Abstract
Introduction
Osteochondritis dissecans (OCD) of the femoral condyle is a rare lesion.
Materials and methods
A retrospective study (level IV evidence) analyzing a series of 40 pediatric cases with juvenile femoral condyles osteochondritis treated by arthroscopic multiple transchondral drilling between February 1999 and June 2008 was undertaken. This lesion affected the medial condyle in 87.5% of cases. The average age at treatment was 13.4 years. Our study took into account the location of the lesion and its radiological evolutionary stage. The average follow up was 14.8 months. The postoperative evaluation was based on the clinical and radiological scores of Hughston.
Results
Good clinical and radiological results in 97.5 and 95% of cases, respectively were obtained, with a significant correlation (P < 0.001) between clinical scores and radiological Hughston scores. The closed nature of the growth plate during surgery has a significant deleterious effect (P < 0.001) on the clinical and radiological score of Hughston.
Conclusion
All patients presenting juvenile condylar osteochondritis with open growth plate during treatment had good clinical and radiological results, confirming the validity and effectiveness of multiple transchondral drilling in this type of lesion.
Keywords: Juvenile osteochondritis dissecans, Femoral condyles, Arthroscopic transchondral drilling
Introduction
Osteochondritis dissecans (OCD), a term introduced by König in 1887 [1], is a rare lesion that affects the articular cartilage and the epiphyseal bone and may result in lack of consolidation to the separation of osteochondral fragment [2–6].
Most cases of OCD (75%) are present at the knees and three-quarters of those occur in the medial femoral condyle [7].
The pathophysiology of this disease is still mysterious and several etiological hypotheses have been discussed [8–10]: repetitive microtrauma, ischemia, lack of ossification, genetic cause, etc.
Treatment is variable and depends on both the lesion itself (stable or unstable) and the patient (closure or non-closure of the growth plate) [2, 7, 8].
The objective of this study is to evaluate the results in the medium and long term of femoral condyles OCD in children and adolescents carried out by arthroscopic multiple transchondral drilling.
Materials and methods
Between February 1999 and June 2008, 39 patients with juvenile osteochondritis of femoral condyles (accounting for 40 cases) were treated by arthroscopic transchondral drilling. Among the patients, 28 (71.8%) were male. The medial condyle was affected in 87.5% of cases, with involvement of the right knee in 14 cases, the left knee in 22 cases, and two cases of bilateral OCD. One patient had a unilateral bicondylar OCD. Among the five cases of OCD of the lateral condyle, two cases (40%) were associated with discoid lateral meniscus.
The mean patient age at diagnosis of OCD was 12 years (range 8–16 years). The average age at the time of surgery was 13.4 years, with age limits of 9.75 and 16.5 years.
Clinically, all patients complained of knee pain at diagnosis and one patient had episodes of locking associated with a discoid lateral meniscus.
Initially, all patients received conservative treatment by restriction of sports activities for an average of 6 months (range 3–12 months) without immobilization or non-weight-bearing gait.
A conventional radiography was performed in all patients (anteroposterior [AP], lateral, and skyline views). A computed tomography (CT) scan was performed in 15 cases (37.5%) and magnetic resonance imaging (MRI) in 21 patients (52.5%).
Surgical indication was raised when symptoms persisted after conservative treatment was followed appropriately and/or when the control radiographs showed a worsening of the lesion of osteochondritis, especially when approaching the end of growth.
The location of OCD was defined according to the classifications of Harding [11] and Cahill and Berg [3, 12] on the lateral and AP views, respectively (Fig. 1).
Fig. 1.
