Abstract
A more effective vaccine against Mycobacterium tuberculosis is needed, and a number of M. tuberculosis vaccine candidates are currently in preclinical or clinical phase I and II studies. One of the strategies to select M. tuberculosis (protein) targets to elicit a CD8+ or CD4+ T-cell response is to gauge the binding of candidate peptides to major histocompatibility complex (MHC) class I or class II molecules, a prerequisite for successful peptide presentation and to expand antigen-specific T cells. We scanned 61 proteins from the M. tuberculosis proteome for potential MHC class II-presented epitopes that could serve as targets for CD4+ T-cell responses. We constructed a peptide microarray consisting of 7,466 unique peptides derived from 61 M. tuberculosis proteins. The peptides were 15-mers overlapping by 12 amino acids. Soluble recombinant DRB1*0101 (DR1), DRB1*1501 (DR2), and DRB1*0401 (DR4) monomers were used to gauge binding to individual peptide species. Out of 7,466 peptides, 1,282, 674, and 1,854 peptides formed stable complexes with HLA-DR1, -DR2, and -DR4, respectively. Five hundred forty-four peptides bound to all three MHC class II molecules, 609 bound to only two, and 756 bound to only a single MHC class II molecule. This allowed us to rank M. tuberculosis proteins by epitope density. M. tuberculosis proteins contained “hot spots,” i.e., regions with enriched MHC class II binding epitopes. Two hundred twenty-two peptides that formed MHC class II-peptide complexes had previously been described as exclusively recognized by IgG in sera from patients with active pulmonary tuberculosis, but not in sera from healthy individuals, suggesting that these peptides serve as B-cell and CD4+ T-cell epitopes. This work helps to identify not only M. tuberculosis peptides with immunogenic potential, but also the most immunogenic proteins. This information is useful for vaccine design and the development of future tools to explore immune responses to M. tuberculosis.
CD4+ T cells play a central role in Mycobacterium tuberculosis-directed cellular immune responses (2, 6, 7, 12). It is most likely that an effective tuberculosis (TB) vaccine would target the expansion of CD8+ and CD4+ T cells, which recognize M. tuberculosis peptides presented by major histocompatibility complex (MHC) class I and class II molecules.
The MHC locus is the most variable gene locus in the human genome, and the variability of MHC class II alleles in different populations is well documented (24). Certain MHC class II alleles have been shown to be associated with M. tuberculosis infection (1, 11, 15, 16, 23): DRB1*0803 and DQB1*0601 were found to be associated with TB disease progression, development of drug resistance, and disease severity in Koreans (16). In South Africa, DRB1*1302 and DQB1*0301 to -0304 were apparently associated with active TB compared to control individuals lacking these alleles (23). The prevalence of HLA-DRB1*0401 and HLA-DRB1*0801 was significantly decreased in Mexican patients with pulmonary TB compared to their prevalence in healthy controls (35).
The association of some MHC class II alleles with “better disease outcome” could be due to the fact that these alleles are “better” at binding and presenting a certain repertoire of peptide epitopes to CD4+ T cells than other alleles. The identification of peptides binding to molecularly defined MHC class II alleles could therefore represent an important first step in identifying potential targets for TB vaccine design and the development of new diagnostic assays. More recently, De Groot and colleagues used a bioinformatics approach, followed by validation with functional assays to identify CD4+ T-cell epitopes that were used to construct an epitope-based M. tuberculosis vaccine (5).
Only a few M. tuberculosis MHC class II binding peptides have been identified so far, and 7% of the M. tuberculosis open reading frames have been explored for both B-cell and T-cell epitopes (3). We described a peptide microarray assay that allowed us to visualize HIV peptide binding to molecularly defined MHC class II alleles (9). The assay has the major advantage that a high number of candidate peptides can be screened within a short time frame. In the current report, we describe M. tuberculosis peptide binding to the three most frequently encountered MHC class II alleles in different populations; DRB1*0101 (DR1), DRB1*1501 (DR2), and DRB1*0401 (DR4). DR1, DR2, and DR4 exhibit population frequencies of 15.4%, 32.9%, and 20.9% among Caucasians. In the Botswana population, HLA-DRB1*01, -DRB1*02, and -DRB1*04 show population frequencies of 21.7%, 21.3%, and 14.4%, respectively. The candidate test peptides are derived from 61 M. tuberculosis proteins that have been tested for IgG and IgA recognition in patients with active pulmonary TB. The data sets contribute to defining “immunogenicity” in M. tuberculosis candidate target proteins, visualize MHC class II epitope “hot spots,” and allow us to link B-cell targets and potential MHC class II-presented M. tuberculosis epitopes.
MATERIALS AND METHODS
Mycobacterium tuberculosis peptides.
Sixty-one M. tuberculosis proteins were printed as overlapping peptide (15-amino-acid) stretches on microarray slides, as reported previously (10). Most of these proteins have not been mapped for MHC class II binding, except for antigen 85B, heat shock protein HSPX, and MPT63 (Rv1926c) (20). These data were therefore available for comparative analysis. The biological functions of the 61 proteins in the M. tuberculosis life cycle have been addressed in detail previously (10), and an overview is provided in Table 1.
TABLE 1.
