Abstract
The absence of a validated surrogate marker for the immune state has complicated the design of a subunit vaccine against asexual stages of Plasmodium falciparum. In particular, it is not known whether the capacity to induce antibodies that inhibit parasite growth in vitro is an important criterion for selection of P. falciparum proteins to be assessed in human vaccine trials. We examined this issue in the Plasmodium yoelii rodent malaria model using the 19-kDa C-terminal fragment of merozoite surface protein 1 (MSP119). To examine the relationship between inhibitory antibodies in immunized mice and the immune state, as indicated by resistance to a blood-stage challenge, we used an allelic replacement strategy to generate a transgenic P. falciparum line that expresses MSP119 from P. yoelii. We show that MSP119 is functionally conserved across these two divergent Plasmodium species, and replacing PfMSP119 with PyMSP119 has no detectable effect on parasite growth in vitro. By comparing growth rates of this transgenic line with a matched transgenic line that expresses the endogenous PfMSP119, we developed an assay to measure the specific growth-inhibitory activity directed exclusively to the PyMSP119 protein in the sera from vaccinated animals. To validate this assay, sera from rabbits immunized with recombinant PyMSP119 were tested and showed specific inhibitory activity in a concentration-dependent manner. In mice that were immunized with recombinant PyMSP119, the levels of PyMSP119-specific inhibitory activity did not correlate with the total antibody levels measured by enzyme-linked immunosorbent assay. Furthermore, they did not correlate with resistance to subsequent blood-stage infection, and some mice with complete protection showed no detectable inhibitory activity in their prechallenge sera. These data indicated that growth-inhibitory activity measured in vitro was not a reliable predictor of immune status in vivo, and the reliance on this criterion to select vaccine candidates for human clinical trials may be misplaced. The transgenic lines further offer useful tools for comparing the efficacy of MSP119-based vaccines that utilize different immunization regimens and antigen formulations.
Infection of humans by Plasmodium falciparum is the cause of severe morbidity and mortality, leading to millions of deaths annually, predominantly in children under 5 years of age. Invasion of red blood cells by asexual-stage parasites is the stage of infection associated with clinical signs and symptoms. Much effort has been directed to the development of a subunit vaccine against asexual blood stages. However, progress has been slow and is hampered by the large number of candidate antigens and alternative modalities of immunization, the complexities of antigen combinations, and the high cost of clinical trials involving good manufacturing practices recombinant protein. There is considerable uncertainty as to how to prioritize the large number of new candidate vaccine molecules revealed by genomic, transcriptomic, and proteomic studies (5). Attention has focused on properties such as location and accessibility to antibodies, efficacy in model systems, sero-epidemiological correlates in clinically immune humans, and coding sequence conservation. Production of antibodies capable of inhibiting parasite growth in vitro by sera raised in experimental animals appears to be a desirable property, but it is not clear whether this should be a prerequisite for selection as a vaccine candidate (27, 36). In particular, there are limited data as to whether this ability correlates closely with protection in model systems. We set out to examine this important relationship in a well-regarded host-parasite system using one of the leading subunit vaccine candidates.
Merozoite surface protein 1 (MSP1) is one of the proteins involved in red blood cell invasion by the parasite, and the 19-kDa C-terminal fragment of this protein (MSP119) is a leading vaccine candidate. Studies in rodent and nonhuman primate models have shown that passive transfer with anti-MSP119 antibodies or immunization with recombinant MSP119 can provide significant protection against lethal challenge (9, 21, 25, 37). Antibodies to MSP119, either affinity purified from immune human sera or monoclonal or polyclonal experimental sera, are capable of inhibiting parasite growth in vitro (3, 12, 32). In field studies, naturally acquired anti-MSP119 antibodies have been shown to be associated with protection from P. falciparum infection (1, 13, 33). However, the correlation between MSP119-specific antibodies and in vivo protection remains unclear. For example, high levels of anti-MSP119 antibodies passively transferred to mice or monkeys were not invariably associated with protection against parasite infection (15, 17), and a lack of correlation between MSP119-specific antibodies in immune humans and their clinical immunity has been reported in several field settings (11, 34). In addition, antibodies directed against MSP119 have been shown to have variable effects on parasite growth, ranging from inhibition to enhancement (16, 28). These findings point out the limitations of using conventional antibody-based detection methods, such as an enzyme-linked immunosorbent assay (ELISA), for the evaluation of the immune status of a subject induced either by natural exposure or by vaccination.
In an attempt to elucidate the relationship between specific antibody levels and functional capacity, O'Donnell et al. used an allelic replacement approach to generate a P. falciparum parasite line that expresses the MSP119 region from the distantly related rodent malaria species Plasmodium chabaudi (30). By comparing the growth rate of this transgenic parasite line with that of a matched transgenic line that expresses the endogenous P. falciparum MSP119, the fraction of inhibitory activity attributable to MSP119-specific antibodies can be determined. Using this assay, O'Donnell et al. reported that MSP119-specific antibodies are a major component of the total inhibitory response in the serum samples from long-term residents living in areas where malaria is endemic in Papua New Guinea (29). Further analysis of a longitudinal cohort of Kenyans indicated that the presence of growth-inhibitory antibodies to MSP119 correlated with the presence of clinical immunity to malaria (19). However, there is uncertainty about whether this can serve as an accurate correlate of protection (6).
