Abstract
Hypoxia-inducible factor-1α (HIF-1α) and the neo-angiogenic factors induced as a result of hypoxia-inducible factor transcriptional activation may contribute to tumorigenesis by inducing vessel formation that in turn provides oxygen and nutrients promoting tumor expansion. In vitro studies of nasopharyngeal carcinoma (NPC), an aggressive malignancy that is nearly always infected by Epstein–Barr virus, show HIF-1α is upregulated by viral latent membrane protein 1 (LMP1). The current study used immunohistochemistry to examine the extent to which HIF-1α and LMP1 are co-expressed in naturally infected NPC tissues. Analytic procedures were optimized for sensitive localization of HIF-1α and LMP1 in fixed tissue sections using immunohistochemistry with sensitive fluorescent and signal amplification technologies. Vessel density was quantified by CD31 immunohistochemistry. LMP1 was expressed focally in all 18 NPCs examined, including 7/8 in situ lesions. There was no consistent co-localization with HIF-1α which was usually only weakly expressed in a subset of neoplastic cells. Neither LMP1 nor HIF-1α expression correlated with vessel density, and degree of vascularization varied widely among cases. Advanced immunohistochemical technologies reveal that LMP1 is expressed more commonly than previously reported in NPC. There is no consistent relationship between LMP1 and either HIF-1α expression or degree of microvasculature. The biologic basis for the wide variation in vessel density deserves further investigation.
Keywords: Nasopharyngeal carcinoma, HIF-1α, Angiogenesis, Immunohistochemistry
Introduction
Neoplasms frequently induce formation of new blood vessels, supplying nutrients and oxygen that facilitate cell growth and invasion. Insufficient neo-angiogenesis may result in tumor necrosis, and a potential strategy for treating cancer is to prevent new vessel formation using pharmacologic means. Angiogenic blockers are now used therapeutically in renal cell carcinoma and in HHV8-related Kaposi’s sarcoma in which the virus is thought to drive vascularization via VEGF [1, 2].
Epstein-Barr virus (EBV) is strongly associated with nasopharyngeal carcinoma (NPC) as evidenced by the presence of EBV DNA within the malignant cells in the majority of cases [3, 4]. EBV infection and neo-angiogenesis in NPC has been previously explored by counting microvessel density and by immunohistochemical analysis of vascular endothelial growth factor (VEGF) expression, and it was found that vessel density and VEGF expression were higher in NPC compared to normal nasopharyngeal tissue [5]. In addition, there was significantly more invasion and metastasis in EBV-infected tumors compared to EBV-negative carcinomas, particularly in older patients [6]. This could be explained, at least in part, by modulation of signaling cascades by EBV in response to hypoxia, as suggested by Lo et al. [7].
Angiogenesis is mediated by a series of proteins beginning with hypoxia-inducible factors 1α and 2α (HIF-1α and HIF-2α) which are transcription factors that respond to changes in available oxygen in the cellular environment. HIF-1α in turn, affects transcription of genes encoding VEGF, carbonic anhydrase IX (CAIX), and matrix metalloproteinase 9 (MMP9) among a transcriptional repertoire of dozens of targets mediating neo-angiogenesis and metastasis [8]. An immunohistochemical study by Hui et al. [9] found poorer survival among NPC patients whose tumors had high HIF-1α expression. The link between HIF-1α expression and survival has also been reported in other cancers including breast cancer [10, 11].
Latent Membrane Protein 1 (LMP1) is considered to be among the most likely EBV proteins to contribute to oncogenesis and tumor maintenance [12, 13]. A relation between LMP1 expression and increased HIF-1α expression was found by Wakisaka et al. [14] in both lymphoblastoid and epithelial cell lines. Subsequently Kondo et al. [15] showed the mechanism by which LMP1 functions—it stabilizes SIAH1, an E3 ubiquitin ligase, which in turn ubiquitinates and destabilizes prolyl hydroxylase proteins (PHD1 and PHD3) that, under normoxic conditions, are responsible for hydroxylation and subsequent degradation of HIF-1α. In this manner, LMP1 expression effectively increases HIF-1α levels leading to downstream transcription of angiogenic factors.
