Abstract
Congenital toxoplasmosis in newborns is generally subclinical, but infected infants are at risk of developing ocular lesions. Diagnosis at birth relies mainly on serological tests. Cell-mediated immunity plays the major role in resistance to infection but is not routinely investigated for diagnostic purposes. Here, we describe a simple test based on the gamma interferon (IFN-γ) response after stimulation of whole blood by crude parasitic antigens. One milliliter of heparinized blood was centrifuged; plasma was kept for routine serological tests, and pellets were resuspended in culture medium. After 24 h of culture in the presence of crude Toxoplasma gondii antigen, the cells were centrifuged and the supernatant was assayed for IFN-γ. For 62 infants under 1 year of age born to mothers who were infected during pregnancy, the sensitivity and specificity of the test were 94% (with positive results for 16 of 17 infected infants) and 98% (with negative results for 44 of 45 uninfected infants), respectively. The false-negative result was for a treated baby who gave positive results after the withdrawal of treatment. The false positive was obtained for a 3-month-old baby. For a cohort of 124 congenitally infected patients between 1 and 30 years of age, the sensitivity of the assay was 100%. We present a simple test based on IFN-γ secretion to assess cell-mediated immunity in toxoplasmosis. As only 1 ml of blood is required to investigate humoral and cellular immunity, our assay is well adapted for the study of congenital toxoplasmosis in infants. Using purified antigens or recombinant peptides may improve the test performance.
Toxoplasma gondii, a ubiquitous intracellular protozoan parasite, is an important cause of morbidity and mortality in congenitally infected individuals. Maternal infection may have serious consequences for the fetus (10). In other cases, infected newborns appear to be totally asymptomatic at birth but are at risk of developing retinal diseases during childhood or adolescence (26). For these patients, the diagnosis of the disease relies mainly on the detection of specific antibodies. Toxoplasma-specific immunoglobulin M (IgM) and IgA, which do not cross the placenta, are considered to be good markers of congenital infection. However, gestational age at maternal infection affects test performance (25), and at birth, the tests cannot detect more than 75% of infected babies (20). Because Toxoplasma-specific IgG crosses the placenta, its presence in the blood of newborns cannot be considered a marker of congenital infection. Maternally transferred IgG usually disappears within 6 to 12 months (20). Therefore, uninfected infants born to mothers who seroconverted during pregnancy have to undergo regular sampling for serological testing for 1 year before congenital toxoplasmosis can be ruled out (16). Clinicians are seeking valid indicators of congenital infection to improve clinical decision making. T. gondii infection results in long-lasting cell-mediated immunity which is highly dependent upon the effector activity of T lymphocytes that produce gamma interferon (IFN-γ) (6). Surprisingly, few studies have investigated the potential role of cell immunity in diagnosis of the disease. Data in the literature are contradictory. An absence of stimulation of lymphocytes by T. gondii antigen in congenitally infected children has been reported previously (18, 27). Recently, Guglietta et al. (13), using synthetic peptides, detected age-related impairment of the specific T-cell response to parasitic antigen in congenital infections. Conversely, a recent publication reported that evaluation of T-cell immunity is important for an early and accurate diagnosis of congenital toxoplasmosis (3). By detecting CD25 expression by flow cytometry, we demonstrated previously that specific cell immunity is detectable in almost all infected patients, including newborns (11). In this study, we evaluate the performance of a whole-blood IFN-γ release assay for the diagnosis of congenital toxoplasmosis. In this clinical setting, the quantity of blood required is limited, and we therefore looked at the possibility of separating plasma from blood cells in order to conduct serological tests (the “gold standard”) and the IFN-γ assay with the same sample.
MATERIALS AND METHODS
Patients. (i) Group 1.
Patient group 1 was used in a pilot study to check the validity of the technique before the testing of infants. It included 172 patients consulting in the outpatient department at Hôpital de la Croix Rousse, Lyon, France, and pregnant women tested for toxoplasmosis serology as part of the French national program of prevention. Fifty-eight subjects were free of infection (with negative serological tests), and 114 either had chronic infection or had recently seroconverted (with positive tests).