The availability of this transgenic parasite line also provides a potential tool to measure MSP119-specific inhibitory antibodies induced by immunization with P. chabaudi MSP119 and assess their possible correlation with the protective status of the immunized mice. However, P. chabaudi is not widely used as a model in MSP119-based vaccine trials, as control of P. chabaudi infection can be achieved by T-cell-dependent mechanisms (22, 24). P. yoelii is considered a superior model, because immunity to this rodent malaria species is predominantly antibody mediated, similar to P. falciparum infection (7, 17, 18, 24, 35). In the present study, we used allelic replacement to generate a P. falciparum parasite line that expresses the MSP119 region from P. yoelii. This new transgenic line allows us to address the relationship between induction of antibodies capable of inhibiting parasite invasion and protective efficacy in a well-studied and tractable experimental model.
MATERIALS AND METHODS
Plasmid construction.
Plasmid pPyMEGF was constructed using a similar approach to that used in the construction of pPcMEGF (29), except that a 300-bp region from PyMSP119 (encoding the two epidermal growth factor-like domains and the glycosylphosphatidylinositol anchor attachment site) was fused to the 900-bp internal region of PfMSP1. To generate the chimeric MSP1 molecule, splice overlap extension PCR was performed using primers p1772 (5′-ATTTCTCGAGAATCCGAAGATAATGACGAATATTTAG-3′), p1773 (5′-GAATATCTCTTGTATCAACACATTGGTGTTGTGAAATGTTTAAC-3′), p1774 (5′-GTTAAACATTTCACAACACCAATGTGTTGATACAAGAGATATTC-3′), and p1775 (5′-TCACTCGAGTTAAAATATATTAAATACAATTAATGTG-3′). Briefly, the 900-bp internal MSP1 fragment was amplified from P. falciparum D10 genomic DNA using primers p1772 and p1773, and the 300-bp PyMSP119 was amplified from P. yoelii YM genomic DNA using primers p1774 and p1775. The two PCR products were joined together to generate a 1,200-bp hybrid product during a third PCR using primers p1772 and p1775. This hybrid product was digested with XhoI and cloned into plasmid pHC2 (Fig. 1A). Two plasmids (pPyMEGF-1 and pPyMEGF-2) were generated containing the insert in forward and reverse orientation, respectively. The plasmids were sequenced to confirm the correct orientation of the insert and absence of mutations.
FIG. 1.
(A) Schematic of the plasmid and the outcome of integration into P. falciparum D10 parasites. Plasmid pPyMEGF was constructed by ligating a chimeric MSP1 molecule (the PfMSP1 gene target with its C-terminal 19-kDa fragment [gray box] replaced with PyMSP119 [black box]) into transfection vector pHC2. The Tg-DHFR selectable marker cassette and Hsp86 3′ UTR are shown. (B) Outcome of amplification using different sets of primers on the following samples: no DNA control (lanes 1), D10 genomic DNA (lanes 2), plasmid pPyMEGF-1 (forward insert orientation) (lanes 3), plasmid pPyMEGF-2 (reverse insert orientation) (lanes 4), genomic DNA from PyMEGF-1 (lanes 5), PyMEGF-2 (lanes 6) after the second round of drug cycling. DNA standards (in bp) are shown on the left. The locations of the primers are shown in panel A.
Parasite culture and transfection.
Synchronization of P. falciparum parasites and transfection were performed using standard procedures (14). Briefly, purified plasmid DNA (PyMEGF-1 or PyMEGF-2) was electroporated into synchronized rings of P. falciparum D10 under low-voltage/high-capacitance conditions. Transfected parasites were initially selected on 0.1 μM pyrimethamine for 4 weeks, then subjected to repeated cycles of 1 μM pyrimethamine for 4 weeks followed by drug removal for 3 to 4 weeks. The parasites containing integrated plasmids were cloned by limiting dilution procedure. Genomic DNA was extracted from the transfectant parasite lines, together with the parental line D10 and D10-PfM3′ (kindly provided by Brendan Crabb) (30). PCR was performed using four pairs of primers (Fig. 1A): p1772/p1773, p1774/p1775, p1836/p1837, and p1836/p1775 (p1836, 5′-GTGAAAATAATAAGAAAGTTAACGAAGC-3′; p1837, 5′-GTATATTGGGGTGATGATAAAATGAAAG-3′).
Western blot analysis.
Parasites from D10, D10-PyMEGF, and D10-PfM3′ were isolated from asynchronous culture by saponin lysis. Parasite lysates were separated on 15% SDS-PAGE gels, transferred onto a polyvinylidene difluoride membrane, and probed with either polyclonal rabbit antibodies to PyMSP119 (S5935; 1:500 dilution) or a monoclonal antibody to PfMSP119 (mAb1E1; 1:5,000 dilution). Anti-rabbit and anti-mouse immunoglobulin antibodies conjugated to horseradish peroxidase (Chemicon) were used for detection, and bands were visualized by enhanced chemiluminescence (Roche).
Immunofluorescence assays (IFA).
D10-PyMEGF and D10-PfM3′ parasites were incubated with a mixture of mAb1E1 and S5935, diluted at 1:2,500 and 1:5,000, respectively. A mixture of Alexa Fluor 488 goat anti-mouse IgG and Alexa Fluor 568 goat anti-rabbit IgG (Invitrogen; both diluted at 1:500) was used for detection, and parasites were visualized by fluorescence microscopy. To observe the parasite nucleus, DNA staining was performed with 4′,6-dimaminidino-2-phenylindole (DAPI).
Growth rate assay.