The current study determines the extent to which LMP1 and HIF-1α expression are associated in naturally infected NPC tissues. Co-localization of LMP1 and HIF-1α would imply that the same biochemical pathways that are operative in cell line models are also operative in vivo, potentially contributing to angiogenesis, tumor growth, and propensity to metastasis in EBV-infected cancer patients. HIF-1α was detected by immunohistochemical analysis of formalin fixed paraffin-embedded biopsy tissue. Chromogenic and immunofluorescent histochemical approaches were compared to optimize sensitive detection of LMP1 expression, and CD31 was used to assist in morphologic quantification of vascularity.
Materials and Methods
Case Selection
Formalin-fixed, paraffin-embedded tissues from 21 NPC patients were retrieved from the archives of the Gadjah Madah University, Yogyakarta, Indonesia (n = 12 originating from Indonesian patients) and from the University of North Carolina at Chapel Hill (n = 9 originating from American patients). Some tumors were collected at initial diagnosis and others represented recurrence following therapy. Specimens were confirmed by a pathologist to represent NPC, and all tumors were previously documented to be EBV-related as shown by localization of EBV-encoded RNA (EBER1) and/or EBV nuclear antigen (EBNA1) to the malignant epithelial cells using the Ventana Benchmark ISH system (Tucson, AZ, USA) for EBER1 detection in the American cases, and the PNA ISH kit with EBER probe (DAKO, Glostrup, Denmark) or immunostaining with EBNA1 OT1X monoclonal antibody for the Indonesian cases [16]. Three cases (two Indonesian, one American) were excluded because of insufficient tumor tissue to complete all analyses, resulting in a total of 18 cases.
Chromogenic Immunohistochemical Stains for LMP1, HIF-1α and CD31
Latent membrane protein 1 (LMP1) was targeted using the mouse monoclonal cocktail CS1-4 (M0897; DAKO) at a dilution of 1:100, while HIF-1α was detected using rabbit polyclonal antibody (sc-10790; SantaCruz, Santa Cruz, CA, USA) at 1:100, and CD31 was detected using mouse monoclonal anti-human CD31 (DAKO) at 1:100. Citrate antigen retrieval (Citra, BioGenex, San Ramon, CA, USA) was performed in a microwave for 30 min, endogenous peroxidase activity was blocked (DAKO peroxidase block solution) for 20 min, and protein blocking (BioGenex) was performed for 10 min. Sections were incubated in primary antibody overnight at 4°C followed by detection using Super Sensitive Polymer-HRP IHCX Detection system (Biogenex) with diaminobenzidine as the substrate. The sections then were counterstained with hematoxylin, dehydrated, and mounted. Control tissues included EBER-positive Hodgkin lymphoma for LMP1, and renal cell carcinoma tissue for HIF-1α and CD31. Additional controls were renal cell carcinoma cell line pellets (RCC4 2-1 over expresses HIF-1α while RCC4 3-14 does not) that were fixed in formalin and paraffin embedded [17]. Specificity was assured in all specimens by parallel stains omitting the primary antibody.
Immunofluorescent Histochemical Stains for LMP1
To maximize low level detection, LMP1 protein was additionally evaluated by immunofluorescence using filters to visualize the relevant bandwidth of the marker. Antigen retrieval remained the same as described above for chromogenic stains. LMP1 was targeted using the same antibody cocktail at 1:100 and results were compared with a higher dilution of 1:500 in combination with the Tyramide Signal Amplification (TSA) kit (PerkinElmer, MA, USA) to enhance signal-to-noise ratio. Of note, DAKO’s catalyzed signal amplification (CSA) system in combination with Direct Labeled Secondary anti-mouse (DAKO) was also tested and produced similar results. Sections were treated with biotin-labeled secondary goat antibody (PerkinElmer) and streptavidin horseradish peroxidase (SA-HRP, BioGenex). For the TSA system additional biotin and avidin blocking steps were implemented (BioGenex). Fluorophore Cyanine 3 (PerkinElmer) reacted with HRP to allow visualization of the signal by immunofluorescent microscopy, and DAPI counterstain revealed nuclear and architectural features to help distinguish benign from malignant cells.
