Abstract
Critically ill patients whose course is complicated by acute kidney injury often receive renal replacement therapy (RRT). For these patients, initiation of RRT results in a considerable escalation in both the complexity and associated cost of care. While RRT is extensively used in clinical practice, there remains uncertainty about the ideal circumstances of when to initiate RRT and for what indications. The process of deciding when to initiate RRT in critically ill patients is complex and is influenced by numerous factors, including patient-specific and clinician-specific factors and those related to local organizational/logistical issues. Studies have shown marked variation between clinicians, and across institutions and countries. As a consequence, analysis of ideal circumstances under which to initiate RRT is challenging. Recognizing this limitation, we review the available data and propose a clinical algorithm to aid in the decision for RRT initiation in critically ill adult patients. The algorithm incorporates several patient-specific factors, based on evidence when available, that may decisively influence when to initiate RRT. The objective of this algorithm is to provide a starting point to guide clinicians on when to initiate RRT in critically ill adult patients. In addition, the proposed algorithm is intended to provide a foundation for prospective evaluation and the development of a broad consensus on when to initiate RRT in critically ill patients.
Introduction
Acute kidney injury (AKI) is a well-recognized complication of critical illness with an important impact on morbidity, mortality and health resource utilization [1-5]. Renal replacement therapy (RRT) is often required and represents a substantial escalation in the complexity and cost of care for critically ill patients with AKI [4]. Despite its extensive use in clinical practice, there is uncertainty about the optimal time and indications for initiation of RRT in the ICU [6]. Clearly, the process involved in deciding when to initiate RRT in critically ill adult patients is complex and can be influenced by numerous factors, including patient-specific and clinician-specific factors and those related to organizational/logistical issues (Table 1). Indeed, studies have shown marked variation of practice between clinicians, and across institutions and countries [7,8].
Table 1.
Summary of selected factors potentially influencing the decision to initiate renal replacement therapy in critically ill patients
| Factors | |
|---|---|
| Patient-specific | Kidney function/reserve |
| Co-morbid disease and physiologic reserve | |
| Primary diagnosis: severity of illness and trajectory | |
| Acute kidney injury: severity and trend | |
| Clinician-specific | Goals of therapy |
| Relative indications and clinician threshold for initiation | |
| Local practice patterns | |
| Prescribing service | |
| Organizational | Country/institution |
| ICU type | |
| Machine and nursing availability | |
| Health costs |
An evaluation of timing of RRT initiation has been the focus of a number of clinical studies. These have recently been summarized in a systematic review and meta-analysis [6,9-13]. Most of these studies have been small, retrospective or secondary analyses, and have arbitrarily dichotomized the study population into 'early' or 'late' RRT initiation based on biochemical criteria, urine output criteria, or by 'door-to-dialysis' time [14]. The meta-analysis by Seabra and colleagues [12] also included five randomized trials. A pooled analysis from these trials showed a non-statistically significant trend towards reduced mortality with earlier initiation of RRT (relative risk 0.64; 95% confidence interval (CI), 0.40 to 1.05, P = 0.08). However, this pooled analysis only included data from 270 patients, thus limiting its statistical power. Accordingly, this limits the inferences about timing of RRT initiation and prohibits a simple translation of such data easily to the bedside to guide clinical management. While large prospective studies are urgently needed, the currently available data would indicate a potential benefit associated with earlier initiation of RRT for those patients where RRT is likely to be needed in terms of both survival and recovery of kidney function [12,15].
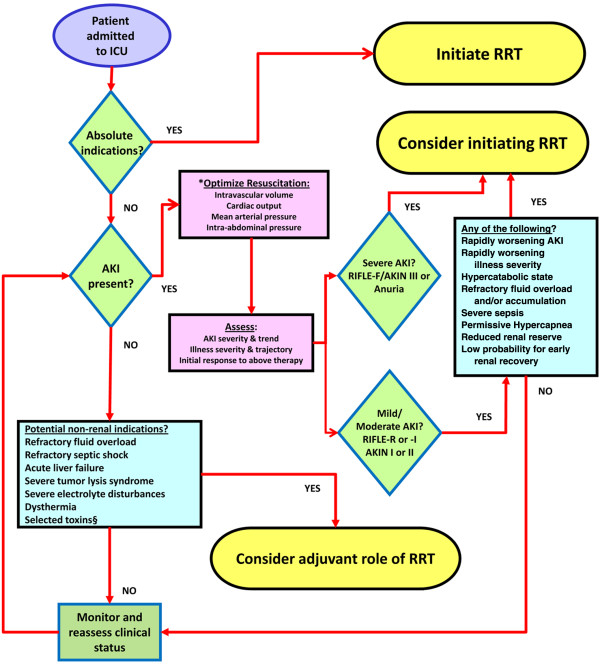
Currently, there exists no broad consensus to guide clinicians on this important issue. In fact, RRT initiation has been repeatedly identified as a research priority [16-18]. Accordingly, we have developed an opinion-based clinical algorithm to aid in the decision on when to consider initiation of RRT in critically ill patients (Figure 1). The algorithm gives a more quantitative characterization of 'timing' and incorporates several patient-specific factors, based on clinical evidence when available, that may influence when to initiate RRT. We adapt the terminology proposed by the Acute Kidney Injury Network (AKIN): 'illness trajectory' refers to the pace of clinical evolution of the patient, and AKI 'trend' refers to the rate of clinical and/or biochemical changes (including urea and creatinine) [16]. The objective of this algorithm is to provide a starting point to guide clinicians on when to consider use of RRT in adult critically ill patients. This algorithm will not specifically address additional key issues in the delivery of renal support, such as RRT modality (continuous versus intermittent), mode (convection versus diffusion) and dose delivery [17-20]. Importantly, the algorithm is also intended to provide a starting point for further prospective evaluation to understand the ideal time/circumstances for when to initiate RRT that could, in due course, promote higher quality of patient care and improved clinical outcomes.