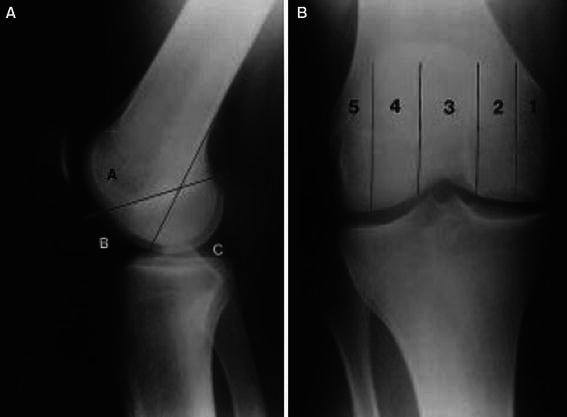
a Harding classification to distinguish anterior, mean, and posterior lesions. b Cahill and Berg classification for medio-lateral localization of the lesions
The radiographic evaluation, as classified by Cahill and Berg, showed a predominance of type 2 lesions (87.5%) and, as classified by Harding, showed a predominance of type B lesions (85%) against 12.5% of type C. One case had a lesion extended to areas B and C of the femoral condyle.
The volume of OCD lesions was measured on AP and lateral views (Fig. 2).
Fig. 2.
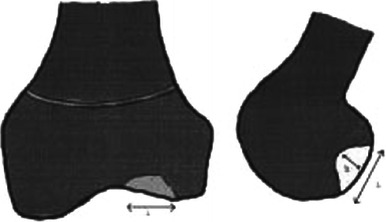
Measures to calculate the lesion volume on anteroposterior (AP) and lateral views of the knee
The mean volume of the lesions was 1,835.4 mm3 (204–6,750 mm3).
The evolutionary stages of condylar osteochondritis were defined according to Bedouelle’s classification [13] (Fig. 3).
Fig. 3.
Bedouelle’s radiological classification
The radiographic evaluation according to the classification of Bedouelle, at the time of surgery, noted 10% stage Ia, 15% Ib, 40% IIa, 22.5% IIb, and 12.5% III; thus, 87.5% of cases were stages I and II. The distal femoral growth plate was open at the time of surgery in 95% of cases.
The postoperative average follow up was 14.8 months (range 8–46 months).
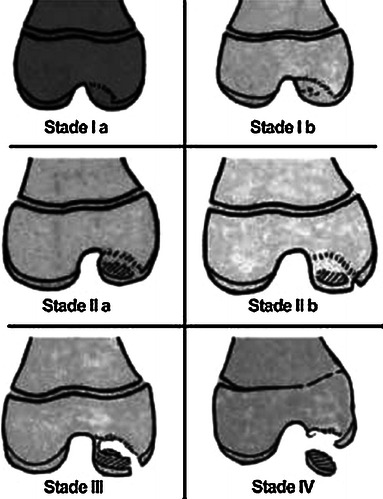
The clinical and radiological evaluation of patients (Fig. 4) was performed by the Hughston score [14] (Tables 1 and 2).
Fig. 4.

a, b A patient with Cahill type 2, Harding type B, and Bedouelle grade IIb osteochondritis dissecans (OCD). c, d The same patient 19 months after a transchondral drilling with a Hughston radiological score of 4
Table 1.
Hughston clinical scale
| Excellent | 4 | Normal sports activity No symptoms Normal physical examination |
| Good | 3 | Normal sports activity Knee pain with intense activities Normal physical examination |
| Average | 2 | Normal sports activity Knee pain and swelling with intense activities Normal physical examination |
| Bad | 1 | Knee pain and swelling with moderate activities Flexum less than 20° |
| Failure | 0 | Restriction of sports Knee pain and swelling with daily activities Flexum more than 20° |
Table 2.
Hughston radiological scale
| 4 | Normal |
| 3 | Defect or sclerosis |
| 2 | Flattening of the condyle |
| 1 | Irregular condyle with narrowing of the joint space less than 50% |
| 0 | Knee arthritis with narrowing of the joint more than 50% |
This is a retrospective descriptive study. The statistical analysis has appealed, for quantitative variables, to nonparametric tests of Spearman, to search for correlations, analysis of variance (ANOVA) by ranks of the Kruskal–Wallis test, and for comparison between groups. For qualitative variables, according to the effectiveness, Fisher’s test or the Chi test were used. The significance level chosen was 0.05.