Scoring of Chromogenic and Immunofluorescent Histochemical Stains
For LMP1, only cytoplasmic and membrane signals were evaluated, whereas for HIF-1α only nuclear signals were evaluated since nuclear HIF-1α is presumed to be the active form of the transcription factor. The proportion score (PS) for neoplastic cells was expressed as a score of 0–5 where 0 is no staining, 1 is 1 out of 100 cells, 2 is 1 out of 10 cells, 3 is 1 out of 3 cells, 4 is 2 out of 3 cells, and 5 is virtually all cells. The intensity score (IS) for neoplastic cells was expressed on a scale of 0–3 where 0 is no staining at all, 1 is weak staining, 2 is intermediate, and 3 is strong staining. When intensity varied within a given neoplasm, the average intensity was judged. Total score was the sum of the PS and IS. The pre-malignant lesions were considered too small for accurate scoring, so results were interpreted qualitatively as positive or negative for each marker. To score the number of vessels in a 40× field, 5 different regions of the neoplasm were evaluated on a CD31-stained slide, and number of vessels was averaged to obtain a score from 0 to 3 where 0 is no vessels, 1 is 1–19 vessels, 2 is 20–39 vessels and 3 is higher than 40 vessels per 40× field.
Results
In a series of 18 Indonesian and American NPCs, every case was confirmed to have invasive carcinoma, and 12 also had premalignant lesions while three had only normal squamous and/or columnar surface epithelium, and another three lacked any surface epithelial component. Since small vessels were often difficult to discern on H&E stained sections, CD31 immunostains targeting endothelial cells assisted in counting the number of vessels in the areas with invasive carcinoma. The amount of microvasculature varied widely among cases from very few to over 40 vessels per 40× field (Table 1).
Table 1.
Expression of EBV LMP1 and HIF-1α, and vessel density in invasive nasopharyngeal carcinomas
| Case # | Geographic origin | Vasculature, CD31 | EBV LMP1* | HIF-1α | ||||
|---|---|---|---|---|---|---|---|---|
| Density score | Proportion score | Intensity score | Total score | Proportion score | Intensity score | Total score | ||
| 1 | Indonesia | 3 | 2 | 1 | 3 | 2 | 2 | 4 |
| 2 | USA | 3 | 2 | 1 | 3 | 1 | 1 | 2 |
| 3 | Indonesia | 3 | 1 | 2 | 3 | 1 | 1 | 2 |
| 4 | Indonesia | 2 | 3 | 2 | 5 | 1 | 1 | 2 |
| 5 | USA | 2 | 3 | 1 | 4 | 1 | 1 | 2 |
| 6 | Indonesia | 2 | 4 | 3 | 7 | 1 | 1 | 2 |
| 7 | Indonesia | 2 | 4 | 2 | 6 | 1 | 1 | 2 |
| 8 | Indonesia | 2 | 2 | 1 | 2 | 0 | 0 | 0 |
| 9 | USA | 1 | 3 | 2 | 5 | 1 | 1 | 2 |
| 10 | Indonesia | 1 | 1 | 2 | 3 | 1 | 1 | 2 |
| 11 | USA | 1 | 4 | 2 | 6 | 0 | 0 | 0 |
| 12 | Indonesia | 1 | 3 | 1 | 4 | 3 | 1 | 4 |
| 13 | USA | 1 | 3 | 1 | 4 | 0 | 0 | 0 |
| 14 | Indonesia | 1 | 1 | 1 | 2 | 1 | 1 | 2 |
| 15 | Indonesia | 1 | 1 | 2 | 3 | 1 | 1 | 2 |
| 16 | USA | 1 | 2 | 1 | 3 | 2 | 1 | 3 |
| 17 | Indonesia | 0 | 2 | 2 | 4 | 1 | 1 | 2 |
| 18 | USA | 0 | 2 | 1 | 3 | 2 | 1 | 3 |
| Total positive | 16/18 | 18/18 | 18/18 | 18/18 | 15/18 | 15/18 | 15/18 | |
LMP1 latent membrane protein 1; HIF-1α hypoxia inducible factor 1 alpha; USA United States of America
* LMP1 scores represent results of immunofluorescent stains using tyramide signal amplification
LMP1 Expression
Chromogenic staining showed focal LMP1 expression in some but not all NPCs. Immunofluorescent staining of LMP1 on the same tissues revealed a greater proportion and intensity of positive signals in malignant cells, suggesting that the fluorescent method was more sensitive than the chromogenic method. Furthermore, including the tyramide signal amplification step as compared to not implementing this step yielded even more robust detection of LMP1 protein among viable tumor cells (Fig. 1). When tested using the most sensitive detection method (immunofluorescence with signal amplification), LMP1 was expressed in all 18 invasive NPCs, usually at weak to moderate intensity and in patterns ranging from rare individual cells to over half of all tumor cells.