Figure 1.
Algorithm for initiation of renal replacement therapy in critically ill patients. *'Optimized resuscitation' of the kidney should also include discontinuation/withholding nephrotoxic medications and anti-hypertensive medications that may exacerbate kidney function. §Exogenous toxins (see [56]) and selected endogenous toxins (for example, myoglobin; see text). AKI, acute kidney injury; AKIN, Acute Kidney Injury Network; RRT, renal replacement therapy.
Algorithm for initiation of renal replacement therapy in critically ill patients
The first priority after a patient is admitted to ICU is determination of whether there are absolute indications and/or emergent need for RRT. A summary of proposed absolute indications for RRT initiation, based on consensus, is presented in Table 2[16]. It is important, however, to recognize that RRT initiation in these circumstances can largely be viewed as 'rescue therapy' where delays may have deleterious consequences for the patient. Moreover, these indications are largely adapted from 'classic conventional' indications for RRT in end-stage kidney disease, wherein the main objective is alleviation of uremic complications.
Table 2.
A summary of absolute or 'rescue therapy' indications for initiation of renal replacement therapy in critically ill patients
| Category | Characteristic |
|---|---|
| Metabolic | |
| Azotemia | Serum urea ≥ 36 mmol/L (100 mg/dL) |
| Uremic complications | Encephalopathy, pericarditis, bleeding |
| Hyperkalemia | K+ ≥ 6 mmol/L and/or electrocardiogram abnormalities |
| Hypermagnesemia | ≥ 4 mmol/L and/or anuria/absent deep tendon reflexes |
| Acidosis | Serum pH ≤ 7.15 |
| Oligo-anuria | Urine output <200 mL/12 h or anuria |
| Fluid overload | Diuretic-resistant organ edema (that is, pulmonary edema) in the presence of acute kidney injury |
Adapted from [16].
Since AKI is common in critical illness, in the absence of absolute indications for RRT, the next logical step is to determine whether patients have AKI. In a multi-center multinational study, Uchino and colleagues [4] found AKI occurred in 5 to 6% of all ICU admissions, with 70% of these eventually receiving RRT. Recent data indicate the incidence of AKI is rising [21-23]. Historically, however, establishing incidence estimates of AKI has been problematic due to the lack of a standardized definition. Fortunately, a consensus-driven classification scheme for AKI, the RIFLE criteria (and modified AKIN criteria), has been recently proposed, which represents a noteworthy advance for clinical practice and research in AKI [24,25]. The RIFLE criteria have been validated and proven robust for clinically relevant outcomes in patients with AKI across numerous studies [3,5,26-29]. Epidemiologic studies of AKI, when defined by the RIFLE criteria, have shown that 11 to 67% of ICU patients may develop AKI during their illness course [29].
The RIFLE/AKIN criteria and initiation of renal replacement therapy
The RIFLE criteria were initially developed to standardize the diagnosis, classify the severity and monitor progression of AKI. Importantly, they were also designed to enable better comparison of clinical studies on the epidemiology and attributable outcomes for AKI [24]. Currently, there is no consensus on how to define timing of RRT initiation due to the aforementioned limitations in available data. The concept of 'timing' remains poorly defined and inconsistent [16]. Previously, timing of RRT has mostly been described by qualitative criteria (early versus late/delayed). The RIFLE/AKIN criteria provide the possibility of a more 'quantitative' characterization of timing. We recognize that these criteria have not been formally evaluated as a tool for guiding clinicians on when to initiate RRT. Yet, data from numerous observational studies have consistently shown that earlier initiation of RRT (however defined) correlated with improved survival. This would appear to provide some justification of 'early', or perhaps a better term could be 'timely', RRT initiation in selected critically ill patients with AKI. However, further investigation, preferably by prospective randomized trials, is undoubtedly warranted. A prospective analysis of the impact of RRT initiation incorporating the RIFLE/AKIN classification schemes on survival and renal recovery is a potential starting point. Can these criteria have bedside utility to aid in clinical decision-making? We believe this is a logical first step in understanding how research evidence may be translated into clinical practice to improve outcomes in patients with AKI.
The RIFLE/AKIN criteria are also able to classify AKI severity and follow trends over time [29]; both are vital to consider in the context of RRT initiation. They are also a tool for dynamic evaluation of response to initial (non-RRT) therapy. We emphasize again this algorithm is not intended to direct all aspects of initial resuscitation and supportive therapy, but rather provide an outline for when to consider RRT initiation. Recent comprehensive reviews, based on consensus, have summarized strategies for initial management of AKI [30].