M. tuberculosis proteins tested for MHC class II peptide binding
| Protein name | Gene name | Functional classification |
|---|---|---|
| 10-kDa chaperonin GROES CAB01005 | Rv3418c | Virulence, detoxification, adaptation |
| 60-kDa chaperonin 2 P0A521 | Rv0440 | Virulence, detoxification, adaptation |
| Heat shock protein HSP CAA17343 | Rv0251c | Virulence, detoxification, adaptation |
| Heat shock protein HSPX CAA17245 | Rv2031c | Virulence, detoxification, adaptation |
| MCE family protein MCE1A YP_177701 | Rv0169 | Virulence, detoxification, adaptation |
| Possible hemolysin CAA16235 | Rv3922c | Virulence, detoxification, adaptation |
| Possible hemolysin-like protein CAA17201 | Rv1085c | Virulence, detoxification, adaptation |
| 3-Oxoacyl-[acyl-carrier protein] synthase 2 KASB CAA94642 | Rv2246 | Lipid metabolism |
| Biotinylated protein TB7.3 CAB08316 | Rv3221c | Lipid metabolism |
| M. Bovis acyl- coenzyme A synthase gene; U75685 | Lipid metabolism | |
| M. Bovis mycocerosic acid synthase gene M95808 | Lipid metabolism | |
| Putative cyclopropane-fatty-acyl-phospholipid synthase UFAA1 NP_854118 | Rv0447c | Lipid metabolism |
| Secreted antigen 85-B FBPB (85B) CAB10044 | Rv1886c | Lipid metabolism |
| Alternate RNA polymerase sigma factor SIGF CAB07069 | Rv3286c | Information pathways |
| Probable 50S ribosomal protein L7/L12 RPLL CAB07109 | Rv0652 | Information pathways |
| RNA polymerase beta subunit AAA21416 | Rv0667 | Information pathways |
| RNA polymerase beta′ subunit AAA21417 | Rv0667 | Information pathways |
| 10-kDa culture filtrate antigen ESXB | Rv3874 | Cell wall and cell processes |
| Immunogenic protein MPT63 CAB06500 | Rv1926c | Cell wall and cell processes |
| Cell surface lipoprotein MPT83 CAB08316 | Rv2873 | Cell wall and cell processes |
| Conserved hypothetical protein TB9.8 CAD93159 | Rv0287 | Cell wall and cell processes |
| ESAT-6-like protein ESXQ CAA16102 | Rv3017c | Cell wall and cell processes |
| Immunogenic protein MPT64 CAA98382 | Rv1980c | Cell wall and cell processes |
| Lipoprotein LPQH precursor P0A5J0 | Rv3763 | Cell wall and cell processes |
| Low-molecular-weight protein antigen 7 ESXH TB10.4 CAA17363 | Rv0288 | Cell wall and cell processes |
| Low-molecular-weight T-cell antigen TB8.4NP_215690 | Rv1174c | Cell wall and cell processes |
| Major secreted immunogenic protein CAA98373 | Rv2875 | Cell wall and cell processes |
| Periplasmic phosphate-binding lipoprotein PSTS1 YP_177770 | Rv0934 | Cell wall and cell processes |
| Periplasmic phosphate-binding lipoprotein PSTS2 YP_177769 | Rv0932c | Cell wall and cell processes |
| Periplasmic phosphate-binding lipoprotein PSTS3 YP_177768 | Rv0928 | Cell wall and cell processes |
| Probable cutinase precursor CFP21 NP_216500 | Rv1984c | Cell wall and cell processes |
| Probable lipoprotein LPRJ CAB10947 | Rv1690 | Cell wall and cell processes |
| Putative ESAT-6-like protein ESXN YP_177838 | Rv1793 | Cell wall and cell processes |
| Secreted ESAT-6-like protein ESXR CAA16104 | Rv3019c | Cell wall and cell processes |
| 6-kDa early secretory antigenic target ESXA(ESAT-6) CAE55648 | Rv3875 | Cell wall and cell processes |
| PE family protein CAE55335 | Rv0916c | PE/PPE |
| PPE family protein CAE55371 | Rv1196 | PE/PPE |
| PPE family protein YP 177963 | Rv3347c | PE/PPE |
| PPE family protein CAE55334 | Rv0915c | PE/PPE |
| PPE family protein CAE55489 | Rv2430c | PE/PPE |
| PPE family protein CAE55504 | Rv2608 | PE/PPE |
| Secreted l-alanine dehydrogenase ALD CAA15575 | Rv2780 | Intermediary metabolism and respiration |
| Possible glycosyltransferase CAB05418 | Rv2958c | Intermediary metabolism and respiration |
| Possible glycosyltransferase CAB05419 | Rv2957 | Intermediary metabolism and respiration |
| Probable isocitrate dehydrogenase CAA17111 | Rv3339c | Intermediary metabolism and respiration |
| Probable isocitrate dehydrogenase CAA16247 | Rv0066c | Intermediary metabolism and respiration |
| Probable molybdopterin-guanine dinucleotide biosynthesis protein CAA16030 | Rv2453c | Intermediary metabolism and respiration |
| Probable serine protease PEPA CAB09453 | Rv0125 | Intermediary metabolism and respiration |
| Probable serine protease PEPD CAA17582 | Rv0983 | Intermediary metabolism and respiration |
| Possible glycosyltransferase CAB05415 | Rv2962c | Intermediary metabolism and respiration |
| MTB48 AAK31576 | Unknown | |
| MTB81 | Unknown | |
| Transmembrane serine/threonine-protein kinasE D PKND NP_215446 | Rv0931c | Regulatory proteins |
| Two-component transcriptional-regulatory protein DEVR NP_217649 | Rv3133c | Regulatory proteins |
| Conserved hypothetical protein CFP17 CAB01474 | Rv1827 | Conserved hypotheticals |
| Conserved hypothetical protein TB16.3CAD97060 | Rv2185c | Conserved hypotheticals |
| Conserved hypothetical protein TB18.5CAD93033 | Rv0164 | Conserved hypotheticals |
| Hypothetical protein NP_217139 | Rv2623 | Conserved hypotheticals |
| Hypothetical protein NP_217142 | Rv2626c | Conserved hypotheticals |
| Iron-regulated conserved hypothetical protein CAB08889 | Rv1636 | Conserved hypotheticals |
| Conserved hypothetical protein CAB08634 | Rv2629 | Conserved hypotheticals |
Peptide microarray printing.
The peptide microarray slides used in this experiment were produced by JPT, Germany. The peptides were synthesized as amino-oxy-acetylated peptides on cellulose membranes in a parallel manner using SPOT synthesis technology (8, 32). The printing process was carried out as reported previously (28), and the slides were stored at 4°C until they were ready for use.
Soluble HLA class II alleles.
Three MHC class II alleles, HLA-DRB1*0101 (DR1), -DRB1*1501 (DR2), and -DRB1*0401 (DR4), were supplied by Beckman Coulter. The process for the production of these alleles has been described in detail elsewhere (29).
Sample processing.
