Abstract
Metastatic disease to thyroid gland is a rare event. Although renal cell carcinoma (RCC) has been reported to metastasize the thyroid gland, metastatic RCC to a thyroid neoplasm is very unusual. We report a case of a 68-year-old man with history of RCC who presented with a 2.5-cm thyroid nodule. Histologic examination demonstrates a renal cell carcinoma metastatic to a papillary carcinoma of the thyroid. The clinicopathologic features of metastatic disease into a thyroid gland neoplasm are shown, and a review of the literature is presented.
Keywords: Renal cell carcinoma, Papillary thyroid carcinoma, Metastasis, Tumor-to-tumor metastasis
Introduction
Metastatic disease to thyroid gland is uncommon. Two to three percent of all thyroid malignant tumors are metastatic; this incidence can be higher in autopsies, ranging from 5 to 24% [1–5], as part of widespread metastatic disease or direct invasion to the gland from an adjacent tumor [6]. Different types of solid tumors can metastasize to the thyroid including malignant melanoma, renal cell carcinoma (RCC), breast cancer, lung carcinoma, hematologic malignancies, and head and neck tumors [1, 7–9]. Interestingly, in the majority of the cases, the metastatic lesions are occult and only discovered during autopsy [1]. In the English literature, there are reports of RCC cases metastasizing to the thyroid gland involving normal parenchyma and in some cases infiltrating an abnormal non-neoplastic gland (e.g. goiter) [1, 10, 11]. However, RCC metastatic to a primary thyroid tumor is exceedingly rare [12–17]. We report herein an unusual occurrence of a RCC metastasizing into a papillary thyroid carcinoma and present a review of the literature.
Case Report
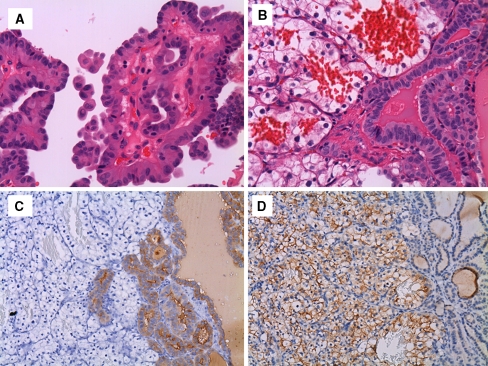
A 68-year-old man with history of RCC was admitted for oncologic follow-up evaluation at The Ohio State Medical Center. During the assessment, a right lobe thyroid nodule was discovered. The patient was asymptomatic and his thyroid function tests were all in the normal range. He underwent a radical left nephrectomy 2 years earlier. The renal tumor was diagnosed as RCC, clear cell type, Fuhrman grade 3 and staged as T3b, N0, MX. Physical examination was unremarkable. An ultrasound (US) examination revealed a 2.5-cm solid and hypervascular nodule in the right thyroid lobe. A needle core biopsy of the nodule was performed and sent for pathologic examination. Microscopic evaluation revealed a neoplasm composed of papillary structures lined by enlarged cells with ovoid and crowded nuclei, displaying intranuclear pseudoinclusions. A positive nuclear staining with thyroid transcription factor-1 (TTF-1) and cytoplasmic thyroglobulin were identified. The tumor was diagnosed as papillary thyroid carcinoma. The patient subsequently underwent a total thyroidectomy. Gross examination of the specimen showed a 2.5 cm × 2.5 cm × 2.0 cm well-circumscribed nodule in the superior half of the right lobe. Cut sections revealed a tan-granular tissue with a red-brown area measuring 0.5 cm × 0.3 cm × 0.3 cm. No other similar area was noted in the right lobe nodule. The remainder of the thyroid parenchyma was unremarkable. Histologic examination of the excised specimen revealed a neoplastic thyroid nodule composed of follicles and papillary structures lined by cells with ovoid enlarged nuclei displaying chromatin clearing and grooves characteristic of papillary thyroid cancer (Fig. 1a). In addition, a well-demarcated area containing sheets of phenotypically distinct tumor cells with a rich capillary network was present within the papillary thyroid cancer nodule. This second population of tumor cells showed ample clear cell cytoplasm, rounded nuclei, and inconspicuous nucleoli (Fig. 1b). This area was only seen in the section corresponding to the red-brown area identified within the thyroid nodule; no additional micronodules were identified within the papillary thyroid carcinoma. Immunostains revealed that these cells displayed diffuse positivity for RCC marker and were negative for thyroglobulin; in contrast, the surrounding papillary thyroid cancer cells were positive for thyroglobulin and negative for RCC marker (Fig. 1c, d).