Initiation of renal replacement therapy: risks versus benefits
Initiation of RRT is not without risk for adverse consequences, including hypotension (and exacerbation of kidney injury), bleeding (depending on the anticoagulant used), dialysis catheter-related complications, and exposure of patient blood to an extracorporeal circuit. In addition, earlier initiation of RRT has the potential to expose patients to this therapy who may have otherwise spontaneously recovered kidney function and/or survived without having received it. This issue, however, is complicated by a paucity of data in critically ill patients with AKI investigating factors that reliably predict whether recovery of kidney function will occur (that is, partial recovery or RRT-free) and whether this can be modified by earlier RRT initiation. We believe this is a research priority. Therefore, recognizing these gaps in knowledge are important along with carefully weighing the potential risks of RRT initiation against the goals of therapy and proposed benefits.
Severe and/or acutely worsening acute kidney injury
In the presence of severe AKI (that is, RIFLE category F or AKIN category III) and/or rapidly deteriorating kidney function, we would consider RRT initiation, particularly if there was failure to respond to initial therapy [30]. Data to support earlier RRT in these patients is largely generated from observational data [3,5,31]. In a single-centre retrospective study of 5,383 critically ill patients, Hoste and colleagues [3] found that of those developing RIFLE class R, 56% progressed to either class I or F, and of those developing RIFLE class I, 36% progressed to RIFLE class F. Patients achieving RIFLE class F had a far worse clinical outcome, characterized by an adjusted hazards ratio for hospital death of 2.7 (95% CI, 2.0 to 3.6) and longer durations of stay in both ICU and hospital. Yet, of these RIFLE class F patients, only 14.2% received RRT. However, no specific analysis was performed in this study to explore whether the higher mortality for this group (RIFLE class F) was modified by earlier RRT initiation. Bell and colleagues [31] performed a 7-year retrospective analysis of 207 patients with AKI receiving RRT. When stratified by RIFLE class at the time RRT was initiated, those with RIFLE class F had considerably higher 30-day mortality when compared to those initiating RRT at either RIFLE class R or I (adjusted hazards ratio 3.4; 95% CI, 1.2 to 9.3; crude 30-day mortality, 57.9% for F versus 23.5% for R versus 22.0% for I). The RIFLE/AKIN class should not likely be used in isolation to decide on when to initiate RRT - but rather together with the overall goals of therapy along with weighing of other relevant clinical variables. We recognize that additional prospective evaluation on this issue is needed to guide clinical practice; however, in many circumstances, the risks of not providing RRT may exceed those of initiation of RRT.
Mild to moderate acute kidney injury
The decision of if, and when, to initiate RRT in critically ill patients with mild-moderate AKI (that is, RIFLE category R/I or AKIN category I/II) is often the most challenging. It is important to recognize that the decision to initiate RRT in these patients is most likely to be multi-factorial and unlikely to be made for any single indication. Several baseline factors should be considered in these patients, including goals of therapy, primary diagnosis, illness severity, baseline kidney function/reserve and the need to potentially anticipate and prevent complications that may be compounded in the presence of AKI. Primary diagnoses associated with high catabolic rates (that is, septic shock, major trauma, burn injury) or those likely to place considerable demand on kidney function (that is, gastrointestinal bleeding, rhabdomyolysis) should be identified in the context of potential need for earlier initiation of RRT.
Dynamic factors
Likewise, several 'dynamic' factors, including the trends in AKI and/or illness severity, warrant consideration. Acute and/or rapid changes in clinical status, such as whether AKI is progressing (and how rapidly), the probability of kidney recovery, whether illness severity is progressing (and how rapidly), and additional measures of acute physiology such as fluid accumulation [32], relative oliguria (that is, urine output >200 ml/12 h, but insufficient to prevent fluid accumulation) and the trajectory of non-kidney organ dysfunction should factor into the decision of when to initiate RRT for those with established mild-moderate AKI.
Co-interventions
Certain co-interventions in the ICU will also influence the decision to initiate RRT in patients with mild to moderate AKI [33]. For example, co-interventions may contribute to urea or fluid accumulation, or systemic acidemia, therefore placing a greater demand on already compromised kidney function. The use of adjuvant corticosteroids in severe sepsis/septic shock is common and can aggravate protein catabolism and azotemia [34]. The increased urea generation coupled with retention of uremic solutes may create a circumstance where RRT initiation may need to be considered in those with mild-moderate AKI.
The concept of early goal-directed therapy as a guide for acute resuscitation in septic shock has represented a significant philosophical shift in the management of these patients [35,36]. A key component of early goal-directed therapy is the administration of fluid therapy, ideally targeted to physiologic endpoints. In the trial by Rivers and colleagues [36], enrolled patients received an estimated 13 to 14 liters of fluid therapy in the first 72 hours (most within the initial 6 hours). While this trial did not provide data on AKI occurrence, oliguria or fluid balance, septic patients are known to be at high risk for AKI [37,38]. In this context, coexistent or rapidly evolving AKI results in impaired free water and solute excretion, and contributes to rapid fluid accumulation and metabolic acidosis (especially with high chloride containing solutions). These complex and integrated conditions present a circumstance where earlier RRT may prove beneficial. Diuretic therapy can be a useful adjunct for management of fluid accumulation; however, their use in patients with AKI should not delay RRT initiation with the intent of avoiding RRT. In one study, diuretic use was associated with increased mortality and non-recovery of kidney function, which may have occurred in part due to delayed initiation of RRT [39].
