Abstract
The in vivo efficacy of posaconazole against 4 clinical Aspergillus fumigatus isolates with posaconazole MICs ranging from 0.03 to 16 mg/liter, as determined by CLSI method M38A, was assessed in a nonneutropenic murine model of disseminated aspergillosis. The underlying resistance mechanisms of the isolates included substitutions in the cyp51A gene at codon 220 (M220I), codon 54 (G54W), and codon 98 (L98H). The latter was combined with a 34-bp tandem repeat in the gene promoter region (TR L98H). The control isolate exhibited a wild-type phenotype without any known resistance mechanism. Oral posaconazole therapy was started 24 h after infection and was given once daily for 14 consecutive days. Mice were treated with four different doses (1 to 64 mg/kg of body weight), and survival was used as the end point. Survival was dependent both on the dose and on the MIC. The Hill equation with a variable slope fitted the relationship between the dose/MIC ratio and 14-day survival well (R2, 0.92), with a 50% effective dose (ED50) of 29.0 mg/kg (95% confidence interval [CI], 15.6 to 53.6 mg/kg). This also applied to the relationship between the area under the plasma concentration-time curve (AUC)/MIC ratio and 14-day survival (50% effective pharmacodynamic index [EI50], 321.3 [95% CI, 222.7 to 463.4]). Near-maximum survival was reached at an AUC/MIC ratio of nearly 1,000. These results indicate that treatment of infections with A. fumigatus strains for which MICs are 0.5 mg/liter requires doses exceeding the present licensed doses. Increasing the standard dosing regimen may have some effect and may be clinically useful if no alternatives are available.
Over recent years, Aspergillus fumigatus has become the most widespread opportunistic fungal pathogen, causing severe and commonly fatal invasive fungal infections in immunocompromised hosts (2, 4, 15). Management of invasive aspergillosis includes prompt treatment with an appropriate antifungal agent at an adequate dose, but patients may fail to respond for many reasons, including the persistence of the underlying condition and associated neutropenia. Although Aspergillus resistance to antifungal compounds is considered uncommon, treatment failure due to acquired resistance of A. fumigatus has been reported more frequently in recent years than it was formerly (8, 16, 22, 31). Azole resistance has been observed in patients with aspergilloma and cavitary aspergillosis who developed resistance during treatment with azoles, most notably itraconazole (6, 8-10, 13, 22). However, azole resistance has also been reported for patients with invasive aspergillosis (25, 28, 29). In addition to pulmonary infections, cases of disease due to azole-resistant isolates have been reported for a patient with osteomyelitis and patients with central nervous system aspergillosis (12, 27).
Azole antifungals impair the ergosterol biosynthesis pathway via the inhibition of the lanosterol 14α-demethylase, which is a product of the cyp51 gene in A. fumigatus. This enzyme removes the methyl group at position C-14 of precursor sterols. In A. fumigatus, there are two distinct but related cyp51 proteins, encoded by cyp51A and cyp51B (18), respectively. Different modifications in the cyp51 gene appear to be associated with the mechanism of azole resistance. These cyp51 modifications were found to be due to specific mutations in the cyp51A gene, and each mutation is associated with a distinct phenotype. The associated phenotype is commonly characterized by a lack of itraconazole activity, but also by reduced activities of the other azole compounds. A phenotype with no itraconazole or posaconazole activity in vitro has been associated with amino acid substitutions at glycine 54 (G54) (17, 22). A phenotype with no itraconazole activity but elevated voriconazole and posaconazole MICs was linked to different amino acid substitutions at methionine 220 (M220) (6, 19). Another A. fumigatus resistance mechanism involved a base change causing an amino acid substitution in cyp51A at codon 98 in combination with the duplication in tandem of a 34-bp sequence in the cyp51A promoter (TR L98H) (20, 25). The corresponding phenotype was characterized by a lack of itraconazole activity and reduced voriconazole and posaconazole activities.
Given the prominent and increasing role of azoles in the management of Aspergillus diseases, it is important to determine if increased MICs correspond with reduced in vivo efficacy. We investigated the correlation between the in vitro and in vivo activities of posaconazole in a nonneutropenic murine model of disseminated invasive aspergillosis in order to determine the pharmacokinetic (PK)-pharmacodynamic properties of posaconazole. For this purpose we used three clinical isolates with different profiles of susceptibility to azoles, which appear to be related to distinct cyp51A substitutions.
MATERIALS AND METHODS
Isolates.
