Abstract
Purpose
Evaluation of a novel instrumentation device for adolescent idiopathic scoliosis.
Methods
A new osteosynthesis implant (Universal Clamp) primarily consisting of a sublaminar band and titanium clamp was prospectively studied in 32 patients (average age, 15 years) with a major thoracic curve.
Results
The Universal Clamp was used without anterior release to reduce and maintain correction of the thoracic curve, which improved from 55.1° preoperatively to 14.5° at 3 months without neurological complication or loss of kyphosis.
Conclusions
This implant distributes stress over a larger area of the laminar cortex than sublaminar wires, patently reducing the risk of laminar fracture for equivalent reduction forces, and permits progressive reduction at several apical levels simultaneously.
Keywords: Adolescent idiopathic scoliosis, Sublaminar, Deformity correction, Surgery
Introduction
There is currently a lack of consensus regarding the ideal surgical technique for treating scoliosis [1–4]. While many surgeons agree that, among posterior techniques, pedicle screw-based deformity reduction and fixation is the method of choice for lumbar scoliosis [5], the use of pedicle screws in the thoracic spine is less widespread despite reports of excellent deformity correction in the coronal plane [6–8]. Aside from risks associated with placing screws outside of the pedicle [9–12], there is growing concern over the low values of thoracic kyphosis often reported in patients with all-screw constructs [2, 7, 13, 14]. Other treatments consist of various types of hybrid constructs with pedicle-screw fixation in the lumbar spine and other anchors in the thoracic spine [3, 13, 15]. Among these thoracic anchors, sublaminar wiring has safety issues [16–19], hooks impinge upon the spinal canal [20] and lack a stable hold on the vertebra [21, 22], and intraspinous wires provide weaker fixation to the posterior arch than either laminar hooks [23] or sublaminar wires [24]. Various soft sublaminar bands have also been proposed as thoracic anchors. They obviate the neurovascular risks associated with screws or wires, provide immediate stability that is lacking with hooks, are anchored around the strongest portion of the neural arch, and apply less stress at any given point on the bony surface than wires, thus reducing the risk of cutout fractures during deformity reduction [25–29]. However, once these bands are tightened, fixation to the fusion rod depends on rudimentary knots, which do not prevent movement up or down the rod.
The drawbacks of sublaminar band techniques were addressed in a novel implant called the Universal Clamp (UC), which consists of a similar soft sublaminar band and metal jaws that secure it strongly to the fusion rod after tightening [30]. This obviated the thorny problem of how to tie the bands after pulling the vertebrae to the rod to correct scoliosis. Furthermore, the stable anchorage of the UC to the rod permitted the application of compression or distraction between vertebrae, as well as in situ bending. The principle of multiple-level progressive reduction avoiding any abrupt traction on the spinal cord was also attractive. To test the effectiveness and safety of this new implant, we performed the present prospective study using a combination of UCs in thoracic curves with conventional systems of pedicle screws at the distal end of the constructs and hook claws at the proximal end. Efficacy was measured in terms of postoperative angular corrections and safety was measured in terms of the percentage of patients without intraoperative or early postoperative complications.
Methods
Implant description
The Universal Clamp (Zimmer Spine, SAS, Bordeaux, France) is a novel implant used in place of pedicle screws, hooks, or sublaminar wiring in fusion constructs. The UC has only three components, a woven polyester band (Dacron), a titanium alloy (or stainless steel) clamp, and a locking screw (Ti alloy or stainless steel) (Fig. 1).
Fig. 1.

The Universal Clamp (Zimmer Spine, SAS, Bordeaux, France)
The UC technique resembles the Luque technique, with sublaminar polyester bands replacing sublaminar wiring. The surface area of contact between the polyester band and lamina is larger than that between wiring or cables, and the lamina permits the application of greater spinal deformity reduction forces with less risk of bone fracture. Deformity correction is applied in step-wise fashion at one or more spinal segments with a reduction tool that is activated in the same simple manner as a rongeur. The strength of the band–rod connection is equivalent to those of screw–rod or hook–rod connections, permitting classical translation, compression, distraction, and in situ bending maneuvers.
A malleable metallic insert in the leading tip of the polyester band facilitates sublaminar insertion (Fig. 2). Before sublaminar passage, that end of the band is slipped through slots on the hinge side of both metal jaws in a top-to-bottom direction. After sublaminar passage, the band leader is rethreaded (without introducing twists in the band) through the same slots in the jaws in the bottom-to-top direction next to the other end of the band, which has two metallic buckles at its extremity. The leader is then passed through both buckles in one direction and back through one buckle in the other direction to create an adjustable loop for the reduction tool on the top side of the jaws. Although the buckles maintain the loop strongly, preventing any slippage of the band when traction is applied to the loop, the loop can be easily shortened or lengthened as necessary to fit the reduction gun.
