Abstract
Background
Effective communication is vital for optimal medical consultation, but there is little current information about physician preferences for effective consultation.
Methods
We invited physicians with at least one post-graduate year of experience at four Minnesota teaching hospitals to complete a 16-question Internet questionnaire about inpatient consultations.
Results
E-mail requests were received by an estimated 651 physicians. Questionnaires were completed by 323 (50%). Of these, 54% had completed training >5 years before, 17% had completed training <5 years before, and 30% were residents or fellows. Three elements were considered essential in consultation requests by most respondents: the specific question to be addressed (94%), whom to call with the response (68%), and consultation urgency (66%). In the consultation note, 71% of subjects placed high importance on simple, concise recommendations and 64% on the rationale behind them, while only 7% placed high importance on citing references. Most (69%) preferred that assessments and recommendations be written in bulleted or numbered format. A plurality (48%) preferred that assessments and recommendations be separated. Most placed high value on recommendations regarding drug therapy that specify dose (80%), duration (80%), and generic medication name (62%). Requesters placed greater importance than consultants (87% vs. 65%, respectively, P = 0.004) on recommendations that included duration of therapy. The majority (63%) stated that telephone requests were needed for emergent or urgent consultations. Those who usually requested consultations were more likely than those who usually responded to consultation requests to prefer telephone requests for routine consultations (43% vs. 20%, P < 0.001).
Conclusions
Physicians agreed on many essential elements for effective consultations. These results should guide efforts to improve communication in the consultation process and design electronic medical record systems.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-009-1142-2) contains supplementary material, which is available to authorized users.
KEY WORDS: referral and consultation, graduate medical education, health care surveys, interprofessional relations
INTRODUCTION
Consultations are common, important components of medical care, but most studies have found that the quality and effectiveness of consultations are variable.1–5 As practice patterns and roles of different specialties evolve,5,6 the elements that make consultation an effective communication process or lead to improved patient outcomes should also evolve.1–5,7 Training programs must prepare physicians for participation in the consultation process later in their careers.8,9 In any setting, ineffective consultations diminish the quality of patient care and education and frustrate physicians and patients.
Widespread adoption of electronic medical record (EMR) systems, especially those with computerized provider order entry, provide many opportunities to improve the consultation process for the benefit of both patients and providers. To provide current information on how consultations can be most effective and how EMR systems might improve consultations, we surveyed physicians to learn what their preferences were for elements of an ideal inpatient medical consultation.
METHODS
The survey was a component of an ongoing quality improvement initiative regarding the consultation process at the Minneapolis Veterans Affairs Medical Center (MVAMC), a teaching hospital affiliated with the University of Minnesota. Since faculty at other university-affiliated hospitals influence house staff attitudes and practices regarding consultations, we included faculty at three other tertiary care hospitals affiliated with the university. The University of Minnesota Medical Center (UMMC) in Minneapolis is owned by an integrated health network. Hennepin County Medical Center (HCMC) is a level 1 trauma center in Minneapolis. Regions Hospital (RH) is a level 1 trauma center in St. Paul, Minnesota, and is owned by a health maintenance organization cooperative. MVAMC had a comprehensive EMR system, and consultation requests and responses were done within that system. At the time of the survey, consultations were requested at UMMC, HCMC, and RH by page or telephone, and consultation responses were written, without templates, on paper charts.
We identified 893 physicians with at least one post-graduate year of experience at four teaching hospitals in July 2005. Lists of names and e-mail addresses were obtained from administrators at the four hospitals. The invitations stated the survey’s purpose and included a survey link. The survey consisted of 16 questions about inpatient consultation (Appendix 1, available online). Four questions were about career status and type of practice. One question asked each respondent the proportion of consultations in which the respondent initiated or responded to consultation requests. Respondents were classified as trainees (residents or fellows), staff <5 years after completion of training, or staff >5 years after completion of training. Two questions asked about the importance of elements of a consultation request. One asked about use of alphanumeric pages for communication. Six questions asked about the importance of elements of a consultation response. One question asked about whether a consultant should sign off once involvement was no longer necessary. For multiple-choice questions, answers were presented in random order to prevent any response-order bias. Free-text response fields were provided for questions to provide respondents the opportunity to elaborate on their answers or offer alternatives. A reminder e-mail was sent to non-respondents 2 weeks later. Participants who completed the questionnaire were entered into a drawing for a book.