Four clinical A. fumigatus isolates were used in this study. Clinical isolates with non-wild-type susceptibility included those with the following substitutions in Cyp51A: M220I (isolate identification number, V28-77), G54W (V59-73), and TR L98H (V52-35). A clinical isolate without substitutions in cyp51A was used as a control (AZN8196). For all isolates, the cyp51A substitutions and strain identifications were confirmed by sequence-based analysis as described previously (25) (Table 1). In addition, microsatellite typing of the four isolates by short tandem-repeat typing (16) was performed to confirm that they were genetically distinct. The isolates had been stored in 10% glycerol broth at −80°C and were revived by subculturing on Sabouraud dextrose agar (SAD) supplemented with 0.02% chloramphenicol for 5 to 7 days at 35°C.
TABLE 1.
Origins, in vitro susceptibilities, and underlying azole resistance mechanisms of the A. fumigatus isolates
| Isolate no. | Origin | Prior azole exposure | Cyp51A substitution | MIC or MEC (mg/liter)a |
||||
|---|---|---|---|---|---|---|---|---|
| AMB | ITZ | VCZ | POS | CAS | ||||
| AZN 8196 | Proven invasive aspergillosis | None | 0.5 | 0.125 | 0.25 | 0.031 | 0.25 | |
| V28-77 | Aspergilloma | ITZ | M220I | 0.5 | >16 | 0.25 | 0.5 | 0.25 |
| V52-35 | Proven invasive aspergillosisb | None | TR L98H | 0.5 | >16 | 2 | 0.5 | 0.25 |
| V59-73 | Clinical, disease entity unknown | Unknown | G54W | 0.5 | >16 | 0.125 | >16 | 0.25 |
AMB, amphotericin B; ITZ, itraconazole; VCZ, voriconazole; POS, posaconazole; CAS, caspofungin. For caspofungin, the minimum effective concentration (MEC) was determined; for all other drugs, the MIC was determined.
See reference 29.
Susceptibility testing was performed based on method M38A of the Clinical and Laboratory Standards Institute (CLSI) using a broth microdilution format (23).
Infection model.
A total of 264 outbred CD-1 (Harlan, Horst, The Netherlands) female mice, 4 to 5 weeks old, weighing 20 to 25 g, were randomized into 6 groups (11 mice per group) for the four different A. fumigatus strains. Before the experiment, the isolate was cultured once on SAD for 7 days at 35°C and subcultured twice on 15-cm Takashio slants for 5 days at 35°C. The conidia were harvested in 20 ml of sterile phosphate-buffered saline (PBS) plus 0.1% Tween 80 (Boom B.V., Meppel, The Netherlands). The conidial suspension was filtered through sterile gauze folded four times to remove any hyphae, and the number of conidia was counted in a hemacytometer. After the inoculum was adjusted to the required concentration, the conidial suspension was stored overnight at 4°C. The 90% lethal dose (LD90) was determined for each isolate.
Mice were infected via injection of an inoculum corresponding to the LD90 of the isolate into the lateral tail vein. The LD90s were 2.4 × 107 (wild-type control), 2.5 × 107 (TR L98H mutant), 5 × 107 (M220I mutant), and 1 × 107 (G54W mutant) conidia, respectively. Postinfection viability counts of the injected inocula were determined to ensure that the correct inoculum had been injected. Therapy was begun 24 h after infection and continued for 14 days. A posaconazole (Schering-Plough B.V., Boxmeer, The Netherlands) oral solution was administered in doses of 1, 4, 16, and 64 mg/kg of body weight by oral gavage once daily. Although a dose of 128 mg/kg was used for some groups, it resulted in toxicity and therefore was not studied further. The control group received single doses of saline. On day 15 postinfection, all remaining mice were humanely euthanized under isoflurane anesthesia, and blood was collected through the orbital vein.
The animals were housed under standard conditions, with drink and feed supplied ad libitum. The animal studies were conducted in accordance with the recommendations of the European Community (Directive 86/609/EEC, 24 November 1986), and all animal procedures were approved by the Animal Welfare Committee of Radboud University (RU-DEC 2007-30 and RU-DEC 2008-105).
The infected mice were examined at least three times daily. These clinical inspections were carried out in order to ensure that there were no cases of desiccation, torticollis, staggering, high weight loss (a decrease of 15% within 48 h or 20% within 24 h), or body temperature drop to below 33°C. Mice demonstrating these signs of disease were humanely terminated.
Pharmacokinetic analysis.
A total of 96 outbred CD-1 (Charles River, The Netherlands) female mice, 4 to 5 weeks old, weighing 20 to 22 g, were used for separate PK experiments. On day zero, mice were infected with the wild-type A. fumigatus isolate through the lateral tail vein, and after 24 h, treatment was initiated, as described above, with dosages of 1, 4, 16, or 64 mg/kg. At day 2 of posaconazole treatment (day 3 after infection), blood samples were drawn through the orbital vein into lithium-heparin-containing tubes at 8 predefined time points: immediately before administration of posaconazole and subsequently at 0.5, 1, 2, 4, 8, 12, and 24 h postdose. Blood samples were centrifuged for approximately 10 min at 1,000 × g within 30 min of collection. Plasma was aspirated, transferred in two 5-ml plastic tubes, and stored at −70°C. Posaconazole samples were measured by a validated (for human and mouse matrices) high-performance liquid chromatography (HPLC) method with fluorescence detection. Samples were pretreated using a protein precipitation procedure. The dynamic range of the assay was 0.05 to 10 mg/liter. The assay had an accuracy range (n = 15 replicates), dependent on the concentration, from 97.9% to 104.1%. Intraday precision ranged from 1.56% to 3.03%, and interday precision was between 1.37 and 4.11%. The assay was externally validated by an international proficiency testing program (5).