Fig. 2.

The malleable leader of the band can easily be shaped by hand to facilitate insertion under the lamina
Once all Universal Clamp implants are placed along the spine and the prebent double-rod frame has been anchored to pedicle screws at the distal end of the construct, the UCs are placed along the fusion rods. When the UC jaws close over the fusion rod, both band strands lie between the fusion rod and the inside of the jaws. After closing the upper jaw of the clamp over the rod, the surgeon inserts the locking screw but does not tighten it (Fig. 3), leaving the band loose enough to permit traction of the vertebrae toward the rod with the reduction tool (Fig. 4). The tip of the reduction tool is placed over the top side of the jaws and upon the rod on both sides of the jaws. The band loop is then placed onto a stump on the reduction tool. In this configuration, each squeeze on the trigger of the reduction tool pulls the lamina closer to the fusion rod, achieving deformity reduction. After reduction maneuvers and optimal band tension have been obtained, the UC (band and jaws) is firmly secured to the rod with the locking screw. The loop of band is removed from the reduction instrument and the excess band strands (including the malleable insert and the metal buckles) are cut and removed.
Fig. 3.

The locking screw is used to secure the jaws and band tightly to the fusion rod. It is initially only partly inserted to permit the band to be pulled by the reduction tool through the jaws and past the rod
Fig. 4.

The reduction tool of the UC system
Patients
Thirty-two patients with idiopathic thoracic scoliosis were included in this study. The patients were operated in two centers by two surgeons. All had Lenke type 1, 2, or 3 curves [31]. Patients with major lumbar curves were excluded. All patients who would have needed anterior release were also excluded, as were those with congenital or neuromuscular scoliosis. Every patient included in the series had preoperative magnetic resonance imaging (MRI) showing an absence of spinal cord disorders.
Operative technique
The spine was instrumented from the neutral vertebra of the curve cranially. When there was a structural lumbar curve, the distal extremity of the arthrodesis was the vertebra situated above the last disc that opened in both directions on lateral bending X-rays. In every patient, instrumentation consisted of a construct with three parts. The proximal portion consisted of self-retaining bilaminar hook claws on the two proximal vertebrae. Around the apex of the thoracic curve, sublaminar UCs were used in the concavity at 3–6 levels. One or two levels were also instrumented on the convex side. In some cases, instead of placing the band simply under the lamina, it was threaded under the lamina and around the transverse process, as shown in Fig. 8. At the distal end of the construct, pedicle screws were used from T11 to the last instrumented vertebra. Intraoperative fluoroscopic guidance was not used. Pedicle screws were placed using the free-hand technique. A frame was obtained with two precontoured 5.5 mm titanium rods united by two transverse traction devices. At the distal end of the construct, the frame was secured to the pedicle screws. The deformity reduction was then begun in the proximal-to-distal direction. When the frame was used to reduce the concavity of the thoracic curves, tension was applied to the UCs progressively and repetitively. Distraction was also regularly applied to the proximal claws while tightening the UCs. The intervention ended with the tightening of the UCs on the convex side. Arthrodesis was performed by resecting the spinous processes and freshening the articular processes of all of the segments being fused. Autologous bone graft was collected from the resected spinous processes, and graft volume was augmented with a synthetic bone substitute (Biosorb®, SBM, Lourdes). Somatosensory and motor evoked potentials were monitored in all patients during the operation.
Fig. 8.
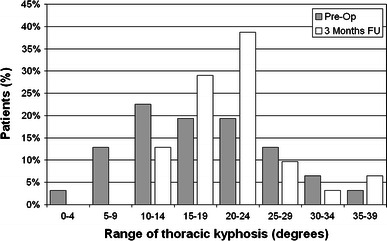
Distributions of preoperative and postoperative angles of thoracic kyphosis
Opiates were administered postoperatively for 5 days in most cases. The patient was returned to the upright position after removal of the intravenous analgesics, generally on the sixth day. No external orthosis was used postoperatively. Mean length of hospital stay was 8 days. Neither the time before return to the upright position nor the duration of hospitalization changed with respect to the thoracic anchors we previously used in similar patients.