Surgical technique
Transchondral drilling was described by Smillie in 1957 [15] and was performed, at that time, by open surgery. Currently, this technique is almost exclusively carried out with arthroscopy. So, after a conventional installation for knee arthroscopy, the diseased area is identified. This identification is made on the gross appearance of articular cartilage, gray or yellowish, with a frosted consistency, and abnormal to palpation due to its softening. In case of doubt, an intraoperative fluoroscopic tracking can help. Multiple perforations (5–10) using a fine 1.2–1.5-mm diameter K-wire are made through the articular cartilage, opposite to the lesion of the subchondral bone and passing beyond the zone of sclerosis that circumscribes the lesion. After the drilling, one must observe bleeding from the healthy underlying bone through the puncture holes [16].
Postoperatively, non-weight-bearing for 1 month using two crutches with free mobilization of the knee has been proposed. Discontinuation of sport was the rule. Follow up involves clinical and radiographic monitoring. The resumption of sports activities was allowed 6 months after surgery.
Results
No complications were encountered during the perioperative period. The Hughston Clinic score was 0 in 2.5%, 3 in 25%, and 4 in 72.5%; thus, giving 97.5% of good results (score 3 or 4). The clinical score of 0 corresponds to a skeletally mature patient.
The Hughston radiographic score was 2 in 5%, 3 in 35%, and 4 in 60%; thus, giving 95% of good results (score 3 or 4) (Fig. 5). The radiological score of 2 was found in two skeletally mature patients. A significant correlation (P < 0.001) was found between the radiological and clinical scores of Hughston.
Fig. 5.
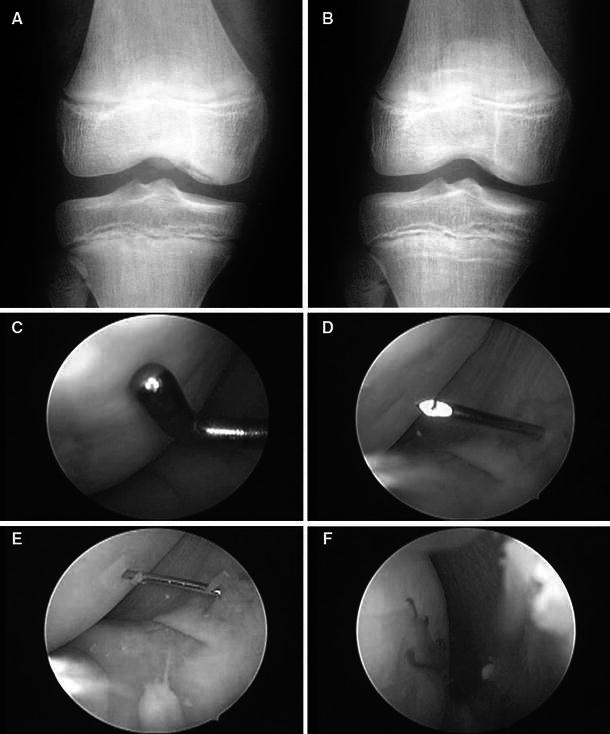
a Grade II b Bedouelle OCD. b Radiograph 6 months later with a Hughston radiological score of 4. c Arthroscopic views for the same patient. Localization of the OCD region. d, e Transchondral drilling with a 1.2-mm K-wire. f Bleeding from the drilling holes
The closed nature of the growth plate at the time of surgery has a significant deleterious effect (P < 0.001) on the clinical and radiographic scores of Hughston.
On the contrary, we have not found any influence on the results of clinical and radiological Hughston scores of the lesion’s volume, its radiological stage, or its location following the Cahill and Berg or Harding classification.
Discussion
The primary goal of the treatment of osteochondritis is to promote the consolidation of the subchondral bone, the preservation of cartilage, and to prevent osteoarthritis.
The ‘immature’ knee, whose physis is still open, has a high potential for cure [2], therefore, conservative treatment should always be the first-line choice in stable juvenile osteochondritis, knowing that about 50% of lesions develop in a positive way in a period of 10–18 months [3, 17].
