Abstract
BACKGROUND
Over 35% of returned Iraq and Afghanistan veterans in VA care have received mental health diagnoses; the most prevalent is post-traumatic stress disorder (PTSD). Little is known about these patients’ use of non-mental health medical services and the impact of mental disorders on utilization.
OBJECTIVE
To compare utilization across three groups of Iraq and Afghanistan veterans: those without mental disorders, those with mental disorders other than PTSD, and those with PTSD.
DESIGN AND PARTICIPANTS
National, descriptive study of 249,440 veterans newly utilizing VA healthcare between October 7, 2001 and March 31, 2007, followed until March 31, 2008.
MEASUREMENTS
We used ICD9-CM diagnostic codes to classify mental health status. We compared utilization of outpatient non-mental health services, primary care, medical subspecialty, ancillary services, laboratory tests/diagnostic procedures, emergency services, and hospitalizations during veterans’ first year in VA care. Results were adjusted for demographics and military service and VA facility characteristics.
MAIN RESULTS
Veterans with mental disorders had 42–146% greater utilization than those without mental disorders, depending on the service category (all P < 0.001). Those with PTSD had the highest utilization in all categories: 71–170% greater utilization than those without mental disorders (all P < 0.001). In adjusted analyses, compared with veterans without mental disorders, those with mental disorders other than PTSD had 55% higher utilization of all non-mental health outpatient services; those with PTSD had 91% higher utilization. Female sex and lower rank were also independently associated with greater utilization.
CONCLUSIONS
Veterans with mental health diagnoses, particularly PTSD, utilize significantly more VA non-mental health medical services. As more veterans return home, we must ensure resources are allocated to meet their outpatient, inpatient, and emergency needs.
KEY WORDS: veterans, post-traumatic stress disorder, psychiatry, health services research, utilization
INTRODUCTION
To date, over 1.6 million US men and women have served in the wars in Iraq (Operation Iraqi Freedom, OIF) and Afghanistan and surrounding regions (Operation Enduring Freedom, OEF). Prior research has shown that returning OEF/OIF veterans are at high risk for mental disorders, and post-traumatic stress disorder (PTSD) is the most commonly diagnosed disorder.1–3 In addition, a recent analysis of over 200,000 returning OEF/OIF veterans seen at Department of Veterans Affairs (VA) healthcare facilities found that the rates of PTSD and other mental disorders were increasing over time.4 Recognizing the serious impact of these conditions, particularly PTSD, and meeting the healthcare needs of veterans with mental disorders has been the focus of high-profile scientific study and media attention.1,5,6
The VA has been one of the largest providers of healthcare for returning veterans and, in the past several years, has expanded access to more veterans of the current conflicts. Over 40% of all separated OEF/OIF veterans have obtained outpatient and/or inpatient care at VA facilities.4 This is a greater proportion than in prior wars; for instance, only 10% of Vietnam veterans enrolled in VA care.7 This increase in VA use may be due to a combination of expansion of VA eligibility and increasing problems with cost and accessibility of private insurance.8 The recognition of the growing prevalence of OEF/OIF veterans with mental health disorders has led to a nationwide effort to expand VA mental health services.1,9 However, far less is known about OEF/OIF veterans’ needs for non-mental health medical services and about the impact of mental disorders on medical service utilization in this population.6,10,11
Studies from OEF/OIF and prior wars have demonstrated that mental disorders, particularly PTSD, are associated with higher rates of physical symptoms, chronic physical illness, and overall mortality.6,12–14 This increased burden of physical diseases may translate into greater non-mental health medical service utilization, as suggested by a study showing that PTSD was associated greater self-reported primary care visits in 2,863 OIF veterans 6 and by studies examining utilization in veterans of prior wars.11,15–19 Yet, mental disorders and their associated stigma and risk for social isolation and cognitive impairment may also act as barriers to medical treatment.16,20 In addition, the unique features of the current wars, including the greater number of woman in combat roles and specific types of injuries (traumatic brain injury), could change utilization patterns and highlight the importance of studying this new cohort of veterans.21,22
Evaluating the rate and types of medical services used by OEF/OIF veterans with and without mental disorders is critical in planning for the care of this growing population of returning veterans. The current climate of limited economic resources makes this information vital not only for the VA, but also for the numerous private and public healthcare institutions where returning veterans seek care. The primary objective of this study was to examine the association of PTSD and other mental disorders with non-mental health outpatient, inpatient, and emergency service utilization using national data from all returning OEF/OIF veterans who sought care at VA facilities. In addition, we determined whether other factors, such as demographics and military service characteristics, independently predicted increased utilization.
METHODS
Study Population
The VA OEF/OIF Roster is a database of veterans who have separated from OEF/OIF military service and have accessed VA healthcare.3 Because our research questions focused on mental health diagnoses associated with OEF/OIF military service, we made exclusions to yield a study population of OEF/OIF veterans who were new users of VA healthcare after the beginning of OEF or OIF. There were 366,417 veterans in the roster with a VA encounter by March 31, 2008. We excluded 36,108 veterans with a first visit prior to October 7, 2001, the date of the US invasion of Afghanistan, and 1,211 veterans who were killed in action during the study period. In addition, to allow all veterans to have at least 1 year of utilization of VA services, we excluded 79,658 veterans who had not had a clinical visit at a VA facility by March 31, 2007. Our final study population consisted of 249,440 separated OEF/OIF veterans who were new users of VA healthcare from October 7, 2001 to March 31, 2007 and who were followed through March 31, 2008. The study was approved by the Committee on Human Research, University of California, San Francisco, and the San Francisco VA Medical Center.