Parasites from D10, D10-PyMEGF, and D10-PfM3′ were synchronized twice with sorbitol at a 4-h interval, then cultured in the presence of pyrimethamine for 8 days (starting with 0.5% rings on day 1). Cultures were diluted 1:5 with fresh medium and red blood cells at 2% hematocrit every 32 h, and blood smears were taken twice a day at the same times each day to determine parasitemia.
Generation of rabbit anti-PyMSP119 antibodies.
PyMSP119 was expressed either as a glutathione S-transferase (GST) fusion protein in Escherichia coli (GST-PyMSP119) or as a hexahistidine-tagged fusion in Saccharomyces cerevisiae (yPyMSP119) (20, 38). To generate PyMSP119-specific antibodies, two female New Zealand White rabbits were injected subcutaneously with 100 μg of GST-PyMSP119 or 50 μg of yPyMSP119, emulsified in complete Freund's adjuvant. Four subsequent immunizations with incomplete Freund's adjuvant were administered at monthly intervals, and sera were collected 2 weeks after the final injection (S5934 and S5935).
Immunization of mice and challenge infection.
Immunization of mice with recombinant PyMSP119 and the subsequent challenge infection were performed as previously described (20, 39). Briefly, BALB/c mice (females, 6 to 8 weeks old) were immunized intraperitoneally with 25 μg or 10 μg of purified recombinant PyMSP119 emulsified in complete Freund's adjuvant. Two subsequent immunizations were delivered at monthly intervals with the same antigen but emulsified in incomplete Freund's adjuvant. Control mice were immunized with phosphate-buffered saline (PBS) in Freund's adjuvants at the same schedule. Sera were collected 10 days after the third immunization. At 2 weeks after the third immunization, mice were challenged intraperitoneally with 105 P. yoelii YM-parasitized red blood cells (RBCs). Blood smears were collected daily starting at day 3, and parasitemias were monitored microscopically.
ELISAs.
PyMSP119-specific antibodies in sera were measured by ELISA as described previously (39). Recombinant yPyMSP119 was used to coat microtiter plates, and sera were tested at a 1:10,000 dilution. The optical density (OD) was read at 405 nm, and the background OD values from PBS-coated plates were subtracted from values obtained from antigen-coated plates.
Invasion inhibition assays.
The invasion inhibition assays were performed as described previously (29), except that D10-PyMEGF was used instead of D10-PcMEGF. Briefly, ring-stage parasites from D10-PyMEGF and D10-PfM3′ were synchronized by sorbitol lysis twice at a 4-h interval, and the assay was set up after incubation for 24 h, at which time parasites had matured to late trophozoites/schizonts. A total volume of 100 μl (for rabbit sera) or 50 μl (for mouse sera) was set up with 0.5 to 1% parasitemia and a 1% hematocrit. Sera were added to a final concentration of 2.5 to 50% for rabbit sera and 10% for mouse sera. All sera were heat inactivated at 56°C for 30 min and preabsorbed against uninfected human RBCs before use. Each serum sample was tested in triplicate on both lines in 96-well microtiter plates. After incubation for 40 to 44 h, late trophozoites or schizont-stage parasites were harvested, fixed with 0.025% glutaraldehyde, and stained with 10 to 15 μg/ml propidium iodide (PI). The parasites were then subjected to a FC500 Beckman Coulter Cytometry Analyser (Becton Dickinson) with a 488-nm laser for excitation and FL-3 channel (670 nm) for emission. One hundred thousand cells were counted for each sample. Uninfected RBCs stained with PI were used to set the gating, with the average area set to be ≤0.05%. Parasitemias were calculated by batch analysis using the FC500 CXP analysis software (Becton Dickinson). The parasite invasion rate was expressed as a percentage of the mean parasitemia observed in parallel cultures of each parasite line in the presence of control sera (prebleed sera). Net inhibition attributable to PyMSP119-specific antibodies was calculated by subtracting the invasion rate of D10-PyMEGF from that of D10-PfM3′. Antibodies specific for P. falciparum apical membrane antigen 1 (AMA-1) were used as a control inhibitory serum that inhibited both transgenic parasite lines to the same degree.
Statistical analyses.
Statistical analyses were performed using Prism 5 software (Gradhpad Software Inc.). Spearman's rank correlation test was used to assess the correlation between inhibitory activity, antibody levels, and parasitemias. The Mann-Whitney test was used to compare the inhibitory levels between different groups.
RESULTS
Generation of a P. falciparum line that expresses P. yoelii MSP119.
P. falciparum D10 parasites were electroporated with plasmids pPyMEGF-1 and pPyMEGF-2, which were designed to replace the MSP119 region with that from P. yoelii. To determine whether the PyMEGF sequences were integrated correctly into the P. falciparum genome, genomic DNA was extracted after the second round of drug cycling and PCR was performed using four pairs of primers. As shown in Fig. 1A, p1772 and p1773 were the forward and reverse primers for the target PfMSP1 sequence, whereas p1774 and p1775 were the forward and reverse primers for the PyMSP119 region, respectively. Primer p1836 is located upstream of the target PfMSP1sequence, and p1837 is located downstream of the PfMSP1 in the genome. PCR analysis revealed that only D10-PyMEGF-2 had the correct insert (1,200 bp) and the expected Hsp86 3′ untranslated region (UTR) (Fig. 1B). This result was confirmed by nucleotide sequencing, and consequently D10-PyMEGF-2 was chosen for cloning by limiting dilution. Six clones were generated, all of which were shown to contain the expected insert by both PCR and nucleotide sequencing (data not shown). One clone, Py2G9, was chosen for use in the subsequent invasion inhibition assays.