All patients in our series have maintained a conservative treatment by restriction of sports activities for an average of 6 months, and the use of surgical treatment was offered to one of the following criteria: instability or fragments sequestration, persistence of symptoms in a compliant patient, and the imminent closure of the physis. These indications were similar to those found in the literature [18–20].
For many authors, multiple transchondral drilling was the preferred treatment of juvenile osteochondritis condylar after failure of conservative treatment. Guhl [18] showed in their study that, among the 15 patients, aged 11–18 years, operated by multiple transchondral drilling, 13 had excellent and good results (86.7%). Cepero et al. [19] showed excellent and good clinical and radiological results in 98% of patients operated on for arthroscopic drilling. Aglietti et al. [20] showed a normalization of radiological images in 87.5% of patients treated by drilling and all patients were clinically asymptomatic at 4 years of decline. Bradley and Dandy [21] have performed this technique and noted a radiological and clinical cure in 91% of patients after 2 years of decline. Anderson et al. [2] noted good results in 90% of patients with condylar juvenile osteochondritis. Transarticular drilling was conducted by Ganley et al. [22] in 49 patients aged under 18 years. The drilling was effective in 83% of immature knees against 75% of adolescents with a closed growth plate. Kocher et al. [23] studied the functional and radiological results of this technique in 23 patients with 30 lesions of osteochondritis for a mean of 3.9 years and found clinical and radiological healing in all patients. Louisia and Beaufils [24] have shown good clinical and radiological results in 70.6% of juvenile osteochondritis against 50% in adult osteochondritis.
In our series, all patients were operated by multiple arthroscopic transchondral drilling with good clinical and radiological results in 97.5 and 95% of cases, respectively. From a radiological point of view, the two patients who scored 2 on the Hughston scale were skeletally mature at the time of the surgery.
Conclusion
All patients with osteochondritis dissecans (OCD) of the femoral condyles with an open growth plate had good postoperative clinical and radiological outcomes, therefore, confirming the validity and effectiveness of multiple transchondral drilling in the treatment of juvenile OCD.
Footnotes
An erratum to this article is available at http://dx.doi.org/10.1007/s11832-014-0614-z.
References
- 1.König F. Ueber freie Körper in den Gelenken. Dtsch Z Chir. 1887;27:90–109. doi: 10.1007/BF02792135. [DOI] [Google Scholar]
- 2.Anderson AF, Richards DB, Pagnani MJ, Hovis WD. Antegrade drilling for osteochondritis dissecans of the knee. Arthroscopy. 1997;13(3):319–324. doi: 10.1016/S0749-8063(97)90028-1. [DOI] [PubMed] [Google Scholar]
- 3.Cahill BR. Osteochondritis dissecans of the knee: treatment of juvenile and adult forms. J Am Acad Orthop Surg. 1995;3:237–247. doi: 10.5435/00124635-199507000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Clanton TO, DeLee JC. Osteochondritis dissecans. History, pathophysiology and current treatment concepts. Clin Orthop Relat Res. 1982;167:50–64. [PubMed] [Google Scholar]
- 5.Glancy GL. Juvenile osteochondritis dissecans. Am J Knee Surg. 1999;12:120–124. [PubMed] [Google Scholar]
- 6.Pappas AM. Osteochondrosis dissecans. Clin Orthop Relat Res. 1981;158:59–69. [PubMed] [Google Scholar]
- 7.Murray JRD, Chitnavis J, Dixon P, Hogan NA, Parker G, Parish EN, et al. Osteochondritis dissecans of the knee; long-term clinical outcome following arthroscopic debridement. Knee. 2007;14:94–98. doi: 10.1016/j.knee.2006.11.011. [DOI] [PubMed] [Google Scholar]