The viability of assaying specific IFN-γ secretion with blood cell pellets resuspended in medium was first investigated using T. gondii antigens at final concentrations of 1.5, 3, and 6 μg/ml. Among these concentrations, 3 μg/ml yielded the best results with respect to sensitivity and specificity (data not shown). Therefore, this concentration was used for the study. Samples processed 24 h after withdrawal were likely to exhibit a decreased IFN-γ response compared to samples processed within 24 h after withdrawal. Results were validated when phytohemagglutinin (PHA)-stimulated wells yielded a positive value and when the optical density (OD; calculated as the mean plus 2 standard deviations after Box-Cox transformation) in wells containing phosphate-buffered saline (PBS) was below 0.75. Under these conditions, for 479 tests performed in the study, results from 25 (5%) were invalidated due to either a lack of positive response to PHA stimulation or spontaneous secretion of IFN-γ.
(ii) Group 2.
Group 2 consisted of 62 infants under 1 year of age who were born to mothers who seroconverted during pregnancy. For all these subjects, maternal seroconversion and ante- and postnatal treatment were fully documented. Congenital toxoplasmosis was diagnosed in 17 cases on the basis of positive PCR results for amniotic fluid, the presence of IgM or IgA in peripheral blood, a positive mother/newborn comparative Western blot, or the presence of specific IgG after 1 year of life. Infected patients were given a 1-year course of pyrimethamine-sulfonamide (Fansidar). According to our protocol, all patients underwent both a clinical and ophthalmological examination and serological testing every 3 months during the first year. Infection was ruled out for 45 children who had negative tests in utero and at birth and had negative serology results at 1 year of age.
(iii) Group 3.
Group 3 comprised 124 congenitally infected patients enrolled at ages 1 to 30 years. All underwent regular annual clinical and ophthalmological examinations. Thirty-one of them presented ocular lesions, and 8 had cerebral calcification at the time of inclusion in the study.
Serological investigations.
T. gondii-specific IgG and IgM antibodies were detected using the Enzygnost toxoplasmosis enzyme-linked immunosorbent assay (ELISA; Siemens Healthcare Diagnostics, Marburg, Germany). A dye test (P. Thulliez, Institut de Puériculture, Paris, France) was performed on samples with discordant results.
T-cell stimulation. (i) Preparation of soluble T. gondii antigen.
T. gondii parasites of the RH strain were harvested from the peritoneal cavities of OF1 mice (Charles River, L'Arbresle, France). Ascites fluid was collected 2 days after infection; parasites were washed in PBS and disrupted by four freeze-thaw cycles and underwent three sonications for 20 s each. The suspension was filtered through 0.2-μm-pore-size membranes and stored at −20°C until use.
(ii) Blood samples and stimulation.
Samples of 1 ml of peripheral blood were drawn into Vacutainer tubes (BD Diagnostics, Franklin Lakes, NJ) that contained lithium heparin anticoagulant. Tubes were centrifuged at 1,600 × g for 15 min at room temperature. Plasma was collected for serological investigations and replaced by the same volume of RPMI medium (Sigma-Aldrich, St. Louis, MO). Aliquots of 300 μl of diluted blood were cultured in sterile propylene tubes (Eppendorf AG, Hamburg, Germany) in the presence of different concentrations of T. gondii antigens. Positive and negative controls consisted of PHA at a final concentration of 20 μg/ml and PBS, respectively. All cultures were incubated for 24 h at 37°C in 5% CO2 in a humidified atmosphere. Culture supernatants were collected from each tube after centrifugation at 1,600 × g for 15 min at room temperature and stored at −40°C until the IFN-γ assay was carried out.
IFN-γ assay.
IFN-γ was assayed in duplicate using a commercial ELISA kit (AbCys, Paris, France). The mean OD of the PBS controls was subtracted from the mean OD of antigen-stimulated samples. The amount of IFN-γ released, expressed in picograms per milliliter, was obtained by converting the OD using the standard curve from the kit.
Ethical aspects.
The study was approved by the local ethical committee. Informed consent was obtained from patients or legal guardians.
Statistical analysis.
The IFN-γ responses in infected and uninfected patients were compared using the Mann-Whitney test for the different groups. A P value under 0.05 was considered statistically significant.
For the group of infants under 1 year, the empirical receiver operating characteristic (ROC) curve was built and the area under the curve (AUC) was estimated using the nonparametric method. The 95% confidence interval was calculated using a logistic transformation of the AUC. For the retained positivity threshold, the sensitivity and specificity were estimated with their exact 95% confidence intervals.