To determine whether the integrated PyMSP119 was expressed correctly, parasite lysates from D10-PyMEGF, as well as the matched transgenic line D10-PfM3′ and the parental line D10, were analyzed by immunoblotting using specific antibodies. As shown in Fig. 2, PyMSP119 expression was detected in D10-PyMEGF, whereas PfMSP119 protein was detected in D10-PfM3′ and D10. The various bands seen on the blot are consistent with the sizes expected for detection of the full-length MSP1 and the various processing products, which include the C terminus of the protein. These data demonstrated that PfMSP19 had been successfully replaced with PyMSP119 in the transgenic line D10-PyMEGF, and no cross-reactivity was detected between PfMSP119 and PyMSP119. This was further confirmed by IFA, which showed PyMSP119 was expressed at the correct cellular location in D10-PyMEGF (Fig. 3).
FIG. 2.
Immunoblot analysis of parasite extracts from D10 (lanes 1), D10-PfM3′ (lanes 2), and D10-PyMEGF (lanes 3) probed with monoclonal antibody 1E1 to PfMSP119 (A) and rabbit polyclonal antibodies to PyMSP119 (B). Arrows indicate MSP119 fragments.
FIG. 3.
Indirect immunofluorescence assay on D10-PfM3′ (A to D) and D10-PyMEGF (E to H) labeled with DAPI (A and E), anti-PfMSP119 antibodies (B and F), and anti-PyMSP119 antibodies (C and G). (D) Merged image of panels A and B; (H) merged image of panels E and G.
To examine whether replacement of PfMSP119 with PyMSP119 resulted in any functional changes, parasites from D10-PyMEGF, D10-PfM3′, and D10 were cultured for a period of 120 h and their growth rates were compared. As shown in Fig. 4, no significant difference in growth rate was observed between any of the parasite lines, all of which replicated 3- to 5-fold per cycle.
FIG. 4.
Comparison of the growth rates of D10-PyMEGF (triangles), D10-PfM3′ (circles), and D10 (diamonds). The medium containing pyrimethamine was changed every day, and the culture was diluted 1:5 with fresh medium and additional red blood cells at a 2% hematocrit every 32 h (indicated by arrows). Parasitemias were counted every 8 h from the duplicated wells of each parasite line. The error bars indicate standard deviations of the means.
Validation of the invasion inhibition assay.
To validate the transgenic lines, we set out to show that antibodies generated against PyMSP119 were capable of inhibiting parasite growth of D10-PyMEGF specifically and that inhibitory antibodies directed against irrelevant proteins did not cause differential inhibition on the parental and transgenic lines. We were also interested in determining whether selective inhibition would be observable with low volumes of added sera, a situation that occurs often when using the limited quantities of serum available from mice. Accordingly, invasion inhibition assays were performed using rabbit antibodies raised against recombinant PyMSP119, either GST-PyMSP119 or yPyMSP119, with final concentrations of 2.5 to 50%. As shown in Fig. 5A, both sera gave similar levels of PyMSP119-specific inhibition, which increased in degree as the serum concentration increased. Antibodies specific for P. falciparum AMA1 inhibited the growth of both lines to a similar level (Fig. 5B), demonstrating that gene replacement of PfMSP119 with PyMSP119 had no effect on the inhibitory capacity of antibodies directed against a distinct vaccine candidate. Rabbit antibodies raised to PfMSP119, when tested at a 10% concentration, gave invasion rates of 53% for D10-PfM3′ and 93% for D10-PyMEGF, resulting in a PfMSP119-specific inhibition of 40% (data not shown).
FIG. 5.
(A) PyMSP119-specific inhibitory activity of rabbit antisera raised to GST-PyMSP119 (empty circles) or yPyMSP119 (filled squares). Each serum was tested in triplicate at a final concentration of 2.5 to 50% on two transgenic lines, D10-PfM3′ and D10-PyMEGF, which express either the endogenous MSP119 or the homologous region from P. yoelii. PyMSP119-specific inhibition was calculated by subtracting the invasion rate of D10-PyMEGF from that of D10-PfM3′. The error bars indicate the standard deviations of the means. (B) Invasion inhibitory activities of PfAMA1-specific IgG on D10-PyMEGF (empty bars) and D10-PfM3′ (filled bars). Purified IgG was tested at a final concentration of 0.2 and 0.1 mg/ml (P > 0.05 at both concentrations).
Lack of correlation between in vitro inhibition and in vivo protection.
