase and in whom new onset of hypertension occurs. This question is important, because people with BP levels in the normal and high-normal range have a substantial risk of developing hypertension over a short-term period. In the Framingham cohort, after a 4-year follow-up, the hypertension incidence rates progressed according to baseline BP category and age: among younger people (age 35–64 years) with optimum, normal, or high-normal baseline BP, the 4-year rates of hypertension were 5.3, 17.6, and 37.3%, respectively; among older people (age 65–94 years), these rates were 16.0, 25.5, and 49.5%, respectively (2). Data from the Women's Health Study have shown that 30.1% of women without baseline hypertension progressed to hypertension (11). The age-adjusted event rate for the primary end point was 1.6/1,000 person-years among women with normal BP, 2.9/1,000 person-years among those with high-normal BP, and 4.3/1,000 person-years among those with baseline hypertension. Compared with women with high-normal BP, those with normal BP had a lower risk of a major cardiovascular event (adjusted HR 0.61, 95% CI 0.48–0.76) and of incident hypertension (0.42, 0.40–0.44). The HR for a major cardiovascular event in women with baseline hypertension was 1.30 (1.08–1.57). Women who progressed to hypertension during the first 48 months of the study had a higher cardiovascular risk than those who remained normotensive (adjusted HR 0.64, 0.50–0.81). Women with high-normal BP at baseline who progressed to hypertension had similar outcome rates to those with baseline hypertension (adjusted HR 1.17, 0.88–1.55) (11). Recent population data confirm that a substantial proportion of CVD is attributable to high BP. This burden applies to different economic regions, age-groups, and BP levels and is not limited to subjects with hypertension, in view of the large number of people with high BP, but who are not classified as hypertensive (12). Worldwide, 7.6 million premature deaths (∼13.5% of the global total) and 92 million disability-adjusted life-years (6.0% of the global total) were attributed to high BP. About 50% of this affliction occurred in individuals with hypertension, but the remainder was in individuals with lesser degrees of high BP (12).
BP VALUES AND CONCOMITANT RISK FACTORS
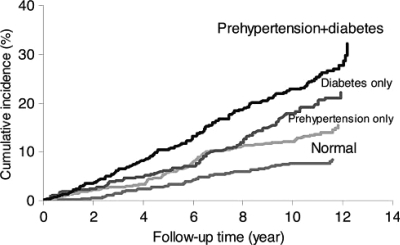
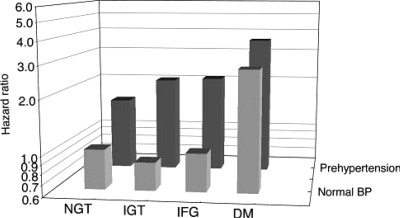
Only a small fraction of the hypertensive population has an elevation of BP alone, with the great majority exhibiting additional cardiovascular risk factors, with a relationship between the severity of the BP elevation and that of alterations in glucose and lipid metabolism. Furthermore, when concomitantly present, BP and metabolic risk factors potentiate each other, leading to a total cardiovascular risk that is greater than the sum of its individual components (4). In fact, after the algorithm of ESH-ESC to stratify cardiovascular risk, subjects with high-normal BP presenting three additional cardiovascular risk factors, metabolic syndrome, or diabetes are considered as high-risk patients (Fig. 2) (4). The Strong Heart Study demonstrated that prehypertension was more prevalent in diabetic than nondiabetic participants (59.4 versus 48.2%), and patients presenting with both diabetes and prehypertension had the highest cumulative incidence of CVD during follow-up (Fig. 3) (13). In nondiabetic participants, prehypertension increased cardiovascular events 1.8-fold compared with their normotensive counterparts. Diabetes alone increased the risk of CVD by 2.9-fold compared with normotensive nondiabetic participants. Diabetes plus prehypertension increased the CVD risk by 3.7-fold. When the prehypertensive category was stratified into those with normal or high-normal BP, HRs for those in the higher group were greater, but there was a significant risk even in those in the lower group. The coexistence of impaired glucose tolerance, or impaired fasting glucose and prehypertension, also increased CVD risk significantly compared with normotensive participants with normal glucose tolerance (Fig. 4) (13).