RESULTS
Group 1.
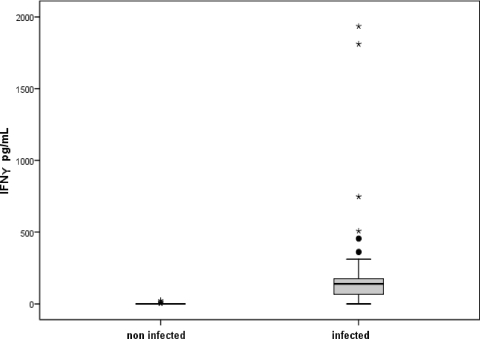
Fig. 1 shows that IFN-γ secretion in the 114 infected patients in group 1 was significantly higher than that in the 58 uninfected patients (P < 0.0001). The test scored a sensitivity of 96% and a specificity of 91%. Among patients who displayed negative serology, five scored weak-positive IFN-γ values ranging from 1.5 to 23.2 pg/ml. All five had nonspontaneous IFN-γ secretion (i.e., no detectable secretion of IFN-γ in negative controls) and did not present an inflammatory syndrome. Two of these subjects were pregnant women who presented an atypical profile of seroconversion with the presence of IgM without IgG despite repeated testing. Both were considered to be recently infected on the basis of the presence of IgM and were given spiramycin treatment. Among patients who tested positive for toxoplasmosis, five had a negative IFN-γ response despite a positive PHA test. No evidence of anergy or immunosuppression was found in the patients' records.
FIG. 1.
IFN-γ responses after stimulation of whole-blood samples from uninfected and infected adults by T. gondii crude antigen (P < 0.0001; Mann-Whitney test). The hinges at the top and bottom of the box represent the upper (75%) and lower (25%) quartiles. The thick black line inside the box represents the median. The horizontal lines above and below the box represent the adjacent values, i.e., the most extreme values in the sample that lie between the hinges and the “inner fences,” which lie at positions 1.5 times the H spread (i.e., the distance between the upper and lower hinges) above and below the hinges. Dots represent outliers (positioned between 1.5 and 3 times the H spread); asterisks represent extreme cases (positioned more than 3 times the H spread).
Group 2.
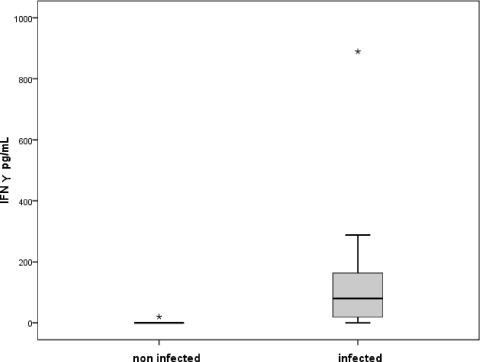
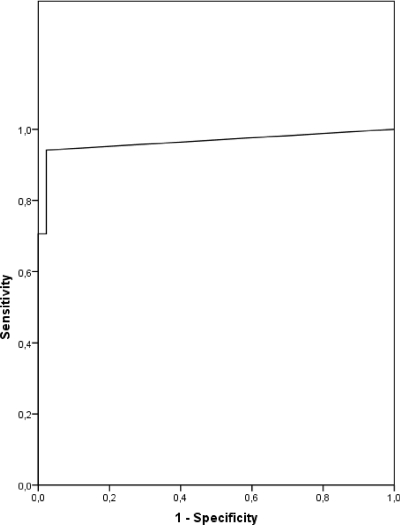
From the first test at inclusion in the study, 17 infected infants displayed a significantly higher level of IFN-γ than uninfected infants (P < 0.0001) (Fig. 2). According to the ROC curve, values above 1 pg/ml were considered to be positive (Fig. 3). Under these conditions, 16 of 17 infected babies produced positive IFN-γ tests. Among these, five infants were diagnosed with subclinical congenital infection between 3 weeks and 3 months of life, and in two cases, this was the only positive criterion for congenital infection. The mothers had seroconverted at different periods during pregnancy, and all were given antenatal treatment for toxoplasmosis. The false-negative test corresponded to an 8-month-old baby who was under treatment when included in the study and displayed positive test results after the withdrawal of treatment. Among 45 uninfected infants, 44 yielded a negative response. In this clinical setting, the sensitivity and specificity of the test were 94% (confidence interval, 69.2 to 99.7%) and 98% (confidence interval, 86.8 to 99.9%), respectively.