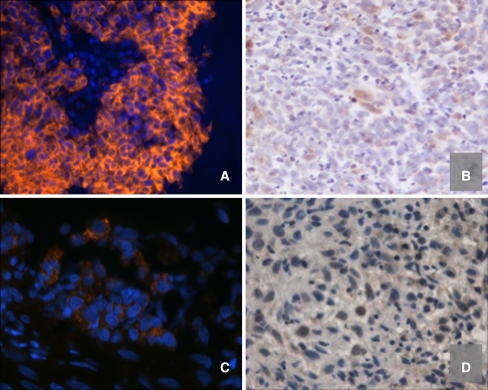
Fig. 1.
In invasive nasopharyngeal carcinomas, intensity of LMP1 expression does not correlate with HIF-1α expression. Panel A (case 6) shows relatively diffuse, strong cytoplasmic LMP1 localized to malignant cells, while panel B (case 6) shows focal weak nuclear HIF-1α expression in large malignant-appearing cells. Panel C (case 12) shows focal weak LMP1 expression in cords of malignant cells, while panel D (case 12) shows nuclear HIF-1α expressed at varying intensity in large malignant-appearing cells [a and c: orange immunofluorescence with blue DAPI counterstain (200× and 400×, respectively); b and d: immunohistochemistry with brown signal and blue hematoxylin counterstain (400×)]
Among the pre-malignant lesions, LMP1 was expressed in a fraction of cells of the surface epithelium representing histologies ranging from low grade dysplasia to carcinoma in situ, whereas normal epithelium had no LMP1 expression in benign surface components, even using the most sensitive detection method of tyramide signal amplification with immunofluorescent staining. This result implies that LMP1 is expressed only in neoplastic cells and not in normal epithelium. Overall, 7/8 patients with evaluable pre-malignant lesions had LMP1 expression in the surface component of their tumor (Table 2).
Table 2.
Comparison of LMP1 and HIF-1α expression in invasive and in situ components of twelve nasopharyngeal carcinomas
| Case # | Geographic origin | Invasive component | Pre-malignant component | ||
|---|---|---|---|---|---|
| EBV LMP1 | HIF-1α | EBV LMP1 | HIF-1α | ||
| Total score | Total score | ||||
| 6 | Indonesia | 7 | 2 | Positive | Positive |
| 9 | USA | 5 | 2 | N/A | Neg |
| 4 | Indonesia | 5 | 2 | Positive | N/A |
| 5 | USA | 4 | 2 | N/A | Positive |
| 13 | USA | 4 | 0 | Neg | N/A |
| 17 | Indonesia | 4 | 2 | Positive | Positive |
| 18 | USA | 3 | 3 | N/A | Positive |
| 2 | USA | 3 | 2 | N/A | Positive |
| 3 | Indonesia | 3 | 2 | Positive | Positive |
| 1 | Indonesia | 3 | 4 | Positive | Positive |
| 15 | Indonesia | 3 | 2 | Positive | Neg |
| 16 | USA | 3 | 3 | Positive | Positive |
Neg negative result; N/A uninterpretable result; HIF-1α hypoxia inducible factor 1 alpha; LMP1 latent membrane protein 1; USA United States of America
HIF-1α Expression and Associations with LMP1 and Vessel Density
Hypoxia-inducible factor-1α (HIF-1α) was expressed focally and weakly in the majority of invasive NPCs (15/18 cases, 83%; Table 1). HIF-1α and LMP1 expression patterns were not similar, nor was the intensity of expression of these two proteins correlated in specific tumors (Table 1). Dual immunostains were not feasible, but evaluation of staining patterns and proportion scores suggested that LMP1 and HIF-1α did not consistently co-localize. Likewise, there was no strong correlation between LMP1 scores and the degree of vascularization as measured with the assistance of CD31 immunostains, nor was there a strong association between HIF-1α scores and degree of vascularization, implying that factors beyond HIF-1α are likely to influence new vessel growth.