Critically ill patients with acute lung injury/acute respiratory distress syndrome receiving lung-protective ventilation may intentionally develop respiratory acidosis due to permissive hypercapnea [40]. Co-existent and/or evolving AKI in these patients will significantly impair capacity for kidney bicarbonate regeneration to buffer systemic acidemia. Earlier RRT may prove beneficial in these patients prior to the development of severe acidemia, worsening acute respiratory distress syndrome and/or volume overload.
Non-kidney and other potential factors influencing initiation of renal replacement therapy
This list of potential 'non-kidney' indications for initiation of RRT in critically patients continues to grow [16]. In this context, the term extracorporeal blood purification (EBP), rather than RRT, may be more appropriate.
Refractory septic shock
The use of EBP in sepsis is controversial. In particular, high-volume hemofiltration has been advocated as a potential adjuvant immunomodulatory therapy in refractory septic shock by some consensus groups [41,42] but not others [35]. Several small clinical trials have shown promising results for improvements in hemodynamics, metabolic parameters and survival [43-45]. In their consensus statement the Acute Dialysis Quality Initiative (ADQI) Working Group concluded that the use of EBP in sepsis has biological rationale that merits further investigation. While confirmatory data from multi-center randomized trials are needed to inform clinical practice on this issue, the authors believe that patients with refractory septic shock may benefit from high-volume EBP [41].
Fluid overload or accumulation
A positive fluid balance and overt clinical fluid overload, in particular when refractory to medical therapy (that is, diuretics), is also an important circumstance where RRT initiation may prove beneficial [46]. In critically ill patients, fluid overload may be under-recognized as an important contributor to morbidity and mortality [32,47-51]. Longer duration of mechanical ventilation, weaning failure, delayed tissue-healing, and cardiopulmonary complications have all been associated with fluid overload [50-52]. Likewise, a positive fluid balance has been shown to predict mortality in critically ill adults, an association likely modified by AKI [47,48]. This significant and independent association between fluid overload and mortality has been further revealed in numerous clinical studies of critically ill children receiving continuous RRT [53-55]. These data collectively present an argument that fluid balance is an important biomarker in critical illness [46]. RRT initiation should therefore be viewed as a potentially important therapeutic measure, not only for treatment of refractory fluid overload, but also for the prevention of excessive fluid accumulation that may contribute to worse clinical outcomes.
Toxins
Although considered controversial, EBP for selected toxins is not infrequently performed [56]. EBP is more likely when the intoxication is complicated by kidney dysfunction, which may further reduce clearance of the toxin and/or its metabolites. In addition to the exogenous toxins, EBP can also be performed to aid in clearance of selected endogenous toxins, particularly in the context of concomitant kidney dysfunction (that is, rhabdomyolysis, tumor lysis syndrome). Electrolyte disturbances and metabolic acidosis induced by certain toxins can also be readily corrected with EBP. Drug and toxin clearance is influenced by several factors, including molecular weight, volume of distribution, degree of protein binding, and water solubility. It is beyond the scope of this review to discuss details of indications and/or prescription of EBP for overdoses/intoxications. Recent comprehensive reviews have been published [56].
Additional indications
RRT initiation for 'non-kidney' indications may also be considered as a therapeutic and/or supportive treatment for several other conditions such as severe electrolyte disturbances (that is, acid-base, dysnatremia) or disorders of thermoregulation. Likewise, RRT can theoretically serve as an adjuvant therapy for interrupting non-kidney organ dysfunction (that is, acute lung injury, congestive heart failure) and attenuating pathologic organ crosstalk [57,58].
It is important to recognize, however, there are numerous, often co-existent, physiologic and clinical insults occurring in critically ill patients that have the potential to negatively impact kidney function (that is, elevated intra-abdominal pressure, mechanical ventilation with elevated positive end-expiratory pressure (PEEP), nephrotoxins, radiocontrast media). Likewise, the early detection of AKI is an obvious clinical priority; however, current diagnostic methods rely on conventional biomarkers and urine output. These are not ideal, fail to reflect real-time declines in glomerular filtration, and provide no data on whether a genuinely injurious process to the kidney has occurred [6,59]. More importantly, these conventional biomarkers require time to accumulate and can translate into delayed recognition of AKI [6,59]. Accordingly, while a patient may not (yet) fulfill the RIFLE criteria for AKI, impaired kidney function may still be present, evolving and undetected. The introduction of novel biomarkers for AKI will hopefully advance this area [60]. As more definitive data become available, incorporation of these biomarkers into the decision-making process is likely.
Conclusion
Critically ill patients whose course is complicated by AKI often receive RRT. RRT is an important therapeutic and supportive measure and is commonly used in clinical practice. However, there remains uncertainty about the ideal circumstances in which to initiate RRT and for what indications. The process of deciding when to initiate RRT in critically ill patients is complex and can be influenced by numerous factors. Currently, there exists large variation in clinical practice between clinicians and across institutions and countries, due, in part, to the lack of consensus on this issue. We have proposed a clinically based algorithm to aid in the decision on when to initiate RRT in critically ill patients that incorporates patient-specific factors and based on available clinical evidence. The intent of this algorithm is to provide a starting point to guide clinicians on when to consider initiation of RRT in critically ill patients and provide a foundation for further prospective evaluation and development of broad consensus on this important issue.