Figure 2.
Stratification of cardiovascular (CV) risk in four categories. From Mancia et al. (4). DBP, diastolic blood pressure; HT, hypertension; MS, metabolic syndrome; OD, subclinical organ damage; SBP, systolic blood pressure.
Figure 3.
Cumulative CVD incidence during 12 years of follow-up by prehypertension and diabetes status in the Strong Heart Study cohort. From Zhang et al. (13).
Figure 4.
Hazard ratios for incident CVD associated with prehypertension and glucose metabolic abnormalities on a logarithmic scale. From Zhang et al. (13). DM, diabetes; IFG, impaired fasting glucose; IGT, impaired glucose tolerance; NGT, normal glucose tolerance.
HIGH-NORMAL BP AND ANTIHYPERTENSIVE THERAPY
The recommendation to initiate treatment in diabetic patients when BP is still in the high-normal range, and to reduce BP to <130/80 mmHg, is supported by European Guidelines (4). The same can be considered for patients with three or more cardiovascular risk factors, presence of target organ damage, or metabolic syndrome. Considering that the presence of the metabolic syndrome is related to an increased cardiovascular risk (14,15), it is possible that hypertensive patients with metabolic syndrome would obtain an additional benefit on cardiovascular prognosis with the achievement of a more aggressive BP goal, similar to that of diabetic patients. The clinical evidence that influenced our attitude toward treating a patient was fundamentally obtained from studies aimed at identifying significant differences on the final consequences of cardiovascular and renal diseases (nonfatal events, chronic or terminal renal insufficiency, and cardiovascular mortality). Nevertheless, cardiovascular and renal diseases have developed progressively throughout many years. This process is accompanied by a parallel progression of atherosclerosis that finally will be converted into atherothrombotic events, which are the fundamental cause of fatal and nonfatal cardiovascular and renal events. Therefore, early detection of an elevated cardiovascular risk through the clustering of cardiovascular risk factors and/or the presence of target organ damage should be followed by prompt intervention. In fact, the Losartan Intervention for End point Reduction (LIFE) study clearly demonstrated that regression of electrocardiographic left ventricular hypertrophy with antihypertensive treatment improved prognosis, independent of BP (16). Moreover, the multicenter double-blind randomized Bergamo Nephrologic Diabetes Complications Trial (BENEDICT) was designed to assess whether ACE inhibitors and nondihydropyridine calcium-channel blockers, alone or in combination, prevent microalbuminuria in subjects with hypertension, type 2 diabetes, and normal urinary albumin excretion (17). The primary end point was the development of persistent microalbuminuria (overnight albumin excretion, ≥20 μg/min at two consecutive visits). This end point was reached in 5.7% of the subjects who received trandolapril plus verapamil, 6.0% trandolapril, 11.9% verapamil, and 10.0% of control subjects who received placebo. In conclusion, in subjects with type 2 diabetes and arterial hypertension, normoalbuminuria, and normal renal function, ACE inhibitor therapy with trandolapril plus verapamil, or trandolapril alone, prevented the onset of microalbuminuria. In our experience, the implementation of guidelines for management of essential hypertension and cardiovascular risk factors facilitates the achievement of similar BP and LDL cholesterol goals, in patients with and without metabolic syndrome. However, it seems that global cardiovascular risk would remain higher in treated hypertensive subjects presenting with metabolic syndrome, as suggested by a threefold higher incidence of new-onset diabetes and double prevalence of positive microalbuminuria (18).
High-normal BP and the initial stage of isolated systolic hypertension represent two situations in which doctors frequently are reluctant to start pharmacologic therapy, albeit according to guidelines, this could clearly be beneficial (19). In diabetic patients with high-normal BP, the American Diabetes Association recommends lifestyle therapy alone for a maximum of 3 months, and then, if targets are not achieved, patients should be treated with the addition of pharmacological agents (20). Updated ESH-ESC guidelines recommend lifestyle changes plus drug treatment at the outset (4).
