Abstract
In the current study, we investigated the activity of lipopolysaccharide (LPS) purified from Yersinia pestis grown at either 27°C or 37°C (termed LPS-27 and LPS-37, respectively). LPS-27 containing hexa-acylated lipid A, similar to the LPS present in usual gram-negative bacteria, stimulated an inflammatory response in human U937 cells through Toll-like receptor 4 (TLR4). LPS-37, which did not contain hexa-acylated lipid A, exhibited strong antagonistic activity to the TLR4-mediated inflammatory response. The phagocytic activity in the cells was not affected by LPS-37. To estimate the activity of LPS in its bacterial binding form, formalin-killed bacteria (FKB) were prepared from Y. pestis cells grown at 27°C or 37°C (termed FKB-27 and FKB-37, respectively). FKB-27 strongly stimulated the inflammatory response. This activity was suppressed in the presence of an anti-TLR4 antibody but not an anti-TLR2 antibody. In addition, this activity was almost completely suppressed by LPS-37, indicating that the activity of FKB-27 is predominantly derived from the LPS-27 bacterial binding form. In contrast, FKB-37 showed no antagonistic activity. The results arising from the current study indicate that Y. pestis causes infection in humans without stimulating the TLR4-based defense system via bacterial binding of LPS-37, even when bacterial free LPS-37 is not released to suppress the defense system. This is in contrast to the findings for bacteria that possess agonistic LPS types, which are easily recognized by the defense system via the bacterial binding forms.
Yersinia pestis is the causative agent of bubonic, septicemic, and pneumonic plague in humans and is primarily a rodent pathogen that is transmitted intradermally to humans through the bite of an infected flea (24). Y. pestis must survive in two different temperature ranges. One temperature range represents that of a flea residing in rodent burrows or mammalian hair (21°C to 28°C), while the other represents the body temperature of the infected rodent or human (37°C to 41°C) (2, 4, 24). It has been demonstrated that the various cellular components of this bacterium are differentially expressed at these temperature ranges. The production of several virulent factors, such as the fraction 1 antigen (6), the pH 6 antigen (14), and Yop proteins (33), are known to be upregulated during growth of the bacterium at 37°C. In contrast, the production of murine toxin (12), which is required for the survival of Y. pestis in the midgut of fleas, is synthesized at approximately 27°C and is downregulated at 37°C.
Y. pestis is a gram-negative bacterium that contains bacterial lipopolysaccharide (LPS) as its major cell wall component. The lipid moiety in LPS that is responsible for immune system activation is lipid A and is composed of a glucosamine-disaccharide backbone carrying acyl chains and phosphate groups. The hexa-acylated type of lipid A was found to be the major component of the Escherichia coli LPS, which exhibits strong immunological activities (8, 13, 17). This particular type of lipid A is widely found among usual gram-negative bacteria, but it is not the sole type of lipid A species. The specific types of lipid A have been shown to differ among bacterial species, and heterogeneous types of lipid A often coexist in a single species (28). We have previously reported that the lipid A present in Y. pestis LPS is heterogeneous (from hexa-acylated to triacylated types) when the bacterium is grown at 27°C and shifts to the hypoacylated types (tetra- and triacylated types) when it is grown at 37°C (16). Such a temperature-dependent shift of lipid A types in the LPS of Y. pestis was further confirmed by another group (29), who demonstrated a similar shift in two additional pathogenic species of Yersinia. Hexa-acylated lipid A is able to strongly activate Toll-like receptor 4 (TLR4), while the tetra-acylated type is a poor activator and serves instead as an antagonist when the target cells are human in origin (10, 22). The alteration of lipid A to hypoacylated types is therefore favorable for the bacterium, as it allows the bacterium to evade the human innate immune system and avoid elimination. It has been indicated that lipid A alterations that result in the evasion of the bacteria from host TLR4 recognition play a more important pathogenic role than the additional virulence factors of Y. pestis (23).
In the current study, we purified LPS or prepared formalin-killed bacteria (FKB) from Y. pestis grown at either 27°C or 37°C and examined their influence on the immune system response in human U937 cells. Our findings suggested that the LPS isolated from Y. pestis grown at 37°C (LPS-37) strongly suppressed the human TLR4-dependent inflammatory response when it was free from the bacterial body. This suppressive activity was not observed when it was bound to the bacterial body. In contrast, the LPS isolated from Y. pestis grown at 27°C (LPS-27) was found to be agonistic toward TLR4 signaling in both the bacterium-free and -bound forms, as FKB grown at 27°C (FKB-27) showed agonistic activity similar to that of LPS-27.
MATERIALS AND METHODS
Bacterial culture, extraction of LPS, and preparation of FKB.
Virulent Y. pestis strain Yreka (National Institute of Infectious Disease, Tokyo, Japan) was cultured on brain heart infusion agar (Difco Laboratories, Detroit, MI) at 27°C or 37°C for 48 h. The bacterial cells were suspended in saline to obtain heat-killed bacteria for the extraction of LPS by the method reported previously (16) and were purified via extraction with 45% phenol containing triethylamine and sodium deoxycholate (21). The LPS forms obtained following growth at 27°C and 37°C were termed LPS-27 and LPS-37, respectively. To prepare FKB, bacterial cells were suspended in 0.3% formalin solution at a dose of 30 mg (wet weight)/ml (9 × 109 bacteria/ml) and were incubated at 37°C with shaking for 5 days to kill the bacteria completely. These preparations, termed FKB-27 and FKB-37, respectively, were then washed and suspended in phosphate-buffered saline.