Fig. 1.
a Papillary thyroid carcinoma: papillary structures lined by cells with longitudinal grooves and intranuclear inclusions (H&E, ×400). b Renal cell carcinoma metastatic to papillary thyroid carcinoma (H&E, ×400). c Thyroglobulin immunostain shows a positive reaction by papillary thyroid carcinoma cells. The renal cell carcinoma cells lack thyroglobulin expression (H&E, ×200). d Metastatic renal cell carcinoma cells are positive for RCC marker, whereas papillary thyroid carcinoma cells are negative (H&E, ×200)
The previous patient’s renal tumor slides were reviewed, and the cytomorphology was similar to that seen in the thyroid tumor. The findings were consistent with papillary thyroid carcinoma focally involved by metastatic renal cell carcinoma.
One-year follow-up after thyroidectomy, no anatomic or radiographic evidence of recurrent papillary thyroid cancer has been identified; nevertheless, foci of metastatic renal cell carcinoma to multiple vertebral bodies were found.
Discussion
The presence of tumor-to-tumor metastasis is rare [16, 18–20]. The definition of cancer metastasizing to cancer has been controversial, and certain strict criteria are now accepted: (1) the recipient tumor must be a true neoplasm, (2) the donor tumor must be a true metastasis (direct contiguous spreading is not acceptable as metastasis) [19, 20].
Very few reports of tumor-to-tumor metastasis are present in the English literature [12–17]. Several hypotheses have been proposed to explain that the proclivity of metastasis to the thyroid gland is related to its rich blood supply; however, some researchers have suggested that the abnormal thyroid gland is vulnerable to metastatic growth due to a decrease in oxygen and iodine content alteration [6].
To the best of our knowledge, only 6 cases of RCC metastatic to a primary thyroid neoplasm have been previously reported in the English-language literature, which are summarized in Table 1. Metastatic RCC has been described involving follicular adenoma [13–15, 17], follicular carcinoma, oncocytic variant, Hurthle cell adenoma, and only two cases, including the present case, are RCC involving a papillary thyroid carcinoma [12, 16].
Table 1.
Renal cell carcinoma metastatic to thyroid gland neoplasm
| Case | Author | Tumor-to-tumor metastasis | IHC of RCC metastasis |
|---|---|---|---|
| 1 | Rosai et al. [12] | RCC into a follicular adenoma | Thyroglobulin (−) |
| 2 | Baloch et al. [16] | RCC into a follicular variant of papillary thyroid carcinoma | Thyroglobulin (equivocal) CK 19 (equivocal) |
| 3 | Wolf et al. [17] | RCC into a microfollicular adenoma | Not done |
| 4 | Qian et al. [14] | RCC into Hurthle cell adenoma | TTF-1 (−), thyroglobulin (−) CD10 (+), vimentin (+) |
| 5 | Koo et al. [15] | RCC into follicular adenoma | TTF-1 (−), thyroglobulin (−) Calcitonin (−), inhibin (−) Equivocal: CK, CD10, galectin-3 |
| 6 | Ryska [13] | RCC into oncocytic thyroid carcinoma | AE1/AE3 (+), thyroglobulin (−) Vimentin (+), EMA (+), calcitonin (−) CEA (−), CK19(−) |
| 7 | Bohn et al. (present case) | RCC into papillary thyroid carcinoma | Thyroglobulin (−) RCC marker (+) |
IHC indicates immunohistochemistry, RCC renal cell carcinoma, CK cytokeratin, TTF-1 thyroid transcription factor 1
RCC clear cell type is the most common malignancy of the kidney and usually shows metastasis at the time of diagnosis [21]. RCC has an unpredictable behavior and its recurrence after nephrectomy is highly variable, presenting as late metastases after several years of the initial diagnosis [22, 23]. Iesalnieks et al. have reported that the mean interval from the nephrectomy to thyroid surgery, when metastatic disease is found, is 12 years [24]. Some studies have shown that metastatic tumor to the thyroid can be the initial presentation of RCC [6, 7, 25]. In our case, a thyroid nodule with metastatic RCC was the first metastatic focus discovered during the post-operative follow-up of this patient. Unfortunately, our patient subsequently developed multiple bone metastases to the spine.
