Abstract
Background
In haemophiliacs, synovectomy is indicated for recurrent joint bleedings, despite medical treatment.
Method
We report a series of 23 surgical synovectomies of the knee with a median follow-up of 8.8 years. The median age of patients at surgery was 13.5 years. Clinical and radiological evaluations were made according to the Petrini and the Pettersson scores, at 1 and 5 years after surgery, and at the last follow-up. Wilcoxon and Spearman’s tests were used for the statistical analysis.
Result
The Petrini score improved at 1 and 5 years (P < 0.001). Nine patients have 20 years of follow-up and a stable result. In more than half of the knees, no episode of recurrent bleeding occurred. The effect of surgery on the range of motion (ROM) was moderate and mobilisation under anaesthesia did not improve it significantly. There was a progressive worsening of the radiological score, but no correlation between clinical and radiological score was noticed (ρ = 0.08, P = 0.77).
Conclusion
Complete synovectomy gives good long-term results in term of bleeding recurrence and overall function.
Keywords: Haemophilia, Knee, Open synovectomy, Long-term results
Introduction
Haemophilia is a cross-linked recessive disease characterised by a factor VIII or IX deficiency. Patients severely affected (<1% of the normal factor level) are prone to frequent spontaneous bleeding episodes, particularly in joints (92%), and most of these (80%) occur in the knee, ankle and elbow [1]. Recurrent joint bleeding episodes lead to haemophilic arthropathy with synovial hypertrophy and progressive joint destruction. Synovectomy is indicated within the frame of management of haemophilic arthropathy, to delay total knee arthroplasty, which the rate of early and late complications has to be considered [2–9]. Long-term results of synovectomy have never been reported. Before less invasive techniques such as arthroscopic, medical or isotopic synovectomies [10–14] have been proposed, open synovectomy was the reference procedure. The goal of this study is to report the long-term results of a monocentric series of open surgical synovectomy of the knee.
Patients and methods
The minimum follow-up to be included in the study was 5 years. Thirty-two patients underwent 35 knee synovectomies from 1977 to 2002. Surgery was decided on a painful chronic effusion in a ‘target joint’ or on severe synovial hypertrophy or on recurrent haemarthrosis, despite 6 months of prophylactic treatment. Twelve synovectomies (34%) were not available for revision: five patients died of human immunodeficiency virus (HIV), four were foreign patients and two were lost to follow-up. Concerning their age and the severity of their disease, these patients were similar to the those included in the series. The remaining 23 synovectomies (21 patients) were included in this study. The median follow-up of this patient series was 8.8 years (range, 5.3–22.7). Clinical evaluation was made pre-operatively and at each multidisciplinary follow-up visit using parameters from the World Federation of Haemophilia adapted by Petrini [15]. This score considers objective and subjective symptoms, and also takes into consideration whether the joint is a target one or if there is a chronic synovitis. Radiological evaluation was made using the Pettersson classification [16], which takes into consideration degenerative arthritis development.
All patients had a severe haemophilia (of whom 20 with an FVIII deficiency). One patient with haemophilia A had a low level of inhibitor just before surgery, allowing an FVIII treatment for the first 4 days. Except for the patient with an inhibitor for which the FVIII treatment was switched to activated prothrombin, all patients received an FVIII/FIX replacement 30 min before surgery, to obtain a factor level at 100%. The factor level remained between 80 and 100% during the first 8 days following surgery, and between 30 and 50% for the next 2 weeks. After the acute post-operative period, the former treatment was administrated.
Open synovectomy under general anaesthesia [12, 17] was performed systematically under tourniquet ischaemia. Two approaches were necessary to perform a complete synovectomy. The long medial parapatellar incision allowed to clean the supra patellar pouch, the medial submeniscal fold and, of the intercondylar notch, around the cruciate ligaments. Through the same approach, the medial retrocondylar fold was cleaned. A posterolateral approach was needed to complete the synovectomy in the supra patellar pouch, the lateral submeniscal fold and the lateral retrocondylar fold. Surgical wound was closed with two suction drains. At the end of the procedure, two sets of plaster splints were made, one in maximal knee extension and one in maximal knee flexion. Patients were postured alternatively every 4 h after surgery. Passive range of knee motion was carried out with physiotherapy, or a continuous passive motion (CPM) machine when available, between the splint immobilisation during the day, 1 h three times a day. Early active physiotherapy was also initiated after surgery: isometric quadriceps and hamstring strengthening exercises were performed. A manipulation under general anaesthesia was indicated in case of no recovery of the pre-operative mobilities around the 15th day after surgery (flexion less than 90°).