Measures
The OEF/OIF Roster includes demographic and military service information for each veteran. Scrambled social security numbers were used to link OEF/OIF Roster data to VA clinical data contained in the VA National Patient Care Database (NPCD) through March 31, 2008. The VA NPCD contains data from outpatient and inpatient visits, including the date of the visit, a code designating the type of visit, and the associated diagnosis(es) classified using the International Classification of Diseases, Ninth Revision Clinical Modification (ICD-9-CM) codes. We used ICD-9-CM codes to categorize veterans into three groups: those with no mental health diagnoses, those with mental health diagnoses other than PTSD (290.0–319.0, excluding 309.81), and those with PTSD (309.81) and co-morbid mental health diagnoses (if any).
Our primary outcome was utilization of non-mental health medical services. Therefore, we excluded outpatient visits to mental health services, inpatient visits with a primary code for a mental health diagnosis, and emergency visits with any code for mental health diagnoses. We used VA clinic codes to create seven categories of non-mental health services: primary care, medical/surgical subspecialty, ancillary services, diagnostic tests/procedures, emergency services, total outpatient services (all visits in the preceding categories), and inpatient hospitalizations.
Statistical Analyses
We examined the proportion of veterans accessing each of the service categories over the entire study period (the maximum amount of time a veteran could have been followed was October 7, 2001–March 31, 2008). We then used modified Poisson regression to compare utilization of each service category among the three mental health groups.23 Poisson regression models are used with count data, such as the number of visits per veteran in each service category. These models yielded a relative risk that compares utilization in veterans with mental health diagnoses (PTSD or mental health diagnosis other than PTSD) to those without mental health diagnoses. Adjusted models included age, sex, race, marital status, military component type (active duty vs. National Guard or Reserve), rank (enlisted vs. officer), branch (Army, Air Force, Marines, Navy/Coast Guard), multiple deployments, distance to and type of nearest VA facility (medical center vs. community-based outpatient clinic), and the number of months each veteran was in VA healthcare (calculated from the date of initial VA visit through study end date, March 31, 2008). We also adjusted for VA facility to account for regional patterns in coding or utilization.
During the study period, the VA provided OEF/OIF veterans free military service-related healthcare for 2 years from their date of military service separation (this was recently extended to 5 years in 2008). Following this period of free care, the cost of VA care is based on each veteran’s income and service-related medical conditions. This variation in cost may affect utilization of VA medical services.24 Thus, we also calculated utilization during each veteran’s first year of VA care to reduce differences in utilization based on cost of care. We chose a 1-year period because veterans may not access care immediately after service separation, and thus their period of free VA care may be less than 2 years. Given the greater proportion of zero count data (zero visits) in this shorter time period, negative binomial regression was used instead of modified Poisson regression. This yielded an incidence rate ratio for utilization of each service category. We controlled for the covariates described above excluding number of months in VA healthcare as 12 months of data were included for each veteran. We also conducted a sensitivity analysis with additional adjustment for the number of primary care visits to examine how primary care affected utilization of other types of services. In addition, we controlled for the number of mental health visits in order to explore whether mental health treatment affected utilization.
Finally, we used negative binomial regression to determine independent predictors of outpatient service utilization in each veteran’s first year of care by entering mental health status and all other sociodemographic and military service covariates simultaneously in the model. All analyses were performed using STATA software (version 9.2).
RESULTS
Prevalence of Mental Disorders
PTSD was the most common mental health diagnosis in the study population (21.5%), followed by depression (18.3%), adjustment disorder (11.1%), anxiety disorder (10.6%), substance use disorder (8.4%), and alcohol use disorder (7.3%). The characteristics of veterans by mental health category are presented in Table 1. Mental health diagnoses other than PTSD were more common in female veterans. PTSD was more common in male veterans and in younger veterans. Veterans of lower rank and those who had served in the Army and Marines were also more likely to be diagnosed with PTSD.
Table 1.
