Abstract
Background
Day laborers in the US, comprised largely of undocumented immigrants from Mexico and Central America, suffer high rates of occupational injury according to recent estimates. Adequate surveillance methods for this highly transient, largely unregulated group do not currently exist. This study explores chart abstraction of hospital-based trauma registry records as a potential injury surveillance method for contingent workers and day laborers. We sought to determine the degree of completeness of work information in the medical records, and to identify day laborers and contingent workers to the extent possible.
Methods
Work-related injury cases from a hospital-based trauma registry (2001–2006) were divided by ethnicity (Hispanic vs. non-Hispanic origin) and presence of social security number (SSN: yes, no), resulting in four groups of cases. Medical records were abstracted for 40 cases from each group; each case was assigned values for the variables “day labor status” (yes, no, probably not, probable, unknown) and “employment type” (contingent, formal, unknown).
Results
Work information was missing for 60% of Hispanic cases lacking SSN, as compared with 33–47% of the other three groups. One “probable” day laborer was identified from the same group. Non-Hispanics with SSN were less frequently identified as contingent workers (5% as compared with 15–19%).
Conclusions
This method revealed severe limitations, including incomplete and inconsistent information in the trauma registry and medical records. Approaches to improve existing resources for use in surveillance systems are identified. The potential of an active surveillance approach at day labor hiring centers is also briefly discussed.
Keywords: day labor, occupational injury surveillance, contingent, trauma registry
A man who came to the U.S. 8 months ago from Mexico was struck by lightning while working on a rooftop in the rain. The lightning entered through the back of his head, burned his chest, and left an exit burn through the foot.
A Caucasian was working on a roof when he fell off backwards, falling 18′ to concrete. Vocationally, he has only worked as a manual laborer and is currently not gainfully employed.
A Spanish-speaking homeless laborer/drywall worker fell 6 feet from scaffolding.
A Russian-speaking worker fell 10–15 feet from a scaffold and died in the emergency room.
These narratives are summarized from the medical records of four work-related injury cases from the King County Trauma Registry.
INTRODUCTION
Occupational injury rates in day laborers are high compared with average rates in the US [Seixas et al., 2008]. These disparities in injury rates may be due to occupational, personal, and political factors. Each day, over 100,000 day laborers across the US await potential employers on street corners or at hiring centers for jobs in construction, landscaping, and moving and hauling [Valenzuela et al., 2006]. Day labor jobs are hazardous, with frequent exposures to chemicals and dust, use of substandard equipment, and lack of personal protective equipment and safety training [Walter et al., 2002; Valenzuela et al., 2006]. Personal factors related to social position may also be associated with injury risk and health disparities, including race/ethnicity, immigration status, language skills, income, and education levels [Quinn et al., 2007]. A national survey of day laborers estimated that 98% of day laborers are male, 93% are foreign-born, 75% are undocumented, and 60% have been in the US for less than 5 years. In particular, an estimated 59% are from Mexico and 28% are from Central America [Valenzuela et al., 2006].
Day labor is one component of the rise in “contingent work” in the US, in which informal, temporary agreements are made between workers and employers in order to ease cost pressures [Valenzuela et al., 2006]. Day laborers tend to work at mobile and informal job sites which are subject to little government regulation; they are paid in cash, and wage theft is common [Theodore et al., 2006]. Fear of economic losses and legal consequences makes day laborers less likely to challenge unsafe conditions. Competition for day labor jobs is intense, further perpetuating low wages and poor working conditions [Theodore et al., 2006].
Recent studies suggest that occupational injury rates in day laborers are high. In 2006, a survey of 180-day laborers was conducted at two hiring centers and a street location in Seattle, and roughly estimated an injury rate of 31 injuries per 100 full-time employees (FTE). The case definition included injuries that “occurred at work, and forced you to stop working and required first aid and/or medical treatment.” A limitation of this approach was the exclusion of more severely injured workers, who would not have been present for the survey [Seixas et al., 2008]. Another study surveyed 2,660 randomly selected day laborers at 264 hiring sites around the country, and estimated that about one in five day laborers had suffered an injury on the job. The definition of injury and the period of exposure were not specified [Valenzuela et al., 2006]. A similar study conducted as a part of the same survey focused on 29 sites in the greater New York City area, and estimated the same injury rate. Authors noted limitations likely to result in the underestimation of day laborers, including the potential for missed sites, workers who had already left the site, and worker absences due to sickness or injury [Theodore et al., 2006].