Data analysis was primarily descriptive. For comparisons between categorical variables, likelihood ratio chi-square analysis was performed with presentation of odds ratio (OR), 95% confidence interval (CI), and two-sided p-values. The threshold for statistical significance was P < 0.05. For ordinal rank data that were not distributed normally, the Mann-Whitney test was used. Where multiple variables were statistically significant by univariate analysis, multivariate logistic regression was used to test for the main effects and interactions between these variables. Significant differences were presented as adjusted OR. The MVAMC Institutional Review Board approved this project.
RESULTS
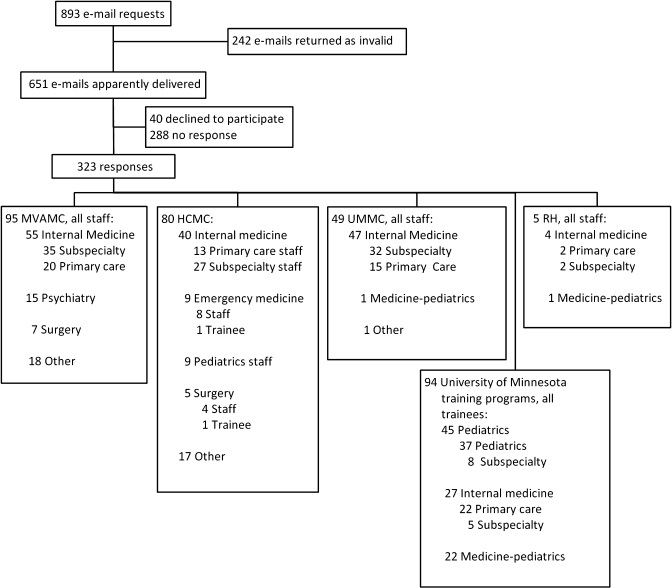
For 242 of the 893 physicians initially identified, e-mails were returned because addresses were no longer valid (Fig. 1). Of the remaining 651 physicians, 323 (50%) completed the survey, 40 (6%) declined, and 288 (44%) did not respond. Of the 323 respondents, 96 (30%) were trainees, 54 (17%) were staff <5 years after completion of training, and 173 (54%) were staff >5 years after completion of training. Twenty-eight percent of trainees were in internal medicine, 46% were in pediatrics, and 23% were in medicine-pediatrics (Table 1). Only 3.7% of all respondents were surgeons. Primary locations of staff were 42% at MVAMC, 34% at HCMC, 22% at UMMC, and 2% at RH.
Figure 1.
Distribution of subjects and respondents.
Table 1.
Composition of Survey Respondents
| Typical role in consultations, n (%) | ||||
|---|---|---|---|---|
| Specialty | Request >60% | Approx. equal | Answer >60% | Total |
| Internal Medicine | 72 (49) | 35 (55) | 66 (61) | 173 (54) |
| Pediatrics | 40 (27) | 9 (14) | 5 (4.6) | 54 (17) |
| Med-Peds | 14 (9.5) | 6 (9.4) | 1 (0.9) | 21 (6.5) |
| Psychiatry | 7 (4.7) | 5 (7.8) | 5 (4.6) | 17 (5.3) |
| Surgery | 0 (0) | 3 (4.7) | 9 (8.3) | 12 (3.7) |
| Emergency Medicine | 8 (5.4) | 1 (1.6) | 0 (0) | 9 (2.8) |
| Othera | 7 (4.7) | 5 (7.8) | 23 (21) | 35 (11) |
| Total | 148 (100) | 64 (100) | 109 (100) | 321 (100) |
aOther included 6 family practice, 6 physical medicine and rehabilitation, 5 neurology, 4 dermatology, 3 dentistry-prosthodontics, 3 obstetrics and gynecology, 2 health psychology, and 1 each of anesthesia, medical genetics, pathology, podiatry, and radiation oncology and 2 who did not respond to this question
To understand perspectives of those who usually requested consultations and those who usually provided consultations, we classified respondents into three groups. Requesters included 83 (26%) who requested consultations >90% of the time and 65 (20%) who requested consultations from 61 to 90% of the time (Table 1). Consultants included 47 (15%) who consulted from 61 to 90% of the time and 62 (19%) who consulted more than 90% of the time. The remaining 64 (20%) requested and consulted each about half of the time (40% to 60%).