Demographic Characteristics of Veterans by Mental Health Category*†
| Variable | Total | No MH Dx | MH Dx (no PTSD) | PTSD (± other) |
|---|---|---|---|---|
| N = 249,440 | N = 157,844 n (%) | N = 37,868 n (%) | N = 53,728 n (%) | |
| Age, years | ||||
| 15–24 | 75,715 | 45,726 (60.4) | 11,859 (15.7) | 18,130 (24.0) |
| 25–29 | 65,117 | 39,734 (61.0) | 10,415 (16.0) | 14,968 (23.0) |
| 30–39 | 54,123 | 33,942 (62.7) | 8,085 (14.9) | 12.096 (22.4) |
| 40–49 | 44,059 | 31,239 (70.9) | 5,869 (13.3) | 6,951 (15.8) |
| 50–59 | 9,906 | 6,815 (68.8) | 1,568 (15.8) | 1,523 (15.4) |
| ≥60 | 505 | 374 (74.1) | 71 (14.1) | 60 (11.9) |
| Sex | ||||
| Male | 217,793 | 137,779 (63.3) | 31,936 (14.7) | 48,078 (22.1) |
| Female | 31,610 | 20,032 (63.4) | 5,929 (18.8) | 5,649 (17.9) |
| Race/ethnicity | ||||
| White | 166,509 | 105,484 (63.4) | 25,113 (15.1) | 35,912 (21.6) |
| Black | 41,700 | 26,320 (63.1) | 6,234 (15.0) | 9,146 (21.9) |
| Hispanic | 27,384 | 16,837 (61.5) | 4,613 (16.9) | 5,934 (21.7) |
| Other | 13,847 | 9,203 (66.5) | 1,908 (13.8) | 2,736 (19.8) |
| Marital status | ||||
| Married | 92,128 | 52,706 (57.2) | 15,131 (16.4) | 24,291 (26.4) |
| Never married | 87,565 | 50,671 (57.9) | 16,137 (18.4) | 20,757 (23.7) |
| Divorced, widowed, or separated | 22,725 | 11,119 (48.9) | 4,796 (21.1) | 6,810 (30.0) |
| Component type | ||||
| National Guard/Reserve | 123,604 | 78,858 (63.8) | 18,919 (15.3) | 25,827 (20.9) |
| Active duty | 125,836 | 78,986 (62.8) | 18,949 (15.1) | 27,901 (22.2) |
| Military rank | ||||
| Officer | 17,767 | 14,416 (81.1) | 1,698 (9.6) | 1,653 (9.3) |
| Enlisted | 231,673 | 143,428 (61.9) | 36,170 (15.6) | 52,075 (22.5) |
| Military branch | ||||
| Army | 163,335 | 97,561 (59.7) | 24,991 (15.3) | 40,783 (25.0) |
| Air Force | 28,684 | 23,093 (80.5) | 3,855 (13.4) | 1,736 (6.0) |
| Marines | 30,483 | 17,631 (57.8) | 4,123 (13.5) | 8,729 (28.6) |
| Navy/Coast Guard | 26,938 | 19,559 (72.6) | 4,899 (18.2) | 2,480 (9.2) |
| Multiple deployments | ||||
| Yes | 78,645 | 48,832 (62.1) | 11,193 (14.2) | 18,620 (23.7) |
| No | 170,795 | 109,012 (63.8) | 26,675 (15.6) | 35,108 (20.6) |
| Main VA facility type | ||||
| Medical center | 195,133 | 124,341 (63.7) | 29,597 (15.2) | 41,195 (21.1) |
| Outpatient clinic | 52,277 | 31,656 (60.6) | 8,156 (15.6) | 12,465 (23.8) |
| Distance to nearest VA | ||||
| ≤25 miles | 130,474 | 83,934 (64.3) | 20,094 (15.4) | 26,446 (20.3) |
| >25 miles | 117,146 | 72,779 (62.1) | 17,500 (14.9) | 26,866 (22.9) |
*† MH Dx = mental health diagnoses. Variables may contain missing data; therefore, numbers for each variable may not sum to total sample N of 249,440
Variations in Utilization of Non-mental Health Services by Mental Health Diagnoses
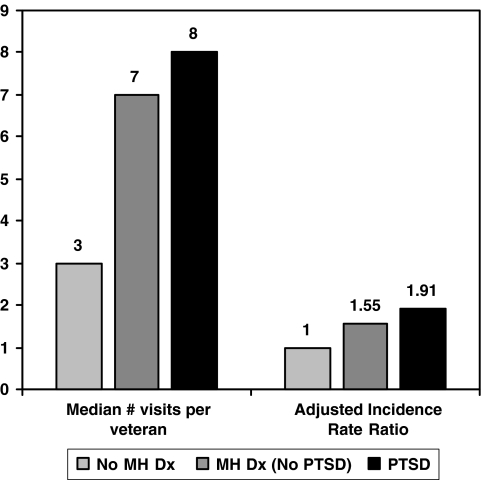
Table 2 shows unadjusted and adjusted utilization of non-mental health services over the entire study period, 2001–2008. In fully adjusted analyses, veterans with mental disorders had significantly greater utilization than veterans without mental disorders in all service categories (all P < 0.001). Veterans with PTSD had even greater utilization than those with other mental disorders (all P < 0.001). Figure 1 shows the median number of visits and the adjusted incidence rate ratios for total outpatient utilization in each veteran’s first year of VA care. Total outpatient utilization was 55% higher in those with mental disorders other than PTSD and 91% higher in veterans with PTSD than in those with no mental health diagnoses. Table 3 compares utilization in each veteran’s first year of VA care. In adjusted analyses, veterans with mental disorders had 42–146% greater utilization than those without mental disorders, depending on the service category (all P < 0.001). Those with PTSD had the highest utilization in all categories: 71–170% greater than those without mental disorders (all P < 0.001).
Table 2.