Cell culture.
The murine macrophage cell line RAW264.7 and the human macrophage cell line U937 (both from the American Type Culture Collection, Manassas, VA) were used in the current study. To obtain mouse peritoneal exudate cells (PECs), 7- to 8-week-old C3H/HeN or C3H/HeJ mice (Japan Charles River, Tokyo, Japan) were injected intraperitoneally with 2 ml of thioglycolate broth (Difco Laboratories). PECs were then obtained 4 days later by peritoneal lavage. All animal experiments were carried out according to the guidelines of the Laboratory Animal Center, Jichi Medical University. The complete medium (CM) used for cell culture was composed of RPMI 1640 medium (ICN Biomedicals, Inc., Aurora, OH) supplemented with 2 mM l-glutamine, 100 U/ml penicillin, 100 μg/ml streptomycin, 0.2% NaHCO3, and 10% heat-inactivated fetal bovine serum (FBS; Flow Laboratories Inc., Rockville, MD). The cells were cultured in a humidified chamber at 37°C with 5% CO2 and 95% air. RAW264.7 cells and PECs suspended in CM at 1 × 106 cells/ml were cultured overnight, and the adherent cells were used in all experiments. U937 cells were suspended in CM supplemented with 100 nM phorbol myristate acetate (PMA; Sigma-Aldrich Co., St. Louis, MO) at a cell density of 5 × 105/ml and were cultured for 3 days to induce differentiation into macrophage-like cells. Only the adherent cells were used in the current study.
Cytokine assay.
RAW264.7 and U937 cells were cultured in 24-well culture plates (500 μl/well; Corning Inc., Corning, NY) and were stimulated with various LPSs, TLR ligands, and FKB. LPS purified from Salmonella enterica serovar Abortus-Equi (7) was a kind gift from C. Galanos (MIP für Immunbiology, Freiburg, Germany) and was used as a reference for the TLR4 ligand. Pam3-Cys-Ser-(Lys)4 hydrochloride (Pam3-Cys), purchased from Calbiochem, EMD Bioscience, Inc. (San Diego, CA), was used as a TLR2 ligand; and flagellin (S. enterica serovar Typhimurium), purchased from InvivoGen (San Diego, CA), was used as a TLR5 ligand. The culture supernatant obtained 6 h after stimulation was assayed for mouse and human cytokines by a specific sandwich enzyme-linked immunosorbent assay (ELISA). The ELISA was performed according to the instructions supplied by Endogen (Woburn, MA) and by using matched antibody pairs. Each cytokine was quantified (in ng/ml or pg/ml) on the basis of the standard curve obtained in each assay. In the suppression experiments, anti-human TLR4/CD284 (anti-TLR4 antibody; MBL Co., Ltd., Nagoya, Japan) (1), anti-human CD282 (TLR2) (anti-TLR2 antibody; BD Pharmingen, Franklin Lakes, NJ) (19), and a human TLR4 antagonist, compound 406 (Daiichi Kagaku Co., Tokyo, Japan) (10, 22), were used as suppressors. Cells were stimulated in the presence of suppressors (added 1 h prior to stimulation), and the culture supernatant was assayed 6 h after stimulation.
Detection of cytokine mRNA by RT-PCR.
U937 cells were cultured in 60-mm culture dishes (Corning Inc.) containing 3 ml of medium and were stimulated with LPS or Pam3-Cys for 2 h in the presence or the absence of LPS-37. Total RNA was then extracted by using Isogen (Nippon Gene Co., Ltd., Tokyo, Japan). One microgram of total RNA was reverse transcribed by using SuperScript II reverse transcriptase (RT; Invitrogen Co., Carlsbad, CA). Aliquots of cDNA equivalent to 50 ng of RNA for the following genes were subsequently amplified by using the indicated primers (3, 5): for human tumor necrosis factor alpha (TNF-α), sense primer 5′-AGA GGG AAG AGT TCC CCA GGG AC-3′ and antisense primer 5′-TGA GTC GGT CAC CCT TCT CCA G-3′; for human interleukin-1β (IL-1β), sense primer 5′-CCA GCT ACG AAT CTC GGA CCA CC-3′ and antisense primer 5′-TTA GGA AGA CAC AAA TTG CAT GGT GAA GTC AGT-3′; for human IL-6, sense primer 5′-ATG AAC TCC TTC TCC ACA AGC GC-3′ and antisense primer 5′-GAA GAG CCC TCA GGC TGG ACT G-3′; for human IL-8, sense primer 5′-ATG ACT TCC AAG CTG GCC GTG-3′ and antisense primer 5′-TTA TGA ATT CTC AGC CCT CTT CAA AAA CTT CTC-3′; for human IL-10, sense primer 5′-ATG CCC CAA GCT GAG AAC CAA GAC CCA-3′ and antisense primer 5′-TCT CAA GGG GCT GGG TCA GCT ATC CCA-3′; for human IL-12p40, sense primer 5′-AGA GGC TCT TCT GAC CCC CAG-3′ and antisense primer 5′-CTC TTG CTC TTG CCC TGG ACC TG-3′; and for human GAPDH, sense primer 5′-TGA AGG TCG GAG TCA ACG GAT TTG GT-3′ and antisense primer 5′-CAT GTG GGC CAT GAG GTC CAC CAC-3′. The PCR conditions included an initial denaturation at 94°C for 1 min, followed by 20 to 32 cycles at 94°C for 1 min, 60°C for 1 min, and 72°C for 2 min. Amplification was repeated for 32 cycles for IL-6, IL-10, and IL-12p40; 25 cycles for TNF-α and GAPDH; and 20 cycles for IL-1β and IL-8. The resulting PCR products were separated by electrophoresis on 1.2% agarose gels, and the gels were stained with ethidium bromide.