Subjects with a high cardiovascular risk due to factors other than diabetes, but a BP still in the high-normal range, should be advised to implement intense lifestyle measures (including smoking cessation), and BP should be closely monitored because of the relatively high chance these individuals have of developing hypertension, which would then require drug treatment. However, physicians and patients may sometimes consider antihypertensive drugs, particularly those more effective in protecting against organ damage, new-onset hypertension, and new-onset diabetes (4). In fact, pharmacologic treatment of prehypertension may prevent or postpone the development of hypertension. The TROPHY (Trial of Preventing Hypertension) trial showed a significant reduction in incident hypertension in participants with prehypertension who had received candesartan. The relative proportion of participants who were hypertension-free was 26.5% greater in the candesartan group (21). Chronic blockade of the renin-angiotensin system appears to be particularly effective in preventing renal and cardiovascular events in patients with type 2 diabetes. Patients with hypertension are at increased cardiovascular risk, which is amplified by the coexistence of type 2 diabetes. Blockade of the renin-angiotensin system lowers BP in both hypertensive and diabetic individuals, suggesting the underlying contribution of angiotensin II to the pathogenesis of these conditions and, possibly, of their renal and cardiovascular complications. This is compatible with the fact that angiotensin II has been recognized as playing a deleterious role early in the course of the atherosclerotic process (22). It appears, therefore, highly desirable to block the renin-angiotensin system in all patients with hypertension and/or type 2 diabetes. Ideally, this should be done early during the course of the disease, since blockers of the renin-angiotensin system are effective in reducing oxidative stress, plasma concentrations of inflammatory mediators, and plasminogen activator inhibitor 1, as well as in improving endothelial function, i.e., abnormalities that may be encountered before the existence of structural vascular damage (23). Blockers of the renin-angiotensin system have an additional advantage compared with other classes of antihypertensive agents: they improve insulin sensitivity and may protect against the progressive impairment of β-cell secretory function observed in patients with type 2 diabetes (24). This beneficial effect may be related in part to the prevention of the angiotensin II–mediated increase in oxidative stress. In pre-diabetic patients, it has been known that diuretic therapy, particularly when combined with a β-blocker, diminishes glucose tolerance and increases the risk of new-onset diabetes, and by contrast, treatment with antihypertensive drugs such as ACE inhibitors, or angiotensin-receptor blockers, and to a lesser extent calcium antagonists, seems to decrease this risk (25). It appears increasingly justified that the use of these drugs in patients with metabolic syndrome should be extended, since inhibition of the renin-angiotensin system not only lowers BP, but also reduces the incidence of new-onset type 2 diabetes (25).
CONCLUSIONS
Epidemiologic studies have demonstrated that systolic and diastolic BP values have a strong, continuous, graded, and etiologically significant positive association with CVD outcomes. This is especially relevant among subjects with high-normal BP, considering that most will or will not receive a more aggressive pharmacologic therapy to control BP values, depending on the presence or absence of concomitant comorbidities (diabetes, clustering of cardiovascular risk factors, target organ damage, and metabolic syndrome). It is well established that the use of pharmacologic therapy from the early stages of BP in these patients will greatly facilitate the achievement of adequate BP control, which will contribute to the prevention of cardiovascular complications.
Acknowledgments
No potential conflicts of interest relevant to this article were reported.
Footnotes
The publication of this supplement was made possible in part by unrestricted educational grants from Eli Lilly, Ethicon Endo-Surgery, Generex Biotechnology, Hoffmann-La Roche, Johnson & Johnson, LifeScan, Medtronic, MSD, Novo Nordisk, Pfizer, sanofi-aventis, and WorldWIDE.