Utilization of Non-Mental Health Medical Services by Mental Health Category over the Entire Study Period (2001–2008)* †‡
| VA Medical Services | No MH Dx | MH Dx (no PTSD) | PTSD (± other) |
|---|---|---|---|
| N = 157,844 | N = 37,868 | N = 53,728 | |
| Primary care | |||
| Any visit: N (%) | 82,287 (52.1) | 32,903 (86.9) | 49,448 (92.0) |
| Unadjusted relative risk (95% CI) | 1.00 | 1.67 (1.66–1.68) | 1.77 (1.76–1.77) |
| Adjusted relative risk (95% CI) | 1.00 | 1.29 (1.28–1.30) | 1.34 (1.33–1.34) |
| Medical/surgical subspecialty | |||
| Any visit: N (%) | 55,501 (35.2) | 20,851 (55.1) | 33,527 (62.4) |
| Unadjusted relative risk (95% CI) | 1.00 | 1.57 (1.55–1.58) | 1.77 (1.76–1.79) |
| Adjusted relative risk (95% CI) | 1.00 | 1.37 (1.35–1.38) | 1.59 (1.58–1.61) |
| Ancillary services | |||
| Any visit: N (%) | 87,219 (55.3) | 28,614 (75.6) | 45,484 (85.0) |
| Unadjusted relative risk (95% CI) | 1.00 | 1.37 (1.36–1.38) | 1.54 (1.53–1.54) |
| Adjusted relative risk (95% CI) | 1.00 | 1.21 (1.20–1.22) | 1.35 (1.34–1.36) |
| Diagnostic tests/procedure | |||
| Any visit: N (%) | 120,896 (76.6) | 34,583 (91.3) | 50,995 (94.9) |
| Unadjusted relative risk (95% CI) | 1.00 | 1.19 (1.19–1.20) | 1.24 (1.24–1.24) |
| Adjusted relative risk (95% CI) | 1.00 | 1.14 (1.13–1.14) | 1.19 (1.18–1.19) |
| Emergency services | |||
| Any visit: N (%) | 38,534 (24.4) | 14,759 (40.6) | 22,724 (44.6) |
| Unadjusted relative risk (95% CI) | 1.00 | 1.66 (1.64–1.69) | 1.83 (1.80–1.85) |
| Adjusted relative risk (95% CI) | 1.00 | 1.32 (1.30–1.35) | 1.55 (1.52–1.57) |
| Inpatient | |||
| Any visit: N (%) | 2,935 (1.9) | 2,103 (5.8) | 3,519 (7.2) |
| Unadjusted relative risk (95% CI) | 1.00 | 3.11 (2.95–3.29) | 3.86 (3.68–4.05) |
| Adjusted relative risk (95% CI) | 1.00 | 2.34 (2.20–2.48) | 3.18 (3.01–3.36) |
*MH Dx = mental health diagnoses
†Relative risk adjusted for age, sex, race, marital status, component type, military rank, military branch, multiple deployments, main VA facility, facility type, distance to nearest VA, and months in VA healthcare
‡all adjusted relative risk between group comparisons P < 0.001
Figure 1.
Total outpatient utilization of non-mental health services during the first year of VA care by mental health category. MH Dx = mental health diagnoses. Incidence rate ratio adjusted for age, sex, race, marital status, component type, military rank, military branch, multiple deployments, main VA facility, VA facility type, and distance to nearest VA.
Table 3.
Utilization of Non-Mental Health Medical Services During the First Year of VA Care by Mental Health Category*†‡§
| VA Medical Services | No MH Dx | MH Dx (no PTSD) | PTSD (± other) |
|---|---|---|---|
| N = 157,844 | N = 37,868 | N = 53,728 | |
| Primary care | |||
| Median no. visits (IQR) | 0 (0–1) | 1 (0–3) | 2 (1–3) |
| No. visits/100 person years | 93 | 194 | 223 |
| Unadjusted IRR | 1.00 | 2.10 (2.07–2.13) | 2.41 (2.38–2.44) |
| Adjusted IRR | 1.00 | 1.61 (1.59–1.63) | 1.85 (1.83–1.88) |
| Medical/surgical subspecialty | |||
| Median no. visits (IQR) | 0 (0–1) | 0 (0–1) | 0 (0–2) |
| No. visits/100 person years | 59 | 106 | 130 |
| Unadjusted IRR | 1.00 | 1.79 (1.75–1.83) | 2.18 (2.14–2.22) |
| Adjusted IRR | 1.00 | 1.55 (1.51–1.58) | 1.95 (1.92–1.99) |
| Ancillary services | |||
| Median no. visits (IQR) | 0 (0–1) | 1 (0–3) | 1 (0–4) |
| No. visits/100 person years | 132 | 262 | 350 |
| Unadjusted IRR | 1.00 | 1.99 (1.95–2.03) | 2.66 (2.61–2.70) |
| Adjusted IRR | 1.00 | 1.67 (1.64–1.70) | 2.19 (2.16–2.23) |
| Diagnostic tests/procedures | |||
| Median no. visits (IQR) | 1 (0–3) | 3 (1–5) | 3 (1–6) |
| No. visits/100 person years | 213 | 368 | 427 |
| Unadjusted IRR | 1.00 | 1.72 (1.70–1.74) | 2.00 (1.98–2.02) |
| Adjusted IRR | 1.00 | 1.50 (1.48–1.51) | 1.82 (1.80–1.84) |
| Emergency services | |||
| Median no. visits (IQR) | 0 (0–0) | 0 (0–1) | 0 (0–1) |
| No. visits/100 person years | 31 | 54 | 60 |
| Unadjusted IRR | 1.00 | 1.75 (1.70–1.79) | 1.95 (1.91–1.99) |
| Adjusted IRR | 1.00 | 1.42 (1.39–1.46) | 1.71 (1.67–1.74) |
| Inpatient | |||
| Median no. visits (IQR) § | 0 (0–0) | 0 (0–0) | 0 (0–0) |
| No. visits/100 person years | 1.4 | 4.2 | 4.4 |
| Unadjusted IRR | 1.00 | 3.09 (2.85–3.35) | 3.29 (3.06–3.54) |
| Adjusted IRR | 1.00 | 2.46 (2.26–2.68) | 2.70 (2.50–2.92) |
*IRR = Incident rate ratio, IQR = interquartile range, MH Dx = mental health diagnoses
†IRR adjusted for age, sex, race, marital status, component type, military rank, military branch, multiple deployments, main VA facility, facility type, and distance to nearest VA
‡All adjusted IRR between group comparisons P < 0.001 except p = 0.04 for comparison of inpatient utilization between MH Dx (no PTSD) and PTSD (± other)
§Medians and interquartile range =0 for some categories because of the relatively low proportion of people utilizing those services
Additional adjustment for primary care visits attenuated the results but did not change our conclusions (utilization was 24–112% greater in those with mental health diagnoses and 39–110% greater in those with PTSD). Similarly, after adjustment for mental health visits, those with mental disorders had 38%–132% greater utilization in the various service categories and those with PTSD had 57–128% greater utilization.