Phagocytic assay.
U937 cells were cultured in 96-well culture plates (100 μl/well; Corning Inc.) and subjected to phagocytic assays, in accordance with the method described previously (36). Briefly, the cells were cultured for 1 h with cytochalasin D (a phagocytosis inhibitor; Wako Pure Chemical Industries, Ltd., Osaka, Japan), anti-TLR4 antibody, or LPS-37. After removal of the culture supernatant, the cells were cultured for 2 h in the presence of fluorescein-labeled Escherichia coli K-12 BioParticles (Molecular Probes, Inc., Eugene, OR). The culture supernatant containing the particles was then removed, and the remaining extracellular fluorescence was quenched by the addition of trypan blue solution (250 μg/ml, pH 4.4). After incubation at room temperature for 3 min, the dye was discarded and the fluorescence intensity (in relative fluorescence units) associated with the intracellular fluorescent particles was measured at an excitation wavelength of 480 nm and an emission wavelength of 525 nm with a SPECTRAmax M5 microplate fluorometer (Molecular Devices Corp., Sunnyvale, CA).
Estimation of LPS levels.
The LPS levels present in the supernatants of the FKB were measured by using an Endospecy test chromogenic endotoxin-specific assay kit (Seikagaku Co., Tokyo, Japan). Briefly, the test sample solution was combined with the kit reagent in a 96-well microplate and the plate was incubated for 30 min at 37°C. The reaction was then stopped by adding 0.6 M acetic acid, and the color reaction was measured at 405 nm. LPS-27 and LPS-37 were used to construct the standard curves for the calculation of the LPS levels in the supernatants of FKB-27 and FKB-37, respectively.
Statistical analysis.
The significance of any difference between the means for the experimental groups was determined by Student's t test. The means were considered significantly different if P was <0.05.
RESULTS
Cytokine production by mouse and human cells stimulated with Y. pestis LPS-27 and LPS-37.
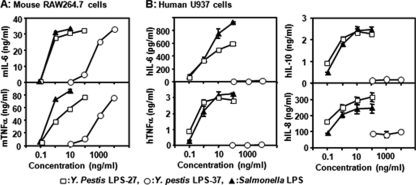
The mouse macrophage cell line RAW264.7 was stimulated with LPS-27, LPS-37, or a reference Salmonella LPS; and the production of cytokines in the stimulated cells was assessed. The stimulation of cells with LPS-27 resulted in the production of both TNF-α and IL-6 when it was administered at a low dose of only 1 ng/ml. The stimulatory activity was similar to that achieved by the reference Salmonella LPS. LPS-37 also had stimulatory activity; however, the stimulation was significantly weaker than that of LPS-27. The activity of LPS-37 administered at 1,000 ng/ml was comparable to that of LPS-27 administered at 1 ng/ml (Fig. 1A). Similar results were also obtained when PECs isolated from C3H/HeN mice were used as target cells. However, the two LPS forms failed to induce cytokine production when PECs isolated from the TLR4 mutant mice (C3H/HeJ) were used as the target cells (data not shown). These results indicate that both LPS preparations function as specific mouse TLR4 agonists and are sufficiently free from detectable contaminants (i.e., they are pure enough) to stimulate the other TLRs.
FIG. 1.
Effects of LPS-27 and LPS-37 isolated from Y. pestis on the stimulation of mouse macrophage RAW264.7 cells and human macrophage U937 cells. (A) Mouse RAW264.7 cells were stimulated with LPS-27, LPS-37, and reference Salmonella LPS at the indicated doses. (B) Human U937 cells were stimulated as described for panel A. The cytokine levels in the culture supernatant at 6 h after stimulation were determined by ELISA. The data are presented as the means ± standard errors of triplicate samples, and a representative result from three independent experiments is shown. h, human; m, mouse.
We next examined the effects of these LPSs in human cells. As shown in Fig. 1B, LPS-27 exhibited strong stimulatory activity in human U937 cells comparable to that of the reference Salmonella LPS. In addition, the dose dependency of LPS-27 for this activity was similar to that for the activation of RAW264.7 cells. In contrast, the activity of LPS-37 in the human cells was remarkably reduced and was undetectable at doses as high as 10 μg/ml. This moderate agonistic activity observed in LPS-37-treated mouse cells and the antagonistic activity observed in treated human cells were similar to the activities observed in cells treated with synthetic tetra-acylated lipid A (compound 406).
Antagonistic activity of LPS-37 to stimulation of TLR4 in human cells.