Arithmetic mean concentrations of posaconazole in plasma from three mice were calculated per time point. Peak concentrations in plasma (Cmax) were directly observed from the data. Pharmacokinetic parameters were derived using noncompartmental analysis with WinNonLin, version 5.2 (Pharsight, Inc). The area under the plasma concentration-time curve (AUC) from time zero to 24 h postinfusion (AUC0-24) was determined by use of the log-linear trapezoidal rule. The elimination rate constant was determined by linear regression of the terminal points of the log-linear plasma concentration-time curve. The terminal half-life was defined as ln2 divided by the elimination rate constant. Clearance (CL) was calculated as dose/AUC0-24.
Statistical analysis.
All data analysis was performed by using the software package of GraphPad Prism, version 5.0, for Windows (GraphPad Software, San Diego, CA). A regression analysis was conducted to determine linearity between dose and AUC. Mortality data were analyzed by the log rank test. The survival data were plotted against dose/MIC and the Hill equation with a variable slope fitted to the data, both for each individual strain and for pooled survival data. The goodness of fit was checked by determination of the R2 and visual inspection. Statistical significance was defined as a P value of <0.05 (two-tailed). Dose/MIC and AUC/MIC ratios were calculated by dividing the dose (in milligrams per kilogram of body weight) or the AUC by the MIC. Dose/MIC and AUC/MIC ratio data were log10 transformed to approximate a normal distribution prior to statistical analysis.
RESULTS
In vitro activity.
The in vitro susceptibility profiles of the four isolates are presented in Table 1. Posaconazole was the most active azole in vitro against the wild-type isolate (MIC, 0.031 mg/liter), but its activity against the M220I and TR L98H mutants (MICs, 0.5 mg/liter) was reduced, and the drug exhibited no significant in vitro activity against the G54W mutant (MIC, >16 mg/liter). All three cyp51A-mutated isolates showed no susceptibility to ITZ, with MICs of >16 mg/liter.
Pharmacokinetic analysis.
Table 2 shows the results of the pharmacokinetic experiments. A total of 96 mice (3 mice per time point, 8 time points, 4 different dosages) were available for pharmacokinetic assessment. All 96 mice were alive at the time of the sample collection. The AUC normalized to a dose of 1 mg/kg resulted in ratios of 10.19, 11.27, 9.96, and 4.64 for dosages of 1, 4, 16, and 64 mg/kg, respectively. The AUC correlated significantly with the dose in a linear fashion from 1 to 16 mg/kg (R2 = 0.99). The dosage of 64 mg/kg resulted in a relatively lower AUC.
TABLE 2.
Pharmacokinetic parameters of posaconazole after doses of 1 to 64 mg/kg administered by oral gavage
| Posaconazole dose (mg/kg) | Value for the following pharmacokinetic parameter (unit)a: |
||||||
|---|---|---|---|---|---|---|---|
| AUC (h·mg/liter) | Dose-normalized AUC [h/(liter·kg)] | CLss/F [liters/(h·kg)] | C24 (mg/liter) | Cavg (mg/liter) | Cmax (mg/liter) | Tmax (h) | |
| 1 | 10.20 | 10.19 | 0.10 | 0.11 (0.05) | 0.42 | 0.98 (0.21) | 4.00 |
| 4 | 45.07 | 11.27 | 0.09 | 0.94 (0.39) | 1.88 | 3.11 (0.68) | 2.00 |
| 16 | 159.42 | 9.96 | 0.10 | 2.70 (0.57) | 6.64 | 9.03 (1.75) | 8.00 |
| 64 | 296.72 | 4.64 | 0.22 | 9.33 (2.77) | 12.36 | 17.83 (4.60) | 8.00 |
For Cmax and the concentration at 24 h (C24), values in parentheses are standard deviations (n = 3).
Survival curves.