Predictors of Highest Utilization
Table 4 shows the independent associations of demographic and military service characteristics with total outpatient utilization. After mental health status, female sex, older age, active duty status, and lower rank were associated with the largest increases in utilization.
Table 4.
Predictors of Total Outpatient Non-Mental Health Medical Service Utilization During First Year of VA Care*
| Incidence rate ratio (95% CI) † | |
|---|---|
| Mental health status | |
| No mental health diagnoses | 1.00 |
| Mental health diagnoses (no PTSD) | 1.58 (1.56–1.59) |
| PTSD (± other) | 1.95 (1.93–1.96) |
| Age, per 10 years | 1.15 (1.14–1.15) |
| Sex | |
| Male | 1.00 |
| Female | 1.23 (1.22–1.25) |
| Race | |
| White | 1.00 |
| Black | 1.04 (1.03–1.05) |
| Hispanic | 1.12 (1.10–1.13) |
| Other | 1.02 (1.01–1.04) |
| Marital status | |
| Married | 1.00 |
| Never married | 1.07 (1.06–1.08) |
| Divorced, widowed, or separated | 1.05 (1.03–1.06) |
| Component type | |
| National Guard/Reserve | 1.00 |
| Active duty | 1.18 (1.16–1.18) |
| Military rank | |
| Officer | 1.00 |
| Enlisted | 1.15 (1.14–1.16) |
| Military branch | |
| Army | 1.00 |
| Air Force | 0.98 (0.97–0.99) |
| Marines | 1.08 (1.07–1.09) |
| Navy/Coast Guard | 1.09 (1.07–1.10) |
| Multiple deployments | |
| No | 1.00 |
| Yes | 1.00 (0.99–1.01) |
| Nearest VA facility | |
| Community clinic | 1.00 |
| Medical center | 1.12 (1.11–1.13) |
| Distance to nearest VA, per 10 miles | 1.00 (1.00–1.00) |
*All variables in the table were included in a single model
†All P ≤ 0.001 except race, other p = 0.006, distance to nearest VA, p = 0.82
DISCUSSION
This is the first national study of VA non-mental health medical service utilization in veterans returning from Iraq and Afghanistan. In this population, those diagnosed with mental disorders had significantly greater utilization of all types of non-mental health outpatient, emergency, and inpatient medical services than those receiving no mental health diagnoses. Veterans diagnosed with PTSD had the greatest utilization in all service categories. In adjusted analyses, compared with those with no mental health diagnoses, total utilization of outpatient non-mental health services was 55% greater in veterans with mental health diagnoses other than PTSD and 91% greater in veterans with PTSD. Though mental health diagnostic status was the strongest independent predictor of utilization, female sex and lower rank were also associated with significantly greater utilization.
The higher rates of utilization among OEF/OIF veterans with mental disorders are notable because this is a relatively young population. The mean age in our study was 31 ± 9 years old, and only 4% were over 50 years of age. Comparing our results to utilization in non-VA populations is challenging because the demographic characteristics and categorization of services differ somewhat. Nevertheless, data from the 2004 United States National Ambulatory Medical Care Survey estimated that men aged 18–44 years (the closest demographic group to our population) had 1.36 general and specialty physician office visits per person.25 In our study, those with no mental health diagnoses had 1.52 primary care or medical/surgical subspecialty visits per year. Thus, VA non-mental health service utilization in OEF/OIF veterans with no mental disorders may approximate that of the general population, underscoring the increased need for veterans with mental disorders.