CHALLENGES IN DAY LABOR INJURY SURVEILLANCE
The two elements necessary for accurate injury surveillance are complete ascertainment of cases, and an accurate description of the at-risk population from which the cases arose. Sources most commonly used for occupational injury surveillance are likely to greatly underestimate the number of occupational injuries in contingent workers, particularly day laborers. Workers’ compensation data depend on worker reporting; however, undocumented workers may be less inclined to report injuries as work-related [Friedman and Forst, 2007]. The Bureau of Labor Statistics (BLS) depends on employer reporting, but this, too, misses workers in informal work relationships. Companies generally hire day laborers off the record, and homeowners, who account for about 50% of day labor hiring [Valenzuela et al., 2006], are not surveyed by the BLS [2002, http://www.bls.gov/iif/oshsum1.htm]. Estimating the population at risk also poses challenges, as there is no registry of informal workers, and it can be difficult to define day labor in particular. Day labor may be a full-time pursuit or a second job, and a worker’s status may fluctuate between job seeker, informal day laborer, and employee in the formal labor market [Theodore et al., 2006]. Person-time at risk also poses challenges, as day laborers work a variable number of days per week and hours per day.
Trauma registries are an important tool used to collect data for research, to evaluate effectiveness of different treatments, and to ensure quality of care [Layde et al., 1996; Guice et al., 2007]. As population-based systems, they offer the opportunity to identify cases which may be missed through employer-based systems. They contain information specifically on severe injuries, which may warrant more attention due to greater individual, societal, and financial impact [Friedman and Forst, 2007]. In 2004, 32 states had a functioning statewide trauma registry with variations in reporting requirements [Guice et al., 2007], inclusion criteria, and coding [Mann et al., 2006].
Trauma registries have been effectively used to describe occupational injuries. A rural emergency-department-based injury surveillance system was used to describe work-related injury in a rural West Virginia population; it included trauma registry cases as well as other emergency department cases. Work relatedness was determined by patient’s report that the injury occurred while at work. Authors summarized demographics, mechanisms and types of injuries, and hospitalization time and costs [Williams et al., 1997]. In another study, annual occupational injury rates were calculated for Illinois workers who were seen at Level I or II trauma centers with a stay of at least 12 hr. Work relatedness was determined by data abstraction of a patient’s records by trained personnel following hospital discharge. Employment data from the Current Population Survey, a household survey conducted by the BLS, was used to estimate rates [Friedman and Forst, 2007]. The Alaska Trauma Registry has also been used for surveillance of occupational injuries related to construction, fishing, and animal exposures. Work relatedness in this trauma registry is similarly determined by data abstraction of medical records [Thomas et al., 2001; Husberg et al., 2005; Mode et al., 2005]. These studies highlight the strengths of trauma registries for identifying occupational injuries and for describing demographic, injury, and outcome characteristics, but the registries do not include information on employment type or contingency of work.
It is essential to improve upon the current occupational injury surveillance methods in difficult-to-study contingent worker populations in order to better understand injury disparities and to more effectively implement and assess prevention programs. The study aimed to explore chart abstraction of trauma registry cases as a potential occupational injury surveillance method for contingent workers and day laborers by determining the degree of completeness of work information in the medical records, and identifying these workers when possible.