- 8.Kocher MS, Tucker R, Ganley TJ, Flynn JM. Management of osteochondritis dissecans of the knee: current concepts review. Am J Sports Med. 2006;34(7):1181–1191. doi: 10.1177/0363546506290127. [DOI] [PubMed] [Google Scholar]
- 9.Mubarak SJ, Carroll NC. Familial osteochondritis dissecans of the knee. Clin Orthop Relat Res. 1979;140:131–136. [PubMed] [Google Scholar]
- 10.Hefti F, Beguiristain J, Krauspe R, Möller-Madsen B, Riccio V, Tschauner C, et al. Osteochondritis dissecans: a multicenter study of the European Pediatric Orthopedic Society. J Pediatr Orthop B. 1999;8:231–245. [PubMed] [Google Scholar]
- 11.Harding WG., 3rd Diagnosis of ostechondritis dissecans of the femoral condyles: the value of the lateral X-ray view. Clin Orthop Relat Res. 1977;123:25–26. [PubMed] [Google Scholar]
- 12.Cahill BR, Berg BC. 99m-Technetium phosphate compound joint scintigraphy in the management of juvenile osteochondritis dissecans of the femoral condyles. Am J Sports Med. 1983;11:329–335. doi: 10.1177/036354658301100509. [DOI] [PubMed] [Google Scholar]
- 13.Bedouelle J (1988) L’ostéochondrite disséquante des condyles fémoraux chez l’enfant et l’adolescent. In: Cahiers d’enseignement de la SOFCOT. Expansion Scientifique Française, pp 61–93
- 14.Hughston JC, Hergenroeder PT, Courtenay BG. Osteochondritis dissecans of the femoral condyles. J Bone Joint Surg Am. 1984;66:1340–1348. [PubMed] [Google Scholar]
- 15.Smillie IS. Treatment of osteochondritis dissecans. J Bone Joint Surg Br. 1957;39:248–260. doi: 10.1302/0301-620X.39B2.248. [DOI] [PubMed] [Google Scholar]
- 16.Lefort G, Moyen B, Beaufils P, De Billy B, Breda R, Cadilhac C, et al. L’ostéochondrite disséquante des condyles fémoraux: analyse de 892 cas. Rev Chir Orthop Traumatol. 2006;92(S5):97–141. [PubMed] [Google Scholar]
- 17.Cahill BR, Phillips MR, Navarro R. The results of conservative management of juvenile osteochondritis dissecans using joint scintigraphy. A prospective study. Am J Sports Med. 1989;17:601–606. doi: 10.1177/036354658901700502. [DOI] [PubMed] [Google Scholar]
- 18.Guhl JF. Arthroscopic treatment of osteochondritis dissecans. Clin Orthop Relat Res. 1982;167:65–74. [PubMed] [Google Scholar]
- 19.Cepero S, Ullot R, Sastre S. Osteochondritis of the femoral condyles in children and adolescents: our experience over the last 28 years. J Pediatr Orthop B. 2005;14:24–29. doi: 10.1097/01202412-200501000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Aglietti P, Buzzi R, Bassi PB, Fioriti M. Arthroscopic drilling in juvenile osteochondritis dissecans of the medial femoral condyle. Arthroscopy. 1994;10:286–291. doi: 10.1016/S0749-8063(05)80113-6. [DOI] [PubMed] [Google Scholar]
- 21.Bradley J, Dandy DJ. Results of drilling osteochondritis dissecans before skeletal maturity. J Bone Joint Surg Br. 1989;71:642–644. doi: 10.1302/0301-620X.71B4.2768313. [DOI] [PubMed] [Google Scholar]
- 22.Ganley TJ, Amro RR, Gregg JR, Halpern KV (2002) Antegrade drilling for osteochondritis dissecans of the knee. Pediatric Orthopaedic Society of North America
- 23.Kocher MS, Micheli LJ, Yaniv M, Zurakowski D, Ames A, Adrignolo AA. Functional and radiographic outcome of juvenile osteochondritis dissecans of the knee treated with transarticular arthroscopic drilling. Am J Sports Med. 2001;29:562–566. doi: 10.1177/03635465010290050701. [DOI] [PubMed] [Google Scholar]
- 24.Louisia S, Beaufils P. Perforations transcartilagineuses dans le traitement de l’ostéochondrite disséquante du condyle fémoral interne. Montpellier: Sauramps Médical; 1997. [Google Scholar]