HLA-DR monomers were incubated with the peptide microarrays as described previously (9). Briefly, MHC class II monomers were diluted to a working concentration of 1 μg/ml using a binding buffer (36 mM phosphate, 14.4 mM citrate, 0.15% bovine serum albumin [BSA], 0.25% octyl beta-d-glucopyranoside, 0.02% NaN3, pH 5.5). Three hundred microliters of the HLA-DR-buffer mixture was incubated with the peptide microarray slide for 48 h at 37°C in a humid chamber. The slides were then washed three times for 5 min each, two times with washing solution (phosphate-buffered saline [PBS] and 0.05% Tween 80), and once with PBS alone. Next, the slides were incubated for 1 h at room temperature with 300 μl of a Cy5-labeled monoclonal antibody (MAb) (clone L243, obtained from Beckman Coulter) diluted to 5 μg/ml in PBS to detect stable MHC class II-peptide complexes. The slides were dried by spinning them for 10 s using a slide spinner (Euro Tech, United Kingdom). Two slides were incubated with each monomer, and two slides were incubated with buffer and the detection antibody to identify peptides that were recognized by secondary antibody. These peptides were excluded from analysis.
Data acquisition. (i) Scanning and analysis.
Each slide was scanned with the GenPix 4000B microarray scanner (Axon Instruments) at two wavelengths, 532 and 635 nm, and the images were saved in TIFF and JPG formats. Image analysis was performed utilizing the circular feature alignment of the GenePix Pro 5.1 software and the Genepix Array List (GAL) files supplied by JPT, Berlin, Germany. Spots with nonuniform foreground or background signals were flagged if they satisfied the following criteria: {[F635 mean] > (1.5 × [F635 median]){ and ([F635 median] > 40) or {[B635 mean] > (1.5 × [B635 median])} and ([B635 median] > 40).
These and other flags assigned by GenePix resulted in four types of spots: “good” or “nonflagged” spots (labeled as 0′), “bad” or “flagged” spots (labeled as −100′), not-found spots (labeled as −50′), and empty spots (labeled as −75′). The image from each subarray was saved as a GenePix result (GPR) file, and the median foreground and background intensities for the 635-nm wavelength from individual peptide spots were used in the response analysis. All GPR files were saved in a common folder and imported into R/Bioconductor using the read.GenePix function from the marray R/bioconductor package.
We examined the distribution of the flags (listed above) to monitor the acquired data for quality control purposes. This quality control exercise was conducted for each of the four groups of slides ([i] slides incubated with buffer only, [ii] HLA-DRB1*0101 slides, [iii] HLA-DRB1*1501 slides, and [iv] HLA-DRB1*0401 slides), both overall and stratified by the type of feature (control or peptide spots). Visual inspection of the images from the individual subarrays was carried out using the Image function in Bioconductor in order to evaluate questionable responses that should be excluded from data analysis. For a measure of the strength of the response, we chose the ratio of the median foreground to background (on a log scale). This response index was computed for all spots with background greater than zero, and any spots with zero background were excluded. The data for each of the four groups of slides were arranged in a large matrix, with columns identifying slide, subarray, and block. All the analyses described below used these master data sets.
(ii) Data reduction.
Using the distribution of the negative controls to define a cutoff for a “detectable” response, we removed the spots with no detectable response on any slide. The method used to define the cutoff has been described previously (23). Any peptide with a high response on slides incubated with buffer only and the Cy5-labeled MAb L243 was considered a false positive and discarded from analysis. After all valid (i.e., unflagged) peptide responses on the buffer slides were normalized using the same linear model as for the negative controls, the cutoff was determined for the definition of a false-positive event.
(iii) Analysis of peptide responses.
For each group of slides incubated with soluble recombinant MHC class II molecules, we used the thresholds defined above to exclude from the analysis any peptide that (i) had no detectable response on any slide or (ii) had a false-positive response in at least 10% of replicates. The remaining peptide responses were normalized using a linear model to remove artifacts due to slide, subarray, and block. Since the systematic effects of slide, subarray, and block were removed, we refer to these as the “normalized responses.” For any peptides that were replicated, the normalized values were averaged. Thus, the preprocessed data consist of a list of unique peptides with their normalized values for each slide.
RESULTS
Peptides binding to the three soluble HLA-DR alleles.
Peptide microarray slides printed with 7,446 unique peptides derived from 61 Mycobacterium tuberculosis proteins were incubated with soluble MHC class II monomers, i.e., DRB1*0101, DRB1*1501, and DRB1*0401. The printed peptides were 15-mers overlapping by 12 amino acids. The peptide microarray slides also contained empty spots, which were used as negative control spots, and Cy3 spots, which were used for GAL file alignment.
The reported average index represents a function of both the binding affinity and the off rate of the MHC class II-peptide interaction. Each of these factors contributes to the signal intensity of the antibody that detects properly folded MHC class II-peptide complexes. Table 1 lists the M. tuberculosis proteins used to screen for MHC class II monomer interaction. The complete list of peptides binding to the MHC class II monomers is provided in Table S1 in the supplemental material. We observed binding of 1,282, 674, and 1,854 peptides to HLA-DRB1*0101, -DRB1*1501, and -DRB1*0401, respectively.
To evaluate the MHC class II-peptide binding pattern for the entire 61 M. tuberculosis proteins (and the three MHC class II alleles), we carried out a Pearson centered hierarchical clustering analysis (Fig. 1). The peptides are clustered into groups recognized by only one monomer, groups recognized by two monomers, and groups recognized by all three MHC class II monomers. There were more peptides binding to HLA-DRB1*0401 than to HLA-DRB1*1501 and -DRB1*0101.
FIG. 1.
Pearson centered hierarchical clustering analysis of M. tuberculosis peptides from 61 proteins binding to MHC class II monomers. Peptides binding to only one of the MHC class II alleles can be identified, as well as peptide groups that bind to only two or a to a single MHC class II molecule. Mtb, M. tuberculosis.
MHC class II epitope densities on M. tuberculosis proteins.