The presence of a thyroid nodule in a patient with a prior cancer can represent a clinically and/or pathologically diagnostic challenge [26]. Some of these thyroid nodules represent primary thyroid processes rather than metastatic deposits [26]. The diagnosis of metastatic carcinoma to the thyroid by core biopsy, frozen section, and permanent sections can be easily misinterpreted as a primary tumor. The possibility of metastatic RCC should always be considered when two different cell populations are identified, and specifically, one should be aware of in the presence of clear cells in a thyroid neoplasm. Rosai et al. [12] consider that features favoring a diagnosis of metastatic RCC are the tumor multiplicity, the sinusoidal pattern of vascularization, and the clear cell appearance of the cytoplasm. However, our case showed the presence of a single focus rather than multiple nodules.
The diagnosis of metastatic disease in a thyroid gland requires a high level of suspicion. Other neoplasms have to be considered in the differential diagnosis, when clear tumor cells are identified within the thyroid gland [27]. Primary tumors with clear cell features including paraganglioma, papillary, follicular, and medullary thyroid carcinomas, and secondary tumors such as those from lung and salivary gland origin also need to be considered. Furthermore, the distinction of a primary from a metastatic tumor can be very difficult without histologic comparison with the patient’s prior material. The support of immunohistochemistry can be very valuable. A selective panel of immunohistochemical stains including thyroid markers such as TTF-1 and thyroglobulin are necessary. In situations where a metastatic tumor such as RCC is considered, RCC marker, vimentin, EMA, and CD10 are generally used and may help to identify the renal tumor deposits.
In summary, this case shows a fascinating occurrence of tumor-to-tumor metastasis of a RCC, clear cell type, involving a papillary thyroid carcinoma. Although very rare, secondary tumors of the thyroid gland should always be considered in the setting of a previous malignancy; furthermore, in the presence of a neoplasm with clear cell features involving the thyroid, the possibility of a metastatic RCC should be entertained.
References
- 1.Shimaoka K, Sokal JE, Pickren JW. Metastatic neoplasms in the thyroid gland. Pathological and clinical findings. Cancer. 1962;15:557–565. doi: 10.1002/1097-0142(196205/06)15:3<557::AID-CNCR2820150315>3.0.CO;2-H. [DOI] [PubMed] [Google Scholar]
- 2.Rizzo M, Rossi RT, Bonaffini O, et al. Thyroid metastasis of clear cell renal carcinoma: report of a case. Diagn Cytopathol. 2009. [DOI] [PubMed]
- 3.Lam KY, Lo CY. Metastatic tumors of the thyroid gland: a study of 79 cases in Chinese patients. Arch Pathol Lab Med. 1998;122(1):37–41. [PubMed] [Google Scholar]
- 4.Lin JD, Weng HF, Ho YS. Clinical and pathological characteristics of secondary thyroid cancer. Thyroid. 1998;8(2):149–153. doi: 10.1089/thy.1998.8.149. [DOI] [PubMed] [Google Scholar]
- 5.Haugen BR, Nawaz S, Cohn A, et al. Secondary malignancy of the thyroid gland: a case report and review of the literature. Thyroid. 1994;4(3):297–300. doi: 10.1089/thy.1994.4.297. [DOI] [PubMed] [Google Scholar]
- 6.Heffess CS, Wenig BM, Thompson LD. Metastatic renal cell carcinoma to the thyroid gland: a clinicopathologic study of 36 cases. Cancer. 2002;95(9):1869–1878. doi: 10.1002/cncr.10901. [DOI] [PubMed] [Google Scholar]
- 7.Green LK, Ro JY, Mackay B, Ayala AG, Luna MA. Renal cell carcinoma metastatic to the thyroid. Cancer. 1989;63(9):1810–1815. doi: 10.1002/1097-0142(19900501)63:9<1810::AID-CNCR2820630925>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 8.Czech JM, Lichtor TR, Carney JA, Heerden JA. Neoplasms metastatic to the thyroid gland. Surg Gynecol Obstet. 1982;155(4):503–505. [PubMed] [Google Scholar]
