Abstract
Background:
We hypothesized that the incidence of ureteral abnormalities on frozen section analysis (FS) at the time of radical cystectomy is much lower than historical values and that FS has minimal impact on outcomes. We also sought to determine the accuracy of FS and the associated costs.
Methods:
We reviewed the records of 301 patients who underwent a radical cystectomy for urothelial carcinoma of the bladder (UC) between March 2000 and January 2007. The ureteral margins were sent for FS and subsequent permanent hematoxyllin and eosin (H&E) sections and results were compared. Analyses were performed to determine the costs of FS and if any association was present with the pathological stage of the primary bladder tumour and regional lymph nodes, the presence of urothelial carcinoma in situ of the bladder (CIS) and survival outcomes with the FS.
Results:
We identified 602 ureters for this study. The incidence of CIS or solid urothelial carcinoma in the ureter was 2.8%. The presence of CIS of the bladder and prostatic urethra was significantly associated with a positive FS (p = 0.02). The FS were not associated with survival outcomes. The cost to pick up 1 patient with any abnormality on FS was $2080. The cost to pick up 1 patient with CIS or solid urothelial carcinoma of the ureter on FS was $6471.
Conclusion:
The incidence of CIS and tumour on FS during radical cystectomy for UC is low. The costs associated with FS are substantial. Frozen section analysis should only be performed in select patients undergoing radical cystectomy.
Résumé
Contexte :
Nous avons avancé l’hypothèse que la fréquence des anomalies urétérales notées par analyse de coupes congelées (CC) lors d’une cystectomie radicale est beaucoup plus basse que les valeurs historiques, et que l’analyse des CC a un impact minimal sur l’issue thérapeutique. Nous avons cherché à déterminer l’exactitude de l’analyse des CC et les coûts qui y sont associés.
Méthodologie :
Nous avons examiné les dossiers de 301 patients ayant subi une cystectomie radicale en raison d’un carcinome urothélial de la vessie entre mars 2000 et janvier 2007. Les marges urétérales avaient été envoyées pour une analyse des CC et une épreuve subséquente de coloration permanente à l’hématoxyline et à l’éosine; les résultats ont ensuite été comparés. Ces analyses ont été menées en vue de déterminer les coûts de l’analyse des CC et de vérifier la présence de tout lien entre les résultats de l’analyse des CC et le stade pathologique de la tumeur vésicale primitive, l’atteinte des ganglions lymphatiques régionaux, la présence d’un carcinome urothélial in situ de la vessie et les taux de survie.
Résultats :
Nous avons examiné des coupes de 602 uretères pour cette étude. La fréquence de carcinomes urothéliaux in situ ou de carcinomes urothéliaux (tumeurs solides) dans l’uretère était de 2,8 %. La présence d’un carcinome in situ de la vessie et de l’urètre prostatique a été associée de façon significative à des résultats positifs à l’analyse des CC (p = 0.02), mais aucune corrélation n’a été dégagée entre l’analyse des CC et les taux de survie. Les coûts engagés pour cerner un patient présentant une anomalie lors de l’analyse des CC étaient de 2080 $, alors que les coûts engagés pour cerner un patient présentant un carcinome in situ ou un carcinome urothélial solide de l’uretère étaient de 6471 $.
Conclusion :
L’incidence des carcinomes in situ et des tumeurs solides déterminées par analyse des CC lors d’une cystectomie radicale en raison d’un carcinome urothélial est faible, et les coûts associés à une analyse des CC sont considérables. Une telle analyse des coupes congelées ne devrait donc pas être effectuée pour tous les patients subissant une cystectomie radicale, mais dans certains cas précis seulement.
Introduction
Frozen section analysis (FS) of the ureteral margin has been performed routinely at many centres, including our own, at the time of radical cystectomy for urothelial carcinoma of the bladder (UC). This practice had been based on historical data indicating that advanced UC is associated with atypia, urothelial carcinoma in situ (CIS) and solid urothelial carcinoma at the ureteral margin at the time of radical cystectomy. The rate of CIS in the distal ureters at the time of radical cystectomy has ranged from 8.5% to 33%.1–3 The justification for FS was to ensure a cancer-free anastomosis, which theoretically should translate into fewer upper tract recurrences, local recurrences at the ureteral-intestinal anastomosis and improved disease-free and disease-specific survival. However, controversy remains about whether FS achieves these goals. We hypothesized that the incidence of ureteral abnormalities on FS at the time of radical cystectomy is much lower than historical values and that FS has minimal impact on the natural history of the UC post-radical cystectomy. We also sought to determine the accuracy of FS and the associated costs.