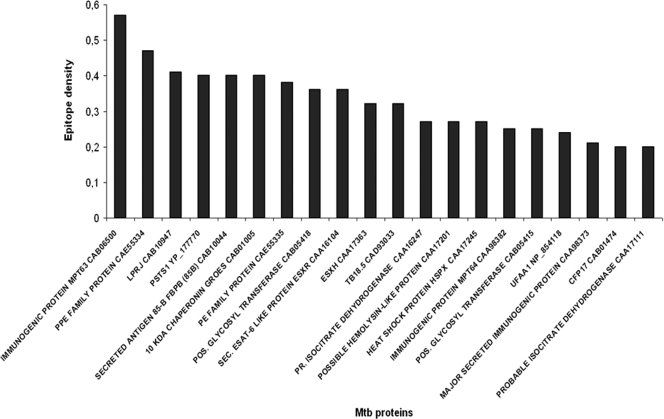
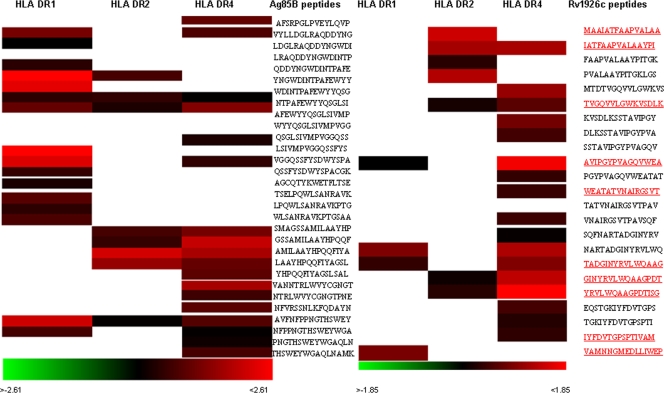
Next, we analyzed M. tuberculosis peptides that bind with a particular index value (i.e., the measure of MHC class II-peptide complex formation) in a reproducible fashion; we set an average index value cutoff of 0.00 in at least 2 of 3 repeats. We then calculated the epitope density of each individual M. tuberculosis protein, defined as the number of peptides binding to any MHC class II monomer per total number of peptides from the respective M. tuberculosis protein. Figure 2 shows the top 20 M. tuberculosis proteins with the highest epitope densities; the epitope densities of the entire set of 61 M. tuberculosis proteins are provided in Table 2. The “epitope density value” provides a good estimate of which proteins are likely to provide epitopes to DRB1*0101, DRB1*1501, and/or DRB1*0401 MHC class II molecules; they are also likely to provide more CD4+ T-cell epitopes, which may lead to T-cell expansion if the appropriate T-cell receptors (TCRs) are present in the TCR repertoire at the time of vaccination or exposure to the nominal target antigen. We then compared the Ag85B and MPT63 peptides that tested positive for MHC class II monomer binding with previously published T-cell epitopes (Fig. 3). For MPT63, most of the peptides identified by use of the current approach have been described as CD4+ T-cell epitopes.
FIG. 2.
Epitope densities of the top 20 M. tuberculosis proteins defined by the number of peptides binding to MHC class II molecules.
TABLE 2.
Number of peptides from each individual M. tuberculosis protein binding to three MHC class II allelesa
| Protein | No. of peptides | No. of epitopes |
No. of epitopes/peptideb | |||
|---|---|---|---|---|---|---|
| DR1 | DR2 | DR4 | Total | |||
| Immunogenic protein MPT63 CAB06500 | 49 | 4 | 7 | 17 | 28 | 0.57 |
| PPE family protein CAE55334 | 137 | 23 | 16 | 25 | 64 | 0.47 |
| Probable lipoprotein LPRJ CAB10947 | 39 | 3 | 4 | 9 | 16 | 0.41 |
| Periplasmic phosphate-binding lipoprotein PSTS1 YP_177770 | 121 | 17 | 12 | 20 | 49 | 0.40 |
| Secreted antigen 85-B FBPB (85B) CAB10044 | 105 | 16 | 8 | 18 | 42 | 0.40 |
| 10-kDa chaperonin GROES CAB01005 | 30 | 6 | 2 | 4 | 12 | 0.40 |
| PE family protein CAE55335 | 29 | 1 | 2 | 8 | 11 | 0.38 |
| Possible glycosyltransferase CAB05418 | 139 | 12 | 10 | 28 | 50 | 0.36 |
| Secreted ESAT-6-like protein ESXR CAA16104 | 28 | 5 | 0 | 5 | 10 | 0.36 |
| Low-molecular-weight protein antigen 7 ESXH CAA17363 | 28 | 3 | 1 | 5 | 9 | 0.32 |
| Conserved hypothetical protein TB18.5CAD93033 | 50 | 6 | 4 | 6 | 16 | 0.32 |
| Probable isocitrate dehydrogenase CAA16247 | 245 | 30 | 9 | 28 | 67 | 0.27 |
| Possible hemolysin-like protein CAA17201 | 77 | 9 | 3 | 9 | 21 | 0.27 |
| Heat shock protein HSPX CAA17245 | 44 | 3 | 3 | 6 | 12 | 0.27 |
| Immunogenic protein MPT64 CAA98382 | 72 | 8 | 2 | 8 | 18 | 0.25 |
| Possible glycosyltransferase CAB05415 | 146 | 10 | 7 | 19 | 36 | 0.25 |
| Putative cyclopropane-fatty-acyl-phospholipid synthase UFAA1 NP_854118 | 139 | 11 | 6 | 16 | 33 | 0.24 |
| Major secreted immunogenic protein CAA98373 | 61 | 2 | 0 | 11 | 13 | 0.21 |
| Conserved hypothetical protein CFP17 CAB01474 | 50 | 2 | 2 | 6 | 10 | 0.20 |
| Probable isocitrate dehydrogenase CAA17111 | 133 | 12 | 5 | 9 | 26 | 0.20 |
| MCE family protein MCE1AYP_177701 | 148 | 15 | 4 | 9 | 28 | 0.19 |
| Heat shock protein HSP CAA17343 | 49 | 2 | 2 | 5 | 9 | 0.18 |
| Conserved hypothetical protein TB16.3CAD97060 | 44 | 5 | 2 | 1 | 8 | 0.18 |
| Possible hemolysin CAA16235 | 36 | 3 | 1 | 2 | 6 | 0.17 |
| M. bovis mycocerosic acid synthase gene; M95808 | 700 | 35 | 16 | 61 | 112 | 0.16 |
| Probable cutinase precursor CFP21 NP_216500 | 69 | 1 | 3 | 7 | 11 | 0.16 |
| Two-component transcriptional regulatory protein DEVR NP_217649 | 69 | 2 | 5 | 4 | 11 | 0.16 |
| Possible glycosyltransferase CAB05419 | 88 | 6 | 4 | 4 | 14 | 0.16 |
| Probable molybdopterin-guanine dinucleotide biosynthesis protein CAA16030 | 63 | 1 | 3 | 6 | 10 | 0.16 |
| Hypothetical protein RV2623 NP_217139 | 95 | 4 | 0 | 11 | 15 | 0.16 |
