Abstract
The ameloblastoma, particularly the solid/multicystic type, is the most clinically significant odontogentic tumor. The tumor is often locally aggressive and has a significant impact and may have a patient’s morbidity and mortality. In this report, we present a case of a large ameloblastoma that presented with the typical radiographic features of variably sized radiolucent loculations. Microscopically the tumor showed a variety of histologic types, with plexiform and follicular predominating. The tumor was treated with a partial resection of the mandible.
Keywords: Ameloblastoma odontogenic tumor, Multicystic ameloblastoma
History
A 28-year old male presented with a mass of the left mandible, increasing in size over several years.
Radiographic Features
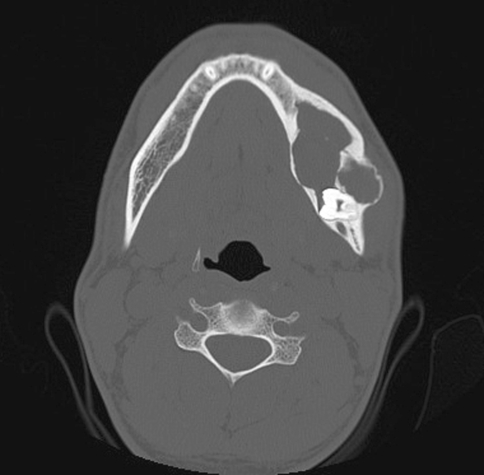
Computed tomography (CT) of the jaw showed a large, well-defined, multilocular radiolucent lesion in the left mandible associated with an unerupted tooth and surrounded by an opaque border. (Fig. 1).
Fig. 1.
Computed tomography scan with a large multilocular lucent lesion in the left mandible associated with an unerupted tooth
Diagnosis
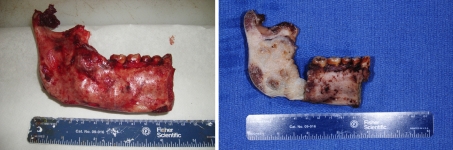
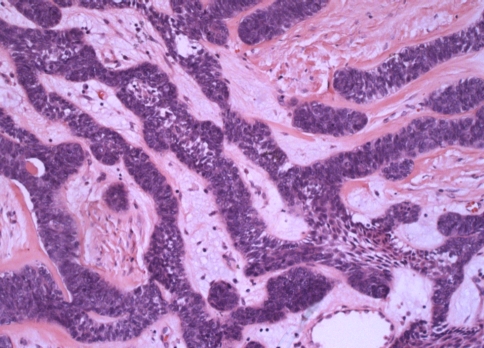
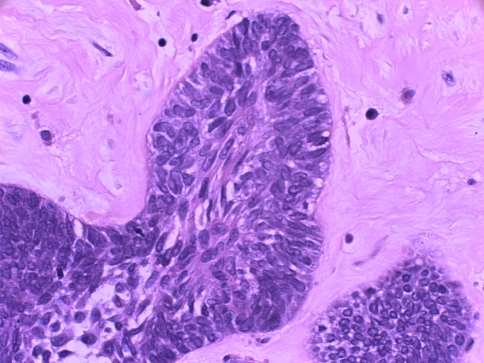
A left hemimandibulectomy was performed. The specimen was remarkable for expansion of the mandibular body and ramus. Decortication revealed a firm, multilocular mass extending from the mid region of the mandibular body to the upper ramus (Fig. 2). Histological examination of hematoxylin and eosin stained slides demonstrated anastomosing cords and islands of odontogenic epithelium set in a fibrous stroma. The epithelium consisted of basal cells showing cytoplasmic vacuolization and reverse polarization of the nuclei. In the center of the islands and cords, the cells were more loosely arranged, resembling stellate reticulum (Figs. 3, 4). Based on the gross and histologic features, a diagnosis of ameloblastoma was rendered.
Fig. 2.
Left image shows the fresh left hemimandible. There is expansion of the body and ramus with partial destruction of the cortex in the retromolar region. The right image is of the decorticated specimen showing involvement of the mandible by multicystic ameloblastoma
Fig. 3.
Low power view showing anastomosing cords of odontogenic epithelium in a fibrous stroma. Some cords contain stellate reticulum-like cells centrally
Fig. 4.
High power view of hyperchromatic basal cells with cytoplasmic vacuolization and reverse polarization of the nuclei
Discussion
The ameloblastoma, an aggressive benign neoplasm of odontogenic epithelium, is the most common clinically significant odontogenic tumor. Ameloblastomas are separated into three categories because of their presentation, treatment and prognosis. The categories are: multicystic or conventional, unicystic and peripheral. This paper will focus on the classic findings of the multicystic (conventional) ameloblastoma.
The multicystic ameloblastoma is a benign epithelial odontogenic tumor of the jaws that is slow-growing, locally aggressive and accounts for approximately 10% of all odontogenic tumors in the jaw. Most cases are diagnosed in young adults, with a median age of 35 years, and no gender predilection. Approximately 80% of ameloblastomas occur in the mandible, usually in the posterior region [1]. A notable exception is African Blacks, in whom any region of the mandible may be involved [2]. Patients may present with a slow-growing mass, malocclusion, loose teeth, or more rarely paresthesia and pain; however, many lesions are detected incidentally on radiographic studies in asymptomatic patients [1]. The lesions usually progress slowly, but are locally invasive and will infiltrate through the medullary spaces and can erode cortical bone. If left untreated, they can resorb the cortical plate and extend into adjacent tissue. Posterior maxillary tumors can obliterate the maxillary sinus and subsequently extend intracranially [2].