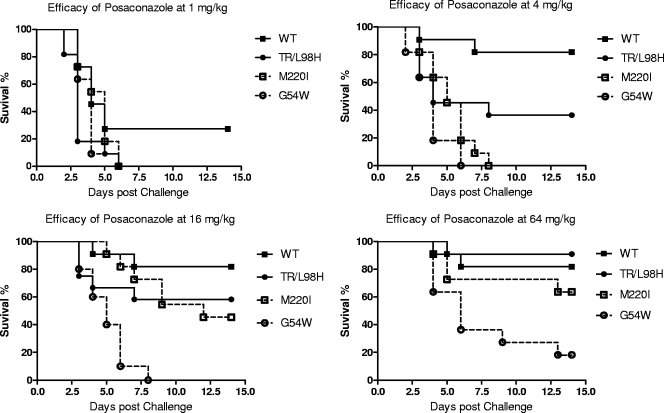
The survival curves for all 4 control groups receiving saline by oral gavage showed a mortality of 90 or 100% and a median survival time of 3 to 3.5 days. Figure 1 shows the survival curves for the 4 isolates by dose. The results show that for each dose, the response decreased as the MIC increased. Similarly, when the dose was increased, an improved response was observed. Table 3 shows a comparison between the various survival curves within each group/strain. This clearly shows that statistically significant differences in survival between treatment and control groups became apparent either when the dose increased or when the MIC was lower. This applied to both the median survival time and the survival rate. The most significant difference was observed between the wild-type and G54W isolates. While the drug was not effective in the infection model at any dose for the G54W mutant, a dose as low as 1 mg/kg had some effect against mice infected with the wild-type isolate, and all higher posaconazole doses had a near-maximum effect for this isolate. The treatment effects on TR L98H and M220I mutant-infected mice were similar, although the response of mice infected with the isolate containing the TR L98H mutation to a 4-mg/kg dose was somewhat higher than that of those infected with the M220I isolate (36.4% versus 0%, respectively).
FIG. 1.
Survival curves of four different isolates of A. fumigatus by posaconazole dose. Shown are data for the wild type (WT) (MIC, 0.031 mg/liter) and for the TR L98H (MIC, 0.5 mg/liter), M220I (MIC, 0.5 mg/liter), and G54W (MIC, >16 mg/liter) mutants.
TABLE 3.
Bonferroni multiple-comparison test for survival curves
| Posaconazole dose (mg/kg) |
P value for the difference between treatment and control groups infected with the following isolatea: |
|||
|---|---|---|---|---|
| WT | M220I mutant | TR L98H mutant | G54W mutant | |
| 64 | <0.0001* | <0.0001* | <0.0001* | <0.0001* |
| 16 | <0.0001* | <0.0001* | 0.0209 | 0.0018* |
| 4 | <0.0001* | 0.0108 | 0.1554 | 0.0724 |
| 1 | 0.0068* | 0.0831 | 0.1554 | 0.0238 |
The Bonferroni Kp value for 4 multiple comparisons was 0.01. P values of ≤0.01, which indicate a significant difference in survival rates between treatment and control groups, are asterisked. WT, wild type.
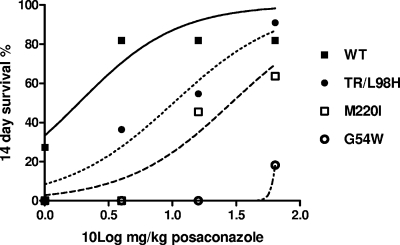
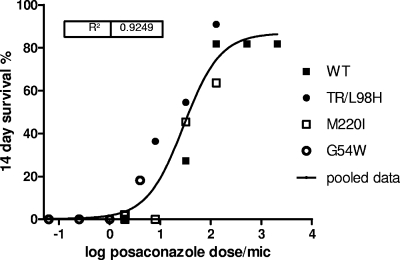
Dose-response analysis.
The dose-response curves for each of the four posaconazole dosing regimens and controls for all four strains are shown in Fig. 2. Posaconazole treatment improved the survival of the mice in a dose-dependent manner for all four isolates. Compared to that for the wild-type control, the dose-response curves of mice infected with the M220I or TR L98H mutant were shifted to the right, indicating that higher doses of posaconazole were required to achieve efficacy similar to those for the wild-type-infected mice, while a maximal response against the G54W strain could not be reached even in mice treated with the highest posaconazole dose. A dose/MIC-survival plot for all four strains is depicted in Fig. 3. The data indicated a clear sigmoidal dose-response relationship. The Hill-type model fitted the data well, with an R2 of 0.92. The 50% effective dose (ED50) was 29.0 mg/kg (95% confidence interval [CI], 15.6 to 53.6 mg/kg). This indicates a direct relationship between MIC, dose, and effect. In total, 82% of the mice were cured when the dose/MIC ratio was ≥130.
FIG. 2.
Fourteen-day survival as a function of posaconazole dose for 4 A. fumigatus isolates. Shown are data for the wild type (WT) (MIC, 0.031 mg/liter) and for the TR L98H (MIC, 0.5 mg/liter), M220I (MIC, 0.5 mg/liter), and G54W (MIC, >16 mg/liter) mutants. The curves indicate fits with the Hill equation for each isolate.