References
- 1. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, Jones DW, Materson BJ, Oparil S, Wright JT, Jr, Roccella EJ: Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee. Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003; 42: 1206– 1252 [DOI] [PubMed] [Google Scholar]
- 2. Vasan RS, Larson MG, Leip EP, Kannel WB, Levy D: Assessment of frequency of progression to hypertension in non-hypertensive participants in the Framingham Heart Study: a cohort study. Lancet 2001; 358: 1682– 1686 [DOI] [PubMed] [Google Scholar]
- 3. European Society of Hypertension-European Society of Cardiology Guidelines Committee 2003 European Society of Hypertension-European Society of Cardiology guidelines for the management of arterial hypertension. J Hypertens 2003; 21: 1011– 1053 [DOI] [PubMed] [Google Scholar]
- 4. Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, Grassi G, Heagerty AM, Kjeldsen SE, Laurent S, Narkiewicz K, Ruilope L, Rynkiewicz A, Schmieder RE, Boudier HA, Zanchetti A, Vahanian A, Camm J, De Caterina R, Dean V, Dickstein K, Filippatos G, Funck-Brentano C, Hellemans I, Kristensen SD, McGregor K, Sechtem U, Silber S, Tendera M, Widimsky P, Zamorano JL, Erdine S, Kiowski W, Agabiti-Rosei E, Ambrosioni E, Lindholm LH, Viigimaa M, Adamopoulos S, Agabiti-Rosei E, Ambrosioni E, Bertomeu V, Clement D, Erdine S, Farsang C, Gaita D, Lip G, Mallion JM, Manolis AJ, Nilsson PM, O'Brien E, Ponikowski P, Redon J, Ruschitzka F, Tamargo J, van Zwieten P, Waeber B, Williams B: Management of Arterial Hypertension of the European Society of Hypertension; European Society of Cardiology: 2007 Guidelines for the Management of Arterial Hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2007; 25: 1105– 1187 [DOI] [PubMed] [Google Scholar]
- 5. Vasan RS, Larson MG, Leip EP, Evans JC, O'Donnell CJ, Kannel WB, Levy D: Impact of high-normal blood pressure on the risk of cardiovascular disease. N Engl J Med 2001; 345: 1291– 1297 [DOI] [PubMed] [Google Scholar]
- 6. PROGRESS Collaborative Study Group: Randomised trial of perindopril based blood pressure-lowering regimen among 6108 individuals with previous stroke or transient ischaemic attack. Lancet 2001; 358: 1033– 1041 [DOI] [PubMed] [Google Scholar]
- 7. Yusuf S, Sleight P, Pogue J, Bosch J, Davies R, Dagenais G: Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients: the Heart Outcomes Prevention Evaluation Study Investigators. N Engl J Med 2000; 342: 145– 153 [DOI] [PubMed] [Google Scholar]
- 8. Schrier RW, Estacio RO, Esler A, Mehler P: Effects of aggressive blood pressure control in normotensive type 2 diabetic patients on albuminuria, retinopathy and stroke. Kidney Int 2002; 61: 1086– 1097 [DOI] [PubMed] [Google Scholar]
- 9. Stamler J, Stamler R, Neaton JD: Blood pressure, systolic and diastolic, and cardiovascular risks: US population data. Arch Intern Med 1993; 153: 598– 615 [DOI] [PubMed] [Google Scholar]
- 10. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R: Prospective Studies Collaboration: age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002; 360: 1903– 1913 [DOI] [PubMed] [Google Scholar]
- 11. Conen D, Ridker PM, Buring JE, Glynn RJ: Risk of cardiovascular events among women with high normal blood pressure or blood pressure progression: prospective cohort study. BMJ 2007; 335: 432– 440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lawes CM, Van der Hoorn S, Rodgers A: for the International Society of Hypertension. Global burden of blood-pressure-related disease, 2001. Lancet 2008; 371: 1515– 1518 [DOI] [PubMed] [Google Scholar]