METHODS
The trauma registry at the Harborview Medical Center (HMC, Seattle, WA) is a part of the Central Region Trauma Registry and the Washington State Trauma Registry (WSTR). The WSTR includes all cases with an ICD-9 injury code of 800–904 (fractures, dislocations, strains, sprains, intracranial and internal injuries, open wounds, injuries to blood vessels), 910–929 (superficial injuries, contusions, crushing injuries), 940–959 (burns, injuries to nerves and spinal cord, unspecified injuries, traumatic complications), 994.1 (drowning), 994.7 (asphyxiation), or 994.8 (electrocution). Additional criteria include that either a surgeon was required, that the patient was dead on arrival, died in the hospital, was transferred by EMS to or from the hospital, or, if over 14 years old, stayed for more than 48 hr [WSTR Inclusion Criteria, 2002; CDC, 2008]. The trauma registry includes over 2,000 variables, which provide demographic and insurance information, injury classifications, and detailed medical treatment information. A work-related variable indicates whether the injury was occupational; this compulsory field is coded by an abstractor using emergency room notes and hospital discharge data. Another variable, the injury severity score (ISS), is an overall anatomical severity score which combines the severity scores of up to three injuries in different body regions [Wong and Leung, 2008]. Researchers obtained the trauma registry records of all injuries which occurred between January 1, 2001, and December 31, 2006, which were coded as work-related, and which were seen at HMC. Because the registry variables did not include any description of work circumstances, medical records were used to search for this information for a subset of cases. All procedures for the study were approved by the Institutional Review Board at the University of Washington.
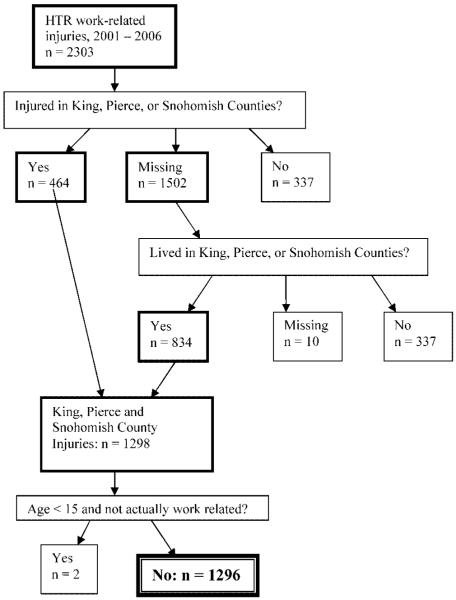
A total of 1,296 cases were identified from the HMC trauma registry as work-related injuries in the Seattle area, which was defined as King, Pierce, and Snohomish Counties (see Fig. 1). The variable county of injury, recorded in 35% of records, was used to exclude injuries occurring outside the Seattle area. For the remaining 65%, the zip code of residence was used to approximate county of injury. Both locations were missing in less than 0.5% of records, and these data were not included. Finally, three of the remaining injury cases were below the age of 15; their charts were read individually and two were removed as they clearly were not work-related.
FIGURE 1.
Case selection procedure.
Of the 1,296 cases, a sample of 160 was selected for the process of chart abstraction in order to investigate the availability of employment information within the medical records. Abstracting all 1,296 cases was not feasible, as chart abstraction is a time-consuming process, requiring careful reading of lengthy transcripts. The 1,296 cases were first divided into four groups based on the trauma registry variables of ethnicity (Hispanic origin: yes/no) and social security number (SSN; yes/no). Recalling that approximately 87% of day laborers nationwide are from Central America or Mexico, and about 75% of day laborers are undocumented [Valenzuela et al., 2006], this grouping was expected to make our investigation of work contingency information more efficient. Specifically, the Hispanic group lacking SSN was expected to have a higher concentration of day laborers. Non-Hispanics with SSN comprised the largest group, with 1,067 cases, followed by Hispanics with SSN (n = 135). Cases lacking SSN included 44 non-Hispanics and 41 Hispanics. Forty cases were randomly selected from each of the four groups, yielding a total of 160 cases for chart abstraction. Medical records for each case were then read, and included coded information similar to that in the registry, such as demographics, injury type, and diagnosis, as well as, in most cases, between one and several dozen written transcripts, including intake and discharge notes, social work notes, operating notes, and lab reports.
The subset of 160 was used to determine whether and to what extent contingent workers, and specifically day laborers, could be identified from medical records. Each case was defined by employment type (Contingent, Formal, Unknown), and the degree of certainty for each (Definite, Probable, Tentative), as well as day labor status (Yes, No, Probably, Probably Not, Unknown), and industry. Levels of certainty were assigned to allow for greater flexibility in cases where the evidence suggested, but did not confirm, an employment type. Data were also collected on work characteristics, injury cause, language, insurance, gender, and race, some of which were used to check for agreement with the trauma registry data. For each of the four groups, the proportions of cases identifiable in terms of both employment type and day labor status, respectively, were estimated. In order to estimate the percent of the 1,296 cases for which chart abstraction could be used to identify employment type and day labor status, weighted averages were calculated. (The subset of 160 cases was not representative of the 1,296 work-related cases in the database, due to the stratified sampling.) Weighted averages were calculated by multiplying the percent identifiable in a particular group by the fraction of the total 1,296 comprised by that group, and then summing across the four groups.