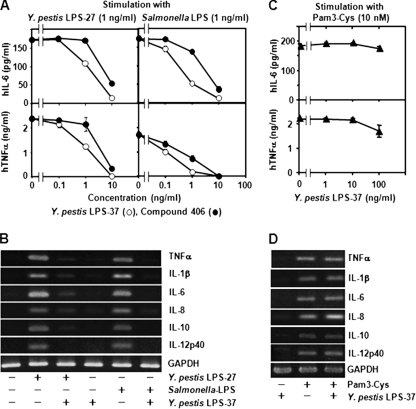
The suppressive effects of LPS-37 on the activation of human cells with various ligands to extracellular TLR were also examined. We used Y. pestis LPS-27 and the reference Salmonella LPS as TLR4 ligands, Pam3-Cys as the TLR2 ligand, and flagellin as the TLR5 ligand. Human U937 cells were stimulated with these agonists in the presence of LPS-37 or compound 406, and cytokine production was assessed. We found that the TLR4-dependent production of cytokines such as TNF-α and IL-6 was strongly suppressed by LPS-37. This result was similar to the response to compound 406 (Fig. 2A). The strong antagonistic activity of LPS-37 against human TLR4 stimulation was confirmed by measuring the levels of expression of various cytokine mRNAs (Fig. 2B). LPS-37 was not observed to have suppressive effects against TLR2-stimulated cytokine production in terms of either protein production or mRNA expression (Fig. 2C and D). Similarly, LPS-37 was not observed to have antagonistic activity against TLR5 stimulation by flagellin (data not shown). These results indicate that LPS-37 acts as a strong antagonist against human TLR4 but not the additional human extracellular TLRs, such as TLR2 and TLR5.
FIG. 2.
Effects of Y. pestis LPS-37 on cytokine production in U937 cells stimulated with TLR4 and TLR2 agonists. (A) U937 cells cultured in the presence of LPS-37 or compound 406 were stimulated with either Y. pestis LPS-27 (1 ng/ml) or Salmonella LPS (1 ng/ml). The cytokine levels in the culture supernatant were determined by ELISA. The data are presented as the means ± standard errors for triplicate samples. (B) U937 cells cultured in the presence of 10 ng/ml LPS-37 were stimulated with 1 ng/ml of LPS-27 or Salmonella LPS. Total RNA was isolated 2 h after stimulation and subjected to RT-PCR for determination of cytokine mRNA expression. PCR products were separated by electrophoresis on 1.2% agarose gels and stained with ethidium bromide. (C) U937 cells cultured in the presence of LPS-37 were stimulated with Pam3-Cys (10 nM), and cytokine production was determined as described for panel A. (D) U937 cells cultured with LPS-37 (10 ng/ml) were stimulated with Pam3-Cys (10 nM), and cytokine mRNA expression was determined as described for panel B. Representative results of three (A and C) or two (B and D) experiments are presented.
Effects of LPS-37 on the phagocytic activity of U937 cells.
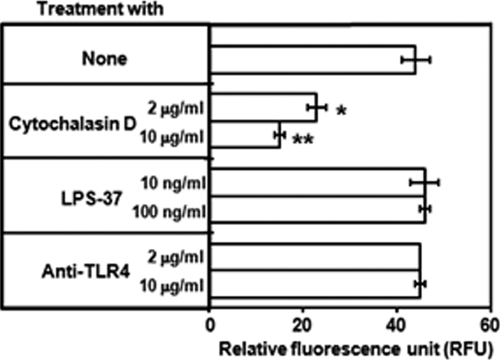
Antiphagocytic factors play an important role in the evasion of bacteria from the host defense network by activating the innate immune system. As LPS-37 strongly suppressed cytokine production on the basis of the host (human) innate immune response, we next investigated the effects of LPS-37 on the phagocytosis of bacteria by U937 cells. The phagocytic activity of U937 cells was assayed with fluorescein-labeled E. coli K-12 BioParticles as the target bacteria, and the fluorescence of the engulfed intracellular bacteria was measured by quenching the fluorescence of the extracellular bacteria with trypan blue. Treatment with LPS-37 or anti-human TLR4 antibody failed to suppress the phagocytic activity in U937 cells, while the addition of cytochalasin D showed a significant suppressive effect (Fig. 3). These results suggest that the suppression of TLR4 signaling by LPS-37 does not affect the role of Y. pestis in the enhancement of resistance to bacterial phagocytes by U937 cells.
FIG. 3.
Effects of LPS-37 on the phagocytosis of bacteria by U937 cells. A total of 5 × 104 U937 cells/well were cultured in 96-well plates in the presence of cytochalasin D, LPS-37, or anti-TLR4 antibody for 1 h. The culture supernatant was then removed, and fluorescein isothiocyanate-labeled E. coli K-12 BioParticles were added at a dose of 5 × 107/well. The cells were cultured for 2 h to phagocytose the E. coli particles and were then treated with trypan blue to quench the extracellular fluorescence. The intensity of the fluorescence associated with intracellular fluorescent particles was then measured with a microplate fluorometer. Intensity is presented as relative fluorescence units. The data presented represent the means from triplicate assays; the error bars indicate ranges and are representative of the results of three experiments. *, P < 0.05 compared to the results for the control, as determined by Student's t test; **, P < 0.01 compared to the results for the control, as determined by Student's t test.
Proinflammatory cytokines produce human cells stimulated with Y. pestis FKB.