Among premalignant lesions, HIF-1α was often expressed in atypical as well as benign-appearing squamous epithelial cell nuclei (Table 2). Interestingly, case #16 had LMP1 and HIF-1α co-expression in basal layers of a mild dysplasia lesion in which cellular atypia was limited to the basal layer (Fig. 2). Expression was confirmed as true positive upon evaluation of the control slide in which omission of the primary antibody resulted in lack of signal. Case #17 also co-expressed LMP1 and HIF-1α in basal cells. Although these two examples of coordinated expression were identified, the majority of cases did not appear to have similar patterns of expression.
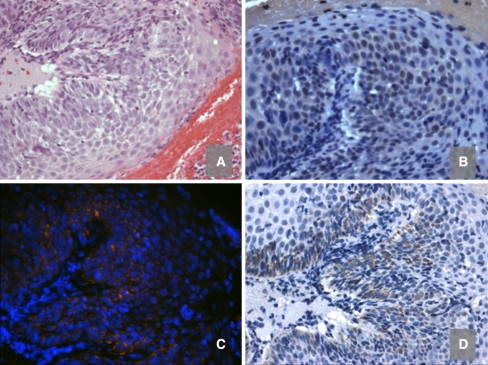
Fig. 2.
HIF-1α and LMP1 are expressed in a premalignant lesion (case 16). H&E stain (a) reveals squamous epithelium with focal mild dysplasia, while HIF-1α immunohistochemistry (b) reveals HIF-1α protein in many epithelial cells throughout the thickness of the surface epithelium. Panels C and D demonstrate LMP1 expression concentrated in the basal layers by inmmunofluorescent and chromogenic methods, respectively (400×)
Discussion
This study describes a sensitive method of detecting LMP1 using fluorescence and signal amplification resulting in identification of LMP1 expression in a much higher proportion of NPC cases than had been identified using traditional chromogenic immunohistochemistry with brightfield microscopy. While both LMP1 and HIF-1α were often expressed in invasive NPC tissues, there does not appear to be a consistent positional or quantitative relationship between LMP1 expression and HIF-1α upregulation within the invasive component of NPC. This implies that HIF-1α expression is controlled by factors beyond LMP1. Likewise, there was no strong correlation between HIF-1α expression and the degree of microvascularization, implying that factors beyond HIF-1α control vessel density. Finally, this study documents a similar distribution of microvasculature counts as well as LMP1 and HIF-1α expression between patient cohorts from Indonesia and the USA, suggesting no geographical bias.
Prior studies showed that LMP1 transfection of lymphoblastoid and carcinoma cell lines induced HIF-1α in vitro [14, 15]. If the same pathway were active in vivo, it might compel clinical trials of newly available anti-angiogenic agents to thwart the effects of LMP1. Anti-angiogenic agents are effective in treating clear cell carcinoma of the kidney where mutation of VHL with accompanying HIF induction is thought to drive tumor growth.
Compared to in vitro models in which LMP1 induced HIF-1α [14, 15], in vivo settings can be expected to behave in a much more complicated fashion. Levels of host genes are influenced, at least in part, by the local tumor environment including oxygenation status, which is a potent regulator of HIF stabilization. HIF proteins are very dynamic, with levels accommodating quickly to a wide variety of genetic and environmental stimuli. Indeed, the human genome has over 100 hypoxia response genes controlling angiogenesis, anaerobic metabolism, apoptosis, and erythrocyte production [18]. Even renal cell carcinomas harboring VHL mutation have variable levels of HIF-1α upregulation, and VHL mutant tumors expressing HIF-2α exclusively display a distinct transcriptional profile [19].
Recognizing that HIF-1α is only one of many factors through which LMP1 might influence angiogenesis, we also measured vessel density using CD31-assisted microscopy. A wide range of vessel counts was found but, again, there was no obvious relationship between LMP1 expression scores and the degree of microvasculature. This does not exclude a relationship between EBV infection and angiogenesis since our sample size was small and we did not account for the fact that natural EBV infection introduces nearly 100 foreign coding sequences of which several beyond LMP1 are typically expressed, at least focally, in NPC. These include the viral gene products EBER1, EBER2, EBNA1, LMP2, BARF1 and several microRNAs [20–22].