Work variables were coded based on the information available in the medical records, as detailed in Table I. For employment type and level of certainty, for example, a “self-employed arborist” was coded as a Definite Contingent worker, as he clearly fit at least one of the contingent criteria (self-employed). Another worker was described as “homeless; lives in Seattle; fell from ladder in AK,” and cited to have multiple jobs, which implied short-term contract work; he was coded as Probable Contingent. Several workers had construction jobs which they lost after the injury, including a painter and a roofer; these were coded as Tentative Contingent, as this was suggestive of temporary or shortterm work. Definite Formal was assigned for a “manager at construction site,” and a “foreman in freight loading,” as records indicated formal, fixed employment. Probable Formal was assigned for a worker who had returned full-time to a job, such as “line worker,” “bus driver,” and “factory worker.” Finally, Tentative Formal was assigned for a case who “wants to return to job at wood plant,” which provided indirect evidence of a steady full-time job.
TABLE I.
Definition of Variable Codes
| Variable | Value | Definition |
|---|---|---|
| Day Labor Status | Yes | Confirmed day labor status, such as mention that work was contracted from a day labor center or the street |
| No | Definite evidence against day labor work, including an employer known not to hire day laborers, a return to a specified, non-day labor job, or a job description which is not consistent with the nature of day labor |
|
| Probably | Evidence that the case was very likely working in day labor | |
| Probably Not | Evidence of job which falls outside of general day labor work, a longer term contract, or long-term work in a specific task |
|
| Unknown | No information helped to distinguish whether the subject was a day laborer | |
| Employment Type | Contingent | One or more of the following: part-time, self-employed, no fixed employer, temporary contract work |
| Formal | Employment was likely full-time, long-term, and with a fixed employer (not self-employed) | |
| Unknown | Employment unknown, or equally likely to be formal or contingent | |
| Contingent Level of Certainty | Definite | The case clearly fits at least one of the criteria (above) for contingent employment type |
| Probable | Probably met at least one of the criteria | |
| Tentative | Records suggest that at least one of the criteria was met | |
| Formal Level of Certainty | Definite | Records included information that specifically identified fixed, non-self-employed work |
| Probable | Formal employment seemed likely based on the employment information, industry, or type of worka | |
| Tentative | Information was suggestive of formal employmenta |
While transcripts often mentioned a subject’s return to the same job post-injury, it was rarely explicitly stated whether the work was full-time, long-term employment; however tentative and probable assignments were made in some cases, based on the nature of the work. Some jobs tend to be formal employment (i.e., bus driver, lawyer), in which case a value of tentative or probable was assigned, whereas others may be formal or contingent (waiter, framer, cook, painting), and in these cases, “unknown” was assigned.
Each of the 160 cases was also assigned a value for Day Labor Status, including Yes, No, Probably, Probably Not, and Unknown (Table I). Some cases were identified as definitely Not day laborers, such as a janitor at a public school. No cases were identified as confirmed day laborers. A worker described as homeless, with occupation identified as “laborer” working in construction, was coded as a Probable day laborer, as day labor seemed highly likely based on the work description. A worker who “has subcontracted window cleaning for the past 7 years” was coded as Probably Not a day laborer, as the description provides evidence of more formal employment. Unknown was assigned for a “construction worker,” with no additional information, as this may or may not describe a day laborer.
Other variables collected during chart abstraction included industry, employer, country of origin, language used, work at time of injury, how injury occurred, occupation, race, and gender. Occupation was found on the demographics page and sometimes in the transcripts; multiple occupations were recorded when they were listed in the records. For example, “laborer” on the demographics page was combined with “drywaller” from the transcripts.