Methods
We reviewed the records of 301 patients who underwent a radical cystectomy at the London Health Sciences Centre-Victoria Hospital between March 2000 and January 2007. Patients undergoing prior pelvic radiotherapy were excluded. All patients underwent preoperative computed tomography (CT) of the abdomen and pelvis and chest roengenography; a bone scan was performed infrequently for staging. Upper urinary tract disease was assessed with CT and/or intravenous pyelography and/or retrograde pyelography. The distal ends of the ureters were sent for FS and later embedded in paraffin for subsequent permanent H&E sections. If the distal ureteral segment was positive for malignancy or demonstrated atypia or dysplasia, another segment of distal ureter was excised for FS. Carcinoma in situ continued to be identified with further ureteral resections and FS, which resulted in 3 patients who eventually underwent a nephroureterectomy during the cystectomy. Step-sectioning was later performed and the FS was compared to the permanent H&E section findings. The permanent section findings were described as normal, atypia, CIS or solid urothelial carcinoma.
The histopathological results were studied to determine if any association was present with the pathological stage of the primary bladder tumour and regional lymph nodes, the presence of CIS in the bladder or prostatic urethra and survival outcomes with the FS results. An ANOVA two-way factor statistical analysis was performed to determine if any possible association existed that was statistically significant. A p-value of less than 0.05 was considered statistically significant. Final pathology was reported according to the TNM classification of 1997. The costs, in Canadian dollars, associated with FS analysis were also evaluated. The cost included direct costs, including all costs incurred in the Department of Pathology, and indirect costs, including all other hospital-related costs, such as Human Resources Department, Materials Management, Information Systems, and Plant and Operations.
Results
A total of 301 patients and 602 ureters were identified for this study. There were a total of 362 ureters analyzed by FS. Some ureters were excluded from FS (Table 1). The incidence of any abnormality on FS is 9.9%. The incidence of CIS or solid urothelial carcinoma in the ureter is even lower at 2.8% (Table 2). The sensitivity was 71.9%, specificity 96.1%, positive predictive value 63.9% and negative predictive value 97.2% (Table 3).
Table 1.
Ureters excluded from frozen section analysis
| Reason for exclusion | No. of ureters |
|---|---|
| Non-oncologic reasons for cystectomy | 14 |
| Non-urothelial carcinoma of the bladder | 16 |
| Previous nephroureterectomy | 6 |
| Concomitant nephroureterectomy | 3 |
| Ureters not analyzed by frozen section (e.g., prior pelvic radiotherapy, surgeon did not do routine frozen section analysis) | 201 |
Table 2.
Incidence of atypia, dysplasia or urothelial carcinoma in situ or solid urothelial carcinoma
| Frozen section negative |
Frozen section positive |
|
|---|---|---|
| Atypia/dysplasia | CIS/UC | |
| 326 | 26 | 10 |
CIS = carcinoma in situ; UC = urethral carcinoma of the bladder.
Table 3.