Patient assessment
The preoperative radiographic work-up included whole-spine erect posterior–anterior (PA), whole-spine erect lateral, and supine bending radiographs. The postoperative X-rays included standing PA and lateral films. Angular measurements were made in terms of Cobb angle [32] by an independent observer. The following ratios were calculated:
-
Preoperative flexibility (PF)
PF (%) = [(preoperative erect Cobb angle − supine bending Cobb angle)/preoperative erect Cobb angle] × 100
-
Postoperative correction: (POC)
POC (%) = [(preoperative erect Cobb angle − postoperative erect Cobb angle)/preoperative erect Cobb angle] × 100
-
Cincinnati correction index (CCI)
CCI = POC/PF
Increase in kyphosis % = [(postoperative kyphosis − preoperative kyphosis)/preoperative kyphosis] × 100.
Paired-samples t-tests were used to analyze differences between preoperative curves and postoperative curves. All statistical tests were two-tailed, and a P value < 0.05 was considered to be significant.
Results
Thirty-two patients were included in this study. There were 28 girls and 4 boys. The average age at operation was 15 years 2 months (range, 12–22 years 1 month). The operation lasted an average of 213 ± 41 min. An average of 5.6 ± 1.6 Universal Clamps were used in each operation.
In the coronal plane, the average preoperative (Fig. 5) value of the major thoracic curve was 55.1 ± 6.6° (range, 42–70°). On the postoperative evaluation (Fig. 6), the average value had been corrected to 13.7 ± 8.6° (range, 8–32°), corresponding to an average correction of 75%. At 3 months, the Cobb angle had slightly decreased to 14.5 ± 6.2° (range, 8–35°), corresponding to an average postoperative correction (POC) of 73.3 ± 11.6%. This correction was highly significant (P < 0.0001).
Fig. 5.
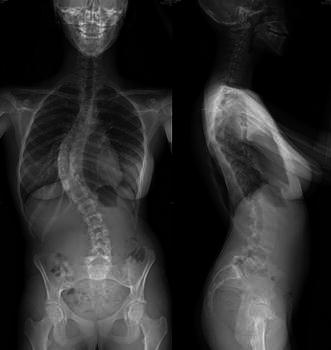
Preoperative PA and lateral X rays showing initial deformations in the coronal and sagittal planes
Fig. 6.
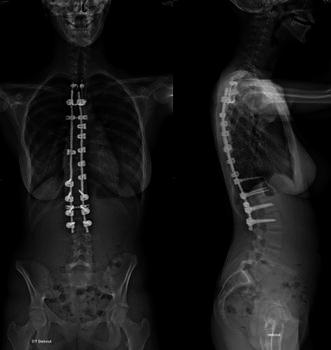
Three months postoperative PA and lateral X rays (same patient) showing the correction obtained in the coronal and sagittal planes
The distributions of the thoracic Cobb angles preoperatively and at the 3-month follow-up are shown on a histogram for clarity (Fig. 7).
Fig. 7.
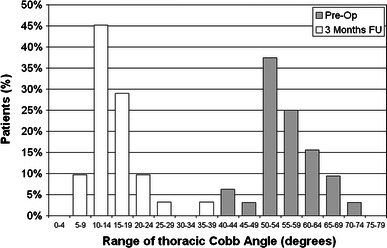
Distributions of thoracic Cobb angles preoperatively and 3 months postoperatively
The preoperative flexibility (PF) was 52.1 ± 12.3% and the average computed Cincinnati correction index (CCI) was 1.48 ± 0.40 at 3 months.
In the histogram presented in Fig. 7, all of the patients but one demonstrated a postoperative thoracic Cobb angle of lower than 30°. The patient demonstrating a postoperative thoracic Cobb angle of greater than 30° (35°) was also the patient with the lowest preoperative flexibility (20%). However, the corresponding CCI was satisfactory (1.50).
The average value of the preoperative lumbar curve was 34.8 ± 14.5° (range, 6–65°). On the postoperative evaluation, the mean lumbar curve was 8.5 ± 8.3° (range, 0–25°), and at 3 months follow-up this value was 9.6 ± 6.1° (range, 1–25°), corresponding to an average correction of 69.5%.
In the sagittal plane, the average preoperative thoracic kyphosis was 18.5 ± 8.2° (range, 4–40°). The average thoracic kyphosis at 3 months increased by 13% to 20.9 ± 6.5° (range, 12–40°). The distributions of both preoperative and postoperative kyphosis angles are also provided on a histogram (Fig. 8).