According to Zhong et al. [23], HIF-1α upregulation is probably an early event in prostate carcinogenesis. It is feasible that HIF-1α is expressed transiently or is active only in specific stages of malignancy. Further evaluation of premalignant lesions is warranted given our anecdotal observation of LMP1 and HIF-1α co-expression in basal epithelial cells in two cases. Indeed, LMP1 is thought to have different biological properties at various stages of disease progression and may induce additional factors that contribute to neovascularisation [24–26].
This study focused on LMP1 because of the previously identified link between LMP1 and HIF-1α in cell lines, and because LMP1 is considered to be among the most oncogenic of the EBV proteins. Sensitive detection of LMP1 is important because it is feasible that even low level LMP1 may trigger downstream functions. Prior studies have shown wide differences in LMP1 positivity among NPC cohorts [6, 27–29]. This work demonstrates that detection of LMP1 expression depends on the sensitivity of the analytic methods that are used. When traditional chromogenic immunohistochemistry was used, less LMP1 expression was identified compared to when fluorescent detection was used. Sensitivity could be enhanced even further using signal amplification technologies. Research is underway to develop systems for measuring fluorescent signals in situ that will facilitate quantification of multiple factors in the same cells or lesions [30–32].
High numbers of microvessels in some of our NPC cases imply that microvasculature may be a critical factor in supporting tumor growth and might represent a potential target for intervention. Further work should be done to explore whether NPC patients benefit from anti-angiogenic therapies and to measure the extent to which laboratory evaluation of vessel density or upstream mediators predicts response to treatment [33, 34].
Acknowledgments
The authors thank Jajah Fachiroh at Gadjah Madah University Medical School, Yogyakarta, Indonesia, for assembling and preparing tissues. We thank Tineke Vendrig, Elizabeth Bloemena, Wim Vos, and Joost Oudejans of Vrije Universiteit Amsterdam, and Joseph Pagano, Robert Bagnell, Mervi Eeva, Courtney Boyd, and Nana Feinberg of the University of North Carolina at Chapel Hill for supporting this study.
Funding This study was supported by the Dutch Cancer Society, Vrije Universiteit Amsterdam Dittmer Fund and Medical Department, and the Department of Pathology and Laboratory Medicine at the University of North Carolina at Chapel Hill.
References
- 1.Delongchamps NB, Peyromaure M. The role of vascular endothelial growth factor in kidney and prostate cancer. Can J Urol. 2007;14(5):3669–3677. [PubMed] [Google Scholar]
- 2.Sgadari C, Barillari G, Toschi E, et al. HIV protease inhibitors are potent anti-angiogenic molecules and promote regression of Kaposi sarcoma. Nat Med. 2002;8(3):225–232. doi: 10.1038/nm0302-225. [DOI] [PubMed] [Google Scholar]
- 3.Gulley ML, Tang W. Laboratory assays for Epstein-Barr virus-related disease. J Mol Diagn. 2008;10(4):279–292. doi: 10.2353/jmoldx.2008.080023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Raab-Traub N, Flynn K, Pearson G, et al. The differentiated form of nasopharyngeal carcinoma contains Epstein-Barr virus DNA. Int J Cancer. 1987;39(1):25–29. doi: 10.1002/ijc.2910390106. [DOI] [PubMed] [Google Scholar]
- 5.Guang-Wu H, Sunagawa M, Jie-En L, et al. The relationship between microvessel density, the expression of vascular endothelial growth factor (VEGF), and the extension of nasopharyngeal carcinoma. Laryngoscope. 2000;110(12):2066–2069. doi: 10.1097/00005537-200012000-00017. [DOI] [PubMed] [Google Scholar]