FIG. 2.
IFN-γ responses after stimulation of whole-blood samples from uninfected and congenitally infected infants under 1 year of age by T. gondii crude antigen (P < 0.0001; Mann-Whitney test).
FIG. 3.
ROC curve for determining the sensitivity and specificity of the IFN-γ test. Using a threshold of one yielded a sensitivity of 94% and a specificity of 98%.
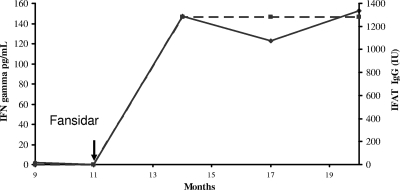
The follow-up findings (96 test results) for all 62 infants were consistent with the diagnoses except that two of the babies displayed transitory negation of the test result when under treatment. Interestingly, at the same time, they displayed negative serology. After withdrawal of treatment, they presented a dramatic increase in both IFN-γ and IgG titers (Fig. 4).
FIG. 4.
Evolution of IFN-γ levels (solid line) and specific antibody titers (dashed line), expressed in international units (IU), in a congenitally infected infant during and after the withdrawal of treatment. The arrow indicates the time of withdrawal of treatment. Months indicate the age of the infant at sample collection. IFAT, indirect fluorescent antibody technique.
Group 3.
All of the 172 congenitally infected subjects had a positive test result, with IFN-γ levels ranging from 9 to 2,285 pg/ml (median, 168.5 pg/ml); there were nonsignificant correlations between IFN-γ levels and lymphocyte counts (r = 0.06; P = 0.5) and between IFN-γ levels and IgG titers (r = 0.08; P = 0.6). No difference between subclinical infection and patent infection was observed (data not shown).
DISCUSSION
We investigated an in vitro assay to measure IFN-γ responses of T cells that had been stimulated by crude T. gondii antigens. The test requires only 1 ml of whole blood and is therefore well suited for application to newborns. Moreover, in addition to the IFN-γ assay with positive and negative controls (PHA and PBS samples, respectively), serological tests can be carried out with the same blood sample. The overall rate of invalidated test results was 5% due to either spontaneous secretion of IFN-γ in control tubes or a lack of positive response in PHA tubes, and the invalid results were observed mainly for adults. The assay was first validated for adults. Seropositive patients with either acute or chronic infection exhibited significantly higher levels of IFN-γ than uninfected patients (Fig. 1). Five samples without spontaneous secretion of IFN-γ were determined to be false positives when the results were compared with IgG serology. Two were from pregnant women who presented an atypical profile but were nevertheless considered to have had recent seroconversions and were treated. Evaluation of IFN-γ may help to interpret an ambiguous serological status which may be encountered in pregnant women. A superantigen effect of T. gondii antigen in uninfected mice, but not in humans, has been reported previously (7). The low number of false positives in our study does not favor this phenomenon. It has been demonstrated previously that T. gondii antigen can elicit marked T-cell proliferation in seronegative subjects. This proliferation appeared to be polyclonal and may result from cross-reactivity with another pathogen such as a coccidian (21). Purification of the antigen may improve the specificity of the test.
The five patients with false-negative results were not immunosuppressed, and all responded positively to PHA. Their lymphocyte counts fell within normal values, but no CD4 phenotyping was performed. All of them presented a chronic toxoplasmic infection, and their lack of response was not due to immunosuppression associated with active disease, as reported previously for tuberculosis patients (9). Other factors such as CD4+ CD25+ FoxP3+ regulatory cells suppress specific immunity in patients with active tuberculosis (2). Interestingly, T. gondii infection has been reported to reduce FoxP3 mRNA expression in pregnant mice (12). Whether this phenomenon is relevant in humans has not yet been demonstrated.