Quantitative variables are presented as median (range). Comparisons of clinical and radiological scores between surgery and 5 years post-operatively were made using the non-parametric paired Wilcoxon test. Correlations between continuous variables were performed with Spearman’s rank test.
Results
The median age at surgery was 13.5 years (7.4–23.7). Indications for synovectomy were chronic joint effusion in 20 cases (87%), synovial hypertrophy in two cases (9%) and recurrent bleeding in one case (4%). Fourteen patients were infected with HIV, without related symptoms. The median length of hospital stay in our series was 32 days (12–60). Eleven knees (47%) had manipulation under general anaesthesia for an incomplete recovery of the pre-operative motilities. Manipulation under general anaesthesia increased the duration of stay at the hospital by 60% (from 22 days to 36 days). The length of stay at the hospital tended to decrease for the more recent patients, as the post-operative physiotherapy could be done in rehabilitation units (no significant difference).
No statistical correlation was observed neither between clinical score at 5 years and the age at procedure (ρ = 0.35, P = 0.12), nor between long-term outcome and the age at initial surgery (given that the younger patients had better scores before the surgery occurred) (P = 0.74).
The pre-operative median Petrini score was 13 (8–22). The youngest patients had the best clinical status (ρ = 0.66, P < 0.001). At 5 years follow-up, we observed a significant improvement of clinical scores (below 4, except for one patient with a score of 8) (P < 0.001). Among the 18 knees with a follow-up of more than 7 years, the score remained under 10, except for one patient who underwent a total knee arthroplasty. For patients with 20 years of follow-up (n = 9), the results were stable in a large majority of patients, but the small number of patients did not lead to any statistical interpretation (Figs. 1 and 2).
Fig. 1.
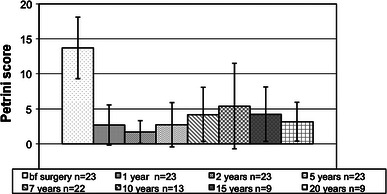
Evolution of the Petrini score at 1, 2, 5, 7, 10, 15 and 20 years post-operatively (median and standard deviation)
Fig. 2.
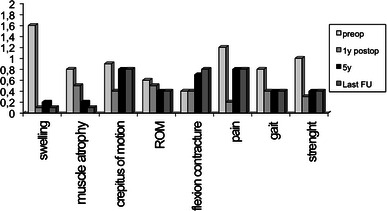
Evolution of the median value of clinical parameters at 1 and 5 years and final follow-up
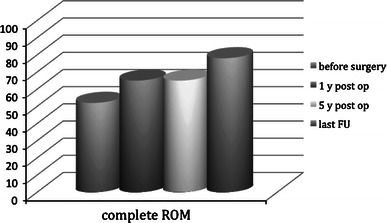
Concerning pain, improvement was observed during the first year: the rate of painful knees was reduced from 65% before surgery to 17% at 1 year. At 5 years follow-up, eight knees (34%) were still painful: three slightly, three moderately and two severely, with a limitation of normal activities for age. At the last follow-up, 14 knees (63%) were pain-free, three knees (13%) were slightly painful and six knees (27%) were moderately or severely painful (Fig. 3).
Fig. 3.

Evolution of the rate of painless patients (%)
Ten knees (43%) had minor bleeding episodes in the years following surgery, but only two (8.6%) had a major haemorrhage in the operated knee. Thirteen knees (57%) had no episode of recurrent bleeding.
Surgery had a moderate effect on global range of motion (ROM) (Fig. 4). At the last follow-up, only two knees had worsened their ROM. There was no statistical difference between patients who underwent a manipulation under general anaesthesia and the others (P = 0.47). Flexion contracture was not modified after surgery. In nine patients, a flexion contracture of around 5° appeared between the 5th year and the last follow-up, but the overall ROM was stable (from 74% of knees free of flexion contracture to 35%).
Fig. 4.
Evolution of the rate of patients with a complete range of motion (ROM) (%)
Gait pattern improved in 13 knees (57%) at 5 years follow-up. This included walking, running, skipping and galloping normal patterns. No patient complained of worsening of gait abnormalities.
Nineteen knees had adequate radiographs for this study. The median Pettersson pre-operative score was 1 (0–7). There was no correlation between clinical and radiological scores at the time of surgery (ρ = 0.08, P = 0.77). The median radiological score at 5 years was 4 (1–11). There was no correlation between the radiological score at the time of surgery and this score at the 5th year post-operatively (ρ = 0.25, P = 0.42). The worsening of the score was highly variable, depending on the patients (Figs. 5 and 6). We did not find any predictable condition influencing the radiological outcome of the joint.