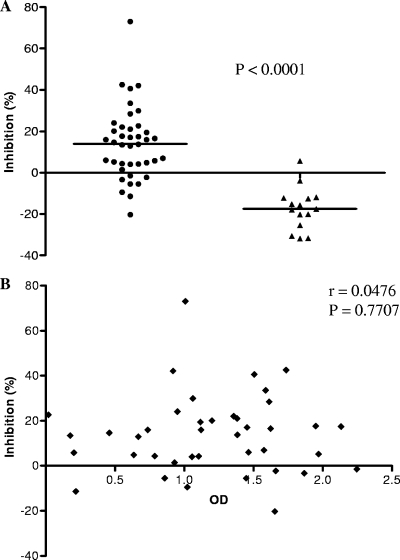
In order to investigate the correlation between in vitro inhibition and in vivo protection, we immunized mice with recombinant PyMSP119 and then challenged them with P. yoelii parasites. The sera taken before challenge were tested for growth-inhibitory activity specific for PyMSP119 and for the level of total antibodies directed to PyMSP119. At a final concentration of 20%, the mouse sera showed significant nonspecific inhibition to both transgenic lines (data not shown). At a 10% concentration, differential rates of invasion by the two parasite lines could be distinguished, and we therefore used this concentration in the inhibition assay. PyMSP119-specific inhibitory activity was expressed as net inhibition after subtracting the invasion rate of D10-PyMEGF from that of D10-PfM3′. Inhibitory activity was considered positive when the net inhibition was greater than 10%. As shown in Fig. 6A, 23 out of the 40 sera taken from PyMSP119-immunized mice (from two independent experiments) showed positive inhibitory activity, ranging from 10% to 73%. The average inhibition of the 23 positive sera was 25.0%, whereas the average inhibition of all 40 sera was 13.9%. In contrast, none of the 15 sera from control mice had positive inhibitory activity, with an average inhibition of −17.4% and range between −31.8% and 5.6%. No correlation was observed between the PyMSP119-specific inhibitory activity and the antibody levels measured by ELISA (Fig. 6B). After parasite challenge, the course of parasitemia was determined, and the level of peak parasitemia was used as an indicator of resistance to infection. As shown in Fig. 7A, a significant negative correlation was observed between the peak parasitemia and the total anti-MSP119 antibodies (Fig. 7A), indicating the substantial in vivo role of these antibodies in controlling the blood-stage infection. However, the level of MSP119-specific inhibitory activity did not correlate with peak parasitemia. Several mice that were completely protected from infection (with zero parasitemia) had no detectable inhibitory activity in their prechallenge sera (Fig. 7B). These data indicated that inhibitory activity measured in vitro was not a reliable predictor of immune status in vivo.
FIG. 6.
(A) PyMSP119-specific inhibitory activity in sera from mice immunized with recombinant PyMSP119 (circles) or PBS control (triangles). Each serum was tested in triplicate at a final concentration of 10% on two transgenic lines, D10-PfM3′ and D10-PyMEGF, which express either the endogenous MSP119 or the homologous region from P. yoelii. PyMSP119-specific inhibition was calculated by subtracting the invasion rate of D10-PyMEGF from that of D10-PfM3′. The horizontal lines indicate the means of the values. (B) Lack of correlation between invasion-inhibitory activity (as a percentage) and antibody level, measured by ELISA (OD at 1:10,000 dilution).
FIG. 7.
Correlation between peak parasitemia and total antibody level (A) directed to PyMSP119, or PyMSP119-specific invasion-inhibitory activity (B). Each serum was tested at a 1:10,000 dilution by ELISA for the total antibody level and at a 10% dilution for the inhibition assay. PyMSP119-specific inhibition was calculated by subtracting the invasion rate of D10-PyMEGF from that of D10-PfM3′.
DISCUSSION
We have generated a transgenic P. falciparum line that expresses the MSP119 region from P. yoelii in place of the endogenous PfMSP119. The successful replacement of PfMSP119 with PyMSP119 is consistent with previous observations that this domain of MSP1 has a conserved function among distantly related malaria species and demonstrates that a wide range of mutations in the primary sequence of this domain can be tolerated by the parasite (10, 30). To date, trials for MSP119-based vaccines using the P. yoelii model have been performed in various laboratories around the world with antigens produced in different host-vector systems, formulated in different adjuvants, and administered in a variety of immunization regimens (4, 8, 17, 23, 38, 41). The efficiency of these regimens in inducing protective immunity has been evaluated mostly by challenge infection studies, the outcomes of which cannot be predicted by antibody levels measured by ELISA. The assay developed in this study could be used to measure the MSP119-specific inhibitory activity of these antibodies and examine whether it can serve as a more accurate correlate of protection. Further, it can allow cross-comparisons between different immunization regimens in terms of the amount of growth-inhibitory antibody produced.
In our study model, we did not find a significant correlation between the level of MSP119-specific inhibitory antibodies and control of parasitemia upon subsequent blood-stage challenge. This contrasts with conclusions from a study using transgenic Plasmodium berghei that expressed P. falciparum MSP119 (10). Differences may relate to the immunization regimen, as MSP119-specific inhibitory antibodies in the other study were generated by repeatedly injecting mice with the transgenic parasites, and the overall protective effect measured may in part have been due to responses to other parasite-derived antigens. Antibodies directed against MSP119 are believed to be a major component of protective immunity; however, the mechanisms by which such antibodies mediate their protective effect remain under debate. We showed a significant correlation between the total anti-MSP119 antibodies and the in vivo control of parasitemia and not to growth-inhibitory activity acting on its own. The in vitro inhibitory assay measures the functional activity of antibodies independent of complement or other cellular mediators, and our results suggest they are important in this model system. Evidence has been accumulating to suggest that antibody action via the Fc interaction with monocytes/macrophages plays an important role in protective immunity (2, 26, 31, 40). Such a mechanism is compatible with the results we have obtained in this experiment, and the anti-MSP119 antibodies we induced may act in vivo by cooperating with monocytes and/or macrophages.