Computed tomographic, CT, images, usually show an expansile, radiolucent, multiloculated cystic lesion, with a characteristic “soap bubble-like” appearance. Other CT findings also include cystic areas of low attenuation with scattered isoattenuating regions, representing soft-tissue components. Thinning and expansion of the cortical plate with erosion through the cortex can be seen. The associated unerupted tooth may be displaced and resorption of the roots of adjacent teeth is common [3]. It is worth noting that the desmoplastic variant of the conventional ameloblastoma usually appears as a mixed radiolucent and radiodense lesion, often resembling a benign fibro-osseous lesion, and is most commonly found in the anterior maxilla.
Histologically, most ameloblastomas have the follicular or plexiform pattern, although basaloid, granular cell or desmoplastic variations may also be seen [4]. It is generally accepted that there is no relationship between the individual patterns and the behavior of the tumor or its prognosis [5]. For this reason, pathologists may choose not to report the histologic pattern. (Histologic pattern is not to be confused with the designation of conventional, unicystic or peripheral types, as these descriptors have considerable impact on the patients’ treatment and prognosis). The case presented showed features of both follicular and plexiform variants, possessing islands and anastomosing strands of odontogenic epithelium enmeshed in a fibrous stroma. These islands and strands contain basal cells that are columnar, hyperchromatic and lined up in a palisaded fashion at the periphery. The cells have vacuolated cytoplasm and the nuclei exhibit reverse polarization away from the connective tissue. The cells in the central portions of the epithelial islands are more loosely arranged, mimicking stellate reticulum. The lesion is cytologically bland with no pleomorphism or mitotic figures noted.
The remainder of the histologic patterns are usually distinguished by the characteristics of the cells central to the islands or nests. Acanthomatous, granular cell and basal cell patterns have central portions composed of epithelial cells with keratin formation, granular cells and uniform basal cells, respectively. The desmoplastic type of conventional ameloblastoma is unique, as it contains small islands and cords of odontogenic epithelium with little evidence of the characteristic ameloblast-like cells. The islands and nests are found in a very dense collagenous stroma [5]. As mentioned previously, the desmoplastic variant also has a unique radiographic appearance.
The mainstay of treatment is surgery, with wide resection recommended due to the high recurrence rate of solid/multicystic ameloblastomas. The recurrence rate after resection is 13–15%, as opposed to 90–100% after curettage [6]. Many authors recommend a margin of 1.5–2 cm beyond the radiological limit to ensure all microcysts are removed [7]. Several studies suggest treatment as an important prognostic factor, specifically implicating undertreatment as a cause of recurrence [6]. While not a first line treatment, radiotherapy should be considered for patients with positive margins who are not amenable to re-excision [1]. Follow-up is essential as most recurrences present within the first 5 years; however, some have been observed more than 10 years after initial treatment [7].
Very rarely, ameloblastomas may metastasize and are referred to as metastasizing (malignant) ameloblastomas. Histologically, they are identical to ameloblastomas that do not metastasize and the diagnosis is made on clinical behavior only. Additionally, there are no morphological criteria identified to predict which ameloblastomas have the potential for metastatic spread. The malignant ameloblastoma spreads through the lymphatics with the lungs being the most common site, followed by cervical lymph nodes and spine. Less common sites of involvement include the liver, skull, brain, kidney and small bowel. Some studies have shown correlation with the extent of the initial tumor, multiple recurrences and surgical interventions to the potential for metastatic spread, but not all cases fall into this category. There is usually a long interval between diagnosis of the primary and development of metastasis (average of 10–12 years) and the median survival time ranges from 3 months to 5 years. Surgery is the treatment of choice for operable lung metastasis and radiation and/or chemotherapy may play a role in non-resectable disease [8].
Disclaimer
The opinions and assertions expressed herein are those of the author and are not to be construed as official or representing the views of the Department of the Navy or the Department of Defense.
References
- 1.Mendenhall WM, Werning JW, Fernandes R, Malyapa RS, Mendenhall NP. Ameloblastoma. Am J Clin Oncol. 2007;30:645–648. doi: 10.1097/COC.0b013e3181573e59. [DOI] [PubMed] [Google Scholar]
- 2.Barnes L, Eveson JW, Reichart P, Sidransky D, editors. World health organization classification of tumours: Head and neck tumours. Lyon, France: IARC Press; 2005. [Google Scholar]
- 3.Dunfee BL, Sakai O, Pistey R, Gohel A. Radiologic and pathologic characteristics of benign and malignant lesions of the mandible. Radiographics. 2006;26:1751–1768. doi: 10.1148/rg.266055189. [DOI] [PubMed] [Google Scholar]
- 4.Thompson LDR, editor. Head and neck pathology (A volume in the foundations in diagnostic pathology series) Philadelphia: Elsevier; 2006. [Google Scholar]
- 5.Gardner DG. Some current concepts on the pathology of ameloblastomas. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;82(6):660–669. doi: 10.1016/S1079-2104(96)80441-0. [DOI] [PubMed] [Google Scholar]
- 6.Chapelle KAOM, Stoelinga PJW, Wilde PCM, Brouns JJA, Voorsmit RACA. Rational approach to diagnosis and treatment of ameloblastomas and odontogenic keratocysts. Br J Oral Maxillofac Surg. 2004;42:381–390. doi: 10.1016/j.bjoms.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 7.Hong J, et al. Long-term follow up on recurrence of 305 ameloblastoma cases. Int J Oral Maxillofac Surg. 2007;36:283–288. doi: 10.1016/j.ijom.2006.11.003. [DOI] [PubMed] [Google Scholar]
- 8.Gilijamse M, et al. Metastasizing ameloblastoma. Int J Oral Maxillofac Surg. 2007;36:462–464. doi: 10.1016/j.ijom.2006.12.005. [DOI] [PubMed] [Google Scholar]