| Transmembrane serine/threonine-protein kinase D PKND NP_215446 | 218 | 13 | 7 | 12 | 32 | 0.15 |
| M. bovis acyl-coenzyme A synthase gene; U75685 | 190 | 7 | 6 | 14 | 27 | 0.14 |
| ESAT-6-Like protein ESXQ CAA16102 | 36 | 0 | 1 | 4 | 5 | 0.14 |
| Conserved hypothetical protein TB9.8 CAD93159 | 29 | 2 | 1 | 1 | 4 | 0.14 |
| RNA polymerase beta subunit AAA21416 | 389 | 19 | 11 | 23 | 53 | 0.14 |
| PPE family protein CAE55371 | 127 | 4 | 1 | 12 | 17 | 0.13 |
| Conserved hypothetical protein CAB08634 | 121 | 2 | 2 | 11 | 15 | 0.12 |
| Secreted l-alanine dehydrogenase ALD CAA15575 | 120 | 3 | 1 | 9 | 13 | 0.11 |
| 10-kDa culture filtrate antigen ESXB CAA17966 | 30 | 0 | 0 | 3 | 3 | 0.10 |
| 3-oxoacyl-[acyl-carrier protein] synthase 2 KASB CAA94642 | 142 | 4 | 3 | 7 | 14 | 0.10 |
| PPE family protein YP_177963 | 1,037 | 33 | 24 | 44 | 101 | 0.10 |
| MTB81 | 243 | 7 | 10 | 6 | 23 | 0.09 |
| Low-molecular-weight T-cell antigen TB8.4 NP_215690 | 33 | 0 | 1 | 2 | 3 | 0.09 |
| Iron-regulated conserved hypothetical protein CAB08889 | 45 | 0 | 0 | 4 | 4 | 0.09 |
| MTB48 AAK31576 | 150 | 4 | 3 | 6 | 13 | 0.09 |
| Probable serine protease PEPD CAA17582 | 151 | 4 | 3 | 6 | 13 | 0.09 |
| Cell surface lipoprotein MPT83 CAA98350 | 70 | 2 | 0 | 4 | 6 | 0.09 |
| Probable serine protease PEPA CAB09453 | 115 | 0 | 1 | 8 | 9 | 0.08 |
| 60-kDa chaperonin 2 P0A521 | 176 | 3 | 5 | 5 | 13 | 0.07 |
| Conserved hypothetical protein CAA15739 | 39 | 0 | 0 | 2 | 2 | 0.05 |
| Conserved hypothetical protein CAB06237 | 130 | 0 | 3 | 2 | 5 | 0.04 |
| Probable 50S ribosomal protein L7/L12 RPLL CAB07109 | 40 | 0 | 0 | 1 | 1 | 0.03 |
| Alternate RNA polymerase sigma factor SIGF CAB07069 | 83 | 0 | 0 | 2 | 2 | 0.02 |
| Lipoprotein LPQH precursor P0A5J0 | 49 | 0 | 0 | 1 | 1 | 0.02 |
DRB1*0101, DRB1*1501, and DRB1*0401.
The “epitope density” of each protein.
FIG. 3.
Locations of peptide binding to MHC class II molecules for two selected epitope-rich proteins. The peptides are arranged from the N to the C terminus of the proteins Ag85B (left) and MPT63 (Rv1926c; right), and only positive binding results are shown. These two M. tuberculosis proteins have previously been explored for HLA class II binding peptides (3, 14, 26, 27). Peptides that have been previously described as CD4+ T-cell epitopes, defined in either functional assays or MHC class II binding or by MHC class II tetramers, are underlined and shown in red.
MHC class II binding peptides represent commonly recognized Ig epitopes in sera from patients with pulmonary TB.
We previously identified three patterns of IgG and IgA reactivity to M. tuberculosis target peptides: (i) epitopes that are exclusively recognized in individuals with pulmonary TB (and not in healthy individuals), (ii) epitopes that are recognized in healthy subjects and not in patients with pulmonary TB, and (iii) epitopes that are recognized in both TB patients and healthy controls, but in a differential manner, i.e., either strongly in one group and weakly in the other group or vice versa. Based on the observation that B- and T-cell epitopes can overlap, as defined by the SEREX approach in screening for tumor-specific B- and T-cell responses (20), we tested whether any MHC class II binding peptide identified in the current report would also serve as targets for an IgG response in sera from patients with acute pulmonary TB. Note that we screened only M. tuberculosis epitopes that were commonly recognized (n = 35/35 patients) in sera from patients with TB and not in any healthy individual (n = 34) for MHC class II binding. Two hundred twenty-two M. tuberculosis peptides that bound to any of the three MHC class II monomers were also defined as IgG epitopes in sera from patients with TB (14). Out of these 222 peptides, 33 bound to all three MHC class II monomers, 24 bound to only two monomers, and 165 bound to only a single MHC class II allele. Eighty peptides bound to HLA-DRB1*0101, 52 bound to HLA-DRB1*1501, and 185 peptides bound to HLA-DRB1*0401. These peptides are listed in Table S2 in the supplemental material.