Consultation Request
For our respondents, the most important element of a high quality consultation request was for the requester to clearly frame the consultation question for the consultant (Table 2). The issue of whom to contact with consultation responses was a common concern, with 68% ranking it as “essential,” second only to providing a specific consultation question (94%). Most respondents felt it was important for requesters to indicate the urgency of consultation requests. The responses of those who usually requested consultations and those who usually consulted were similar. Results did not vary substantially by job classification, hospital, department, or experience of responders.
Table 2.
Importance of Elements of a Consultation Request
| Perceived importance n (%) | ||||
|---|---|---|---|---|
| Consultation element | Essential | Moderate | Minimal | Unimportant |
| Consultation question | 296 (94) | 16 (5) | 3 (1) | 0 (0) |
| Whom to call with response | 214 (68) | 76 (24) | 25 (8) | 0 |
| Urgency | 208 (66) | 95 (30) | 12 (4) | 0 |
| HPI (brief) | 145 (46) | 123 (39) | 41 (13) | 6 (2) |
| Patient location | 145 (46) | 80 (25) | 64 (20) | 26 (8) |
| Diagnostic workup to date | 120 (38) | 142 (45) | 44 (14) | 9 (3) |
| Reason for hospitalization | 117 (37) | 132 (42) | 47 (15) | 19 (6) |
| Relevant labs | 101 (32) | 132 (42) | 66 (21) | 16 (5) |
| Current therapy/plan | 98 (31) | 147 (47) | 57 (18) | 13 (4) |
| Previous consultation in field | 72 (23) | 132 (42) | 86 (27) | 25 (8) |
| Co-morbidities | 70 (22) | 140 (44) | 92 (29) | 13 (4) |
| Past medical history | 63 (20) | 139 (44) | 100 (32) | 13 (4) |
| Physical examination | 60 (19) | 88(28) | 126 (40) | 41 (13) |
| Code status | 25 (8) | 80 (25) | 127 (40) | 83 (26) |
One question asked when the requester should telephone to notify the consultant that a consultation was requested. Most (242, 75%) survey respondents preferred that requests for emergent consultations be made by telephone. Requesters were twice as likely as consultants (43% vs. 20%) to prefer telephone contact when requesting a routine consultation (RR 2.1; 95% CI: 1.4 to 3.2; P < 0.001). Physicians at the MVAMC were more likely than physicians at other hospitals to prefer that emergency consultation requests be made by telephone (OR: 3.2; 95% CI: 1.8 to 6.2; P < 0.001) and less likely to prefer telephone requests for routine consultation requests (OR: 0.15; 95% CI: 0.06 to 0.37; P < 0.001).
Consultation Response
Respondents were asked how consultants should communicate with requesters when a non-emergent consultation was completed. Respondents preferred that consultants communicate recommendations verbally (best) in addition to a written report or by leaving a written note only (second best, Table 3). Consultants were more likely than requesters to prefer use of an alert in the hospital electronic medical record system (EMR) to notify a requester that a consultation had been completed (P < 0.001). Alphanumeric text messaging was least popular and considered by many respondents to be unreliable. Opinions about text messaging varied markedly with career status. Trainees were more likely than staff to view alphanumeric text paging as useful for consultation requests (39%; OR for trainees vs. staff 2.7; 95% CI: 1.5 to 4.8; P = 0.001), routine consultation recommendations (41%; OR for trainees vs. staff: 3.2; 95% CI: 1.8 to 5.7; P < 0.001), and general updates (41%; OR for trainees vs. staff: 5.4; 95% CI: 2.9 to 10.0; P < 0.001). Many survey respondents emphasized in free-text comments that verbal communication was highly desirable and enhanced written consultation responses.