In addition, from a practical point of view, although a similar P. falciparum line that expresses P. chabaudi MSP119 has been available, the generation of the P. yoelii transgenic line provides a useful reagent for assessment of subunit vaccines against the asexual blood-stage infection. P. chabaudi is believed to display similar clinical symptoms to P. falciparum, including sequestration, and therefore is a good model for immune mechanism and pathogenesis studies, whereas P. yoelii YM is preferable for vaccination studies because, as in humans, immunity to infection is dependent on antibody responses (7, 17) and P. yoelii provides clear results on susceptibility and resistance (22). This transgenic line can serve as a valuable tool to dissect the various aspects of MSP119-induced immune responses and to evaluate the efficacy of MSP1-based vaccines. Using this newly generated transgenic line, together with a matched line that expresses endogenous PfMSP119, we have shown that polyclonal antibodies raised to recombinant PyMSP119 have significant antigen-specific inhibitory activity that is concentration dependent. The finding that a final serum dilution of 5% still provided significant inhibition suggested that as little as 5 μl of serum per well would be sufficient, making the assay feasible for testing mouse sera, which are often available in limited quantities.
Our study has a number of important implications for the understanding and measurement of immunity against malaria and the development of blood-stage vaccines. First, although MSP119-specific inhibitory antibodies are reported to be a major component of the total inhibitory response in human immune sera (29), they may not be necessary for protection and the reliance on inhibition assay to select antigens for progression to human clinical trial may be misplaced (5). Second, it is possible that not only may inhibitory antibodies not be necessary; they may not even be sufficient for protection. Our experimental design evidenced the fact that inhibitory antibodies present in some protected mice may not necessarily be associated with protection, suggesting caution may be needed when interpreting some associations in human field data.
Acknowledgments
We thank the Australian Red Cross Blood Service for the provision of human blood and serum. We also thank Brendan Crabb for kindly providing the D10-PfM3′ line and Tony Holder for providing the monoclonal antibody mAb1E1.
This work was supported by the National Health and Medical Research Council of Australia and National Institutes of Health grant DK32094. E.E.H.M. is a recipient of an AusAID scholarship.
Editor: J. H. Adams
Footnotes
Published ahead of print on 16 November 2009.
REFERENCES
- 1.al-Yaman, F., B. Genton, K. J. Kramer, S. P. Chang, G. S. Hui, M. Baisor, and M. P. Alpers. 1996. Assessment of the role of naturally acquired antibody levels to Plasmodium falciparum merozoite surface protein-1 in protecting Papua New Guinean children from malaria morbidity. Am. J. Trop. Med. Hyg. 54:443-448. [DOI] [PubMed] [Google Scholar]
- 2.Badell, E., C. Oeuvray, A. Moreno, S. Soe, N. van Rooijen, A. Bouzidi, and P. Druilhe. 2000. Human malaria in immunocompromised mice: an in vivo model to study defense mechanisms against Plasmodium falciparum. J. Exp. Med. 192:1653-1660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blackman, M. J., T. J. Scott-Finnigan, S. Shai, and A. A. Holder. 1994. Antibodies inhibit the protease-mediated processing of a malaria merozoite surface protein. J. Exp. Med. 180:389-393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Calvo, P. A., T. M. Daly, and C. A. Long. 1996. Both epidermal growth factor-like domains of the merozoite surface protein-1 from Plasmodium yoelii are required for protection from malaria. Ann. N. Y. Acad. Sci. 797:260-262. [DOI] [PubMed] [Google Scholar]
- 5.Coppel, R. L. 2009. Vaccinating with the genome: a Sisyphean task? Trends Parasitol. 25:205-212. [DOI] [PubMed] [Google Scholar]
- 6.Corran, P. H., R. A. O'Donnell, J. Todd, C. Uthaipibull, A. A. Holder, B. S. Crabb, and E. M. Riley. 2004. The fine specificity, but not the invasion inhibitory activity, of 19-kilodalton merozoite surface protein 1-specific antibodies is associated with resistance to malarial parasitemia in a cross-sectional survey in The Gambia. Infect. Immun. 72:6185-6189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Daly, T. M., and C. A. Long. 1995. Humoral response to a carboxyl-terminal region of the merozoite surface protein-1 plays a predominant role in controlling blood-stage infection in rodent malaria. J. Immunol. 155:236-243. [PubMed] [Google Scholar]