FIG. 3.
Fourteen-day survival as a function of the posaconazole dose/MIC ratio for 4 A. fumigatus isolates. Shown are data for the wild type (WT) (MIC, 0.031 mg/liter) and for the TR L98H (MIC, 0.5 mg/liter), M220I (MIC, 0.5 mg/liter), and G54W (MIC, >16 mg/liter) mutants. The curve is the model fit with the Hill equation for pooled data.
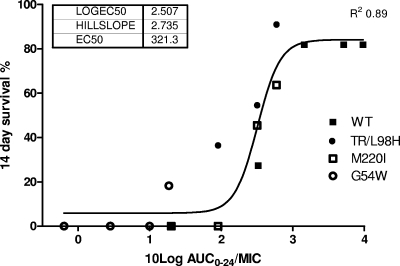
Exposure-response analysis.
The AUC for each dose, as determined from the pharmacokinetic experiments, was used to calculate the AUC from 0 to 24 h (AUC0-24)/MIC ratios for each strain. These are shown in Fig. 4. Like the dose-response relationship, the exposure-response relationship had a sigmoidal shape. The Hill model with a variable slope fitted the data well, with an R2 of 0.88. The 50% effective pharmacodynamic index (EI50) was 321.3 (95% CI, 222.7 to 463.4). Near-maximum survival was reached at a AUC/MIC ratio of nearly 1,000. We also determined the Cmax/MIC-response relationship. Because we used a once-daily dose only, this relationship was comparable to the AUC/MIC relationship. However, the R2 of the model fit was slightly less, 0.84, because of pharmacokinetic differences between doses.
FIG. 4.
Fourteen-day survival as a function of the posaconazole AUC/MIC ratio for 4 A. fumigatus isolates. Shown are data for the wild type (WT) (MIC, 0.031 mg/liter) and for the TR L98H (MIC, 0.5 mg/liter), M220I (MIC, 0.5 mg/liter), and G54W (MIC, >16 mg/liter) mutants. The curve is the model fit with the Hill equation for pooled data.
DISCUSSION
We investigated the comparative efficacies of various regimens of posaconazole against clinical A. fumigatus cyp51A-mutated isolates in a nonneutropenic murine model of disseminated aspergillosis. We believe that this research question is highly relevant, because the azoles are the main drug class for the management of invasive aspergillosis and the only class that can be administered orally. Our study shows that the MIC of the isolate has a major impact on the efficacy of posaconazole, an agent shown to be highly active in vitro and in animal models of invasive aspergillosis due to wild-type A. fumigatus isolates. We observed a 50% loss of efficacy in those isolates harboring cyp51A substitutions, i.e., the TR L98H and M220I substitutions, associated with a phenotype that increased the MIC of posaconazole by four 2-fold dilution steps, from 0.03 to 0.5 mg/liter. While this loss of efficacy was completely or partly compensated for by increasing the posaconazole dose, the drug showed no meaningful efficacy in mice infected with the G54W-containing isolate, which exhibited no in vitro susceptibility to posaconazole.
Recently, Arendrup et al. (3) showed reduced efficacy of posaconazole in a neutropenic murine model of invasive aspergillosis against a multiazole-resistant A. fumigatus isolate (posaconazole MIC, 4 mg/liter), genetically identified as an M220K mutant of the cyp51A gene. However, the study did not investigate a full dose range of posaconazole. In our study, treatment with posaconazole significantly prolonged survival at a dose of 64 mg/kg for mice infected with the TR L98H or M220I mutated isolate as well as for those infected with the wild-type control isolate. Interestingly, although the TR L98H and M220I isolates had the same MIC, efficacy comparable to that for the mice infected with the wild-type isolate could be achieved only with the TR L98H isolate at a higher posaconazole dose, and not at all with the M220I isolate. This suggests that the underlying resistance mechanism may have an impact on drug efficacy in addition to the phenotype, i.e., MIC. This topic requires further investigation, since our study was not sufficiently powered to determine significant differences between the TR L98H and M220I isolates. Also, other factors, such as the presence of virulence factors or the fitness of the different isolates, might be important. In this respect, our model did not reveal significant differences in inoculum size and survival between wild-type isolates and those with Cyp51A mutations, although additional studies of the impact of mutations on the fitness of isolates are warranted.