When considering the overall group of patients, this difference was not statistically significant (P = 0.14). However, when considering the patients (n = 12) with a thoracic kyphosis angle (TK) < 15°, i.e., patients who were either hypokyphotic (TK < 10°) or in the lowest range of normal kyphosis (10° < TK < 15°), the difference between the preoperative kyphosis angle (10.4 ± 3.6°) and the postoperative kyphosis angle (19.3 ± 3.3°) was highly significant (P < 0.0001). For these patients, the corresponding increase in thoracic kyphosis was 86%. For the twenty patients whose preoperative thoracic kyphosis was greater than 15°, the postoperative kyphosis angle was not statistically different from the preoperative value (23.6 vs. 21.9°, P = 0.48).
The average value of preoperative lumbar lordosis was −45.4 ± 11.9° (range, −30 to −70°). The average value of postoperative lordosis was −43.3 ± 10.1° (range, −30 to −66°). There was no difference between the two groups (P = 0.31).
The radiological results are summarized in Table 1.
Table 1.
Preoperative and postoperative measurements
| Preop | 3 m Postop | P | % Correction | |
|---|---|---|---|---|
| Thoracic curve | 55.1 ± 6.6° | 14.5 ± 6.2° | P < 0.0001 | 73.3 |
| Th curve flexibility | 52.1 ± 12.3% | |||
| Cincinnati index | 1.48 ± 0.40 | |||
| Thoracic kyphosis | 18.5 ± 8.2° | 20.9 ± 6.5° | NS (P = 0.14) | 13.0 |
| Lumbar curve | 34.8 ± 14.5° | 9.6 ± 6.1° | P < 0.0001 | 69.5 |
| Lumbar lordosis | 45.4 ± 11.9° | 43.3 ± 10.1° | NS (P = 0.31) | −4.6 |
Average ± SD
No intraoperative neurological complication was observed. There was no dural tear. There was no observed superficial or deep infection. Modification of the somatosensory and motor evoked potentials was not observed during sublaminar insertion and passage of the UC bands. One transverse process fracture occurred during tightening of the band. Clinically, no lasting postoperative neurological deficit was found. One patient had transient difficulty mobilizing the lower limbs in the immediate postoperative period (ASIA score of 0/5 in all lower limb muscle groups) without modifications of intraoperative evoked potentials, but this resolved spontaneously 3 h postoperatively without further complications. One patient, in whom the last instrumented level was L3, experienced right L5 nerve root pain. A computed tomographic scan showed no misplaced implant. The nerve root pain resolved after 2 months. Five patients experienced transient postoperative scapular pain.
Discussion
The surgical treatment of idiopathic scoliosis should combine an effective arthrodesis with the best correction possible in the coronal and sagittal planes. The overall surgical procedure should be performed with the lowest possible rate of complications. Segmental pedicle screw fixation has been shown to be superior to other techniques in lumbar scoliosis [5]. In contrast, the best thoracic curve correction technique in terms of efficacy/risk remains controversial.
Segmental pedicle screw constructs are widely held to provide better correction of thoracic Cobb angles in the coronal plane than other techniques [6–8]. Nevertheless, despite the possibility of good sagittal outcome with thoracic pedicle screws [33, 34], significantly lower values of thoracic kyphosis have been demonstrated in patients with all-screw constructs compared to hybrid instrumentation [2, 7, 13, 14]. In addition, neurovascular risks related to free-hand insertion of pedicle screws into the thoracic spine [9–12] are obviated using sublaminar fixation techniques, including the Universal Clamp. To reduce the risk of neurovascular complications related to the placement of screws outside of the pedicles, the use of imaging techniques such as fluoroscopy, preoperative computed tomography or neuronavigation has been recommended by several authors for insertion of pedicle screws [35–37]. These techniques that improve pedicle screw placement inevitably increase operating time and irradiation. Fluoroscopy is not needed for sublaminar anchorage, which can consequently reduce the radiation exposures of the patient, surgeon, and other operating room professionals. In the present series, the coronal correction of 73% obtained with the Universal Clamp hybrid instrumentation was similar to that achieved with all-screw constructs reported elsewhere. At the same time, a significant improvement in thoracic kyphosis was achieved among the patients who had low preoperative values of thoracic kyphosis, and no lasting neurovascular complication was observed. This would suggest that the Universal Clamp technique may be as good, if not better, than segmental pedicle screw instrumentation in terms of efficacy/risk, whether the loss of thoracic kyphosis in patients with all-screw constructs is considered a complication or an absence of efficacy.