- 13. Zhang Y, Lee ET, Devereux RB, Yeh J, Best LG, Fabsitz RR, Howard BV: Prehypertension, diabetes, and cardiovascular disease risk in a population-Based Sample: The Strong Heart Study. Hypertension 2006; 47: 410– 414 [DOI] [PubMed] [Google Scholar]
- 14. Ford ES: Risk for all-cause mortality, cardiovascular disease, and diabetes associated with the metabolic syndrome: a summary of the evidence. Diabetes Care 2005; 28: 1769– 1778 [DOI] [PubMed] [Google Scholar]
- 15. Eberly LE, Prineas R, Cohen JD, Vazquez G, Zhi X, Neaton JD, Kuller LH: Multiple Risk Factor Intervention Trial Research Group Metabolic syndrome: risk factor distribution and 18-year mortality in the multiple risk factor intervention trial. Diabetes Care 2006; 29: 123– 130 [DOI] [PubMed] [Google Scholar]
- 16. Devereux RB, Wachtell K, Gerdts E, Boman K, Nieminen MS, Papademitriou V, Rokkedal J, Harris K, Aurup P, Dahlöf B: Prognostic significance of left ventricular mass change during treatment of hypertension. JAMA 2004; 292: 2350– 2356 [DOI] [PubMed] [Google Scholar]
- 17. Ruggenenti P, Fassi A, Ilieva AP, Bruno S, Iliev IP, Grusegan V, Rubis N, Gherardi G, Arnoldi F, Ganeva M, Ene-Iordache B, Gaspari F, Perna A, Bossi A, Trevisan R, Dodesini AR, Remuzzi G: Bergamo Nephrologic Diabetes Complications Trial (BENEDICT) Investigators: Preventing microalbuminuria in type 2 diabetes. N Engl J Med 2004; 351: 1941– 1951 [DOI] [PubMed] [Google Scholar]
- 18. Segura J, Banegas JR, Garcia-Donaire JA, Rodriguez-Artalejo F, de la Cruz JJ, Praga M, Ruilope LM: Should hypertension guidelines be changed for hypertensive patients with the metabolic syndrome? J Clin Hypertens (Greenwich) 2007; 9: 595– 600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ruilope LM, Usan L, Segura J, Bakris GL: Intervention at lower blood pressure levels to achieve target goals in type 2 diabetes: PRADID (PResión Arterial en DIabéticos tipo DOS) study. J Hypertens 2004; 22: 217– 222 [DOI] [PubMed] [Google Scholar]
- 20. American Diabetes Association: Executive summary: standards of medical care in diabetes: 2008. Diabetes Care 2008; 31 ( Suppl. 1): S5– S11 [DOI] [PubMed] [Google Scholar]
- 21. Julius S, Nesbitt SD, Egan BM, Weber MA, Michelson EL, Kaciroti N, Black HR, Grimm RH, Messerli FH, Oparil S, Schork MA: Trial of Preventing Hypertension (TROPHY) Study Investigators: Feasibility of treating prehypertension with an angiotensin-receptor blocker. N Engl J Med 2006; 354: 1685– 1697 [DOI] [PubMed] [Google Scholar]
- 22. Schmieder RE, Hilgers KF, Schlaich MP, Schmidt BM: Renin-angiotensin system and cardiovascular risk. Lancet 2007; 369: 1208– 1219 [DOI] [PubMed] [Google Scholar]
- 23. Duprez DA: Role of the renin-angiotensin-aldosterone system in vascular remodeling and inflammation: a clinical review. J Hypertens 2006; 24: 983– 991 [DOI] [PubMed] [Google Scholar]
- 24. Leung PS: Mechanisms of protective effects induced by blockade of the renin-angiotensin system: novel role of the pancreatic islet angiotensin-generating system in type 2 diabetes. Diabetes Med 2007; 24: 110– 116 [DOI] [PubMed] [Google Scholar]
- 25. Elliot WJ, Meyer PM: Incident diabetes in clinical trials of antihypertensive drugs: a network meta-analysis. Lancet 2007; 369: 201– 207 [DOI] [PubMed] [Google Scholar]