Our findings expand upon studies of mental disorders and utilization of medical services conducted in veterans of prior wars.11,15–19 In a study of 2,508 female veterans receiving care at an urban VA medical center between 1996 and 2000, Dobie and colleagues found that after adjusting for demographics, smoking, service access, and medical comorbidities, those who screened positive for PTSD had a significantly greater likelihood of having a medical or surgical hospitalization (OR 1.37, 95% CI 1.04–1.79).11 They were also significantly more likely to be in the highest quartile of utilization for emergency room, primary care, and ancillary services. Another study of 996 veterans, primarily from the Vietnam era, evaluated between 1992 and 1998, demonstrated that those who met criteria for PTSD had significantly greater utilization of non-mental health outpatient services than those without PTSD (median of 18 versus 10 visits per year).15 Other studies have demonstrated that the increase in health services utilization in veterans with PTSD is not due to co-morbid psychiatric conditions, such as anxiety and depression.26,27 Our study adds to this prior research by using national-level data, adjusting for several additional military service characteristics, and exploring utilization in OEF/OIF veterans, a group for which data are very limited.6
There are several possible explanations for our finding of increased utilization of non-mental health services in OEF/OIF veterans with mental disorders, particularly PTSD. First, exposure to combat or other traumatic events that resulted in mental health disorders may have also caused physical problems such as traumatic brain injury or musculoskeletal injuries.20,21 Second, mental disorders are frequently associated with somatic symptoms, and these physical symptoms as well as stigma surrounding mental health issues might prompt patients to seek care in non-mental health clinics.6 Third, mental disorders and PTSD may cause biological and behavioral changes that increase the risk of physical disease, leading to greater medical utilization.28, 29,12–14,30–34 Finally, there may be an increased likelihood of detection of medical problems in veterans with mental health problems, for example, through symptoms identified by mental health providers. Veterans with comorbid mental and physical problems may also be more likely to enroll in primary care, which could lead to increased utilization of other services, such as preventive screening through laboratory and diagnostic tests. However, we explored the influence of mental health and primary care visits in sensitivity analyses and found that these had only a modest effect on utilization.
Beyond mental health status, we examined several sociodemographic and military service characteristics as predictors of utilization. It is unclear whether the gender and racial differences in utilization seen in this study reflect disparities in general health, trauma exposure, preferences for VA care, or access to non-VA care.22,35 Prior studies have demonstrated that military sexual trauma is more common in female veterans and is associated with mental and physical comorbidities.36 Though we did not have data on military sexual trauma, it would be interesting to explore how this impacts gender differences in utilization. Our finding that active duty and lower rank veterans had increased utilization may be explained by the greater exposure to combat-related trauma in these veterans who were likely on the front lines.37 Other factors, such as differential access to private insurance in these generally younger veterans, could also affect utilization of VA care.38
Our results should be interpreted in light of several limitations. First, because we examined only OEF/OIF veterans who have accessed VA care, our findings may not generalize to all OEF/OIF veterans. Examining the effects of mental health conditions on utilization of non-VA services will provide valuable information for the many other systems that provide care to returning veterans. A second limitation is our use of ICD-9-CM diagnostic codes to classify veterans by mental health status. ICD-9-CM codes may be used by clinicians as “rule out” rather than definitive mental health diagnoses. However, in a prior study, we found that the majority of these diagnoses were confirmed on subsequent visits and by mental health providers.3 Still, reliance on ICD-9-CM codes could have led to over- or under-diagnosis of mental health conditions.
Third, because we defined mental health status by diagnoses made over the entire study period, some of a veteran’s utilization may have occurred prior to the date of diagnosis. However, it is well established that due to barriers in seeking and obtaining care, patients typically experience mental health symptoms for years prior to their date of diagnosis.38–40 In addition, we cannot determine the direction of the association between mental disorders and increased non-mental health service utilization. Finally, though our analyses provide information on veterans’ use of VA services, detailed economic analyses and analyses of the VA’s capacity to meet demand for services were beyond the scope of this study.
Despite these limitations, our findings have important implications for healthcare systems that care for returning OEF/OIF veterans and for future research directions. We found that mental health disorders and several demographic and military factors were associated with increased use of outpatient, emergency, and inpatient non-mental health services. As more veterans return home, many with mental and physical injuries, evaluating the capacity of the VA and other healthcare systems to meet these needs will be increasingly important. Future work should also explore how new models of care affect utilization in veterans with comorbid mental and physical health problems. For example, integrating mental health and primary care is a priority in the VA as it can reduce stigma and improve access to mental health treatment. Though such integration of care has been found to improve clinical outcomes, its affect on utilization deserves further study.9 This information could be used to improve the quality and efficiency of care for returning veterans and to guide allocation of resources to ensure the medical needs of the growing veteran population are met.
Acknowledgments
We acknowledge and thank veterans of the wars in Iraq and Afghanistan for their service. This study was funded by a VA Health Services Research and Development (HSR&D) Career Development Transition Award and a grant from the VA Seattle Epidemiological Research and Information Center. Dr. Cohen was supported by NIH/NCRR/OD UCSF-CTSI grant no. KL2 RR024130. We are grateful for the support of the San Francisco VA Medical Center HSR&D Research Enhancement Award Program (REA 01–097). The manuscript contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH or other funding agencies. Preliminary data for this paper were presented as an abstract at the Society of General Internal Medicine 2008 National Meeting.
The authors have no conflicts of interest.