Abbreviations
AKI: acute kidney injury; AKIN: Acute Kidney Injury Network; CI: confidence interval; EBP: extracorporeal blood purification; RRT: renal replacement therapy.
Competing interests
SMB, DNC, NG and CR have all participated in ADQI workgroups. NG and CR have participated in AKIN workgroups.
Contributor Information
Sean M Bagshaw, Email: sean.bagshaw@capitalhealth.ca.
Dinna N Cruz, Email: dinnacruzmd@yahoo.com.
RT Noel Gibney, Email: ngibney@ualberta.ca.
Claudio Ronco, Email: cronco@goldnet.it.
Acknowledgements
SMB is supported by a Clinical Investigator Award from the Alberta Heritage Foundation for Medical Research.
References
- Ahlstrom A, Tallgren M, Peltonen S, Rasanen P, Pettila V. Survival and quality of life of patients requiring acute renal replacement therapy. Intensive Care Med. 2005;31:1222–1228. doi: 10.1007/s00134-005-2681-6. [DOI] [PubMed] [Google Scholar]
- Bagshaw SM, Laupland KB, Doig CJ, Mortis G, Fick GH, Mucenski M, Godinez-Luna T, Svenson LW, Rosenal T. Prognosis for long-term survival and renal recovery in critically ill patients with severe acute renal failure: a population-based study. Crit Care. 2005;9:R700–R709. doi: 10.1186/cc3879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoste EA, Clermont G, Kersten A, Venkataraman R, Angus DC, De Bacquer D, Kellum JA. RIFLE criteria for acute kidney injury are associated with hospital mortality in critically ill patients: a cohort analysis. Crit Care. 2006;10:R73. doi: 10.1186/cc4915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uchino S, Kellum JA, Bellomo R, Doig GS, Morimatsu H, Morgera S, Schetz M, Tan I, Bouman C, Macedo E, Gibney N, Tolwani A, Ronco C. Beginning and Ending Supportive Therapy for the Kidney (BEST Kidney) Investigators. Acute renal failure in critically ill patients: a multinational, multicenter study. JAMA. 2005;294:813–818. doi: 10.1001/jama.294.7.813. [DOI] [PubMed] [Google Scholar]
- Cruz DN, Bolgan I, Perazella MA, Bonello M, de Cal M, Corradi V, Polanco N, Ocampo C, Nalesso F, Piccinni P, Ronco C. North East Italian Prospective Hospital Renal Outcome Survey on Acute Kidney Injury (NEiPHROS-AKI): targeting the problem with the RIFLE Criteria. Clin J Am Soc Nephrol. 2007;2:418–425. doi: 10.2215/CJN.03361006. [DOI] [PubMed] [Google Scholar]
- Bagshaw SM, Bellomo R. Early diagnosis of acute kidney injury. Curr Opin Crit Care. 2007;13:638–644. doi: 10.1097/MCC.0b013e3282f07570. [DOI] [PubMed] [Google Scholar]
- Ricci Z, Ronco C, D'Amico G, De Felice R, Rossi S, Bolgan I, Bonello M, Zamperetti N, Petras D, Salvatori G, Dan M, Piccinni P. Practice patterns in the management of acute renal failure in the critically ill patient: an international survey. Nephrol Dial Transplant. 2006;21:690–696. doi: 10.1093/ndt/gfi296. [DOI] [PubMed] [Google Scholar]
- Overberger P, Pesacreta M, Palevsky PM. Management of renal replacement therapy in acute kidney injury: a survey of practitioner prescribing practices. Clin J Am Soc Nephrol. 2007;2:623–630. doi: 10.2215/CJN.00780207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gettings LG, Reynolds HN, Scalea T. Outcome in post-traumatic acute renal failure when continuous renal replacement therapy is applied early versus late. Intensive Care Med. 1999;25:805–813. doi: 10.1007/s001340050956. [DOI] [PubMed] [Google Scholar]
- Kresse S, Schlee H, Deuber HJ, Koall W, Osten B. Influence of renal replacement therapy on outcome of patients with acute renal failure. Kidney Int Suppl. 1999. pp. S75–78. [DOI] [PubMed]
- Liu KD, Himmelfarb J, Paganini EP, Ikizler A, Soroko S, Mehta RL, Chertow GM. Timing of initiation of dialysis in critically ill patients with acute kidney injury. CJASN. 2006;1:915–919. doi: 10.2215/CJN.01430406. [DOI] [PubMed] [Google Scholar]
- Seabra VF, Balk EM, Liangos O, Sosa MA, Cendoroglo M, Jaber BL. Timing of renal replacement therapy initiation in acute renal failure: a meta-analysis. Am J Kidney Dis. 2008;52:272–284. doi: 10.1053/j.ajkd.2008.02.371. [DOI] [PubMed] [Google Scholar]
- Splendiani G, Mazzarella V, Cipriani S, Zazzaro D, Casciani CU. Continuous renal replacement therapy: our experience in intensive care unit. Ren Fail. 2001;23:259–264. doi: 10.1081/JDI-100103497. [DOI] [PubMed] [Google Scholar]