For infants under 1 year of age born to mothers who were infected during pregnancy, the results of the first test (Fig. 2) yielded a sensitivity and specificity of 94 and 98%, respectively. The test ruled out the disease in 44 of 45 uninfected infants and would have made IgG monitoring during the first year of life unnecessary. The only false positive was observed for a 6-month-old baby who presented a transitory positive test result, without clinical inflammatory syndrome; further testing was negative. Sixteen of 17 infected infants were identified by the test. In two patients under 3 months of age, IFN-γ secretion was the only sign of infection and would have prompted a decision to treat. These data demonstrated that, for infants, the IFN-γ release assay is a good marker of congenital toxoplasmosis, and it has also been reported previously to be effective for diagnosing perinatal tuberculosis (4); neither the stage of pregnancy at maternal contamination nor antenatal treatment hampered the test. The only false-negative result was obtained for an 8-month-old, treated baby who displayed an important rise in IFN-γ after withdrawal of treatment. The diagnosis of congenital toxoplasmosis was made on the basis of serological tests before inclusion in the study. During the follow-up with these patients, a total of 96 tests were performed. All but two results matched the clinical statuses of the infants. The two false negatives were obtained for treated patients who also presented a rise in IFN-γ titers after withdrawal of treatment. As presented in Fig. 4, IgG titers paralleled IFN-γ levels. This antibody profile (i.e., transitory negation followed by rebound) is commonly observed for treated patients (14, 24). The impact of treatment in reducing the IFN-γ-specific response in tuberculosis has been described previously (1, 9, 15) and suggests that such tests could be used for monitoring patient response to treatment (1). This pattern may be due to a reduction in antigen load originating from parasitic cysts or to a direct effect of pyrimethamine and sulfonamide on activated lymphocytes through activation of the mitochondrial apoptotic pathway (22). A large discrepancy in drug levels observed in babies (5) may explain why this phenomenon is not observed in all infants. The sustained IFN-γ response observed in subclinical patients in group 3 30 years after infection is a marker of continuous parasitic antigen production by cysts that maintain specific effector T cells in the bloodstream. The acute phase of the disease is characterized by the presence of fast-replicating tachyzoites which differentiate into slow-replicating bradyzoites under the pressure of the immune system, especially the Th1 response (17). Bradyzoites form cysts in different tissues and persist throughout life. Both parasitic stages express specific antigens (23). During the chronic phase of the disease, bradyzoite antigens are able to maintain an efficient immune response (8). Interestingly, our data also demonstrated that T cells from cyst-bearing patients could respond to crude extracts of tachyzoites of a noncystogenic strain (the RH strain), which suggests the lifelong presence of circulating antigens common to the two parasitic stages in humans.
In conclusion, we demonstrated that evaluation of the IFN-γ response after stimulation of whole blood by crude toxoplasmic antigen is a simple, easily performed test that is suitable for diagnosing congenital toxoplasmosis in newborns. This test could reliably rule out congenital infection at birth and avoid unnecessary anxiety and serological follow-up. Conversely, when giving positive results, it could prompt an early decision to treat, which is believed to reduce infection sequelae, although the exact benefits are still being debated (19). The use of purified antigens or synthetic peptides to improve the performance of the test should be investigated. Additional cases are needed in order to evaluate more precisely the sensitivity of the test. It may also be a useful tool for screening potential vaccine antigens in humans (8).
Acknowledgments
We thank V. Meroni (Department of Infectious Diseases, Pavia, Italy) and G. Cozon (Hôpital Lyon Sud, Lyon, France) for their comments and P. Thulliez (Institut de Puériculture, Paris, France) for his help.
None of the authors has a financial relationship with a commercial entity that has an interest in the subject of this report.
Footnotes
Published ahead of print on 18 November 2009.