Table 3.
Preferences for How a Consultant Should Communicate with Requester When a Non-emergent Consultation Has Been Completed
| Method | Preference n (%) | |||
|---|---|---|---|---|
| Best | 2nd Best | 3rd Best | Least | |
| Verbally | 112 (40) | 77 (27) | 63 (22) | 30 (11) |
| Written note | 86 (31) | 97 (35) | 59 (21) | 38 (14) |
| Electronic medical record alert | 82 (30) | 58 (21) | 71 (26) | 65 (24) |
| Text message paging | 24 (9) | 46 (17) | 69 (26) | 129 (48) |
Respondents expressed strong preferences regarding the format for consultation recommendations. A majority (69%) preferred that recommendations be bulleted or numbered rather than written in paragraph format. More respondents preferred assessments and recommendations in separate sections (48%) than combined by problem (37%). Forty-eight percent preferred recommendations be placed at the bottom and 26% preferred that recommendations be placed at the top of the consultation response.
Respondents valued simple concise recommendations in a consultation response along with the rationale to support the recommendations (Table 4). Respondents placed little value on references to support recommendations. Requesters were more likely than consultants (47% vs. 29%, respectively, P = 0.05) to consider it important that the consultant provide recommendations for future steps depending on outcomes of more proximal decisions or actions.
Table 4.
Characteristics and Content of New Recommendations
| Importance | ||||
|---|---|---|---|---|
| Characteristics or content | High | Moderate | Minimal | Unimportant |
| Simple, concise | 208 (71) | 70 (24) | 14 (4.8) | 1 (0.3) |
| Rationale behind decision making | 188 (64) | 100 (34) | 5 (1.7) | 0 (0) |
| Future decisions based on current plan | 117 (38) | 155 (53) | 26 (8.9) | 2 (0.6) |
| Differential diagnosis | 110 (38) | 155 (52) | 26 (8.9) | 2 (0.7) |
| Literature references as support | 20 (6.8) | 114 (39) | 143 (49) | 16 (5.5) |
For consultation responses that recommend a new drug, 80% felt that the generic name was of great or moderate importance, while only 28% felt that the brand name was of great or moderate importance (P < 0.001). Eighty percent of respondents placed great importance on recommendations that included the dose and duration of new drugs. Requesters placed greater importance than consultants did (87% vs. 65%, respectively, P = 0.004) on recommendations that included duration of therapy. Seventy-six percent of all respondents placed great or moderate importance on consultation responses that recommended one or more alternative therapies.
Consultation Sign Off
When active involvement of the consultant was no longer needed, the majority (76%) of respondents felt the consultant should write a sign-off note and stop following the patient. Eighteen percent preferred that the consultant write a sign-off note but keep track of the patient without being actively involved. Preferences for sign-off were similar for residents and staff and similar for requesters and consultants.
Seventy-four percent of respondents felt the consultant should recommend a general time frame for follow-up care, 44% percent desired that the consultant schedule a follow-up appointment, and 37% desired that the consultant specify a detailed outpatient management plan. These preferences were similar for requesters and consultants. Respondents volunteered that when they saw patients following hospitalizations that included consultations for specific problems, the respondents often had difficulty discerning the management plans for the problems.