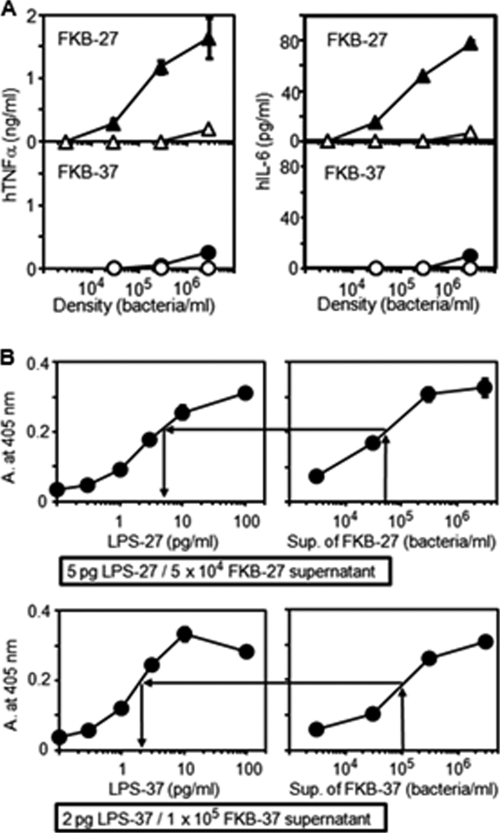
FKB-27 and FKB-37 were prepared by the method used in the production of formalin vaccine, and the ability of these FKB to stimulate cytokine production in U937 cells was investigated. Similar to treatment with LPS, the activity of FKB-27 was found to be strong, while the activity of FKB-37 was very weak, if it was present at all (Fig. 4A). The contribution of the free LPS released from the bacterial body to FKB-27 activity levels was found to be negligible. To estimate the amount of LPS released into the supernatant of the FKB stock suspension, each of the supernatants isolated from the FKB-27- and FKB-37 suspensions was analyzed by the Endospecy test, and the levels were compared to the activity of the corresponding LPS (Fig. 4B). We found that 5 pg of LPS-27 was released from a suspension of 5 × 104 FKB-27 and that 2 pg of LPS-37 was released from a suspension of 1 × 105 FKB-37. These results indicate that the effect of the released LPS on FKB activity was negligible.
FIG. 4.
Stimulation of cytokine production in U937 cells treated with formalin-killed Y. pestis. (A) U937 cells were stimulated with FKB-27 (▴) and FKB-37 (•). The supernatants collected from FKB-27 (Δ) and FKB-37 (○) stock suspensions obtained by centrifugation were also used to stimulate the cells. The cytokine levels in the culture supernatant were determined by ELISA. The data are presented as the means ± standard errors for triplicate samples. A representative result from three independent experiments is shown. (B) The amount of free LPS released from each FKB was estimated by use of an Endospecy test kit. The activity level in each supernatant (Sup.), measured as the absorbance (A.) at 405 nm, was compared to that of the corresponding LPS. Data are presented as the means ± standard errors for duplicate samples. A representative result from two independent experiments is shown.
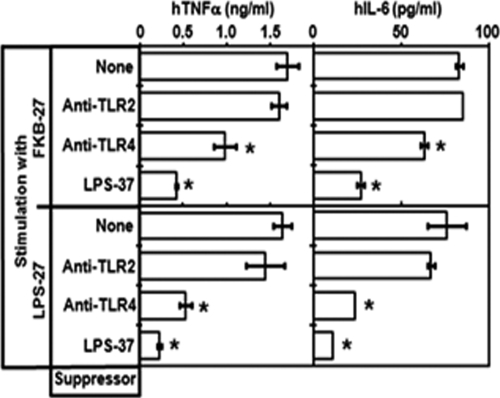
Effects of TLR antibodies and LPS-37 on the activity of FKB-27.
To estimate the contribution of bacterium-bound LPS to the strong FKB-27 activity, we next investigated the effects of anti-TLR4 antibody, anti-TLR2 antibody, and LPS-37 on the activity of FKB-27 that stimulates human U937 cells. As presented in Fig. 5, we found that this activity was significantly suppressed in the presence of both anti-TLR4 antibody and LPS-37 but not in the presence of anti-TLR2 antibody. These findings were similar to the LPS-27 activity responses observed in the presence of antibody or suppressor. These results suggest that the bound form of LPS-27 significantly contributes to the activity of FKB-27.
FIG. 5.
Effects of anti-TLR2 antibody, anti-TLR4 antibody, and LPS-37 on the ability of FKB-27 to stimulate cytokine production in U937 cells. U937 cells were cultured with anti-TLR2 antibody (10 μg/ml), anti-TLR4 antibody (10 μg/ml), or LPS-37 (1 ng/ml) for 1 h; and then FKB-27 (3 × 105/ml) or LPS-27 (1 ng/ml) was added to stimulate the cells. The cytokine levels in the culture supernatants were determined by ELISA. The data are presented as the means ± standard errors for triplicate samples. A representative result from three independent experiments is shown. *, P < 0.05 compared to the results for the control, as determined by Student's t test.
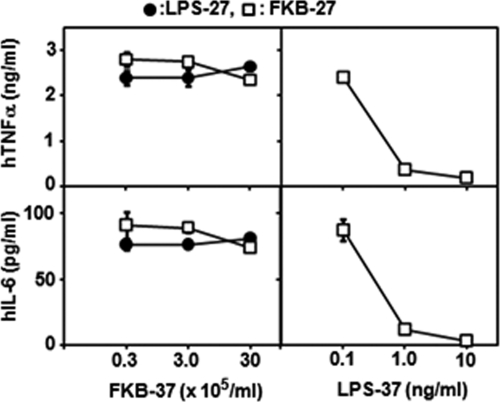
Effects of FKB-37 on cytokine response in U937 cells following TLR4 stimulation.
As the bacterium-free form of LPS-37 showed strong antagonistic activity to human TLR4 stimulation, we next examined whether FKB-37 also demonstrated a similar antagonistic activity. We found that FKB-37 did not exhibit antagonistic activity against the stimulation of human TLR4 in the presence of either LPS-27 or FKB-27. In addition, we also confirmed the strong antagonistic activity of LPS-37 (Fig. 6). In contrast to the bacterium-bound form of LPS-27, the bound form of LPS-37 did not exhibit the level of antagonistic activity observed in its bacterium-free form.