The most cost-effective technique of fixation may be sublaminar wiring [13]. From the outset, the segmental instrumentation by means of sublaminar wiring described by Luque obtained a coronal curve correction of 72% [16]. However, we believe that many surgeons abandoned the use of sublaminar wires subsequent to early reports of neurological lesions that occurred during the primary operation [16, 18], postoperatively by wire breakage [17], or at removal during revision procedures [19]. The present device would appear to provide equivalent results without the same level of risk thanks to the soft sublaminar band that cannot be inadvertently thrust into the spinal canal. In a study of similar polyethylene terephthalate sublaminar bands in large baboons, macroscopic and histologic examination showed the soft bands to be substantially safer and to impinge less upon the canal than steel wiring [27]. Only longer-term results in a greater number of patients will show if the Universal Clamp truly is safer than sublaminar wiring. If this is indeed the case, then efficacy/risk would be in favor of this new system.
Segmental instrumentation including hooks, as proposed by Cotrel and Dubousset, achieved correction rates ranging from 50 to 70% [38–40]. Compared to the Universal Clamp, hooks have two disadvantages. For one thing, while sublaminar wires have been shown to impinge upon the canal more than soft sublaminar bands [27], the impingement of sublaminar wires is only negligible compared to that of even appropriately placed hooks [20]. The second disadvantage of hooks is the relative instability of their hold on the vertebrae, allowing them to dislodge intraoperatively during deformity-correcting maneuvers [22] or postoperatively [21]. Once the UC band has been passed around a lamina and back through the jaws, the UC cannot be inadvertently dislodged from the vertebra, an advantage that the UC shares with pedicle screws. This indicates that the UC has an equivalent efficacy/risk ratio, if not a more favorable one.
Wisconsin wiring is another correction and fixation technique applied through a posterior approach [1, 41, 42]. This system includes segmental fixation by wiring through button-like devices placed at the base of the spinous processes. Using this technique, Herrera-Soto et al. [15] reported a correction of 69% at 2 years follow-up even without associated anterior release. If care is taken not to violate the dome-shaped neural canal when placing intraspinous wires, they obviate the neurologic risks associated with sublaminar wiring [24]. Unfortunately, the resistance to failure by cutout of intraspinous wires is roughly half that of sublaminar wires or laminar hooks [23, 24]. Soft sublaminar bands distribute the stress over a larger area of bone than sublaminar wires or hooks, theoretically reducing the risk of failure at the device–bone interface [28]. In comparative biomechanical tests, both UCs and sublaminar wiring failed in most cases by pedicle base fracture, but sublaminar wiring cut through the lamina in one specimen, while no lamina fracture was observed with the UC [43]. The higher resistance to cutout of sublaminar wires compared to intraspinous wires suggests that UC fixation would have greater resistance to mechanical failure than intraspinous wire fixation, and consequently may be superior to intraspinous wiring in terms of efficacy/risk.
We chose to use a system of fixation that combined what we consider to be the most effective implants in the portions of the spine where we used them. We used pedicle screws systematically below T10. At the proximal extremity, fixation was obtained with bilaminar hooks. In the middle thoracic spine, we used Universal Clamps. Hybrid constructs have long been validated and are known to improve sagittal balance [1, 15]. Vora et al. [2] compared three series of AIS patients, one group with hook-and-intraspinous wire constructs, a second group with hybrid constructs consisting of proximal hooks, distal pedicle screws, and sublaminar wiring in the apical portion, and a third group with all-screw constructs. Our results were consistent with those reported for their sublaminar wiring group, particularly regarding the maintenance of thoracic kyphosis. In the present series, as in the hybrid constructs of Vora et al. and Herrera Soto et al. [2, 15], sagittal balance appeared to be more satisfactorily preserved than by all-screw constructs.
The polyester structure appeared to us to make the sublaminar passage safer. We believe that the progressive reduction by alternating segmental translation is the most essential advantage in terms of protecting the spinal cord. All of our patients had a precontoured frame made of two rods united by two transverse traction devices. This frame was secured to the distal lumbar pedicle screws. It was then connected to proximal bilaminar hook claws, preserving the possibility of gentle progressive distraction. Subsequently, the reduction by the UCs was begun in a distal-to-proximal direction, then repeated twice. During this reduction, mild proximal distraction was pursued to maintain tension in the system. During the application of tension, several polyester bands were severed by the reduction tool. In each of these rare events, tension was easily reapplied to the same implant, which did not have to be replaced. Although one transverse process fracture occurred, there was no case of lamina fracture.
Conclusion
In our experience, the Universal Clamp is primarily useful for three reasons: (1) it is straightforward, with a short learning curve and a less aggressive structure than that of Luque sublaminar wiring; (2) it permits progressive multiple-level reduction of the apex of thoracic curves while preserving satisfactory sagittal balance; and (3) the action of the UCs during reduction was accessible to direct visual control, in contrast to thoracic pedicle screws (the possible intraoperative complications of which are not readily visible). This study was consistent with the intraoperative safety of the system. Longer follow-up will show if correction is maintained and the quality of bone fusion in order to confirm the short-term efficacy demonstrated in this preliminary study.