- Gibney RT, Bagshaw SM, Kutsogiannis DJ, Johnston C. When should renal replacement therapy for acute kidney injury be initiated and discontinued? Blood Purif. 2008;26:473–484. doi: 10.1159/000157325. [DOI] [PubMed] [Google Scholar]
- Bagshaw SM, Uchino S, Bellomo R, Morimatsu H, Morgera S, Schetz M, Tan I, Bouman C, Macedo E, Gibney N, Tolwani A, Oudemans-van Straaten HM, Ronco C, Kellum JA. Beginning and Ending Supportive Therapy for the Kidney (BEST Kidney) Investigators. Timing of renal replacement therapy and clinical outcomes in critically ill patients with severe acute kidney injury. J Crit Care. 2009;24:129–140. doi: 10.1016/j.jcrc.2007.12.017. [DOI] [PubMed] [Google Scholar]
- Gibney N, Hoste E, Burdmann EA, Bunchman T, Kher V, Viswanathan R, Mehta RL, Ronco C. Timing of initiation and discontinuation of renal replacement therapy in AKI: unanswered key questions. Clin J Am Soc Nephrol. 2008;3:876–880. doi: 10.2215/CJN.04871107. [DOI] [PubMed] [Google Scholar]
- Davenport A, Bouman C, Kirpalani A, Skippen P, Tolwani A, Mehta RL, Palevsky PM. Delivery of renal replacement therapy in acute kidney injury: what are the key issues? Clin J Am Soc Nephrol. 2008;3:869–875. doi: 10.2215/CJN.04821107. [DOI] [PubMed] [Google Scholar]
- Palevsky PM. Indications and timing of renal replacement therapy in acute kidney injury. Crit Care Med. 2008;36:S224–228. doi: 10.1097/CCM.0b013e318168e3fb. [DOI] [PubMed] [Google Scholar]
- Bagshaw SM, Berthiaume LR, Delaney A, Bellomo R. Continuous versus intermittent renal replacement therapy for critically ill patients with acute kidney injury: a meta-analysis. Crit Care Med. 2008;36:610–617. doi: 10.1097/01.CCM.0B013E3181611F552. [DOI] [PubMed] [Google Scholar]
- Pannu N, Klarenbach S, Wiebe N, Manns B, Tonelli M. Renal replacement therapy in patients with acute renal failure: a systematic review. JAMA. 2008;299:793–805. doi: 10.1001/jama.299.7.793. [DOI] [PubMed] [Google Scholar]
- Ali T, Khan I, Simpson W, Prescott G, Townend J, Smith W, Macleod A. Incidence and outcomes in acute kidney injury: a comprehensive population-based study. J Am Soc Nephrol. 2007;18:1292–1298. doi: 10.1681/ASN.2006070756. [DOI] [PubMed] [Google Scholar]
- Bagshaw SM, George C, Bellomo R. Changes in the incidence and outcome for early acute kidney injury in a cohort of Australian intensive care units. Crit Care. 2007;11:R68. doi: 10.1186/cc5949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xue JL, Daniels F, Star RA, Kimmel PL, Eggers PW, Molitoris BA, Himmelfarb J, Collins AJ. Incidence and mortality of acute renal failure in Medicare beneficiaries, 1992 to 2001. J Am Soc Nephrol. 2006;17:1135–1142. doi: 10.1681/ASN.2005060668. [DOI] [PubMed] [Google Scholar]
- Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P. Acute renal failure - definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2004;8:R204–212. doi: 10.1186/cc2872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ronco C, Levin A, Warnock DG, Mehta R, Kellum JA, Shah S, Molitoris BA. Improving outcomes from acute kidney injury (AKI): Report on an initiative. Int J Artif Organs. 2007;30:373–376. [PubMed] [Google Scholar]
- Bagshaw SM, George C, Dinu I, Bellomo R. A multi-centre evaluation of the RIFLE criteria for early acute kidney injury in critically ill patients. Nephrol Dial Transplant. 2008;23:1203–1210. doi: 10.1093/ndt/gfm744. [DOI] [PubMed] [Google Scholar]
- Ostermann M, Chang RW. Acute kidney injury in the intensive care unit according to RIFLE. Crit Care Med. 2007;35:1837–1843. doi: 10.1097/01.CCM.0000277041.13090.0A. quiz 1852. [DOI] [PubMed] [Google Scholar]
- Uchino S, Bellomo R, Goldsmith D, Bates S, Ronco C. An assessment of the RIFLE criteria for acute renal failure in hospitalized patients. Crit Care Med. 2006;34:1913–1917. doi: 10.1097/01.CCM.0000224227.70642.4F. [DOI] [PubMed] [Google Scholar]
- Ricci Z, Cruz D, Ronco C. The RIFLE criteria and mortality in acute kidney injury: A systematic review. Kidney Int. 2008;73:538–546. doi: 10.1038/sj.ki.5002743. [DOI] [PubMed] [Google Scholar]
- Himmelfarb J, Joannidis M, Molitoris B, Schietz M, Okusa MD, Warnock D, Laghi F, Goldstein SL, Prielipp R, Parikh CR, Pannu N, Lobo SM, Shah S, D'Intini V, Kellum JA. Evaluation and initial management of acute kidney injury. Clin J Am Soc Nephrol. 2008;3:962–967. doi: 10.2215/CJN.04971107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell M, Liljestam E, Granath F, Fryckstedt J, Ekbom A, Martling CR. Optimal follow-up time after continuous renal replacement therapy in actual renal failure patients stratified with the RIFLE criteria. Nephrol Dial Transplant. 2005;20:354–360. doi: 10.1093/ndt/gfh581. [DOI] [PubMed] [Google Scholar]