RESULTS
The 1,296 work-related injury cases from the Trauma Registry were mostly white males of non-Hispanic origin with SSN and a mean age of 40 years (Table II). The number of occupational injuries per year ranged from 172 to 270. For cases of Hispanic ethnicity, race was coded as either White (n = 107) or Other (n = 69); these cases accounted for all but two cases of race “Other.” Thus, race “Other” is essentially synonymous with Hispanic origin within this data set. Nearly 1 in 4 cases of Hispanic origin was missing SSN, as compared with just 1 in 25 for non-Hispanic cases. The average age of Hispanic cases was 8 years less than that of non-Hispanics, with mean ages of 32 and 40 years, respectively. Those lacking SSN similarly had a mean age of 32 as compared with a mean age of 40 in those with SSN. Nearly a quarter of non-Hispanics without SSN were found to have died at HMC or were dead on arrival, as compared with less than 5% of the other groups, thus several analyses were compared with and without deaths.
TABLE II.
Work-Related Injuries in King, Pierce, and Snohomish Counties: Demographics, Injury Severity, and Deaths
| Cases, n (%) | ISS mean (std dev.) (n = 1,293) |
Number of deaths, n (%) |
|
|---|---|---|---|
| Total | 1,296 (100) | 11 (11.3) | 35 (100) |
| Gender | |||
| Male | 1,158 (89) | 12 (11.1) | 31 (89) |
| Female | 138 (11) | 11 (13.0) | 4 (11) |
| Missing | 1 (0.1) | — | 0 |
| Race | |||
| White | 1,039 (80) | 12 (11.3) | 28 (80) |
| Black | 57 (4) | 10 (12.4) | 2 (6) |
| Native American | 5 (0.4) | 6 (6.5) | 0 |
| Asian | 71 (6) | 12 (12.3) | 4 (11) |
| Other | 71 (6) | 12 (12.2) | 1 (3) |
| Missing | 53 (4) | 8 (7.0) | 0 |
| Ethnic | |||
| Hispanic origin | 176 (14) | 10 (9.8) | 2 (6) |
| Non-Hispanic origin | 1,111 (86) | 10 (8.8) | 33 (94) |
| Missing | 9 (0.7) | — | 0 |
| Age category | |||
| 5–14 | 1 (0.1) | 9 (—) | 0 |
| 15–24 | 185 (14) | 9 (10.8) | 3 (9) |
| 25–34 | 329 (25) | 11 (10.6) | 4 (11) |
| 35–64 | 760 (59) | 12 (11.8) | 28 (80) |
| 65+ | 21 (2) | 13 (8.2) | 0 |
| Has SSN | |||
| Yes | 1,211 (93) | 11 (10.6), 10 (9.5)a | 22 (63) |
| No | 85 (7) | 18 (17.5), 14 (11.9)a | 13 (37) |
| Year | |||
| 2001 | 172 (13) | 10 (12.2) | 3 (9) |
| 2002 | 215 (17) | 10 (9.2) | 9 (26) |
| 2003 | 190 (15) | 10 (9.8) | 4 (11) |
| 2004 | 194 (15) | 10 (9.2) | 5 (14) |
| 2005 | 248 (19) | 12 (11.1) | 3 (9) |
| 2006 | 270 (21) | 15 (14.3) | 11 (31) |
Excluding deaths.
Chart abstraction for work arrangement information was conducted for the full sample of 160 cases stratified by presence of SSN and ethnicity. Five of these cases were found to be non-occupational injuries and were excluded from the analysis. Employment Type was able to be identified (definitely, probably, or tentatively) in 54% of cases (Table III). One quarter of these were identified as contingent, and three quarters as formal. Information on Employment Type was missing in the remaining 46% of cases.
TABLE III.