- 6.Khabir A, Karray H, Rodriguez S, et al. EBV latent membrane protein 1 abundance correlates with patient age but not with metastatic behavior in north African nasopharyngeal carcinomas. Virol J. 2005;2:39. doi: 10.1186/1743-422X-2-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kwok Fung Lo A, Liu Y, Wang X, et al. Identification of downstream target genes of latent membrane protein 1 in nasopharyngeal carcinoma cells by suppression subtractive hybridization. Biochim Biophys Acta. 2001;1520(2):131–140. doi: 10.1016/s0167-4781(01)00260-3. [DOI] [PubMed] [Google Scholar]
- 8.Brahimi-Horn C, Pouyssegur J. The role of the hypoxia-inducible factor in tumor metabolism growth and invasion. Bull Cancer. 2006;93(8):E73–E80. [PubMed] [Google Scholar]
- 9.Hui EP, Chan AT, Pezzella F, et al. Coexpression of hypoxia-inducible factors 1alpha and 2alpha, carbonic anhydrase IX, and vascular endothelial growth factor in nasopharyngeal carcinoma and relationship to survival. Clin Cancer Res. 2002;8(8):2595–2604. [PubMed] [Google Scholar]
- 10.Glaser SL, Hsu JL, Gulley ML. Epstein-Barr virus and breast cancer: state of the evidence for viral carcinogenesis. Cancer Epidemiol Biomarkers Prev. 2004;13(5):688–697. [PubMed] [Google Scholar]
- 11.Vleugel MM, Greijer AE, Shvarts A, et al. Differential prognostic impact of hypoxia induced and diffuse HIF-1alpha expression in invasive breast cancer. J Clin Pathol. 2005;58(2):172–177. doi: 10.1136/jcp.2004.019885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hatzivassiliou E, Mosialos G. Cellular signaling pathways engaged by the Epstein-Barr virus transforming protein LMP1. Front Biosci. 2002;7:d319–d329. doi: 10.2741/hatziva. [DOI] [PubMed] [Google Scholar]
- 13.Zheng H, Li LL, Hu DS, et al. Role of Epstein-Barr virus encoded latent membrane protein 1 in the carcinogenesis of nasopharyngeal carcinoma. Cell Mol Immunol. 2007;4(3):185–196. [PubMed] [Google Scholar]
- 14.Wakisaka N, Kondo S, Yoshizaki T, et al. Epstein-Barr virus latent membrane protein 1 induces synthesis of hypoxia-inducible factor 1 alpha. Mol Cell Biol. 2004;24(12):5223–5234. doi: 10.1128/MCB.24.12.5223-5234.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kondo S, Seo SY, Yoshizaki T, et al. EBV latent membrane protein 1 up-regulates hypoxia-inducible factor 1alpha through Siah1-mediated down-regulation of prolyl hydroxylases 1 and 3 in nasopharyngeal epithelial cells. Cancer Res. 2006;66(20):9870–9877. doi: 10.1158/0008-5472.CAN-06-1679. [DOI] [PubMed] [Google Scholar]
- 16.Stevens SJ, Verkuijlen SA, Hariwiyanto B, et al. Noninvasive diagnosis of nasopharyngeal carcinoma: nasopharyngeal brushings reveal high Epstein-Barr virus DNA load and carcinoma-specific viral BARF1 mRNA. Int J Cancer. 2006;119(3):608–614. doi: 10.1002/ijc.21914. [DOI] [PubMed] [Google Scholar]
- 17.Rathmell WK, Hickey MM, Bezman NA, et al. In vitro and in vivo models analyzing von Hippel-Lindau disease-specific mutations. Cancer Res. 2004;64(23):8595–8603. doi: 10.1158/0008-5472.CAN-04-1430. [DOI] [PubMed] [Google Scholar]
- 18.Greijer AE, Groep P, Kemming D, et al. Up-regulation of gene expression by hypoxia is mediated predominantly by hypoxia-inducible factor 1 (HIF-1) J Pathol. 2005;206(3):291–304. doi: 10.1002/path.1778. [DOI] [PubMed] [Google Scholar]