A previous study with a murine model of candidiasis (1) demonstrated that the pharmacokinetic behavior of posaconazole was nonlinear for single administrations of doses within the range of 20 to 320 mg/kg. Our investigation revealed a linear PK profile for multiple posaconazole administrations in doses as high as 16 mg/kg. As with humans (7), the plasma drug concentration for the 1- to 16-mg/kg dose range increased proportionally to the dose. Nomeir and colleagues (24) studied single administrations of posaconazole in the dose range of 20 to 160 mg/kg and reported that the dose-related increase in the AUC was slower than that in Cmax, which was explained by slower absorption at higher doses. We observed the same Cmax effect within the dose-range of 1 to 64 mg/kg. In addition, there was a 2-fold increase in oral clearance (CLss/F) at a dose of 64 mg/kg. This was an unexpected finding, since the limited metabolism of posaconazole is mediated predominantly through the UDP-glucuronosyltransferase (UGT) enzyme pathway (11) and not through both the UGT and CYP (cytochrome P450) pathways, as usually reported in the literature on the metabolism of most hepatically cleared xenobiotics and endobiotics. In humans, only 15% of the total posaconazole dose is metabolized, and the majority of the metabolites are glucuronide conjugates (14), excreted mostly in feces. Therefore, it was more likely that for mice, oral clearance would remain unchanged with an increase in dose. However, since no data have been obtained after administration with full bioavailability, it is not clear whether lower AUCs are due to increased clearance or to lower absorption. These findings do indicate that it is important to use AUCs based on measured pharmacokinetic profiles rather than the dose as a measure of drug exposure.
Given that the pharmacokinetic profile of posaconazole in both humans and mice is near-linear, an important question is whether we could use the observations from our murine model to predict if humans with azole-resistant aspergillosis can still be treated with posaconazole, and which doses are needed to result in efficacy. In our studies, maximum survival was achieved for mice infected with the wild-type isolate, with a MIC of 0.031 mg/liter. This corresponded with an AUC/MIC ratio of around 1,000 for total drug. This value is comparable to the AUC/MIC ratios for Candida species found by Andes and colleagues (1) and indicates that the pharmacokinetic/pharmacodynamic relationships found for yeasts are comparable to those for A. fumigatus. We did not determine the degree of protein binding of posaconazole in our model, but at present there are no indications that protein binding of posaconazole in humans and mice differ to a great extent, and that for mice is 98 to 99% (1). In fact, the dose-normalized AUC values are similar in mice and humans, around 10 per mg/kg in both cases, at least as determined with human volunteers (7). Thus, for strains for which MICs are 0.5 mg/liter, a 50-mg/kg dose of posaconazole would be needed for an optimal effect, or 4 g per day for a human weighing 80 kg if the survival end point used in this study is meaningful for predicting clinical outcome. While this is not feasible at present, the AUC/MIC relationship also indicates that some effect is reached at ratios of 100, or 400 mg/day. The EI50 was 321, and this is reached with 1,200 mg per day. Thus, if no alternative treatment option is available, higher doses of posaconazole may in part overcome the decreased susceptibility. The AUC/MIC relationship can also be used to determine optimal doses for patients who have a higher clearance or who display nonlinear exposure-dose relationships. For instance, Ullmann and colleagues (26) administered posaconazole to bone marrow transplant (BMT) patients and other patients with probable fungal infections, and the total drug AUC0-24 levels were at least 4-fold less than those for healthy volunteers (7), even though posaconazole doses were higher than 800 mg. The AUCs obtained were, however, sufficient to treat wild-type isolates.
With respect to the discussion above, two issues should be noted. The first is that we used survival as an end point. While this is the most stringent measure of drug efficacy, there are some caveats, as discussed elsewhere (21, 30). The second is that we used an intravenous model and therefore studied disseminated aspergillosis, while most human infections are pulmonary infections, in which dissemination, if present, is from the lungs. It would be interesting to determine whether the effects observed in a pulmonary model would corroborate those found here with respect to the pharmacodynamic target.
We conclude that our model supports the view that the efficacy of posaconazole treatment in A. fumigatus is dependent both on drug exposure and on the MIC for the isolate, as with other antifungal drugs (21, 30). In addition, the quantitative relationship between exposure and effect is comparable to that found for Candida strains (1). These relationships can be used to optimize the treatment of human infections.
Acknowledgments
Part of this research was supported by an unrestricted grant from Schering-Plough.
Footnotes
Published ahead of print on 16 November 2009.