Acknowledgments
Funding for this study was provided by Zimmer Spine, S.A. (Bordeaux, France).
Conflict of interest statement
None.
Footnotes
J.-L. Jouve and J. S. de Gauzy are consultants for Zimmer Spine, S.A. (Bordeaux, France).
Contributor Information
Jean-Luc Jouve, Email: jean-luc.jouve@ap-hm.fr.
Benjamin Blondel, Email: benjblondel@yahoo.fr.
References
- 1.Bridwell KH, Hanson DS, Rhee JM, Lenke LG, Baldus C, Blanke K. Correction of thoracic adolescent idiopathic scoliosis with segmental hooks, rods, and Wisconsin wires posteriorly: it’s bad and obsolete, correct? Spine. 2002;27:2059–2066. doi: 10.1097/00007632-200209150-00018. [DOI] [PubMed] [Google Scholar]
- 2.Vora V, Crawford A, Babekhir N, Boachie-Adjei O, Lenke L, Peskin M, et al. A pedicle screw construct gives an enhanced posterior correction of adolescent idiopathic scoliosis when compared with other constructs: myth or reality. Spine. 2007;32:1869–1874. doi: 10.1097/BRS.0b013e318108b912. [DOI] [PubMed] [Google Scholar]
- 3.Winter RB, Lonstein JE, Denis F. How much correction is enough? Spine. 2007;32:2641–2643. doi: 10.1097/BRS.0b013e31815a5207. [DOI] [PubMed] [Google Scholar]
- 4.Lenke LG, Kuklo TR, Ondra S, Polly DW., Jr Rationale behind the current state-of-the-art treatment of scoliosis (in the pedicle screw era) Spine. 2008;33:1051–1054. doi: 10.1097/BRS.0b013e31816f2865. [DOI] [PubMed] [Google Scholar]
- 5.Hamill CL, Lenke LG, Bridwell KH, Chapman MP, Blanke K, Baldus C. The use of pedicle screw fixation to improve correction in the lumbar spine of patients with idiopathic scoliosis. Is it warranted? Spine. 1996;21:1241–1249. doi: 10.1097/00007632-199605150-00020. [DOI] [PubMed] [Google Scholar]
- 6.Kim YJ, Lenke LG, Cho SK, Bridwell KH, Sides B, Blanke K. Comparative analysis of pedicle screw versus hook instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine. 2004;29:2040–2048. doi: 10.1097/01.brs.0000138268.12324.1a. [DOI] [PubMed] [Google Scholar]
- 7.Kim YJ, Lenke LG, Kim J, Bridwell KH, Cho SK, Cheh G, et al. Comparative analysis of pedicle screw versus hybrid instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine. 2006;31:291–298. doi: 10.1097/01.brs.0000197865.20803.d4. [DOI] [PubMed] [Google Scholar]
- 8.Suk SI, Lee CK, Kim WJ, Chung YJ, Park YB. Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine. 1995;20:1399–1405. [PubMed] [Google Scholar]
- 9.Bergeson RK, Schwend RM, DeLucia T, Silva SR, Smith JE, Avilucea FR. How accurately do novice surgeons place thoracic pedicle screws with the free hand technique? Spine (Phila Pa 1976) 2008;33:E501–507. doi: 10.1097/BRS.0b013e31817b61af. [DOI] [PubMed] [Google Scholar]
- 10.Di Silvestre M, Parisini P, Lolli F, Bakaloudis G. Complications of thoracic pedicle screws in scoliosis treatment. Spine. 2007;32:1655–1661. doi: 10.1097/BRS.0b013e318074d604. [DOI] [PubMed] [Google Scholar]
- 11.Modi HN, Suh SW, Fernandez H, Yang JH, Song HR. Accuracy and safety of pedicle screw placement in neuromuscular scoliosis with free-hand technique. Eur Spine J. 2008;17:1686–1696. doi: 10.1007/s00586-008-0795-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Senaran H, Shah SA, Gabos PG, Littleton AG, Neiss G, Guille JT. Difficult thoracic pedicle screw placement in adolescent idiopathic scoliosis. J Spinal Disord Tech. 2008;21:187–191. doi: 10.1097/BSD.0b013e318073cc1d. [DOI] [PubMed] [Google Scholar]
- 13.Cheng I, Kim Y, Gupta MC, Bridwell KH, Hurford RK, Lee SS, et al. Apical sublaminar wires versus pedicle screws—which provides better results for surgical correction of adolescent idiopathic scoliosis? Spine. 2005;30:2104–2112. doi: 10.1097/01.brs.0000179261.70845.b7. [DOI] [PubMed] [Google Scholar]