DISCUSSION
This study confirms many elements of effective consultation and provides several new insights. Some findings have implications for evolution in the approach to consultations as the penetration of EMRs in US medicine continues to increase and as practice patterns evolve in different specialties.5,6
Our results reinforce that the first priority for a consultation request is that it state clearly the question or reason for consultation.2,5,7,10,11 In a previous study in which both requestor and consultant were interviewed after consultations, disagreement about the consultation question occurred in 21%.2 Our results supported and extended other tenets of effective consultation, including that requests indicate urgency, and that consultants should keep notes and recommendations concise.1–3,5,7,10
This study added new insights. Our respondents emphasized the need for consultants to clearly indicate when they will no longer follow a patient, often referred to as a “sign-off note.” Previous authors have emphasized that consultants should follow up after recommendations are made,7 but to our knowledge none has emphasized that the consultant should let the requestor know when the consultant is no longer following the patient. Without a sign-off note, absence of a comment or a note may be interpreted by the requester as agreement or acquiescence with the current patient management or lack of need to test further or change course. This ambiguity can be avoided with a note specifying that the consultant will no longer be involved in a case. If a consultant has signed off, and there are further questions, the requestor will know to contact the consultant again.
Our respondents answered that consultants who recommend new drug therapy should specify dosage and duration of new drugs. Requesters placed greater value on details of duration than did consultants. Inclusion of specific details has been associated with greater likelihood that drug therapy recommendations will be heeded.1,4 Generic drug names were much preferred over brand names, which may signal lessening of the influence of pharmaceutical industry marketing compared with non-commercial sources of information on drug effectiveness and costs or may reflect the academic nature of study hospitals.
The numbers of physicians involved in inpatient care has steadily increased, and immediate responsibility for care changes multiple times during typical hospitalizations, which necessitates what are frequently called “handoffs.”12 Respondents seemed to have this in mind when they answered that a consultation request should clearly specify the person that the consultant should contact and how the contact should occur.
The preference among consultants for use of an EMR alert to notify a requester that a consultation has been completed may reflect difficulty in knowing whom to contact. The efficiency of the Veterans Affairs EMR may have been one reason why MVAMC practitioners preferred that requests for routine consultation be made through the EMR. Interestingly, alphanumeric text messaging was least popular and considered by many respondents to be unreliable because of lack of verification that messages were received or understood.
Legibility has long been an issue,3 becoming less so as EMRs replace paper charts with handwritten notes. But legibility does not guarantee comprehensibility.13 Our respondents placed great value on consultation responses that were written clearly and concisely, listed specific recommendations, and outlined the rationale for the recommendations. Large majorities preferred assessments and recommendations in numbered or bulleted lists rather than in paragraphs.
While the EMR facilitates communication, 67 percent of respondents ranked verbal communication of the essence of the consultation response best or second best. Many previous reports have emphasized the importance of verbal communication between consultant and requestor.3,5,7,14 An alternative view was posed by a study of outpatient consultations in which the content of the communication was more important that the mode of communication.15 The evidence suggests that the advantage of verbal communication between consultant and requester is that it increases the likelihood that communication will be accurate, comprehensive, and understood and that the consultant will be available for questions or further discussion.
Respondents preferred consultations that recommend a specific follow-up plan and decisions for future management based on results of more proximate steps. While such plans and decisions may be intuitive for consultants, primary physicians felt these elements should be included in the consultation response. A sign-off note would be a good place to recommend follow-up and future management plans because it would be easily identifiable later on. Previous studies found a positive association between the number of “follow-up” notes written by consultants and the likelihood that the recommendations would be followed.1,7 Some authorities have recommended that contingency plans be provided,7 but we are unaware of empirical data on whether better outcomes are associated with follow-up notes or contingency plans.
Respondents wanted consultants to state the rationale supporting recommendations, but they did not care much about references to support the recommendations. Some authorities have suggested that references be supplied judiciously,7 but a recent survey found that only 27% of physicians felt that literature references are useful as part of the consult.5 It may be that physicians in large, metropolitan hospitals have easy, quick access to secondary and tertiary sources for guidelines and review articles and may not have interest or time in reading articles cited in consultation responses.