- Bouchard J, Soroko SB, Chertow GM, Himmelfarb J, Ikizler TA, Paganini EP, Mehta RL. Fluid accumulation, survival and recovery of kidney function in critically ill patients with acute kidney injury. Kidney Int. 2009;76:422–427. doi: 10.1038/ki.2009.159. [DOI] [PubMed] [Google Scholar]
- Liu KD, Matthay MA, Chertow GM. Evolving practices in critical care and potential implications for management of acute kidney injury. Clin J Am Soc Nephrol. 2006;1:869–873. doi: 10.2215/CJN.00450206. [DOI] [PubMed] [Google Scholar]
- Slotman GJ, Fisher CJ Jr, Bone RC, Clemmer TP, Metz CA. Detrimental effects of high-dose methylprednisolone sodium succinate on serum concentrations of hepatic and renal function indicators in severe sepsis and septic shock. The Methylprednisolone Severe Sepsis Study Group. Crit Care Med. 1993;21:191–195. doi: 10.1097/00003246-199302000-00008. [DOI] [PubMed] [Google Scholar]
- Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, Reinhart K, Angus DC, Brun-Buisson C, Beale R, Calandra T, Dhainaut JF, Gerlach H, Harvey M, Marini JJ, Marshall J, Ranieri M, Ramsay G, Sevransky J, Thompson BT, Townsend S, Vender JS, Zimmerman JL, Vincent JL. International Surviving Sepsis Campaign Guidelines Committee; American Association of Critical-Care Nurses; American College of Chest Physicians; American College of Emergency Physicians; Canadian Critical Care Society; European Society of Clinical Microbiology and Infectious Diseases et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med. 2008;36:296–327. doi: 10.1097/01.CCM.0000298158.12101.41. [DOI] [PubMed] [Google Scholar]
- Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–1377. doi: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
- Bagshaw SM, George C, Bellomo R. Early acute kidney injury and sepsis: a multicentre evaluation. Crit Care. 2008;12:R47. doi: 10.1186/cc6948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagshaw SM, Uchino S, Bellomo R, Morimatsu H, Morgera S, Schetz M, Tan I, Bouman C, Macedo E, Gibney N, Tolwani A, Oudemans-van Straaten HM, Ronco C, Kellum JA. Beginning and Ending Supportive Therapy for the Kidney (BEST Kidney) Investigators. Septic acute kidney injury in critically ill patients: clinical characteristics and outcomes. Clin J Am Soc Nephrol. 2007;2:431–439. doi: 10.2215/CJN.03681106. [DOI] [PubMed] [Google Scholar]
- Mehta RL, Pascual MT, Soroko S, Chertow GM. Diuretics, mortality, and nonrecovery of renal function in acute renal failure. JAMA. 2002;288:2547–2553. doi: 10.1001/jama.288.20.2547. [DOI] [PubMed] [Google Scholar]
- ARDS NET Investigators. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. N Engl J Med. 2000;342:1301–1308. doi: 10.1056/NEJM200005043421801. [DOI] [PubMed] [Google Scholar]
- Bellomo R, Honore PM, Matson J, Ronco C, Winchester J. Extra-corporeal blood treatment (EBT) methods in SIRS/Sepsis. Int J Artif Organs. 2005;28:450–458. doi: 10.1177/039139880502800505. [DOI] [PubMed] [Google Scholar]
- Honore PM, Joannes-Boyau O. High volume hemofiltration (HVHF) in sepsis: a comprehensive review of rationale, clinical applicability, potential indications and recommendations for future research. Int J Artif Organs. 2004;27:1077–1082. doi: 10.1177/039139880402701211. [DOI] [PubMed] [Google Scholar]
- Cornejo R, Downey P, Castro R, Romero C, Regueira T, Vega J, Castillo L, Andresen M, Dougnac A, Bugedo G, Hernandez G. High-volume hemofiltration as salvage therapy in severe hyperdynamic septic shock. Intensive Care Med. 2006;32:713–722. doi: 10.1007/s00134-006-0118-5. [DOI] [PubMed] [Google Scholar]
- Honore PM, Jamez J, Wauthier M, Lee PA, Dugernier T, Pirenne B, Hanique G, Matson JR. Prospective evaluation of short-term, high-volume isovolemic hemofiltration on the hemodynamic course and outcome in patients with intractable circulatory failure resulting from septic shock. Crit Care Med. 2000;28:3581–3587. doi: 10.1097/00003246-200011000-00001. [DOI] [PubMed] [Google Scholar]