- 19.Gordan JD, Bertout JA, Hu CJ, et al. HIF-2alpha promotes hypoxic cell proliferation by enhancing c-myc transcriptional activity. Cancer Cell. 2007;11(4):335–347. doi: 10.1016/j.ccr.2007.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cosmopoulos K, Pegtel M, Hawkins J, et al. Comprehensive profiling of Epstein-Barr virus microRNAs in nasopharyngeal carcinoma. J Virol. 2009;83(5):2357–2367. doi: 10.1128/JVI.02104-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lo AK, To KF, Lo KW, et al. Modulation of LMP1 protein expression by EBV-encoded microRNAs. Proc Natl Acad Sci USA. 2007;104(41):16164–16169. doi: 10.1073/pnas.0702896104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Young LS, Murray PG. Epstein-Barr virus and oncogenesis: from latent genes to tumours. Oncogene. 2003;22(33):5108–5121. doi: 10.1038/sj.onc.1206556. [DOI] [PubMed] [Google Scholar]
- 23.Zhong H, Semenza GL, Simons JW, et al. Up-regulation of hypoxia-inducible factor 1alpha is an early event in prostate carcinogenesis. Cancer Detect Prev. 2004;28(2):88–93. doi: 10.1016/j.cdp.2003.12.009. [DOI] [PubMed] [Google Scholar]
- 24.Cheung FM, Pang SW, Yau TK, et al. Nasopharyngeal intraepithelial lesion: latent Epstein-Barr virus infection with malignant potential. Histopathology. 2004;45(2):171–179. doi: 10.1111/j.1365-2559.2004.01935.x. [DOI] [PubMed] [Google Scholar]
- 25.Ren Q, Sato H, Murono S, et al. Epstein-Barr virus (EBV) latent membrane protein 1 induces interleukin-8 through the nuclear factor-kappa B signaling pathway in EBV-infected nasopharyngeal carcinoma cell line. Laryngoscope. 2004;114(5):855–859. doi: 10.1097/00005537-200405000-00012. [DOI] [PubMed] [Google Scholar]
- 26.Tan EL, Sam CK. Biological properties of TW01 cells expressing latent membrane protein-1 gene of EBV-derived from nasopharyngeal carcinoma cells at different stages of malignancy. Exp Oncol. 2007;29(3):166–174. [PubMed] [Google Scholar]
- 27.Liebowitz D. Nasopharyngeal carcinoma: the Epstein-Barr virus association. Semin Oncol. 1994;21(3):376–381. [PubMed] [Google Scholar]
- 28.Niedobitek G, Young LS, Sam CK, et al. Expression of Epstein-Barr virus genes and of lymphocyte activation molecules in undifferentiated nasopharyngeal carcinomas. Am J Pathol. 1992;140(4):879–887. [PMC free article] [PubMed] [Google Scholar]
- 29.Taheri-Kadkhoda Z, Magnusson B, Svensson M, et al. Expression modes and clinical manifestations of latent membrane protein 1, Ki-67, cyclin-B1, and epidermal growth factor receptor in nonendemic nasopharyngeal carcinoma. Head Neck. 2009;31(4):482–492. doi: 10.1002/hed.21002. [DOI] [PubMed] [Google Scholar]
- 30.McCabe A, Dolled-Filhart M, Camp RL, et al. Automated quantitative analysis (AQUA) of in situ protein expression, antibody concentration, and prognosis. J Natl Cancer Inst. 2005;97(24):1808–1815. doi: 10.1093/jnci/dji427. [DOI] [PubMed] [Google Scholar]
- 31.Rubin MA, Zerkowski MP, Camp RL, et al. Quantitative determination of expression of the prostate cancer protein alpha-methylacyl-CoA racemase using automated quantitative analysis (AQUA): a novel paradigm for automated and continuous biomarker measurements. Am J Pathol. 2004;164(3):831–840. doi: 10.1016/s0002-9440(10)63171-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sullivan CA, Ghosh S, Ocal IT, et al. Microvessel area using automated image analysis is reproducible and is associated with prognosis in breast cancer. Hum Pathol. 2009;40(2):156–165. doi: 10.1016/j.humpath.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 33.Hoogsteen IJ, Marres HA, Bussink J, et al. Tumor microenvironment in head and neck squamous cell carcinomas: predictive value and clinical relevance of hypoxic markers. A review. Head Neck. 2007;29(6):591–604. doi: 10.1002/hed.20543. [DOI] [PubMed] [Google Scholar]
- 34.Jonathan RA, Wijffels KI, Peeters W, et al. The prognostic value of endogenous hypoxia-related markers for head and neck squamous cell carcinomas treated with ARCON. Radiother Oncol. 2006;79(3):288–297. doi: 10.1016/j.radonc.2006.04.008. [DOI] [PubMed] [Google Scholar]