- 14.Lowenstein JE, Matsumoto H, Vitale MG, Weidenbaum M, Gomez JA, Lee FY, et al. Coronal and sagittal plane correction in adolescent idiopathic scoliosis: a comparison between all pedicle screw versus hybrid thoracic hook lumbar screw constructs. Spine. 2007;32:448–452. doi: 10.1097/01.brs.0000255030.78293.fd. [DOI] [PubMed] [Google Scholar]
- 15.Herrera-Soto JA, Lewis R, Nosir HR, Crawford AH. The use of multiple anchors for the treatment of idiopathic scoliosis. Spine. 2007;32:E517–522. doi: 10.1097/BRS.0b013e318133fd1d. [DOI] [PubMed] [Google Scholar]
- 16.Luque ER (1982) Segmental spinal instrumentation for correction of scoliosis. Clin Orthop Relat Res 163:192–198 [PubMed]
- 17.Bernard TN, Jr, Johnston CE, 2nd, Roberts JM, Burke SW. Late complications due to wire breakage in segmental spinal instrumentation. Report of two cases. J Bone Joint Surg Am. 1983;65:1339–1345. [PubMed] [Google Scholar]
- 18.Wilber RG, Thompson GH, Shaffer JW, Brown RH, Nash CL., Jr Postoperative neurological deficits in segmental spinal instrumentation. A study using spinal cord monitoring. J Bone Joint Surg Am. 1984;66:1178–1187. [PubMed] [Google Scholar]
- 19.Nicastro JF, Hartjen CA, Traina J, Lancaster JM. Intraspinal pathways taken by sublaminar wires during removal. An experimental study. J Bone Joint Surg Am. 1986;68:1206–1209. [PubMed] [Google Scholar]
- 20.Polly DW, Jr, Potter BK, Kuklo T, Young S, Johnson C, Klemme WR. Volumetric spinal canal intrusion: a comparison between thoracic pedicle screws and thoracic hooks. Spine. 2004;29:63–69. doi: 10.1097/01.BRS.0000105525.06564.56. [DOI] [PubMed] [Google Scholar]
- 21.Schlenzka D, Poussa M, Muschik M (1993) Operative treatment of adolescent idiopathic thoracic scoliosis. Harrington-DTT versus Cotrel–Dubousset instrumentation. Clin Orthop Relat Res 297:155–160 [PubMed]
- 22.van Laar W, Meester RJ, Smit TH, van Royen BJ. A biomechanical analysis of the self-retaining pedicle hook device in posterior spinal fixation. Eur Spine J. 2007;16:1209–1214. doi: 10.1007/s00586-006-0288-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Coe JD, Warden KE, Herzig MA, McAfee PC. Influence of bone mineral density on the fixation of thoracolumbar implants. A comparative study of transpedicular screws, laminar hooks, and spinous process wires. Spine (Phila Pa 1976) 1990;15:902–907. doi: 10.1097/00007632-199009000-00012. [DOI] [PubMed] [Google Scholar]
- 24.Heller KD, Prescher A, Schneider T, Block FR, Forst R. Stability of different wiring techniques in segmental spinal instrumentation. An experimental study. Arch Orthop Trauma Surg. 1998;117:96–99. doi: 10.1007/BF00703452. [DOI] [PubMed] [Google Scholar]
- 25.Gaines RW, Jr, Abernathie DL. Mersilene tapes as a substitute for wire in segmental spinal instrumentation for children. Spine (Phila Pa 1976) 1986;11:907–913. doi: 10.1097/00007632-198611000-00011. [DOI] [PubMed] [Google Scholar]
- 26.O’Brien JP, Stephens MM, Prickett CF, Wilcox A, Evans JH (1986) Nylon sublaminar straps in segmental instrumentation for spinal disorders. Clin Orthop Relat Res 203:168–171 [PubMed]
- 27.Grobler LJ, Gaines RW, Kempff PG (1997) Comparing Mersilene tape and stainless steel wire as sublaminar spinal fixation in the Chagma baboon (Papio ursinus). Iowa Orthop J 17:20–31 [PMC free article] [PubMed]
- 28.Fujita M, Diab M, Xu Z, Puttlitz CM. A biomechanical analysis of sublaminar and subtransverse process fixation using metal wires and polyethylene cables. Spine (Phila Pa 1976) 2006;31:2202–2208. doi: 10.1097/01.brs.0000232831.63589.22. [DOI] [PubMed] [Google Scholar]