FIG. 6.
Effects of FKB-37 on cytokine production in U937 cells stimulated with FKB-27 or LPS-27 and compared to the effects of LPS-37. U937 cells were stimulated with FKB-27 (□) at 3 × 105/ml or LPS-27 (•) at 1 ng/ml in the presence of FKB-37 or LPS-37 supplemented 1 h prior to stimulation. The cytokine levels in the culture supernatants were determined by ELISA. The data are presented as the means ± standard errors for triplicate samples. A representative result from three independent experiments is shown.
DISCUSSION
In the current study, we demonstrated that purified LPS-37 strongly suppresses proinflammatory cytokine production in human U937 cells stimulated with the TLR4 ligands Salmonella LPS and LPS-27. Activity was clearly observed when these ligands were administered at a dose of 1 ng/ml and reached a maximal level of activity (complete suppression) at approximately 10 ng/ml (Fig. 2). These doses were comparable to those required by Salmonella LPS and LPS-27 to exhibit agonistic activities, indicating that LPS-37 may serve as an antagonist in an infected host at a dose as low as that of an LPS that exhibits endotoxic activity. However, antagonistic activity was observed only when LPS-37 was in its bacterium-free form and not when it was bound to bacteria (FKB-37). Considering the low stimulatory activity of FKB-37 in U937 cells, the failure of Y. pestis LPS-37 to activate the host TLR4 defense system during the early stages of infection may significantly contribute to pathogenesis. Thus, suppression of the TLR4 function may contribute only to the later stages of infection, after bacterial lysis has already occurred.
We thought that it was interesting that the activity of FKB-27 was suppressed in the presence of the anti-TLR4 antibody but not in the presence of the anti-TLR2 antibody. Moreover, the activity was suppressed almost completely by LPS-37, which is a suppressor of TLR4 but not the additional extracellular TLRs, such as TLR2 and TLR5. Considering the relatively low levels of free LPS-27 released from FKB-27, together with the results mentioned above, the activity of FKB-27 may have been predominantly caused by LPS-27 in the form bound to the bacterial body. Similar LPS activity in its bacterium-bound form has not been reported previously. In contrast, FKB-37 did not exhibit antagonistic activity, suggesting that LPS-37 does not exhibit these activities in its bound form but does so in its free form. The human TLR4-based defense system may therefore remain unaffected during the early stages of Y. pestis infection.
Francisella tularensis is a gram-negative bacterium that causes the zoonotic infection tularemia. This bacterial species contains an LPS similar in structure and pathology to those of LPS-37 isolated from Y. pestis. One of the major lipid A molecules present in the LPS isolated from F. tularensis was reported to exhibit a tetra-acylated structure that contained three 3-OH C18 fatty acids, one C16 fatty acid, and one phosphate group (25, 34). We have previously reported that LPS-37 also exhibits a tetra-acylated structure but contains four 3-OH C14 fatty acids and two phosphate groups (16). In contrast to LPS-37, LPS isolated from F. tularensis was reported to be neither stimulatory nor antagonistic to human and murine cells via TLR4 (11). This difference was thought to be caused by the variations in their compositions, as monophosphoryl lipid A has been reported to have weaker activity than diphosphoryl lipid A (13) and longer acyl chains such as C16 have been reported to have weaker activity than C14 (22). These so-called silent characteristics of F. tularensis LPS are thought to contribute to its capacity to evade mammalian immune defense mechanisms and to promote survival in an infected host (9, 30). More recently, the effects of the preventive administration of a synthetic TLR4 agonist on the protection of mice from experimental pneumonic tularemia have been demonstrated (18). Similar prophylactic activation of TLR4 may also prove useful against Y. pestis infection.
The synthetic antagonist prototype termed compound 406 is a lipid IVA that is a biosynthetic precursor of E. coli lipid A (hexa-acylated) (26-27). This precursor structure, however, is not normally found in the outer membrane of E. coli or other usual members of the Enterobacteriaceae family. LPS is the major structural component of the cell wall outer membrane of gram-negative bacteria and plays an important role in the stabilization of the bacterial body. A mutant strain of E. coli that synthesizes only the lipid IVA precursor and that contains only this type of lipid A species in its LPS has been reported to grow very slowly and to be unstable, as judged by its antibiotic hypersensitivity and easy lysis following centrifugation (35). However, Y. pestis grown at 37°C does not appear to be sensitive to oscillatory shock or susceptible to antibacterial factors in the serum of the infected host. It has been reported that the minimal LPS structure required for the viability of E. coli and Salmonella enterica serovar Typhimurium is lipid A glycosylated with 3-deoxy-d-manno-octulosonic acid (Kdo) residues but that Y. pestis can survive without Kdo residues in its LPS (32). In combination, these results suggest that Y. pestis differs from E. coli and other usual species of the Enterobacteriaceae, as it contains additional factors that may allow the construction of a strong outer membrane and the formation of a stable bacterial body, thus compensating for its insufficient LPS structure.
It has been reported that Y. pestis grown at a lower temperature (21°C) is readily phagocytosed by human neutrophils (15) but that Y. pestis grown at 37°C is resistant to phagocytosis (31). In the current study, we did not observe any antiphagocytic effects of LPS-37 on bacterial phagocytes in U937 cells, even though LPS-37 strongly suppressed the TLR4-mediated inflammatory responses of these cells. Several antiphagocytic factors produced by Y. pestis are known to be upregulated during growth at 37°C. These factors include the type III secretion system (TTSS) and several effecter Yop proteins expressed on plasmid pCD1 (33) and the F1 capsule protein expressed on plasmid pMT1 (6, 20). These factors have been shown to contribute to the extracellular survival of the bacterium following infection of humans (31). These results suggest that LPS-37 does not function as an antiphagocytic factor or that some additional factors expressed at 37°C are responsible for the antiphagocytic activity.