REFERENCES
- 1.Carrara, S., D. Vincenti, N. Petrosillo, M. Amicosante, E. Girardi, and D. Goletti. 2004. Use of a T cell-based assay for monitoring efficacy of antituberculosis therapy. Clin. Infect. Dis. 38:754-756. [DOI] [PubMed] [Google Scholar]
- 2.Chen, X., B. Zhou, M. Li, Q. Deng, X. Wu, X. Le, C. Wu, N. Larmonier, W. Zhang, H. Zhang, H. Wang, and E. Katsanis. 2007. CD4(+)CD25(+)FoxP3(+) regulatory T cells suppress Mycobacterium tuberculosis immunity in patients with active disease. Clin. Immunol. 123:50-59. [DOI] [PubMed] [Google Scholar]
- 3.Ciardelli, L., V. Meroni, M. A. Avanzini, L. Bollani, C. Tinelli, F. Garofoli, A. Gasparoni, and M. Stronati. 2008. Early and accurate diagnosis of congenital toxoplasmosis. Pediatr. Infect. Dis. J. 27:125-129. [DOI] [PubMed] [Google Scholar]
- 4.Connell, T., N. Bar-Zeev, and N. Curtis. 2006. Early detection of perinatal tuberculosis using a whole blood interferon-gamma release assay. Clin. Infect. Dis. 42:e82-e85. [DOI] [PubMed] [Google Scholar]
- 5.Corvaisier, S., B. Charpiat, C. Mounier, M. Wallon, G. Leboucher, M. Al Kurdi, J. F. Chaulet, and F. Peyron. 2004. Population pharmacokinetics of pyrimethamine and sulfadoxine in children treated for congenital toxoplasmosis. Antimicrob. Agents Chemother. 48:3794-3800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Denkers, E. Y. 1999. T lymphocyte-dependent effector mechanisms of immunity to Toxoplasma gondii. Microbes Infect. 1:699-708. [DOI] [PubMed] [Google Scholar]
- 7.Denkers, E. Y., P. Caspar, and A. Sher. 1994. Toxoplasma gondii possesses a superantigen activity that selectively expands murine T cell receptor V beta 5-bearing CD8+ lymphocytes. J. Exp. Med. 180:985-994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Di Cristina, M., P. Del Porto, W. Buffolano, E. Beghetto, A. Spadoni, S. Guglietta, E. Piccolella, F. Felici, and N. Gargano. 2004. The Toxoplasma gondii bradyzoite antigens BAG1 and MAG1 induce early humoral and cell-mediated immune responses upon human infection. Microbes Infect. 6:164-171. [DOI] [PubMed] [Google Scholar]
- 9.Dominguez, J., M. De Souza-Galvao, J. Ruiz-Manzano, I. Latorre, C. Prat, A. Lacoma, C. Mila, M. A. Jimenez, S. Blanco, J. Maldonado, N. Altet, and V. Ausina. 2009. T-cell responses to the Mycobacterium tuberculosis-specific antigens in active tuberculosis patients at the beginning, during, and after antituberculosis treatment. Diagn. Microbiol. Infect. Dis. 63:43-51. [DOI] [PubMed] [Google Scholar]
- 10.Dunn, D., M. Wallon, F. Peyron, E. Petersen, C. Peckham, and R. Gilbert. 1999. Mother-to-child transmission of toxoplasmosis: risk estimates for clinical counselling. Lancet 353:1829-1833. [DOI] [PubMed] [Google Scholar]
- 11.Fatoohi, A. F., G. J. Cozon, M. Wallon, S. Kahi, F. Gay-Andrieu, T. Greenland, and F. Peyron. 2003. Cellular immunity to Toxoplasma gondii in congenitally infected newborns and immunocompetent infected hosts. Eur. J. Clin. Microbiol. Infect. Dis. 22:181-184. [DOI] [PubMed] [Google Scholar]
- 12.Ge, Y. Y., L. Zhang, G. Zhang, J. P. Wu, M. J. Tan, E. Hu, Y. J. Liang, and Y. Wang. 2008. In pregnant mice, the infection of Toxoplasma gondii causes the decrease of CD4+CD25+-regulatory T cells. Parasite Immunol. 30:471-481. [DOI] [PubMed] [Google Scholar]
- 13.Guglietta, S., E. Beghetto, A. Spadoni, W. Buffolano, P. Del Porto, and N. Gargano. 2007. Age-dependent impairment of functional helper T cell responses to immunodominant epitopes of Toxoplasma gondii antigens in congenitally infected individuals. Microbes Infect. 9:127-133. [DOI] [PubMed] [Google Scholar]