- 29.Takahata M, Ito M, Abumi K, Kotani Y, Sudo H, Ohshima S, et al. Comparison of novel ultra-high molecular weight polyethylene tape versus conventional metal wire for sublaminar segmental fixation in the treatment of adolescent idiopathic scoliosis. J Spinal Disord Tech. 2007;20:449–455. doi: 10.1097/BSD.0b013e318030d30e. [DOI] [PubMed] [Google Scholar]
- 30.Mazda K, Ilharreborde B, Even J, Lefevre Y, Fitoussi F, Pennecot GF. Efficacy and safety of posteromedial translation for correction of thoracic curves in adolescent idiopathic scoliosis using a new connection to the spine: the Universal Clamp. Eur Spine J. 2009;18:158–169. doi: 10.1007/s00586-008-0839-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lenke LG, Betz RR, Harms J, Bridwell KH, Clements DH, Lowe TG, et al. Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am. 2001;83-A:1169–1181. [PubMed] [Google Scholar]
- 32.Cobb JR (1948) In: Edwards JW (ed) Instructional course lectures. The American Academy of Orthopaedic Surgeons, Ann Arbor, pp 261–275
- 33.Clement JL, Chau E, Kimkpe C, Vallade MJ. Restoration of thoracic kyphosis by posterior instrumentation in adolescent idiopathic scoliosis: comparative radiographic analysis of two methods of reduction. Spine (Phila Pa 1976) 2008;33:1579–1587. doi: 10.1097/BRS.0b013e31817886be. [DOI] [PubMed] [Google Scholar]
- 34.Suk SI, Kim WJ, Kim JH, Lee SM. Restoration of thoracic kyphosis in the hypokyphotic spine: a comparison between multiple-hook and segmental pedicle screw fixation in adolescent idiopathic scoliosis. J Spinal Disord. 1999;12:489–495. [PubMed] [Google Scholar]
- 35.Carbone JJ, Tortolani PJ, Quartararo LG. Fluoroscopically assisted pedicle screw fixation for thoracic and thoracolumbar injuries: technique and short-term complications. Spine. 2003;28:91–97. doi: 10.1097/00007632-200301010-00021. [DOI] [PubMed] [Google Scholar]
- 36.Farber GL, Place HM, Mazur RA, Jones DE, Damiano TR. Accuracy of pedicle screw placement in lumbar fusions by plain radiographs and computed tomography. Spine. 1995;20:1494–1499. doi: 10.1097/00007632-199507000-00010. [DOI] [PubMed] [Google Scholar]
- 37.Kim YJ, Lenke LG, Bridwell KH, Cho YS, Riew KD. Free hand pedicle screw placement in the thoracic spine: is it safe? Spine. 2004;29:333–342. doi: 10.1097/01.BRS.0000109983.12113.9B. [DOI] [PubMed] [Google Scholar]
- 38.Burton DC, Asher MA, Lai SM. The selection of fusion levels using torsional correction techniques in the surgical treatment of idiopathic scoliosis. Spine. 1999;24:1728–1739. doi: 10.1097/00007632-199908150-00015. [DOI] [PubMed] [Google Scholar]
- 39.Fitch RD, Turi M, Bowman BE, Hardaker WT (1990) Comparison of Cotrel–Dubousset and Harrington rod instrumentations in idiopathic scoliosis. J Pediatr Orthop 10:44–47 [PubMed]
- 40.Lenke LG, Bridwell KH, Baldus C, Blanke K, Schoenecker PL (1992) Cotrel–Dubousset instrumentation for adolescent idiopathic scoliosis. J Bone Joint Surg Am 74:1056–1067 [PubMed]
- 41.Drummond D, Guadagni J, Keene JS, Breed A, Narechania R. Interspinous process segmental spinal instrumentation. J Pediatr Orthop. 1984;4:397–404. doi: 10.1097/01241398-198408000-00001. [DOI] [PubMed] [Google Scholar]
- 42.Neuwirth MG, Drummond DS, Casden AS. Results of interspinous segmental instrumentation in the sagittal plane. J Spinal Disord. 1993;6:1–4. [PubMed] [Google Scholar]
- 43.Hongo M, Ilharreborde B, Gay RE, Zhao C, Zhao KD, Berglund LJ, et al. Biomechanical evaluation of a new fixation device for the thoracic spine. Eur Spine J. 2009;18:1213–1219. doi: 10.1007/s00586-009-0999-4. [DOI] [PMC free article] [PubMed] [Google Scholar]