DISCUSSION
Only 7% of the 4,000 open reading frames of M. tuberculosis have been explored for B-cell and T-cell epitopes. This is due to the size of the M. tuberculosis genome, i.e., the number of protein targets to be tested, and to the lack of appropriate technology to explore such a massive data set in an affordable manner. This report describes the detailed analysis of an M. tuberculosis peptide microarray using 7,446 overlapping peptides from 61 individual M. tuberculosis proteins to identify potential T-cell epitopes that could be presented by three common MHC class II alleles, HLA-DRB1*0101, -DRB1*1501, and -DRB1*0401. Most of the peptides that we identified bound to more than a single MHC class II molecule; only a few peptides bound to only one MHC class II allele. This is not surprising, since MHC class II peptide binding is quite promiscuous (17, 30), and all MHC class II binding M. tuberculosis peptides listed by Blythe and coworkers bound to three or more MHC class II alleles (3).
We identified more M. tuberculosis peptides that bound to HLA-DRB1*0401 than to HLA-DRB1*0101 or -DRB1*1501. HLA-DRB1*0401 was found to be associated with pulmonary TB in Italian patients (31). Thus, whether a broader M. tuberculosis peptide epitope presentation by HLA-DRB1*0401 is beneficial or detrimental to mounting a protective anti-M. tuberculosis-directed CD4+ T-cell response has to be explored in future studies.
Ranking of M. tuberculosis proteins by epitope densities identified MPT63 Rv1926c and PPE CAE55334/Rv0915c as the 2 of 61 M. tuberculosis proteins with the highest epitope densities. Immunization of C57BL/6 mice with MTB41 Rv0915c DNA induced protection against M. tuberculosis infection comparable to the protection induced by Mycobacterium bovis BCG (34), and the cellular immune responses were dominated by CD4+ T cells. Analysis of T-cell responses was carried out using the Rv0915c protein, and the immune responses were not determined on the peptide level.
Rv1926c, an M. tuberculosis-secreted protein, has recently been shown to be recognized (26) in healthy BCG-vaccinated subjects. Peptides binding to different MHC class II alleles were identified using a virtual matrix-based prediction program (ProPred). Nine (Rv1926c) peptides predicted to serve as promiscuous CD4+ T-cell epitopes (24) show significant overlap with the peptides that we identified as binding to the three MHC class II alleles. This lends support to our approach that MHC class II binding peptide species, defined by the interaction of soluble MHC class II molecules and immobilized peptides on a microarray chip, serve as CD4+ T-cell epitopes (9).
We were able to match MHC class II binding M. tuberculosis epitopes with peptide epitopes that were exclusively recognized by IgG from patients with TB (10). These candidate epitopes may represent clinically relevant targets for diagnostics. Conversely, MHC class II binding M. tuberculosis peptides recognized in individuals who have been exposed to M. tuberculosis but who are protected from development of disease may represent reasonable M. tuberculosis vaccine candidates. The identification of such M. tuberculosis targets (i.e., exclusive recognition in a clinically well-defined population) in association with “good immunogenicity,” defined by MHC class II epitope density, is currently under way in our laboratory.
The current study is limited, since we did not test the identified HLA-DR binding peptides for CD4+ T-cell recognition using peripheral blood mononuclear cells (PBMCs) from HLA-DR-matched patients with tuberculosis; corresponding CD4+ T cells endowed with a clonotypic TCR may not be part of the TCR repertoire in individual patients. The disadvantages of testing peptide-specific T-cell recognition may include the facts that (i) a single cytokine, e.g., interferon, may not reflect the breadth of a CD4+ T-cell response and (ii) individual peptide species may not be stable and may be quickly degraded in a standard assay gauging intracellular cytokine production. Not mutually exclusive, anti-M. tuberculosis responses may also be anergic in individuals with active pulmonary TB (33, 36). Tetramer-guided analysis may represent a remedy to this problem. However, the fact that some of the identified peptides have been reported previously (3, 26, 27) using functional assays or tetramer-guided analysis (14) supports the validity of the approach reported here. It is also important to note that some of the candidate test peptides might not bind to the HLA-DR alleles in vivo due to differential protein processing and subsequent presentation: peptide processing is dependent on the three-dimensional structure of proteins (18, 21, 22, 25). Future tetramer-guided analysis of PBMCs from patients with TB will aid in determining which peptides are presented in vivo and lead to expansion of antigen-specific CD4+ T cells.
Of note, MHC class II-presented peptides may also drive immunosuppressive immune responses associated with CD4+ regulatory T cells (Tregs). This may be considered in rational vaccine design, since Tregs have been associated with the suppression of Th1-type immune responses in M. tuberculosis infection (13). In addition, instability of the transcription factor Foxp3 may lead to the generation of antigen-specific memory T cells with altered effector properties. This has recently been shown to be true for Tregs with an activated-memory T-cell phenotype, which gave rise to potentially autoreactive effector T cells (37).
We hypothesize that most of the M. tuberculosis peptides that formed stable complexes with HLA-DRB1*0101, -DRB1*1502, and -DRB1*0401 may serve as CD4+ T-cell epitopes and that these peptides could be useful in designing a rational epitope-based vaccine against M. tuberculosis. We suggest that the integrated analysis of IgG-recognized targets from clinically very well-characterized patient cohorts will help make the best choice for M. tuberculosis vaccine targets. (Peptide) antigen-specific B cells may serve as professional antigen-presenting cells (19) for CD4+ T cells. Conversely, CD4+ T cells may provide help for B cells and CD8+ T cells. Therefore, M. tuberculosis vaccine target identification should be accompanied by MHC class I peptide binding analysis, since CD8+ T cells are instrumental in conferring long-term immune memory in TB (4), particularly in patients with HIV coinfection and decreased CD4+ T-cell numbers.
Supplementary Material
Acknowledgments
The work was supported in part by an EU Marie Curie Fellowship to S.G. and by grants from Vetenskapsrådet and SIDA, Sweden, to M.M.
Footnotes
Published ahead of print on 28 October 2009.
Supplemental material for this article may be found at http://cvi.asm.org/.