References
- 1.Hoge CW, Auchterlonie JL, Milliken CS. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA. 2006;295:1023–1032. doi: 10.1001/jama.295.9.1023. [DOI] [PubMed] [Google Scholar]
- 2.Milliken CS, Auchterlonie JL, Hoge CW. Longitudinal assessment of mental health problems among active and reserve component soldiers returning from the Iraq war. JAMA. 2007;298:2141–2148. doi: 10.1001/jama.298.18.2141. [DOI] [PubMed] [Google Scholar]
- 3.Seal KH, Bertenthal D, Miner CR, Sen S, Marmar C. Bringing the war back home: mental health disorders among 103,788 US veterans returning from Iraq and Afghanistan seen at Department of Veterans Affairs facilities. Arch Intern Med. 2007;167:476–482. doi: 10.1001/archinte.167.5.476. [DOI] [PubMed] [Google Scholar]
- 4.Seal KH, Metzler T, Gima K, Bertenthal D, Maguen S, Marmar CR. Trends and risk factors for mental health diagnoses among Iraq and Afghanistan veterans using Department of Veterans Affairs healthcare, 2002–2008. AJPH 2008;99:1651–8. [DOI] [PMC free article] [PubMed]
- 5.Friedman MJ. Acknowledging the psychiatric cost of war. N Engl J Med. 2004;351:75–77. doi: 10.1056/NEJMe048129. [DOI] [PubMed] [Google Scholar]
- 6.Hoge CW, Terhakopian A, Castro CA, Messer SC, Engel CC. Association of posttraumatic stress disorder with somatic symptoms, health care visits, and absenteeism among Iraq war veterans. Am J Psychiatry. 2007;164:150–153. doi: 10.1176/appi.ajp.164.1.150. [DOI] [PubMed] [Google Scholar]
- 7.Kulka RA, Schlenger WE, Fiarbank JA, et al. Trauma and the Vietnam War Generation: Findings from the National Vietnam Veterans Readjustment Study. New York; 1990.
- 8.Long JA, Polsky D, Metlay JP. Changes in veterans’ use of outpatient care from 1992 to 2000. Am J Public Health. 2005;95:2246–2251. doi: 10.2105/AJPH.2004.061127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zeiss AM, Karlin BE. Integrating mental health and primary care services in the Department of Veterans Affairs healthcare system. J Clin Psychol Med Settings. 2008;15:73–78. doi: 10.1007/s10880-008-9100-4. [DOI] [PubMed] [Google Scholar]
- 10.Erbes C, Westermeyer J, Engdahl B, Johnsen E. Post-traumatic stress disorder and service utilization in a sample of service members from Iraq and Afghanistan. Mil Med. 2007;172:359–363. doi: 10.7205/milmed.172.4.359. [DOI] [PubMed] [Google Scholar]
- 11.Dobie DJ, Maynard C, Kivlahan DR, et al. Posttraumatic stress disorder screening status is associated with increased VA medical and surgical utilization in women. J Gen Intern Med. 2006;21(Suppl 3):S58–S64. doi: 10.1111/j.1525-1497.2006.00376.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Boscarino JA. Diseases among men 20 years after exposure to severe stress: implications for clinical research and medical care. Psychosom Med. 1997;59:605–614. doi: 10.1097/00006842-199711000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Boscarino JA. Posttraumatic stress disorder and mortality among U.S. Army veterans 30 years after military service. Ann Epidemiol. 2006;16:248–256. doi: 10.1016/j.annepidem.2005.03.009. [DOI] [PubMed] [Google Scholar]
- 14.Kang HK, Bullman TA, Taylor JW. Risk of selected cardiovascular diseases and posttraumatic stress disorder among former World War II prisoners of war. Ann Epidemiol. 2006;16:381–386. doi: 10.1016/j.annepidem.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 15.Calhoun PS, Bosworth HB, Grambow SC, Dudley TK, Beckham JC. Medical service utilization by veterans seeking help for posttraumatic stress disorder. Am J Psychiatry. 2002;159:2081–2086. doi: 10.1176/appi.ajp.159.12.2081. [DOI] [PubMed] [Google Scholar]
- 16.Druss BG, Rosenheck RA. Use of medical services by veterans with mental disorders. Psychosomatics. 1997;38:451–458. doi: 10.1016/S0033-3182(97)71422-1. [DOI] [PubMed] [Google Scholar]
- 17.Schnurr PP, Friedman MJ, Sengupta A, Jankowski MK, Holmes T. PTSD and utilization of medical treatment services among male Vietnam veterans. J Nerv Ment Dis. 2000;188:496–504. doi: 10.1097/00005053-200001000-00012. [DOI] [PubMed] [Google Scholar]
- 18.Elhai JD, North TC, Frueh BC. Health service use predictors among trauma survivors: a critical review. Psychological Services. 2005;2:3–19. doi: 10.1037/1541-1559.2.1.3. [DOI] [Google Scholar]
- 19.Richardson JD, Elhai JD, Pedlar DJ. Association of PTSD and depression with medical and specialist care utilization in modern peacekeeping veterans in Canada with health-related disabilities. J Clin Psychiatry. 2006;67:1240–1245. doi: 10.4088/JCP.v67n0810. [DOI] [PubMed] [Google Scholar]
- 20.Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery. In: Tanielian T, Jaycox LH, eds. Santa Monica: RAND Corporation; 2008.