Reliability of frozen section analysis
| Frozen section analysis |
Permanent section |
|
|---|---|---|
| Postive | Negative | |
| Positive | 23 | 13 |
| Negative | 9 | 317 |
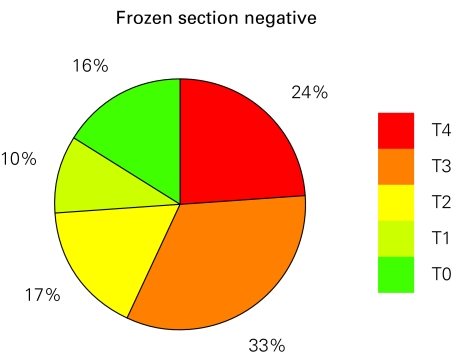
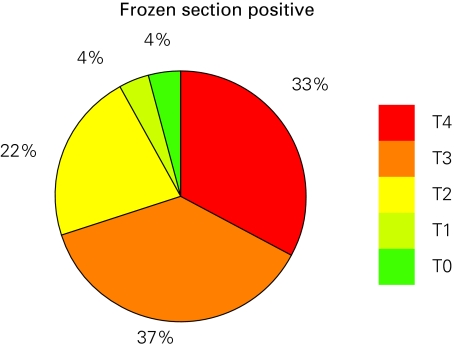
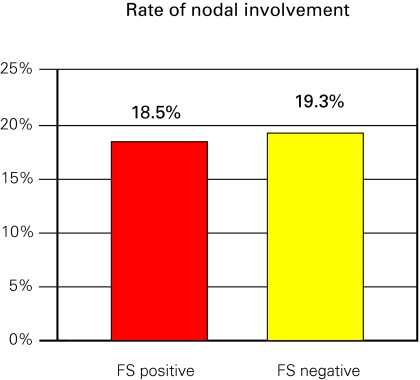
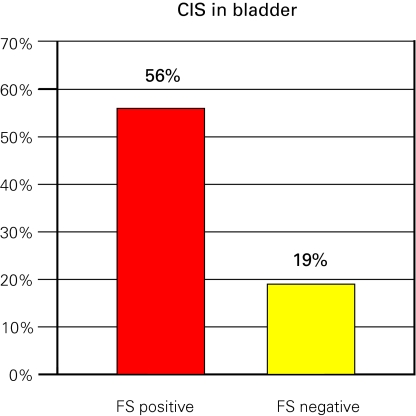
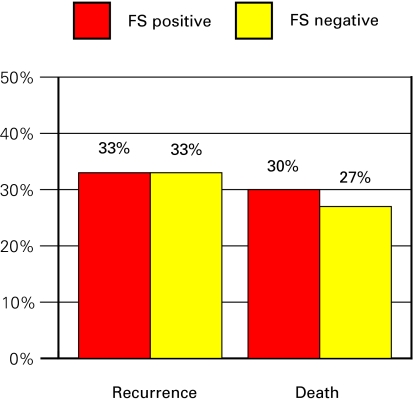
Pathologic stage of the primary bladder tumour did not predict for a positive FS (Fig. 1). Furthermore, the status of the regional lymph nodes did not predict for a positive FS (Fig. 2). However, the presence of CIS of the bladder or prostatic urethra was significantly associated with a positive FS, p < 0.02 (Fig. 3). Results of the FS were not associated with survival outcomes (Fig. 4).
Fig. 1.
The ureteral frozen section results were not associated with the pathologic stage of the primary bladder tumour.
Fig. 2.
The frozen section (FS) results were not associated with regional lymph node metastases.
Fig. 3.
A positive frozen section (FS) was associated with the presence of urothelial carcinoma in situ (CIS) in the bladder and/or prostatic urethra (p < 0.02).
Fig. 4.
A positive frozen section (FS) was not associated with disease-specific or overall survival with a mean follow-up of 31.3 months.
Upper urinary tract recurrence occurred in 6 patients (2%). These recurrences were all more proximal than the ureteral-intestinal anastomoses. Four of these patients had a negative FS. Two patients did not have FS analysis performed. One patient had a positive FS and subsequent further resections into the mid-ureter were also positive of FS and a nephroureterectomy was performed. The mean follow-up was 31.3 months.
Twenty-eight different patients demonstrated either atypia, CIS or solid tumour on FS and 9 patients demonstrated CIS or solid urothelial carcinoma of the ureter out of the 180 tested. The costs for a sending a section of the distal ureter for FS and permanent sections are listed in Table 4. The cost to pick up 1 patient with any abnormality on FS was $2080. The cost to pick up 1 patient with CIS or solid urothelial carcinoma of the ureter on FS was $6471.
Table 4.
Direct and indirect costs of frozen section analysis and hematoxyllin and eosin stained permanent sections
| Description | Direct cost | Indirect cost | Total |
|---|---|---|---|
| FS Block Freeze | $3.73 | $0.90 | $4.63 |
| FS Case Setup | $19.06 | $5.39 | $24.45 |
| FS Cut & HE | $14.46 | $4.04 | $18.50 |
| FS Cut Slide | $3.73 | $0.90 | $4.63 |
| FS Cut, Stain Extra HE | $11.40 | $3.14 | $14.54 |
| FS Embed & HE | $7.57 | $2.02 | $9.59 |
| Final Pathology Report | $188.32 | $58.89 | $247.21 |
| Total | $248.27 | $75.28 | $323.55 |
Direct costs involved the Department of Pathology budget. Indirect costs involved corporate overhead (Human Resources Department, Materials Management, Information Systems and Plant & Operations).