- Joannes-Boyau O, Rapaport S, Bazin R, Fleureau C, Janvier G. Impact of high volume hemofiltration on hemodynamic disturbance and outcome during septic shock. Asaio J. 2004;50:102–109. doi: 10.1097/01.MAT.0000104846.27116.EA. [DOI] [PubMed] [Google Scholar]
- Bagshaw SM, Brophy PD, Cruz D, Ronco C. Fluid balance as a biomarker: impact of fluid overload on outcome in critically ill patients with acute kidney injury. Crit Care. 2008;12:169. doi: 10.1186/cc6948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alsous F, Khamiees M, DeGirolamo A, Amoateng-Adjepong Y, Manthous CA. Negative fluid balance predicts survival in patients with septic shock: a retrospective pilot study. Chest. 2000;117:1749–1754. doi: 10.1378/chest.117.6.1749. [DOI] [PubMed] [Google Scholar]
- Payen D, de Pont AC, Sakr Y, Spies C, Reinhart K, Vincent JL. A positive fluid balance is associated with a worse outcome in patients with acute renal failure. Crit Care. 2008;12:R74. doi: 10.1186/cc6916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakr Y, Vincent JL, Reinhart K, Groeneveld J, Michalopoulos A, Sprung CL, Artigas A, Ranieri VM. High tidal volume and positive fluid balance are associated with worse outcome in acute lung injury. Chest. 2005;128:3098–3108. doi: 10.1378/chest.128.5.3098. [DOI] [PubMed] [Google Scholar]
- Upadya A, Tilluckdharry L, Muralidharan V, Amoateng-Adjepong Y, Manthous CA. Fluid balance and weaning outcomes. Intensive Care Med. 2005;31:1643–1647. doi: 10.1007/s00134-005-2801-3. [DOI] [PubMed] [Google Scholar]
- Wiedemann HP, Wheeler AP, Bernard GR, Thompson BT, Hayden D, deBoisblanc B, Connors AF Jr, Hite RD, Harabin AL. Comparison of two fluid-management strategies in acute lung injury. N Engl J Med. 2006;354:2564–2575. doi: 10.1056/NEJMoa062200. [DOI] [PubMed] [Google Scholar]
- Brandstrup B, Tønnesen H, Beier-Holgersen R, Hjortsø E, Ørding H, Lindorff-Larsen K, Rasmussen MS, Lanng C, Wallin L, Iversen LH, Gramkow CS, Okholm M, Blemmer T, Svendsen PE, Rottensten HH, Thage B, Riis J, Jeppesen IS, Teilum D, Christensen AM, Graungaard B, Pott F. Danish Study Group on Perioperative Fluid Therapy. Effects of intravenous fluid restriction on postoperative complications: comparison of two perioperative fluid regimens: a randomized assessor-blinded multicenter trial. Ann Surg. 2003;238:641–648. doi: 10.1097/01.sla.0000094387.50865.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillespie RS, Seidel K, Symons JM. Effect of fluid overload and dose of replacement fluid on survival in hemofiltration. Pediatr Nephrol. 2004;19:1394–1399. doi: 10.1007/s00467-004-1655-1. [DOI] [PubMed] [Google Scholar]
- Goldstein SL, Currier H, Graf C, Cosio CC, Brewer ED, Sachdeva R. Outcome in children receiving continuous ven-ovenous hemofiltration. Pediatrics. 2001;107:1309–1312. doi: 10.1542/peds.107.6.1309. [DOI] [PubMed] [Google Scholar]
- Goldstein SL, Somers MJ, Baum MA, Symons JM, Brophy PD, Blowey D, Bunchman TE, Baker C, Mottes T, McAfee N, Barnett J, Morrison G, Rogers K, Fortenberry JD. Pediatric patients with multi-organ dysfunction syndrome receiving continuous renal replacement therapy. Kidney Int. 2005;67:653–658. doi: 10.1111/j.1523-1755.2005.67121.x. [DOI] [PubMed] [Google Scholar]
- Holubek WJ, Hoffman RS, Goldfarb DS, Nelson LS. Use of hemodialysis and hemoperfusion in poisoned patients. Kidney Int. 2008;74:1327–1334. doi: 10.1038/ki.2008.462. [DOI] [PubMed] [Google Scholar]
- Imai Y, Parodo J, Kajikawa O, de Perrot M, Fischer S, Edwards V, Cutz E, Liu M, Keshavjee S, Martin TR, Marshall JC, Ranieri VM, Slutsky AS. Injurious mechanical ventilation and end-organ epithelial cell apoptosis and organ dysfunction in an experimental model of acute respiratory distress syndrome. JAMA. 2003;289:2104–2112. doi: 10.1001/jama.289.16.2104. [DOI] [PubMed] [Google Scholar]
- Ranieri VM, Giunta F, Suter PM, Slutsky AS. Mechanical ventilation as a mediator of multisystem organ failure in acute respiratory distress syndrome. JAMA. 2000;284:43–44. doi: 10.1001/jama.284.1.43. [DOI] [PubMed] [Google Scholar]
- Bagshaw SM, Gibney RT. Conventional markers of kidney function. Crit Care Med. 2008;36:S152–158. doi: 10.1097/CCM.0b013e318168c613. [DOI] [PubMed] [Google Scholar]
- Coca SG, Yalavarthy R, Concato J, Parikh CR. Biomarkers for the diagnosis and risk stratification of acute kidney injury: a systematic review. Kidney Int. 2008;73:1008–1016. doi: 10.1038/sj.ki.5002729. [DOI] [PubMed] [Google Scholar]