- 9.Elliott RH, Jr, Frantz VK. Metastatic carcinoma masquerading as primary thyroid cancer: a report of authors’ 14 cases. Ann Surg. 1960;151:551–561. doi: 10.1097/00000658-196004000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ivy HK. Cancer metastatic to the thyroid: a diagnostic problem. Mayo Clin Proc. 1984;59(12):856–859. doi: 10.1016/s0025-6196(12)65622-5. [DOI] [PubMed] [Google Scholar]
- 11.Carcangiu ML, Sibley RK, Rosai J. Clear cell change in primary thyroid tumors. A study of 38 cases. Am J Surg Pathol. 1985;9(10):705–722. doi: 10.1097/00000478-198510000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Rosai J, Carcangiu ML, DeLellis R. Tumors of the thyroid gland. Washington, DC: Armed Forces Institute of Pathology; 1992. pp. 289–296. [Google Scholar]
- 13.Ryska A, Cap J. Tumor-to-tumor metastasis of renal cell carcinoma into oncocytic carcinoma of the thyroid. Report of a case and review of the literature. Pathol Res Pract. 2003;199(2):101–106. doi: 10.1078/0344-0338-00361. [DOI] [PubMed] [Google Scholar]
- 14.Qian L, Pucci R, Castro CY, Eltorky MA. Renal cell carcinoma metastatic to Hurthle cell adenoma of thyroid. Ann Diagn Pathol. 2004;8(5):305–308. doi: 10.1016/j.anndiagpath.2004.07.011. [DOI] [PubMed] [Google Scholar]
- 15.Koo HL, Jang J, Hong SJ, Shong Y, Gong G. Renal cell carcinoma metastatic to follicular adenoma of the thyroid gland. A case report. Acta Cytol. 2004;48(1):64–68. doi: 10.1159/000326285. [DOI] [PubMed] [Google Scholar]
- 16.Baloch ZW, LiVolsi VA. Tumor-to-tumor metastasis to follicular variant of papillary carcinoma of thyroid. Arch Pathol Lab Med. 1999;123(8):703–706. doi: 10.5858/1999-123-0703-TTTMTF. [DOI] [PubMed] [Google Scholar]
- 17.Wolf G, Aigner RM, Humer-Fuchs U, Schwarz T, Krippl P, Wehrschuetz M. Renal cell carcinoma metastasis in a microfollicular adenoma of the thyroid gland. Acta Med Austriaca. 2002;29(4):141–142. doi: 10.1046/j.1563-2571.2002.02009.x. [DOI] [PubMed] [Google Scholar]
- 18.Rabson SM, Stier PL, Baumgartner JC, Rosenbaum D. Metastasis of cancer to cancer. Am J Clin Pathol. 1954;24(5):572–579. doi: 10.1093/ajcp/24.5.572. [DOI] [PubMed] [Google Scholar]
- 19.Campbell LV, Jr, Gilbert E, Chamberlain CR, Jr, Watne AL. Metastases of cancer to cancer. Cancer. 1968;22(3):635–643. doi: 10.1002/1097-0142(196809)22:3<635::AID-CNCR2820220320>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 20.Dobbing J. Cancer to cancer. Guys Hosp Rep. 1958;107(1):60–65. [PubMed] [Google Scholar]
- 21.Holland JM. Proceedings: cancer of the kidney–natural history and staging. Cancer. 1973;32(5):1030–1042. doi: 10.1002/1097-0142(197311)32:5<1030::AID-CNCR2820320502>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 22.Nakhjavani MK, Gharib H, Goellner JR, Heerden JA. Metastasis to the thyroid gland. A report of 43 cases. Cancer. 1997;79(3):574–578. doi: 10.1002/(SICI)1097-0142(19970201)79:3<574::AID-CNCR21>3.0.CO;2-#. [DOI] [PubMed] [Google Scholar]
- 23.Wada N, Hirakawa S, Rino Y, et al. Solitary metachronous metastasis to the thyroid from renal clear cell carcinoma 19 years after nephrectomy: report of a case. Surg Today. 2005;35(6):483–487. doi: 10.1007/s00595-004-2953-8. [DOI] [PubMed] [Google Scholar]
- 24.Iesalnieks I, Trupka A, Raab M, et al. Renal cell carcinoma metastases to the thyroid gland-8 cases reported. Thyroid. 2007;17(1):49–52. doi: 10.1089/thy.2006.0176. [DOI] [PubMed] [Google Scholar]
- 25.Hadjadj S, Geoffrois L, Aubert V, Weryha G, Leclere J. Thyroid metastases from cancer of the kidney. Two cases. Presse Med. 1995;24(30):1386–1388. [PubMed] [Google Scholar]
- 26.Watts NB. Carcinoma metastatic to the thyroid: prevalence and diagnosis by fine-needle aspiration cytology. Am J Med Sci. 1987;293(1):13–17. doi: 10.1097/00000441-198701000-00004. [DOI] [PubMed] [Google Scholar]
- 27.Schroder S, Bocker W. Clear-cell carcinomas of thyroid gland: a clinicopathological study of 13 cases. Histopathology. 1986;10(1):75–89. doi: 10.1111/j.1365-2559.1986.tb02462.x. [DOI] [PubMed] [Google Scholar]