REFERENCES
- 1.Amirzargar, A. A., A. Yalda, M. Hajabolbaghi, F. Khosravi, H. Jabbari, N. Rezaei, M. H. Niknam, B. Ansari, B. Moradi, and B. Nikbin. 2004. The association of HLA-DRB, DQA1, DQB1 alleles and haplotype frequency in Iranian patients with pulmonary tuberculosis. Int. J. Tuberc. Lung Dis. 8:1017-1021. [PubMed] [Google Scholar]
- 2.Beveridge, N. E., D. A. Price, J. P. Casazza, A. A. Pathan, C. R. Sander, T. E. Asher, D. R. Ambrozak, M. L. Precopio, P. Scheinberg, N. C. Alder, M. Roederer, R. A. Koup, D. C. Douek, A. V. Hill, and H. McShane. 2007. Immunisation with BCG and recombinant MVA85A induces long-lasting, polyfunctional Mycobacterium tuberculosis-specific CD4+ memory T lymphocyte populations. Eur. J. Immunol. 37:3089-3100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blythe, M. J., Q. Zhang, K. Vaughan, R. de Castro, Jr., N. Salimi, H. H. Bui, D. M. Lewinsohn, J. D. Ernst, B. Peters, and A. Sette. 2007. An analysis of the epitope knowledge related to mycobacteria. Immunome Res. 3:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Day, C. L., N. Mkhwanazi, S. Reddy, Z. Mncube, M. van der Stok, P. Klenerman, and B. D. Walker. 2008. Detection of polyfunctional Mycobacterium tuberculosis-specific T cells and association with viral load in HIV-1-infected persons. J. Infect. Dis. 197:990-999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.De Groot, A. S., J. McMurry, L. Marcon, J. Franco, D. Rivera, M. Kutzler, D. Weiner, and B. Martin. 2005. Developing an epitope-driven tuberculosis (TB) vaccine. Vaccine 23:2121-2131. [DOI] [PubMed] [Google Scholar]
- 6.D'Souza, S., M. Romano, J. Korf, X. M. Wang, P. Y. Adnet, and K. Huygen. 2006. Partial reconstitution of the CD4+-T-cell compartment in CD4 gene knockout mice restores responses to tuberculosis DNA vaccines. Infect. Immun. 74:2751-2759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Endsley, J. J., A. Hogg, L. J. Shell, M. McAulay, T. Coffey, C. Howard, C. F. Capinos Scherer, W. R. Waters, B. Nonnecke, D. M. Estes, and B. Villarreal-Ramos. 2007. Mycobacterium bovis BCG vaccination induces memory CD4+ T cells characterized by effector biomarker expression and anti-mycobacterial activity. Vaccine 25:8384-8394. [DOI] [PubMed] [Google Scholar]
- 8.Frank, R. 2002. The SPOT-synthesis technique. Synthetic peptide arrays on membrane supports—principles and applications. J. Immunol. Methods 267:13-26. [DOI] [PubMed] [Google Scholar]
- 9.Gaseitsiwe, S., D. Valentini, R. Ahmed, S. Mahdavifar, I. Magalhaes, J. Zerweck, M. Schutkowski, E. Gautherot, F. Montero, A. Ehrnst, M. Reilly, and M. Maeurer. 2009. Major histocompatibility complex class II molecule-human immunodeficiency virus peptide analysis using a microarray chip. Clin. Vaccine Immunol. 16:567-573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gaseitsiwe, S., D. Valentini, S. Mahdavifar, I. Magalhaes, D. F. Hoft, J. Zerweck, M. Schutkowski, J. Andersson, M. Reilly, and M. J. Maeurer. 2008. Pattern recognition in pulmonary tuberculosis defined by high content peptide microarray chip analysis representing 61 proteins from M. tuberculosis. PLoS ONE 3:e3840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goldfeld, A. E., J. C. Delgado, S. Thim, M. V. Bozon, A. M. Uglialoro, D. Turbay, C. Cohen, and E. J. Yunis. 1998. Association of an HLA-DQ allele with clinical tuberculosis. JAMA 279:226-228. [DOI] [PubMed] [Google Scholar]
- 12.Goletti, D., O. Butera, F. Bizzoni, R. Casetti, E. Girardi, and F. Poccia. 2006. Region of difference 1 antigen-specific CD4+ memory T cells correlate with a favorable outcome of tuberculosis. J. Infect. Dis. 194:984-992. [DOI] [PubMed] [Google Scholar]
- 13.Guyot-Revol, V., J. A. Innes, S. Hackforth, T. Hinks, and A. Lalvani. 2006. Regulatory T cells are expanded in blood and disease sites in patients with tuberculosis. Am. J. Respir. Crit. Care Med. 173:803-810. [DOI] [PubMed] [Google Scholar]
- 14.Hohn, H., C. Kortsik, I. Zehbe, W. E. Hitzler, K. Kayser, K. Freitag, C. Neukirch, P. Andersen, T. M. Doherty, and M. Maeurer. 2007. MHC class II tetramer guided detection of Mycobacterium tuberculosis-specific CD4+ T cells in peripheral blood from patients with pulmonary tuberculosis. Scand. J. Immunol. 65:467-478. [DOI] [PubMed] [Google Scholar]
- 15.Kettaneh, A., L. Seng, K. P. Tiev, C. Toledano, B. Fabre, and J. Cabane. 2006. Human leukocyte antigens and susceptibility to tuberculosis: a meta-analysis of case-control studies. Int. J. Tuberc. Lung Dis. 10:717-725. [PubMed] [Google Scholar]
- 16.Kim, H. S., M. H. Park, E. Y. Song, H. Park, S. Y. Kwon, S. K. Han, and Y. S. Shim. 2005. Association of HLA-DR and HLA-DQ genes with susceptibility to pulmonary tuberculosis in Koreans: preliminary evidence of associations with drug resistance, disease severity, and disease recurrence. Hum. Immunol. 66:1074-1081. [DOI] [PubMed] [Google Scholar]
- 17.Kobayashi, H., M. Wood, Y. Song, E. Appella, and E. Celis. 2000. Defining promiscuous MHC class II helper T-cell epitopes for the HER2/neu tumor antigen. Cancer Res. 60:5228-5236. [PubMed] [Google Scholar]