- 21.Hoge CW, McGurk D, Thomas JL, Cox AL, Engel CC, Castro CA. Mild traumatic brain injury in U.S. Soldiers returning from Iraq. N Engl J Med. 2008;358:453–463. doi: 10.1056/NEJMoa072972. [DOI] [PubMed] [Google Scholar]
- 22.Frayne SM, Yu W, Yano EM, et al. Gender and use of care: planning for tomorrow’s Veterans Health Administration. J Womens Health (Larchmt) 2007;16:1188–1199. doi: 10.1089/jwh.2006.0205. [DOI] [PubMed] [Google Scholar]
- 23.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 24.Kussman M. Statement of the Deputy Under Secretary for Health, Department of Veterans’ Affairs, before the Committee on Veterans Affairs, U.S. House of Representatives; Washington, DC. July 27, 2005. 2005.
- 25.National Center for Health Statistics. Health, United States, 2006 With Chartbook on Trends in the Health of Americans. Hyattsville, MD; 2006. [PubMed]
- 26.Schnurr PP, Spiro A, 3rd, Paris AH. Physician-diagnosed medical disorders in relation to PTSD symptoms in older male military veterans. Health Psychol. 2000;19:91–97. doi: 10.1037/0278-6133.19.1.91. [DOI] [PubMed] [Google Scholar]
- 27.Marshall RP, Jorm AF, Grayson DA, O’Toole BI. Posttraumatic stress disorder and other predictors of health care consumption by Vietnam veterans. Psychiatr Serv. 1998;49:1609–1611. doi: 10.1176/ps.49.12.1609. [DOI] [PubMed] [Google Scholar]
- 28.Buckley TC, Mozley SL, Bedard MA, Dewulf AC, Greif J. Preventive health behaviors, health-risk behaviors, physical morbidity, and health-related role functioning impairment in veterans with post-traumatic stress disorder. Mil Med. 2004;169:536–540. doi: 10.7205/milmed.169.7.536. [DOI] [PubMed] [Google Scholar]
- 29.Schnurr PP, Green BL. Understanding relationships among trauma, post-tramatic stress disorder, and health outcomes. Adv Mind Body Med. 2004;20:18–29. [PubMed] [Google Scholar]
- 30.Bedi US, Arora R. Cardiovascular manifestations of posttraumatic stress disorder. J Natl Med Assoc. 2007;99:642–649. [PMC free article] [PubMed] [Google Scholar]
- 31.Gander ML, Kanel R. Myocardial infarction and post-traumatic stress disorder: frequency, outcome, and atherosclerotic mechanisms. Eur J Cardiovasc Prev Rehabil. 2006;13:165–172. doi: 10.1097/01.hjr.0000214606.60995.46. [DOI] [PubMed] [Google Scholar]
- 32.Killgore WD, Stetz MC, Castro CA, Hoge CW. The effects of prior combat experience on the expression of somatic and affective symptoms in deploying soldiers. J Psychosom Res. 2006;60:379–385. doi: 10.1016/j.jpsychores.2006.02.012. [DOI] [PubMed] [Google Scholar]
- 33.Kubzansky LD, Koenen KC, Spiro A, 3rd, Vokonas PS, Sparrow D. Prospective study of posttraumatic stress disorder symptoms and coronary heart disease in the Normative Aging Study. Arch Gen Psychiatry. 2007;64:109–116. doi: 10.1001/archpsyc.64.1.109. [DOI] [PubMed] [Google Scholar]
- 34.Vaccarino V, McClure C, Johnson BD, et al. Depression, the metabolic syndrome and cardiovascular risk. Psychosom Med. 2008;70:40–48. doi: 10.1097/PSY.0b013e31815c1b85. [DOI] [PubMed] [Google Scholar]
- 35.Washington DL, Yano EM, Horner RD. The health and health care of women veterans: perspectives, new insights, and future research directions. J Gen Intern Med. 2006;21:S3–S4. doi: 10.1111/j.1525-1497.2006.00367.x. [DOI] [Google Scholar]
- 36.Kimerling R, Gima K, Smith MW, Street A, Frayne S. The Veterans Health Administration and military sexual trauma. Am J Public Health. 2007;97:2160–2166. doi: 10.2105/AJPH.2006.092999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hoge CW, Toboni HE, Messer SC, Bell N, Amoroso P, Orman DT. The occupational burden of mental disorders in the U.S. military: psychiatric hospitalizations, involuntary separations, and disability. Am J Psychiatry. 2005;162:585–591. doi: 10.1176/appi.ajp.162.3.585. [DOI] [PubMed] [Google Scholar]
- 38.Milliken CS, Auchterlonie JL, Hoge CW. Longitudinal Assessment of Mental Health Problems Among Active and Reserve Component Soldiers Returning From the Iraq War. Jama. 2007;298:2141–2148. doi: 10.1001/jama.298.18.2141. [DOI] [PubMed] [Google Scholar]
- 39.Wang PS, Angermeyer M, Borges G, et al. Delay and failure in treatment seeking after first onset of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry. 2007;6:177–185. [PMC free article] [PubMed] [Google Scholar]
- 40.Wang PS, Berglund P, Olfson M, Pincus HA, Wells KB, Kessler RC. Failure and delay in initial treatment contact after first onset of mental disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:603–613. doi: 10.1001/archpsyc.62.6.603. [DOI] [PubMed] [Google Scholar]