REFERENCES
- 1.Andes, D., K. Marchillo, R. Conklin, G. Krishna, F. Ezzet, A. Cacciapuoti, and D. Loebenberg. 2004. Pharmacodynamics of a new triazole, posaconazole, in a murine model of disseminated candidiasis. Antimicrob. Agents Chemother. 48:137-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Andriole, V. T. 1993. Infections with Aspergillus species. Clin. Infect. Dis. 17(Suppl. 2):S481-S486. [DOI] [PubMed] [Google Scholar]
- 3.Arendrup, M. C., S. Perkhofer, S. J. Howard, G. Garcia-Effron, A. Vishukumar, D. Perlin, and C. Lass-Florl. 2008. Establishing in vitro-in vivo correlations for Aspergillus fumigatus: the challenge of azoles versus echinocandins. Antimicrob. Agents Chemother. 52:3504-3511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beck-Sagué, C., and W. R. Jarvis. 1993. Secular trends in the epidemiology of nosocomial fungal infections in the United States, 1980-1990. J. Infect. Dis. 167:1247-1251. [DOI] [PubMed] [Google Scholar]
- 5.Brüggemann, R. J. M., D. J. Touw, R. E. Aarnoutse, P. E. Verweij, and D. M. Burger. 2009. International interlaboratory proficiency testing program for measurement of azole antifungal plasma concentrations. Antimicrob. Agents Chemother. 53:303-305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen, J., H. Li, R. Li, D. Bu, and Z. Wan. 2005. Mutations in the cyp51A gene and susceptibility to itraconazole in Aspergillus fumigatus serially isolated from a patient with lung aspergilloma. J. Antimicrob. Chemother. 55:31-37. [DOI] [PubMed] [Google Scholar]
- 7.Courtney, R., S. Pai, M. Laughlin, J. Lim, and V. Batra. 2003. Pharmacokinetics, safety, and tolerability of oral posaconazole administered in single and multiple doses in healthy adults. Antimicrob. Agents Chemother. 47:2788-2795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dannaoui, E., E. Borel, M. F. Monier, M. A. Piens, S. Picot, and F. Persat. 2001. Acquired itraconazole resistance in Aspergillus fumigatus. J. Antimicrob. Chemother. 47:333-340. [DOI] [PubMed] [Google Scholar]
- 9.Dannaoui, E., D. Garcia-Hermoso, J. M. Naccache, I. Meneau, D. Sanglard, C. Bouges-Michel, D. Valeyre, and O. Lortholary. 2006. Use of voriconazole in a patient with aspergilloma caused by an itraconazole-resistant strain of Aspergillus fumigatus. J. Med. Microbiol. 55:1457-1459. [DOI] [PubMed] [Google Scholar]
- 10.Denning, D. W., K. Venkateswarlu, K. L. Oakley, M. J. Anderson, N. J. Manning, D. A. Stevens, D. W. Warnock, and S. L. Kelly. 1997. Itraconazole resistance in Aspergillus fumigatus. Antimicrob. Agents Chemother. 41:1364-1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ghosal, A., N. Hapangama, Y. Yuan, J. Chanfuo-Yeboah, R. Iannucci, S. Chowdhury, K. Alton, J. E. Patrick, and S. Zbaida. 2004. Identification of human UDP-glucuronosyltransferase enzyme(s) responsible for the glucuronidation of posaconazole (Noxafil). Drug Metab. Dispos. 32:267-271. [DOI] [PubMed] [Google Scholar]
- 12.Hodiamont, C., K. Dolman, I. Ten Berge, W. Melchers, P. Verweij, and D. Pajkrt. 2009. Multiple-azole-resistant Aspergillus fumigatus osteomyelitis in a patient with chronic granulomatous disease successfully treated with long-term oral posaconazole and surgery. Med. Mycol. 47:217-220. [DOI] [PubMed] [Google Scholar]
- 13.Howard, S. J., D. Cerar, M. J. Anderson, A. Albarrag, M. C. Fisher, A. C. Pasqualotto, M. Laverdiere, M. C. Arendrup, D. S. Perlin, and D. W. Denning. 2009. Azole resistance in Aspergillus fumigatus associated with treatment failure. Emerg. Infect. Dis. 15(7). http://www.cdc.gov/EID/content/15/7/1068.htm. [DOI] [PMC free article] [PubMed]
- 14.Krieter, P., B. Flannery, T. Musick, M. Gohdes, M. Martinho, and R. Courtney. 2004. Disposition of posaconazole following single-dose oral administration in healthy subjects. Antimicrob. Agents Chemother. 48:3543-3551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Latgé, J. P. 1999. Aspergillus fumigatus and aspergillosis. Clin. Microbiol. Rev. 12:310-350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Manavathu, E. K., J. L. Cutright, D. Loebenberg, and P. H. Chandrasekar. 2000. A comparative study of the in vitro susceptibilities of clinical and laboratory-selected resistant isolates of Aspergillus spp. to amphotericin B, itraconazole, voriconazole and posaconazole (SCH 56592). J. Antimicrob. Chemother. 46:229-234. [DOI] [PubMed] [Google Scholar]