In conclusion, the current study reports on a possible role for the Y. pestis LPS during the infection of humans. LPS-37 appears to preserve the bacterium from elimination from the host via activation of the human TLR4 defense system during the early stages of infection when it is present in the bacterium-bound form and as a suppressor of the defense system when it is present in the bacterium-free form. We also found that LPS-27, an agonistic form of LPS expressed by numerous gram-negative bacterial species, was easily recognized by human TLR4 even in the bacterium-bound form.
Footnotes
Published ahead of print on 4 November 2009.
REFERENCES
- 1.Akashi, S., H. Ogata, F. Kirikae, T. Kirikae, K. Kawasaki, M. Nishijima, R. Shimazu, Y. Nagai, K. Fukudome, M. Kimoto, and K. Miyake. 2000. Regulatory roles for CD14 and phosphatidylinositol in the signaling via Toll-like receptor 4-MD-2. Biochem. Biophys. Res. Commun. 268:172-177. [DOI] [PubMed] [Google Scholar]
- 2.Anisimov, A. P., L. E. Lindler, and G. B. Pier. 2004. Intraspecific diversity of Yersinia pestis. Clin. Microbiol. Rev. 17:434-464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Braun, M. C., J. He, C. Y. Wu, and B. L. Kelsall. 1999. Cholera toxin suppresses interleukin (IL)-12 production and IL-12 receptor beta1 and beta2 chain expression. J. Exp. Med. 189:541-552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brubaker, R. R. 1991. Factors promoting acute and chronic diseases caused by yersiniae. Clin. Microbiol. Rev. 4:309-324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.de Waal Malefyt, R., J. Abrams, B. Bennett, C. G. Figdor, and J. E. de Vries. 1991. Interleukin 10 (IL-10) inhibits cytokine synthesis by human monocytes: an autoregulatory role of IL-10 produced by monocytes. J. Exp. Med. 174:1209-1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Du, Y., R. Rosqvist, and A. Forsberg. 2002. Role of fraction 1 antigen of Yersinia pestis in inhibition of phagocytosis. Infect. Immun. 70:1453-1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Galanos, C., O. Lüderitz, and O. Westphal. 1979. Preparation and properties of standard lipopolysaccharide from Salmonella abortus equi. Zentralbl. Bacteriol. Microbiol. Hyg. Abt. 1 Orig. Reihe A 243:226-244. [PubMed] [Google Scholar]
- 8.Galanos, C., O. Luderitz, E. T. Rietschel, O. Westphal, H. Brade, L. Brade, M. Freudenberg, U. Schade, M. Imoto, H. Yoshimura, et al. 1985. Synthetic and natural Escherichia coli free lipid A express identical endotoxic activities. Eur. J. Biochem. 148:1-5. [DOI] [PubMed] [Google Scholar]
- 9.Gallagher, L. A., E. Ramage, M. A. Jacobs, R. Kaul, M. Brittnacher, and C. Manoil. 2007. A comprehensive transposon mutant library of Francisella novicida, a bioweapon surrogate. Proc. Natl. Acad. Sci. U. S. A. 104:1009-1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Golenbock, D. T., R. Y. Hampton, N. Qureshi, K. Takayama, and C. R. Raetz. 1991. Lipid A-like molecules that antagonize the effects of endotoxins on human monocytes. J. Biol. Chem. 266:19490-19498. [PubMed] [Google Scholar]
- 11.Hajjar, A. M., M. D. Harvey, S. A. Shaffer, D. R. Goodlett, A. Sjostedt, H. Edebro, M. Forsman, M. Bystrom, M. Pelletier, C. B. Wilson, S. I. Miller, S. J. Skerrett, and R. K. Ernst. 2006. Lack of in vitro and in vivo recognition of Francisella tularensis subspecies lipopolysaccharide by Toll-like receptors. Infect. Immun. 74:6730-6738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hinnebusch, B. J., A. E. Rudolph, P. Cherepanov, J. E. Dixon, T. G. Schwan, and A. Forsberg. 2002. Role of Yersinia murine toxin in survival of Yersinia pestis in the midgut of the flea vector. Science 296:733-735. [DOI] [PubMed] [Google Scholar]
- 13.Homma, J. Y., M. Matsuura, S. Kanegasaki, Y. Kawakubo, Y. Kojima, N. Shibukawa, Y. Kumazawa, A. Yamamoto, K. Tanamoto, T. Yasuda, et al. 1985. Structural requirements of lipid A responsible for the functions: a study with chemically synthesized lipid A and its analogues. J. Biochem. 98:395-406. [DOI] [PubMed] [Google Scholar]
- 14.Huang, X. Z., and L. E. Lindler. 2004. The pH 6 antigen is an antiphagocytic factor produced by Yersinia pestis independent of Yersinia outer proteins and capsule antigen. Infect. Immun. 72:7212-7219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jarrett, C. O., E. Deak, K. E. Isherwood, P. C. Oyston, E. R. Fischer, A. R. Whitney, S. D. Kobayashi, F. R. DeLeo, and B. J. Hinnebusch. 2004. Transmission of Yersinia pestis from an infectious biofilm in the flea vector. J. Infect. Dis. 190:783-792. [DOI] [PubMed] [Google Scholar]