FS = frozen section analysis; HE = hematoxyllin and eosin staining.
Discussion
The incidence of upper tract recurrence after radical cystectomy is low ranging from 2% to 8.7% (Table 5). Risk factors for upper urinary tract recurrence have been established as: history of diffuse CIS, multifocal tumour, intramural ureteral involvement with CIS, prior ureteral tumour, prostatic involvement and urethral involvement.4–7 The ureteral FS does not appear to add any independent predictive ability over these established factors for future upper urinary tract recurrences. In addition, with its low positive predictive value, FS has a tendency to overestimate disease at the ureteral margin.
Table 5.
Rates of urothelial carcinoma in situ of the ureteral margin submitted for frozen section and hematoxyllin and eosin stained permanent sections
| Reference | No. of patients | % Ureteral FS positive for CIS | % Final HE positive for CIS |
|---|---|---|---|
| Johnson et al.4 | 403 | 2 | n/a |
| Schoenberg et al.5 | 97 | 8 | n/a |
| Silver et al.6 | 401 | 6.2 | 3.7 |
| Schumacher et al.8 | 805 | 4.8 | 3.6 |
| Culp et al.9 | 231 | 6 | n/a |
| Sharma et al.10 | 205 | 8.5 | n/a |
| Linker et al.11 | 107 | 8.7 | n/a |
| Herr et al.12 | 105 | n/a | 29 |
| Batista et al.13 | 242 | 5.7 | n/a |
| Raj et al.14 | 1330 | 6 | n/a |
FS = frozen section analysis; CIS = carcinoma in situ; HE = hematoxyllin and eosin staining.
Furthermore, FS at the time of cystectomy also remains controversial in terms of its ability to enhance the prevention of upper urinary tract recurrences. The pagetoid spread of CIS makes it impossible to guarantee that a negative FS ensures that CIS is not more proximal. One study confirmed that the incidence of upper tract recurrence is higher if the initial FS was positive for CIS (16.7% vs. 2.9%).8 However, in this study by Schumacher and colleagues, the ureter was resected more proximally at the bifurcation of the common iliac vessels, which suggests that if one does perform a ureteral FS at the time of radical cystectomy, then performing the ureteral margin at the level of the iliac vessels may be of benefit.8 Other studies that have addressed the value of FS at the time of radical cystectomy question the value of this strategy in tailoring the intraoperative procedure, as segmental sectioning of the ureter until only normal urothelium is identified does not eliminate the risk of anastomotic or upper tract recurrences nor does it seem to affect survival outcomes.5,12,14
The potential shortfalls of this study were its retrospective study design, the fact that a significant number of ureters were not examined and the lack of uniformity in the management of positive frozen sections (i.e., some patients with dysplasia/ atypia were implanted without further resection). These factors would lead to selection bias. The strengths of this study are that this is one of the larger series examining FS at the time of radical cystectomy, one of the only studies to examine the sensitivity and specificity of FS of the ureters and the first to examine both the direct and indirect costs related to FS.
These data further indicate that the incidence of a ureteral abnormality and malignancy at the ureteral margin is very low in a contemporary series. The decreased incidence observed may be secondary to improved imaging of the upper tract with CT urography and better ureteroscopic instrumentation and techniques. These data also support the use of ureteral FS in patients with CIS of the bladder and/or prostatic urethra. When other risk factors associated with an increased risk for upper tract recurrences are present, such as multifocal tumour, intramural ureteral involvement with CIS, prior ureteral tumour and prostatic or urethral involvement of UC,4–7 one may also consider ureteral FS at the time of radical cystectomy. This would certainly mitigate the significant direct and indirect costs associated with FS and would not appear to place the patients at significant risk for more upper urinary tract recurrences, problems at the ureteral-intestinal anastomosis or worse survival outcomes.
Conclusion
The incidence of CIS and tumour on FS during radical cystectomy for UC is low. Frozen section analysis has the tendency to overestimate disease at the ureteral margin. Carcinoma in situ in the bladder or prostatic urethra constitutes a predictor of a positive FS. There appears to be no difference in disease recurrence or death between patients with negative or positive FS. The costs associated with FS are substantial and should be considered given the questionable clinical value of this test. Therefore, FS should be performed in select patients undergoing radical cystectomy in the following circumstances: where CIS is present in the bladder, intramural ureter or prostate; where there is multifocal tumour, prior ureteral tumour and prostatic stromal; or where there is urethral involvement of UC.