This survey had both strengths and weaknesses. The 50% response rate, good for surveys of this type, was a limitation, and surgeons and surgical-subspecialists made up only 3.7% of respondents. Seventy-eight percent practiced in internal medicine and/or pediatrics, and the results are most likely reflective of these disciplines. Some questions allowed respondents to rate many consultation elements positively rather than constraining them to prioritize. It was difficult in some cases to discern the elements that were truly critical in the minds of respondents. The study was done in four independent hospitals with individual affiliations with a single medical school and was limited to inpatient consultations, and the results may not be fully applicable to other settings. A strength was that many questions asked about specific details that have practical importance in daily work. Another was that we were able to compare responses of physicians who usually requested consultations with responses of physicians who were usually consultants. This was an opinion survey, and we did not measure the impact of respondents’ preferences on patient outcomes.
Our results have implications for development of consultation guidelines and policies, education, and possible incorporation into service level agreements between requestors and consultants.5,6 Physicians in training have been involved in the consultation process for decades,9,16 and the most recent Accreditation Council for Graduate Medical Education (ACGME) education requirements state that internal medicine residents must have a structured clinical experience to act, under supervision, as consultants to physicians in other specialties.17 Until recently research on how to educate physicians on how to most effectively request or respond to consultations has been meager.8,16
EMRs provide powerful opportunities to improve the consultation process. Templates should be developed for both requesters and consultants to encourage adoption of the specific characteristics this and previous studies have found are desired or associated with improved adherence to recommendations or better patient outcomes. A provider who requests a consultation may not be on duty when the consultation is completed. EMRs should enable a requester to designate one or more surrogates who would be alerted if a consultation is completed when the requester is off duty. EMRs should have a separate template and note title for consultation sign-off notes so that others are able to easily locate and understand the recommended plan. By standardizing consultations, EMR templates could facilitate research that would determine which of the popular elements of consultation requests or responses are associated with improved outcomes.
Other changes in delivery of care and practice patterns will also influence how consultations should be done. These changes include demands for surgeons to spend more of their time in operations, increased prevalence of co-management involving requesters and consultants, and an increasing percentage of consultations performed by medical subspecialists as opposed to general internists.5 Consultation tools within EMR systems should be designed to reflect these changes. Several previous studies have shown that a portion of consultant recommendations are not followed.3,4,18 While there may be valid reasons for some of this lack of conformance with consultant recommendations, non-conformance often reflects failures of communication or follow-through or lack of familiarity with how to carry out recommendations.3–5,18 A recent study showed that an EMR tool that allowed referring providers to review and implement electronic recommendations from consultants improved the percentage of recommendations that were implemented.19
This and previous studies have documented elements considered important for effective consultations. The recent studies show how consultations can be most effective with current practice patterns and technology. The evidence should guide efforts to improve the consultation process through policy, service level agreements, and EMR design.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors wish to thank Drs. Cristina Baker and Michael Aylward for conceptual discussions. DRB is supported by the National Institute of Allergy and Infectious Diseases (T32AI055433; L30AI066779; K12RR023247). Parts of the material were presented at the Infectious Diseases Society of America Annual Meeting, San Diego, CA, October 5, 2007.
All authors meet authorship criteria and have no financial conflicts of interest. GAF is a federal employee.