- 18.Landry, S. J. 2008. Three-dimensional structure determines the pattern of CD4+ T-cell epitope dominance in influenza virus hemagglutinin. J. Virol. 82:1238-1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lanzavecchia, A. 1996. Mechanisms of antigen uptake for presentation. Curr. Opin. Immunol. 8:348-354. [DOI] [PubMed] [Google Scholar]
- 20.Lee, S. Y., and D. Jeoung. 2007. The reverse proteomics for identification of tumor antigens. J. Microbiol. Biotechnol. 17:879-890. [PubMed] [Google Scholar]
- 21.Li, H., P. C. Chien, Jr., M. Tuen, M. L. Visciano, S. Cohen, S. Blais, C. F. Xu, H. T. Zhang, and C. E. Hioe. 2008. Identification of an N-linked glycosylation in the C4 region of HIV-1 envelope gp120 that is critical for recognition of neighboring CD4 T cell epitopes. J. Immunol. 180:4011-4021. [DOI] [PubMed] [Google Scholar]
- 22.Li, H., C. F. Xu, S. Blais, Q. Wan, H. T. Zhang, S. J. Landry, and C. E. Hioe. 2009. Proximal glycans outside of the epitopes regulate the presentation of HIV-1 envelope gp120 helper epitopes. J. Immunol. 182:6369-6378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lombard, Z., D. L. Dalton, P. A. Venter, R. C. Williams, and L. Bornman. 2006. Association of HLA-DR, -DQ, and vitamin D receptor alleles and haplotypes with tuberculosis in the Venda of South Africa. Hum. Immunol. 67:643-654. [DOI] [PubMed] [Google Scholar]
- 24.Middleton, D., L. Menchaca, H. Rood, and R. Komerofsky. 2003. New allele frequency database. Tissue Antigens 61:403-407. [DOI] [PubMed] [Google Scholar]
- 25.Mirano-Bascos, D., M. Tary-Lehmann, and S. J. Landry. 2008. Antigen structure influences helper T-cell epitope dominance in the human immune response to HIV envelope glycoprotein gp120. Eur. J. Immunol. 38:1231-1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mustafa, A. S. 2009. Th1 cell reactivity and HLA-DR binding prediction for promiscuous recognition of MPT63 (Rv1926c), a major secreted protein of Mycobacterium tuberculosis. Scand. J. Immunol. 69:213-222. [DOI] [PubMed] [Google Scholar]
- 27.Mustafa, A. S., A. T. Abal, F. Shaban, A. M. El-Shamy, and H. A. Amoudy. 2005. HLA-DR binding prediction and experimental evaluation of T-cell epitopes of mycolyl transferase 85B (Ag85B), a major secreted antigen of Mycobacterium tuberculosis. Med. Princ. Pract. 14:140-146. [DOI] [PubMed] [Google Scholar]
- 28.Nahtman, T., A. Jernberg, S. Mahdavifar, J. Zerweck, M. Schutkowski, M. Maeurer, and M. Reilly. 2007. Validation of peptide epitope microarray experiments and extraction of quality data. J. Immunol. Methods 328:1-13. [DOI] [PubMed] [Google Scholar]
- 29.Novak, E. J., A. W. Liu, G. T. Nepom, and W. W. Kwok. 1999. MHC class II tetramers identify peptide-specific human CD4(+) T cells proliferating in response to influenza A antigen. J. Clin. Invest. 104:R63-R67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Panina-Bordignon, P., A. Tan, A. Termijtelen, S. Demotz, G. Corradin, and A. Lanzavecchia. 1989. Universally immunogenic T cell epitopes: promiscuous binding to human MHC class II and promiscuous recognition by T cells. Eur. J. Immunol. 19:2237-2242. [DOI] [PubMed] [Google Scholar]
- 31.Ruggiero, G., E. Cosentini, D. Zanzi, V. Sanna, G. Terrazzano, G. Matarese, A. Sanduzzi, F. Perna, and S. Zappacosta. 2004. Allelic distribution of human leucocyte antigen in historical and recently diagnosed tuberculosis patients in Southern Italy. Immunology 111:318-322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Scharn, D., H. Wenschuh, U. Reineke, J. Schneider-Mergener, and L. Germeroth. 2000. Spatially addressed synthesis of amino- and amino-oxy-substituted 1,3,5-triazine arrays on polymeric membranes. J. Comb. Chem. 2:361-369. [DOI] [PubMed] [Google Scholar]
- 33.Seitzer, U., K. Kayser, H. Hohn, P. Entzian, H. H. Wacker, S. Ploetz, H. D. Flad, J. Gerdes, and M. J. Maeurer. 2001. Reduced T-cell receptor CD3zeta-chain protein and sustained CD3epsilon expression at the site of mycobacterial infection. Immunology 104:269-277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Skeiky, Y. A., P. J. Ovendale, S. Jen, M. R. Alderson, D. C. Dillon, S. Smith, C. B. Wilson, I. M. Orme, S. G. Reed, and A. Campos-Neto. 2000. T cell expression cloning of a Mycobacterium tuberculosis gene encoding a protective antigen associated with the early control of infection. J. Immunol. 165:7140-7149. [DOI] [PubMed] [Google Scholar]
- 35.Teran-Escandon, D., L. Teran-Ortiz, A. Camarena-Olvera, G. Gonzalez-Avila, M. A. Vaca-Marin, J. Granados, and M. Selman. 1999. Human leukocyte antigen-associated susceptibility to pulmonary tuberculosis: molecular analysis of class II alleles by DNA amplification and oligonucleotide hybridization in Mexican patients. Chest 115:428-433. [DOI] [PubMed] [Google Scholar]
- 36.Weichold, F. F., S. Mueller, C. Kortsik, W. E. Hitzler, M. J. Wulf, D. M. Hone, J. C. Sadoff, and M. J. Maeurer. 2007. Impact of MHC class I alleles on the M. tuberculosis antigen-specific CD8+ T-cell response in patients with pulmonary tuberculosis. Genes Immun. 8:334-343. [DOI] [PubMed] [Google Scholar]
- 37.Zhou, X., S. L. Bailey-Bucktrout, L. T. Jeker, C. Penaranda, M. Martinez-Llordella, M. Ashby, M. Nakayama, W. Rosenthal, and J. A. Bluestone. 2009. Instability of the transcription factor Foxp3 leads to the generation of pathogenic memory T cells in vivo. Nat. Immunol. 10:1000-1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.