Footnotes
Competing interests: None declared.
This paper has been peer-reviewed.
References
- 1.Sharma TC, Melamed MR, Whitmore WF., Jr Carcinoma in-situ of the ureter in patients with bladder carcinoma treated by cystectomy. Cancer. 1970;26:583–7. doi: 10.1002/1097-0142(197009)26:3<583::aid-cncr2820260313>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 2.Cooper PH, Waisman J, Johnston WH, et al. Severe atypia of transitional epithelium and carcinoma of the urinary bladder. Cancer. 1973;31:1055–60. doi: 10.1002/1097-0142(197305)31:5<1055::aid-cncr2820310503>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 3.Schade RO, Turingen, Serck-Hannson A, et al. Morphological changes in the ureter in cases of bladder carcinoma. Cancer. 1971;27:1267–72. doi: 10.1002/1097-0142(197105)27:5<1267::aid-cncr2820270535>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 4.Johnson DE, Wishnow KI, Tenney D. Are frozen- section examinations of ureteral margins required for all patients undergoing radical cystectomy for bladder cancer? Urology. 1989;33:451–4. doi: 10.1016/0090-4295(89)90127-1. [DOI] [PubMed] [Google Scholar]
- 5.Schoenberg MP, Carter HB, Epstein JI. Ureteral frozen section analysis during cystectomy: a reassessment. J Urol. 1996;155:1218–20. [PubMed] [Google Scholar]
- 6.Silver DA, Stroumbakis N, Russo P, et al. Ureteral carcinoma in situ at radical cystectomy: does the margin matter? J Urol. 1997;158:768–71. doi: 10.1097/00005392-199709000-00020. [DOI] [PubMed] [Google Scholar]
- 7.Sanderson KM, Cai J, Miranda G, et al. Upper tract urothelial recurrence following radical cystectomy for transitional cell carcinoma of the bladder: an analysis of 1,069 patients with 10-year followup. J Urol. 2007;177:2088–94. doi: 10.1016/j.juro.2007.01.133. [DOI] [PubMed] [Google Scholar]
- 8.Schumacher MC, Scholz M, Weise EK, et al. Is there an indication for frozen section examination of the ureteral margins during cystectomy for transitional cell carcinoma of the bladder. J Urol. 2006;176:2409–13. doi: 10.1016/j.juro.2006.07.162. [DOI] [PubMed] [Google Scholar]
- 9.Culp OS, Utz DC, Harrison EG., Jr Experiences with ureteral carcinoma in situ detected during operations for vesical neoplasm. J Urol. 1967;97:679–82. doi: 10.1016/S0022-5347(17)63097-0. [DOI] [PubMed] [Google Scholar]
- 10.Sharma TC, Melamed MR, Whitmore WF., Jr Carcinoma in situ of the ureter in patients treated with cystectomy. Cancer. 1970;26:583–7. doi: 10.1002/1097-0142(197009)26:3<583::aid-cncr2820260313>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 11.Linker DG, Whitmore WF. Ureteral carcinoma in situ. J Urol. 1975;113:777–80. doi: 10.1016/s0022-5347(17)59579-8. [DOI] [PubMed] [Google Scholar]
- 12.Herr H, Whitmore WF., Jr Ureteral carcinoma in situ after successful intravesical therapy for superficial bladder tumors: incidence, possible pathogenesis and management. J Urol. 1987;138:292–4. doi: 10.1016/s0022-5347(17)43123-5. [DOI] [PubMed] [Google Scholar]
- 13.Batista JE, Palou J, Iglesias J, et al. Significance of ureteral carcinoma in situ in specimens of cystectomy. Eur Urol. 1994;25:313–5. doi: 10.1159/000475308. [DOI] [PubMed] [Google Scholar]
- 14.Raj GV, Tal R, Vickers A, et al. Significance of intraoperative ureteral evaluation at radical cystectomy for urothelial cancer. Cancer. 2006;107:2167–72. doi: 10.1002/cncr.22238. [DOI] [PubMed] [Google Scholar]