- 14.Jaisson-Hot, I., M. Wallon, M. al Kurdi, P. Thulliez, S. Kahi, G. Cozon, and F. Peyron. 2001. Congenital toxoplasmosis. Transitory negative serology. Presse Med. 30:1001-1004. (In French.) [PubMed] [Google Scholar]
- 15.Lalvani, A., P. Nagvenkar, Z. Udwadia, A. A. Pathan, K. A. Wilkinson, J. S. Shastri, K. Ewer, A. V. Hill, A. Mehta, and C. Rodrigues. 2001. Enumeration of T cells specific for RD1-encoded antigens suggests a high prevalence of latent Mycobacterium tuberculosis infection in healthy urban Indians. J. Infect. Dis. 183:469-477. [DOI] [PubMed] [Google Scholar]
- 16.Lebech, M., D. H. Joynson, H. M. Seitz, P. Thulliez, R. E. Gilbert, G. N. Dutton, B. Ovlisen, E. Petersen, et al. 1996. Classification system and case definitions of Toxoplasma gondii infection in immunocompetent pregnant women and their congenitally infected offspring. Eur. J. Clin. Microbiol. Infect. Dis. 15:799-805. [DOI] [PubMed] [Google Scholar]
- 17.Lyons, R. E., R. McLeod, and C. W. Roberts. 2002. Toxoplasma gondii tachyzoite-bradyzoite interconversion. Trends Parasitol. 18:198-201. [DOI] [PubMed] [Google Scholar]
- 18.McLeod, R., M. O. Beem, and R. G. Estes. 1985. Lymphocyte anergy specific to Toxoplasma gondii antigens in a baby with congenital toxoplasmosis. J. Clin. Lab. Immunol. 17:149-153. [PubMed] [Google Scholar]
- 19.McLeod, R., K. Boyer, T. Karrison, K. Kasza, C. Swisher, N. Roizen, J. Jalbrzikowski, J. Remington, P. Heydemann, A. G. Noble, M. Mets, E. Holfels, S. Withers, P. Latkany, and P. Meier. 2006. Outcome of treatment for congenital toxoplasmosis, 1981-2004: the National Collaborative Chicago-Based, Congenital Toxoplasmosis Study. Clin. Infect. Dis. 42:1383-1394. [DOI] [PubMed] [Google Scholar]
- 20.Montoya, J. G., and O. Liesenfeld. 2004. Toxoplasmosis. Lancet 363:1965-1976. [DOI] [PubMed] [Google Scholar]
- 21.Purner, M. B., R. L. Berens, S. Tomavo, L. Lecordier, M. F. Cesbron-Delauw, B. L. Kotzin, and T. J. Curiel. 1998. Stimulation of human T lymphocytes obtained from Toxoplasma gondii-seronegative persons by proteins derived from T. gondii. J. Infect. Dis. 177:746-753. [DOI] [PubMed] [Google Scholar]
- 22.van der Werff Ten Bosch, J., P. Schotte, A. Ferster, N. Azzi, T. Boehler, G. Laurey, M. Arola, C. Demanet, R. Beyaert, K. Thielemans, and J. Otten. 2002. Reversion of autoimmune lymphoproliferative syndrome with an antimalarial drug: preliminary results of a clinical cohort study and molecular observations. Br. J. Haematol. 117:176-188. [DOI] [PubMed] [Google Scholar]
- 23.Villavedra, M., C. Rampoldi, H. Carol, A. Baz, J. J. Battistoni, and A. Nieto. 2001. Identification of circulating antigens, including an immunoglobulin binding protein, from Toxoplasma gondii tissue cyst and tachyzoites in murine toxoplasmosis. Int. J. Parasitol. 31:21-28. [DOI] [PubMed] [Google Scholar]
- 24.Wallon, M., G. Cozon, R. Ecochard, P. Lewin, and F. Peyron. 2001. Serological rebound in congenital toxoplasmosis: long-term follow-up of 133 children. Eur. J. Pediatr. 160:534-540. [DOI] [PubMed] [Google Scholar]
- 25.Wallon, M., D. Dunn, D. Slimani, V. Girault, F. Gay-Andrieu, and F. Peyron. 1999. Diagnosis of congenital toxoplasmosis at birth: what is the value of testing for IgM and IgA? Eur. J. Pediatr. 158:645-649. [DOI] [PubMed] [Google Scholar]
- 26.Wallon, M., L. Kodjikian, C. Binquet, J. Garweg, J. Fleury, C. Quantin, and F. Peyron. 2004. Long-term ocular prognosis in 327 children with congenital toxoplasmosis. Pediatrics 113:1567-1572. [DOI] [PubMed] [Google Scholar]
- 27.Wilson, C. B., G. Desmonts, J. Couvreur, and J. S. Remington. 1980. Lymphocyte transformation in the diagnosis of congenital toxoplasma infection. N. Engl. J. Med. 302:785-788. [DOI] [PubMed] [Google Scholar]