References
- 1.Horwitz RI, Henes CG, Horwitz SM. Developing strategies for improving the diagnostic and management efficacy of medical consultations. J Chronic Dis. 1983;36:213–218. doi: 10.1016/0021-9681(83)90096-6. [DOI] [PubMed] [Google Scholar]
- 2.Lee T, Pappius EM, Goldman L. Impact of inter-physician communication on the effectiveness of medical consultations. Am J Med. 1983;74:106–112. doi: 10.1016/0002-9343(83)91126-9. [DOI] [PubMed] [Google Scholar]
- 3.Lo E, Rezai K, Evans AT, et al. Why don't they listen? Adherence to recommendations of infectious disease consultations. Clin Infect Dis. 2004;38:1212–1218. doi: 10.1086/383315. [DOI] [PubMed] [Google Scholar]
- 4.Popkin MK, Mackenzie TB, Hall RC, Garrard J. Physicians' concordance with consultants' recommendations for psychotropic medication. Arch Gen Psychiatry. 1979;36:386–389. doi: 10.1001/archpsyc.1979.01780040028002. [DOI] [PubMed] [Google Scholar]
- 5.Salerno SM, Hurst FP, Halvorson S, Mercado DL. Principles of effective consultation: An update for the 21st-century consultant. Arch Intern Med. 2007;167:271–275. doi: 10.1001/archinte.167.3.271. [DOI] [PubMed] [Google Scholar]
- 6.Linzer M, Myerburg RJ, Kutner JS, et al. Exploring the generalist-subspecialist interface in internal medicine. Am J Med. 2006;119:528–537. doi: 10.1016/j.amjmed.2006.03.007. [DOI] [PubMed] [Google Scholar]
- 7.Goldman L, Lee T, Rudd P. Ten commandments for effective consultations. Arch Intern Med. 1983;143:1753–1755. doi: 10.1001/archinte.143.9.1753. [DOI] [PubMed] [Google Scholar]
- 8.Devor M, Renvall M, Ramsdell J. Practice patterns and the adequacy of residency training in consultation medicine. J Gen Intern Med. 1993;8:554–560. doi: 10.1007/BF02599639. [DOI] [PubMed] [Google Scholar]
- 9.Moore RA, Kammerer WS, McGlynn TJ, Trautlein JJ, Burnside JW. Consultations in internal medicine: A training program resource. J Med Educ. 1977;52:323–327. doi: 10.1097/00001888-197704000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Sibert L, Lachkar A, Grise P, Charlin B, Lechevallier J, Weber J. Communication between consultants and referring physicians: A qualitative study to define learning and assessment objectives in a specialty residency program. Teach Learn Med. 2002;14:15–19. doi: 10.1207/S15328015TLM1401_5. [DOI] [PubMed] [Google Scholar]
- 11.Conley J, Jordan M, Ghali WA. Audit of the consultation process on general internal medicine services. Qual Saf Health Care. 2009;18:59–62. doi: 10.1136/qshc.2007.025486. [DOI] [PubMed] [Google Scholar]
- 12.Landrigan CP, Czeisler CA, Barger LK, et al. Effective implementation of work-hour limits and systemic improvements. Jt Comm J Qual Patient Saf. 2007;33:19–29. doi: 10.1016/s1553-7250(07)33110-3. [DOI] [PubMed] [Google Scholar]
- 13.Hayrinen K, Saranto K, Nykanen P. Definition, structure, content, use and impacts of electronic health records: A review of the research literature. Int J Med Inform. 2008;77:291–304. doi: 10.1016/j.ijmedinf.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 14.Haldis TA, Blankenship JC. Telephone reporting in the consultant-generalist relationship. J Eval Clin Pract. 2002;8:31–35. doi: 10.1046/j.1365-2753.2002.00313.x. [DOI] [PubMed] [Google Scholar]
- 15.Byrd JC, Moskowitz MA. Outpatient consultation: Interaction between the general internist and the specialist. J Gen Intern Med. 1987;2:93–98. doi: 10.1007/BF02596304. [DOI] [PubMed] [Google Scholar]
- 16.Saunders TC. Consultation-referral among physicians: Practice and process. J Fam Pract. 1978;6:123–128. [PubMed] [Google Scholar]
- 17.Accreditation Council for Graduate Medical Education. Program requirements for residency education in internal medicine. Available at: http://www.acgme.org/acWebsite/downloads/RRC_progReq/140pr703_u704.pdf. Accessed September 11, 2009.
- 18.Ballard WP, Gold JP, Charlson ME. Compliance with the recommendations of medical consultants. J Gen Intern Med. 1986;1:220–224. doi: 10.1007/BF02596186. [DOI] [PubMed] [Google Scholar]
- 19.Were MC, Abernathy G, Hui SL, Kempf C, Weiner M. Using computerized provider order entry and clinical decision support to improve referring physicians' implementation of consultants' medical recommendations. J Am Med Inform Assoc. 2009;16:196–202. doi: 10.1197/jamia.M2932. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Below is the link to the electronic supplementary material.