- 8.Daly, T. M., and C. A. Long. 1996. Influence of adjuvants on protection induced by a recombinant fusion protein against malarial infection. Infect. Immun. 64:2602-2608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Daly, T. M., and C. A. Long. 1993. A recombinant 15-kilodalton carboxyl-terminal fragment of Plasmodium yoelii yoelii 17XL merozoite surface protein 1 induces a protective immune response in mice. Infect. Immun. 61:2462-2467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.de Koning-Ward, T. F., R. A. O'Donnell, D. R. Drew, R. Thomson, T. P. Speed, and B. S. Crabb. 2003. A new rodent model to assess blood stage immunity to the Plasmodium falciparum antigen merozoite surface protein 119 reveals a protective role for invasion inhibitory antibodies. J. Exp. Med. 198:869-875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dodoo, D., T. G. Theander, J. A. Kurtzhals, K. Koram, E. Riley, B. D. Akanmori, F. K. Nkrumah, and L. Hviid. 1999. Levels of antibody to conserved parts of Plasmodium falciparum merozoite surface protein 1 in Ghanaian children are not associated with protection from clinical malaria. Infect. Immun. 67:2131-2137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Egan, A. F., P. Burghaus, P. Druilhe, A. A. Holder, and E. M. Riley. 1999. Human antibodies to the 19kDa C-terminal fragment of Plasmodium falciparum merozoite surface protein 1 inhibit parasite growth in vitro. Parasite Immunol. 21:133-139. [DOI] [PubMed] [Google Scholar]
- 13.Egan, A. F., J. Morris, G. Barnish, S. Allen, B. M. Greenwood, D. C. Kaslow, A. A. Holder, and E. M. Riley. 1996. Clinical immunity to Plasmodium falciparum malaria is associated with serum antibodies to the 19-kDa C-terminal fragment of the merozoite surface antigen, PfMSP-1. J. Infect. Dis. 173:765-769. [DOI] [PubMed] [Google Scholar]
- 14.Fidock, D. A., and T. E. Wellems. 1997. Transformation with human dihydrofolate reductase renders malaria parasites insensitive to WR99210 but does not affect the intrinsic activity of proguanil. Proc. Natl. Acad. Sci. U. S. A. 94:10931-10936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gozalo, A., C. Lucas, M. Cachay, B. T. Wellde, T. Hall, B. Bell, J. Wood, D. Watts, M. Wooster, J. A. Lyon, J. K. Moch, J. D. Haynes, J. S. Williams, C. Holland, E. Watson, K. E. Kester, D. C. Kaslow, and W. R. Ballou. 1998. Passive transfer of growth-inhibitory antibodies raised against yeast-expressed recombinant Plasmodium falciparum merozoite surface protein-1(19). Am. J. Trop. Med. Hyg. 59:991-997. [DOI] [PubMed] [Google Scholar]
- 16.Guevara Patino, J. A., A. A. Holder, J. S. McBride, and M. J. Blackman. 1997. Antibodies that inhibit malaria merozoite surface protein-1 processing and erythrocyte invasion are blocked by naturally acquired human antibodies. J. Exp. Med. 186:1689-1699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hirunpetcharat, C., J. H. Tian, D. C. Kaslow, N. van Rooijen, S. Kumar, J. A. Berzofsky, L. H. Miller, and M. F. Good. 1997. Complete protective immunity induced in mice by immunization with the 19-kilodalton carboxyl-terminal fragment of the merozoite surface protein-1 (MSP1[19]) of Plasmodium yoelii expressed in Saccharomyces cerevisiae: correlation of protection with antigen-specific antibody titer, but not with effector CD4+ T cells. J. Immunol. 159:3400-3411. [PubMed] [Google Scholar]
- 18.Hui, G. S., C. Nikaido, C. Hashiro, D. C. Kaslow, and W. E. Collins. 1996. Dominance of conserved B-cell epitopes of the Plasmodium falciparum merozoite surface protein, MSP1, in blood-stage infections of naive Aotus monkeys. Infect. Immun. 64:1502-1509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.John, C. C., R. A. O'Donnell, P. O. Sumba, A. M. Moormann, T. F. de Koning-Ward, C. L. King, J. W. Kazura, and B. S. Crabb. 2004. Evidence that invasion-inhibitory antibodies specific for the 19-kDa fragment of merozoite surface protein-1 (MSP-119) can play a protective role against blood-stage Plasmodium falciparum infection in individuals in a malaria endemic area of Africa. J. Immunol. 173:666-672. [DOI] [PubMed] [Google Scholar]
- 20.Kedzierski, L., C. G. Black, M. W. Goschnick, A. W. Stowers, and R. L. Coppel. 2002. Immunization with a combination of merozoite surface proteins 4/5 and 1 enhances protection against lethal challenge with Plasmodium yoelii. Infect. Immun. 70:6606-6613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kumar, S., A. Yadava, D. B. Keister, J. H. Tian, M. Ohl, K. A. Perdue-Greenfield, L. H. Miller, and D. C. Kaslow. 1995. Immunogenicity and in vivo efficacy of recombinant Plasmodium falciparum merozoite surface protein-1 in Aotus monkeys. Mol. Med. 1:325-332. [PMC free article] [PubMed] [Google Scholar]
- 22.Langhorne, J., S. J. Quin, and L. A. Sanni. 2002. Mouse models of blood-stage malaria infections: immune responses and cytokines involved in protection and pathology. Chem. Immunol. 80:204-228. [DOI] [PubMed] [Google Scholar]
- 23.Ling, I. T., S. A. Ogun, P. Momin, R. L. Richards, N. Garcon, J. Cohen, W. R. Ballou, and A. A. Holder. 1997. Immunization against the murine malaria parasite Plasmodium yoelii using a recombinant protein with adjuvants developed for clinical use. Vaccine 15:1562-1567. [DOI] [PubMed] [Google Scholar]
- 24.Long, C. A., T. M. Daly, P. Kima, and I. Srivastava. 1994. Immunity to erythrocytic stages of malarial parasites. Am. J. Trop. Med. Hyg. 50:27-32. [DOI] [PubMed] [Google Scholar]
- 25.Majarian, W. R., T. M. Daly, W. P. Weidanz, and C. A. Long. 1984. Passive immunization against murine malaria with an IgG3 monoclonal antibody. J. Immunol. 132:3131-3137. [PubMed] [Google Scholar]