Fig. 5.
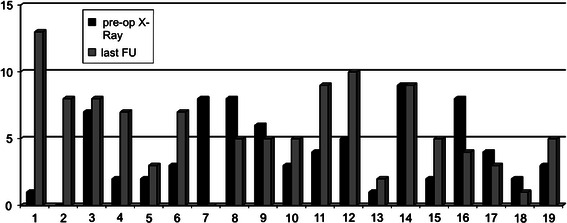
Pettersson’s score in individual patients (n = 19)
Fig. 6.

X-ray at the last follow-up of patient 11
Discussion
Haemorrhage is a concern in the post-operative period after open procedures in haemophiliacs [12, 13, 18–21]. As it might increase the rate of post-operative period bleeding, many authors avoid physiotherapy in the first post-operative days [11, 13, 19] and suggest waiting until the end of the first week to begin rehabilitation. With an appropriate factor substitution and a complete synovectomy, including a posterolateral approach to remove the posterior synovial, we did not encounter any haemorrhage requiring surgical evacuation.
We did not find any significant benefit of manipulation under general anaesthesia as far as long-term ROM recovery is concerned. Therefore, we no longer recommend manipulation under general anaesthesia. Unlike many authors [11, 13, 14, 19, 21], we did not observe a severe loss of ROM as far as long-term results are concerned. There is between 50 to almost 100% of worsening knees in the literature [11, 13, 14, 19, 21]. In our series, at the last follow-up, only two patients had worsened their ROM.
As previously reported [11–13], synovectomy improves pain in the first few years following surgery. Our series is the first to report on long-term results (more than 10 years) of open synovectomy. It is interesting to notice that, among the nine patients followed for between 10 and over 20 years, and despite a severe arthropathy, the clinical results remain stable, with only one patient requiring a knee replacement.
The recurrence of haemarthrosis is between 20 and 100% in the literature [11–13, 19, 21]. In our series, nearly 60% of the joints were dried by the procedure. In the other patients, bleeding episodes were less serious, less painful and required fewer factors that concentrated on replacement than before surgery. To our mind, the low rate of recurrence of the bleeding in our series is related to the extensive synovectomy, including the posterior part of the joint, through the posterolateral approach.
As with many authors, we agree that synovectomy does not stop the radiographic deterioration of the joint [12, 13, 21], but only delays its onset. In spite of synovectomy, the natural course of haemophilic knees is towards chronic arthropathy. However, the degenerative changes are not systematically related to clinical deterioration and most of the patients have a good clinical outcome.
Conclusion
Surgical synovectomy seems to be outdated and of low interest with the emergence of less invasive techniques. With early joint mobilisation and appropriate substitution, we did not encounter severe loss of range of motion (ROM) and post-operative haemorrhage, despite an invasive procedure. The complete removal of the pathological synovial tissue maximises the effects of the medical treatment and delays the onset of symptomatic arthritis. We believe that the long-term results of this technique are of interest, to compare them to those of less invasive procedures.
References
- 1.Pergantou H, Matsinos G, Papadopoulos A, Platokouki H, Aronis S. Comparative study of validity of clinical, X-ray and magnetic resonance imaging scores in evaluation and management of haemophilic arthropathy in children. Haemophilia. 2006;12:241–247. doi: 10.1111/j.1365-2516.2006.01208.x. [DOI] [PubMed] [Google Scholar]
- 2.Thomason HC, 3rd, Wilson FC, Lachiewicz PF, Kelley SS. Knee arthroplasty in hemophilic arthropathy. Clin Orthop Relat Res. 1999;360:169–173. doi: 10.1097/00003086-199903000-00020. [DOI] [PubMed] [Google Scholar]
- 3.Rodriguez-Merchan EC, Wiedel JD. General principles and indications of synoviorthesis (medical synovectomy) in haemophilia. Haemophilia. 2001;7(Suppl 2):6–10. doi: 10.1046/j.1365-2516.2001.00102.x. [DOI] [PubMed] [Google Scholar]