- 16.Kawahara, K., H. Tsukano, H. Watanabe, B. Lindner, and M. Matsuura. 2002. Modification of the structure and activity of lipid A in Yersinia pestis lipopolysaccharide by growth temperature. Infect. Immun. 70:4092-4098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kotani, S., H. Takada, M. Tsujimoto, T. Ogawa, I. Takahashi, T. Ikeda, K. Otsuka, H. Shimauchi, N. Kasai, J. Mashimo, et al. 1985. Synthetic lipid A with endotoxic and related biological activities comparable to those of a natural lipid A from an Escherichia coli re-mutant. Infect. Immun. 49:225-237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lembo, A., M. Pelletier, R. Iyer, M. Timko, J. C. Dudda, T. E. West, C. B. Wilson, A. M. Hajjar, and S. J. Skerrett. 2008. Administration of a synthetic TLR4 agonist protects mice from pneumonic tularemia. J. Immunol. 180:7574-7581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lien, E., T. J. Sellati, A. Yoshimura, T. H. Flo, G. Rawadi, R. W. Finberg, J. D. Carroll, T. Espevik, R. R. Ingalls, J. D. Radolf, and D. T. Golenbock. 1999. Toll-like receptor 2 functions as a pattern recognition receptor for diverse bacterial products. J. Biol. Chem. 274:33419-33425. [DOI] [PubMed] [Google Scholar]
- 20.Liu, F., H. Chen, E. M. Galvan, M. A. Lasaro, and D. M. Schifferli. 2006. Effects of Psa and F1 on the adhesive and invasive interactions of Yersinia pestis with human respiratory tract epithelial cells. Infect. Immun. 74:5636-5644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Manthey, C. L., and S. N. Vogel. 1994. Elimination of trace endotoxin protein from rough chemotype LPS. J. Endotoxin Res. 1:84-91. [Google Scholar]
- 22.Matsuura, M., M. Kiso, and A. Hasegawa. 1999. Activity of monosaccharide lipid A analogues in human monocytic cells as agonists or antagonists of bacterial lipopolysaccharide. Infect. Immun. 67:6286-6292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Montminy, S. W., N. Khan, S. McGrath, M. J. Walkowicz, F. Sharp, J. E. Conlon, K. Fukase, S. Kusumoto, C. Sweet, K. Miyake, S. Akira, R. J. Cotter, J. D. Goguen, and E. Lien. 2006. Virulence factors of Yersinia pestis are overcome by a strong lipopolysaccharide response. Nat. Immunol. 7:1066-1073. [DOI] [PubMed] [Google Scholar]
- 24.Perry, R. D., and J. D. Fetherston. 1997. Yersinia pestis—etiologic agent of plague. Clin. Microbiol. Rev. 10:35-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Phillips, N. J., B. Schilling, M. K. McLendon, M. A. Apicella, and B. W. Gibson. 2004. Novel modification of lipid A of Francisella tularensis. Infect. Immun. 72:5340-5348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Raetz, C. R. 1993. Bacterial endotoxins: extraordinary lipids that activate eucaryotic signal transduction. J. Bacteriol. 175:5745-5753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Raetz, C. R., C. M. Reynolds, M. S. Trent, and R. E. Bishop. 2007. Lipid A modification systems in gram-negative bacteria. Annu. Rev. Biochem. 76:295-329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Raetz, C. R., and C. Whitfield. 2002. Lipopolysaccharide endotoxins. Annu. Rev. Biochem. 71:635-700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rebeil, R., R. K. Ernst, B. B. Gowen, S. I. Miller, and B. J. Hinnebusch. 2004. Variation in lipid A structure in the pathogenic yersiniae. Mol. Microbiol. 52:1363-1373. [DOI] [PubMed] [Google Scholar]
- 30.Sjostedt, A. 2006. Intracellular survival mechanisms of Francisella tularensis, a stealth pathogen. Microbes Infect. 8:561-567. [DOI] [PubMed] [Google Scholar]
- 31.Spinner, J. L., J. A. Cundiff, and S. D. Kobayashi. 2008. Yersinia pestis type III secretion system-dependent inhibition of human polymorphonuclear leukocyte function. Infect. Immun. 76:3754-3760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tan, L., and C. Darby. 2005. Yersinia pestis is viable with endotoxin composed of only lipid A. J. Bacteriol. 187:6599-6600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Viboud, G. I., and J. B. Bliska. 2005. Yersinia outer proteins: role in modulation of host cell signaling responses and pathogenesis. Annu. Rev. Microbiol. 59:69-89. [DOI] [PubMed] [Google Scholar]
- 34.Vinogradov, E., M. B. Perry, and J. W. Conlan. 2002. Structural analysis of Francisella tularensis lipopolysaccharide. Eur. J. Biochem. 269:6112-6118. [DOI] [PubMed] [Google Scholar]
- 35.Vorachek-Warren, M. K., S. Ramirez, R. J. Cotter, and C. R. Raetz. 2002. A triple mutant of Escherichia coli lacking secondary acyl chains on lipid A. J. Biol. Chem. 277:14194-14205. [DOI] [PubMed] [Google Scholar]
- 36.Wan, C. P., C. S. Park, and B. H. Lau. 1993. A rapid and simple microfluorometric phagocytosis assay. J. Immunol. Methods 162:1-7. [DOI] [PubMed] [Google Scholar]