- 17.Mann, P. A., R. M. Parmegiani, S. Q. Wei, C. A. Mendrick, X. Li, D. Loebenberg, B. DiDomenico, R. S. Hare, S. S. Walker, and P. M. McNicholas. 2003. Mutations in Aspergillus fumigatus resulting in reduced susceptibility to posaconazole appear to be restricted to a single amino acid in the cytochrome P450 14α-demethylase. Antimicrob. Agents Chemother. 47:577-581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mellado, E., T. M. Az-Guerra, M. Cuenca-Estrella, and J. L. Rodriguez-Tudela. 2001. Identification of two different 14-α sterol demethylase-related genes (cyp51A and cyp51B) in Aspergillus fumigatus and other Aspergillus species. J. Clin. Microbiol. 39:2431-2438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mellado, E., G. Garcia-Effron, L. Cazar-Fuoli, M. Cuenca-Estrella, and J. L. Rodriguez-Tudela. 2004. Substitutions at methionine 220 in the 14α-sterol demethylase (Cyp51A) of Aspergillus fumigatus are responsible for resistance in vitro to azole antifungal drugs. Antimicrob. Agents Chemother. 48:2747-2750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mellado, E., G. Garcia-Effron, L. Cazar-Fuoli, W. J. G. Melchers, P. E. Verweij, M. Cuenca-Estrella, and J. L. Rodriguez-Tudela. 2007. A new Aspergillus fumigatus resistance mechanism conferring in vitro cross-resistance to azole antifungals involves a combination of cyp51A alterations. Antimicrob. Agents Chemother. 51:1897-1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mouton, J. W., D. T. A. Te Dorsthorst, J. F. G. M. Meis, and P. E. Verweij. 29 January 2009. Dose-response relationships of three amphotericin B formulations in a non-neutropenic murine model of invasive aspergillosis. Med. Mycol. 209:1-7. [Epub ahead of print.] [DOI] [PubMed] [Google Scholar]
- 22.Nascimento, A. M., G. H. Goldman, S. Park, S. A. E. Marras, G. Delmas, U. Oza, K. Lolans, M. N. Dudley, P. A. Mann, and D. S. Perlin. 2003. Multiple resistance mechanisms among Aspergillus fumigatus mutants with high-level resistance to itraconazole. Antimicrob. Agents Chemother. 47:1719-1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Committee for Clinical Laboratory Standards. 1998. Reference method for broth dilution antifungal susceptibility testing of conidium-forming filamentous fungi; proposed standard. National Committee for Clinical Laboratory Standards, Wayne, PA.
- 24.Nomeir, A. A., P. Kumari, M. J. Hilbert, S. Gupta, D. Loebenberg, A. Cacciapuoti, R. Hare, G. H. Miller, C. C. Lin, and M. N. Cayen. 2000. Pharmacokinetics of SCH 56592, a new azole broad-spectrum antifungal agent, in mice, rats, rabbits, dogs, and cynomolgus monkeys. Antimicrob. Agents Chemother. 44:727-731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Snelders, E., H. A. van der Lee, J. Kuijpers, A. J. Rijs, J. Varga, R. A. Samson, E. Mellado, A. R. Donders, W. J. Melchers, and P. E. Verweij. 2008. Emergence of azole resistance in Aspergillus fumigatus and spread of a single resistance mechanism. PLoS Med. 5:e219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ullmann, A. J., O. A. Cornely, A. Burchardt, R. Hachem, D. P. Kontoyiannis, K. Topelt, R. Courtney, D. Wexler, G. Krishna, M. Martinho, G. Corcoran, and I. Raad. 2006. Pharmacokinetics, safety, and efficacy of posaconazole in patients with persistent febrile neutropenia or refractory invasive fungal infection. Antimicrob. Agents Chemother. 50:658-666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.van der Linden, J. W. M., R. R. Jansen, D. Bresters, C. E. Visser, S. E. Geerlings, E. J. Kuijper, W. J. G. Melchers, and P. E. Verweij. 2009. Azole-resistant central nervous system aspergillosis. Clin. Infect. Dis. 48:1111-1113. [DOI] [PubMed] [Google Scholar]
- 28.van Leer-Buter, C., R. P. Takes, K. M. Hebeda, W. J. Melchers, and P. E. Verweij. 2007. Aspergillosis—and a misleading sensitivity result. Lancet 370:102. [DOI] [PubMed] [Google Scholar]
- 29.Verweij, P. E., E. Mellado, and W. J. Melchers. 2007. Multiple-triazole-resistant aspergillosis. N. Engl. J. Med. 356:1481-1483. [DOI] [PubMed] [Google Scholar]
- 30.Verweij, P. E., D. T. Te Dorsthorst, W. H. Janssen, J. F. Meis, and J. W. Mouton. 2008. In vitro activities at pH 5.0 and pH 7.0 and in vivo efficacy of flucytosine against Aspergillus fumigatus. Antimicrob. Agents Chemother. 52:4483-4485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Warris, A., C. M. Weemaes, and P. E. Verweij. 2002. Multidrug resistance in Aspergillus fumigatus. N. Engl. J. Med. 347:2173-2174. [DOI] [PubMed] [Google Scholar]