- 4.Figgie MP, Goldberg VM, Figgie HE, 3rd, Heiple KG, Sobel M. Total knee arthroplasty for the treatment of chronic hemophilic arthropathy. Clin Orthop Relat Res. 1989;248:98–107. [PubMed] [Google Scholar]
- 5.Vastel L, Courpied JP, Sultan Y, Kerboull M. Arthroplastie totale du genou chez l’hémophile. Rev Chir Orthop Reparatrice Appar Mot. 1999;85(5):458–465. [PubMed] [Google Scholar]
- 6.Bae DK, Yoon KH, Kim HS, Song SJ. Total knee arthroplasty in hemophilic arthropathy of the knee. J Arthroplasty. 2005;20(5):664–668. doi: 10.1016/j.arth.2005.01.008. [DOI] [PubMed] [Google Scholar]
- 7.Silva M, Luck JV., Jr Long-term results of primary total knee replacement in patients with hemophilia. J Bone Joint Surg Am. 2005;87(1):85–91. doi: 10.2106/JBJS.C.01609. [DOI] [PubMed] [Google Scholar]
- 8.Sheth DS, Oldfield D, Ambrose C, Clyburn T. Total knee arthroplasty in hemophilic arthropathy. J Arthroplasty. 2004;19(1):56–60. doi: 10.1016/j.arth.2003.08.008. [DOI] [PubMed] [Google Scholar]
- 9.Solimeno LP, Mancuso ME, Pasta G, Santagostino E, Perfetto S, Mannucci PM. Factors influencing the long-term outcome of primary total knee replacement in haemophiliacs: a review of 116 procedures at a single institution. Br J Haematol. 2009;145:227–234. doi: 10.1111/j.1365-2141.2009.07613.x. [DOI] [PubMed] [Google Scholar]
- 10.Storti E, Traldi A, Tosatti E, Davoli PG. Synovectomy, a new approach to haemophilic arthropathy. Acta Haematol. 1969;41:193–205. doi: 10.1159/000208851. [DOI] [PubMed] [Google Scholar]
- 11.Triantafyllou SJ, Hanks GA, Handal JA, 3rd Greer RB. Open and arthroscopic synovectomy in hemophilic arthropathy of the knee. Clin Orthop Relat Res. 1992;283:196–204. [PubMed] [Google Scholar]
- 12.Montane I, McCollough NC, 3rd, Lian EC. Synovectomy of the knee for hemophilic arthropathy. J Bone Joint Surg Am. 1986;68(2):210–216. [PubMed] [Google Scholar]
- 13.Wiedel JD. Arthroscopic synovectomy of the knee in hemophilia: 10-to-15 year followup. Clin Orthop Relat Res. 1996;328:46–53. doi: 10.1097/00003086-199607000-00010. [DOI] [PubMed] [Google Scholar]
- 14.Van den Berg HM, Dunn A, Fischer K, Blanchette VS. Prevention and treatment of musculoskeletal disease in the haemophilia population: role of prophylaxis and synovectomy. Haemophilia. 2006;12(Suppl 3):159–168. doi: 10.1111/j.1365-2516.2006.01281.x. [DOI] [PubMed] [Google Scholar]
- 15.Hill FGH, Ljung R. Third and fourth Workshops of the European Paediatric Network for Haemophilia Management. Haemophilia. 2003;9:223–228. doi: 10.1046/j.1365-2516.2003.00746.x. [DOI] [PubMed] [Google Scholar]
- 16.Pettersson H, Ahlberg A, Nilsson IM. A radiologic classification of hemophilic arthropathy. Clin Orthop Relat Res. 1980;149:153–159. [PubMed] [Google Scholar]
- 17.Herring JA. Chapter 36. Hematologic disorders. In: Herring JA, editor. Tachdjian’s pediatric orthopaedics. 4. Philadelphia, PA: Saunders Elsevier; 2007. [Google Scholar]
- 18.Arnold WD, Hilgartner MW. Hemophilic arthropathy. Current concepts of pathogenesis and management. J Bone Joint Surg Am. 1977;59(3):287–305. [PubMed] [Google Scholar]
- 19.Le Balch T, Girard F, Chaix O, Françoy P, Jouanin T, Mazas F. La synovectomie arthroscopique du genou chez l’hémophile. Rev Chir Orthop Reparatrice Appar Mot. 1987;73(Suppl II):122–125. [PubMed] [Google Scholar]
- 20.Tamurian RM, Spencer EE, Wojtys EM. The role of arthroscopic synovectomy in the management of hemarthrosis in hemophilia patients: financial perspectives. Arthroscopy. 2002;18(7):789–794. doi: 10.1053/jars.2002.32621. [DOI] [PubMed] [Google Scholar]
- 21.Dunn AL, Busch MT, Wyly JB, Sullivan KM, Abshire TC. Arthroscopic synovectomy for hemophilic joint disease in a pediatric population. J Pediatr Orthop. 2004;24(4):414–426. doi: 10.1097/01241398-200407000-00013. [DOI] [PubMed] [Google Scholar]