- 26.McIntosh, R. S., J. Shi, R. M. Jennings, J. C. Chappel, T. F. de Koning-Ward, T. Smith, J. Green, M. van Egmond, J. H. Leusen, M. Lazarou, J. van de Winkel, T. S. Jones, B. S. Crabb, A. A. Holder, and R. J. Pleass. 2007. The importance of human FcγRI in mediating protection to malaria. PLoS Pathog. 3:e72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Miura, K., H. Zhou, S. E. Moretz, A. Diouf, M. A. Thera, A. Dolo, O. Doumbo, E. Malkin, D. Diemert, L. H. Miller, G. E. Mullen, and C. A. Long. 2008. Comparison of biological activity of human anti-apical membrane antigen-1 antibodies induced by natural infection and vaccination. J. Immunol. 181:8776-8783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nwuba, R. I., O. Sodeinde, C. I. Anumudu, Y. O. Omosun, A. B. Odaibo, A. A. Holder, and M. Nwagwu. 2002. The human immune response to Plasmodium falciparum includes both antibodies that inhibit merozoite surface protein 1 secondary processing and blocking antibodies. Infect. Immun. 70:5328-5331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.O'Donnell, R. A., T. F. de Koning-Ward, R. A. Burt, M. Bockarie, J. C. Reeder, A. F. Cowman, and B. S. Crabb. 2001. Antibodies against merozoite surface protein (MSP)-1(19) are a major component of the invasion-inhibitory response in individuals immune to malaria. J. Exp. Med. 193:1403-1412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.O'Donnell, R. A., A. Saul, A. F. Cowman, and B. S. Crabb. 2000. Functional conservation of the malaria vaccine antigen MSP-119 across distantly related Plasmodium species. Nat. Med. 6:91-95. [DOI] [PubMed] [Google Scholar]
- 31.Pleass, R. J., S. A. Ogun, D. H. McGuinness, J. G. van de Winkel, A. A. Holder, and J. M. Woof. 2003. Novel antimalarial antibodies highlight the importance of the antibody Fc region in mediating protection. Blood 102:4424-4430. [DOI] [PubMed] [Google Scholar]
- 32.Reed, Z. H., M. P. Kieny, H. Engers, M. Friede, S. Chang, S. Longacre, P. Malhotra, W. Pan, and C. Long. 2009. Comparison of immunogenicity of five MSP1-based malaria vaccine candidate antigens in rabbits. Vaccine 27:1651-1660. [DOI] [PubMed] [Google Scholar]
- 33.Riley, E. M., S. J. Allen, J. G. Wheeler, M. J. Blackman, S. Bennett, B. Takacs, H. J. Schonfeld, A. A. Holder, and B. M. Greenwood. 1992. Naturally acquired cellular and humoral immune responses to the major merozoite surface antigen (PfMSP1) of Plasmodium falciparum are associated with reduced malaria morbidity. Parasite Immunol. 14:321-337. [DOI] [PubMed] [Google Scholar]
- 34.Riley, E. M., G. E. Wagner, M. F. Ofori, J. G. Wheeler, B. D. Akanmori, K. Tetteh, D. McGuinness, S. Bennett, F. K. Nkrumah, R. F. Anders, and K. A. Koram. 2000. Lack of association between maternal antibody and protection of African infants from malaria infection. Infect. Immun. 68:5856-5863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sabchareon, A., T. Burnouf, D. Ouattara, P. Attanath, H. Bouharoun-Tayoun, P. Chantavanich, C. Foucault, T. Chongsuphajaisiddhi, and P. Druilhe. 1991. Parasitologic and clinical human response to immunoglobulin administration in falciparum malaria. Am. J. Trop. Med. Hyg. 45:297-308. [DOI] [PubMed] [Google Scholar]
- 36.Spring, M., J. Cummings, C. Ockenhouse, S. Dutta, R. Reidler, E. Angov, E. Bergmann-Leitner, V. Stewart, S. Bittner, L. Juompan, M. Kortepeter, R. Nielsen, U. Krzych, E. Tierney, L. Ware, M. Dowler, C. Hermsen, R. Sauerwein, S. de Vlas, O. Ofori-Anyinam, D. Lanar, J. Williams, K. Kester, K. Tucker, M. Shi, E. Malkin, C. Long, C. Diggs, L. Soisson, M. Dubois, W. Ballou, J. Cohen, and J. Heppner. 2009. Phase 1/2a study of the malaria vaccine candidate apical membrane antigen-1 (AMA-1) administered in adjuvant system AS01B or AS02A. PLoS One 4:e5254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vukovic, P., P. M. Hogarth, N. Barnes, D. C. Kaslow, and M. F. Good. 2000. Immunoglobulin G3 antibodies specific for the 19-kilodalton carboxyl-terminal fragment of Plasmodium yoelii merozoite surface protein 1 transfer protection to mice deficient in Fc-γRI receptors. Infect. Immun. 68:3019-3022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wang, L., M. W. Goschnick, and R. L. Coppel. 2004. Oral immunization with a combination of Plasmodium yoelii merozoite surface proteins 1 and 4/5 enhances protection against lethal malaria challenge. Infect. Immun. 72:6172-6175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang, L., L. Kedzierski, S. L. Wesselingh, and R. L. Coppel. 2003. Oral immunization with a recombinant malaria protein induces conformational antibodies and protects mice against lethal malaria. Infect. Immun. 71:2356-2364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yoneto, T., S. Waki, T. Takai, Y. Tagawa, Y. Iwakura, J. Mizuguchi, H. Nariuchi, and T. Yoshimoto. 2001. A critical role of Fc receptor-mediated antibody-dependent phagocytosis in the host resistance to blood-stage Plasmodium berghei XAT infection. J. Immunol. 166:6236-6241. [DOI] [PubMed] [Google Scholar]
- 41.Zhang, Z. H., P. H. Jiang, N. J. Li, M. Shi, and W. Huang. 2005. Oral vaccination of mice against rodent malaria with recombinant Lactococcus lactis expressing MSP-119. World J. Gastroenterol. 11:6975-6980. [DOI] [PMC free article] [PubMed] [Google Scholar]