Employment Type, Day Labor Status by Hispanic Ethnicity and SSN Information
| Employment type: n (%) |
Day labor status: n (%) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Hispanic | SSN | n | Formal | Contingent | Unknown | No/prob. not | Probable | Unknown |
| N | Y | 38 | 18 (47) | 2 (5) | 18 (47) | 28 (74) | 0 (0) | 10 (26) |
| N | N | 37 | 14 (38) | 7 (19) | 16 (43) | 28 (76) | 0 (0) | 9 (24) |
| Y | Y | 40 | 21 (53) | 6 (15) | 13 (33) | 28 (70) | 0 (0) | 12 (30) |
| Y | N | 40 | 10 (25) | 6 (15) | 24 (60) | 15 (38) | 1 (3) | 24 (60) |
| Total | 155 | 63 (41) | 21 (14) | 71 (46) | 99 (64) | 1 (1) | 55 (36) | |
Employment type was able to be classified with a “definite” level of certainty in 14 cases (9%), including 6 contingent cases and 8 formal cases (Table IV). Hispanics lacking SSN were twice as likely as other groups to be missing information on Employment Type. Non-Hispanics with SSN were less likely to be identified as contingent workers (5% as compared with 15–19%). Of cases with an identifiable Employment Type, presence of SSN appeared to be a more important factor than ethnicity. Cases lacking SSN were more likely to be contingent workers, a pattern which was more extreme when hospital deaths were excluded; about 40% of cases with no SSN were contingent, as compared with 10% and 22% of cases with SSN, for non-Hispanics and Hispanics, respectively.
TABLE IV.
Availability of EmploymentType and Day Labor Status in Sample and as Applied to All Work-Related Cases
| Employment type: n (%) |
Day labor status: n (%) |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Hispanic | SSN | n | Definite | Probable/ tentative |
Unknown | Definite | Probable/ tentative |
Unknown | Weight of each groupa |
| N | Y | 38 | 2 (5) | 18 (47) | 18 (47) | 20 (53) | 8 (21) | 10 (26) | 0.829 |
| N | N | 37 | 2 (5) | 19 (51) | 16 (43) | 25 (68) | 3 (8) | 9 (24) | 0.034 |
| Y | Y | 40 | 6 (15) | 21 (53) | 13 (33) | 23 (58) | 5 (13) | 12 (30) | 0.105 |
| Y | N | 40 | 4 (10) | 12 (30) | 24 (60) | 12 (30) | 4 (10) | 24 (60) | 0.032 |
| Total | 155 | 14 (9) | 70 (45) | 71 (46) | 80 (52) | 20 (13) | 53 (34) | ||
| Estimated % of cases identifiableb | 6% | 47% | 46% | 53% | 19% | 28% | |||
The proportion of all 1,296 work-related cases constituted by each group, for example, non-Hispanics with SSN make up 82.9% of work-related cases.
Estimated proportion of all work-related cases which would be identifiable using chart abstraction. Original percentages are multiplied by their corresponding “weight“; for example, 5% of non-Hispanics with SSN were assigned a “Definite” employment type, which is multiplied by 0.829. The 5% of non-Hispanics lacking SSN were multiplied by a weight of 0.034, and so on. Percentages were then summed.
Day Labor Status was identified in 65% of the 155 work-related cases abstracted, though it was unable to be identified due to missing information in the remaining 35% of cases (Table IV). It was identified definitively (specifically, as No) in 52% of cases, and with a Probable level of certainty in another 13% of cases; 1 was a Probable day laborer (0.6%), while 19 were Probably Not day laborers (12%) (see Table III). The one Probable day laborer was identified in the group of Hispanics lacking SSN; cases in this group were also at least twice as likely to be missing information on day labor status, and half as likely to be identified as Not or Probably Not day laborers. Weighting these estimates by the relative size of each group suggests that day labor status would be identifiable in an estimated 72% of work-related cases (53% definitely), and employment type in 54% (6% definitely) (Table IV).
Construction was overwhelmingly the largest identifiable industry for both; more so for Hispanics (58%) than for non-Hispanics (29%). Food services were the second-largest industry for cases of Hispanic origin (11%), while transport was the second-largest industry for cases of non-Hispanic origin (11%).
DISCUSSION
Occupational injury surveillance for workers in contingent employment situations is extremely challenging, particularly for day laborers. In this study, we explored the use of a regional hospital-based trauma registry to identify occupational injuries in this workforce. While the registry was coded to identify the occupational cause of the injury, no information about the nature of the employment was present in the registry database. Therefore, we explored the utility of medical records in identifying this information.
One anticipated challenge was the difficulty in estimating the size of the at-risk population, in part because trauma registries have an uncertain catchment area [Layde et al., 1996]. Catchment depends on injury location and severity, and availability and preparedness of alternate hospitals. Within a smaller radius of the trauma center, all injuries requiring hospital attention may go to the trauma center, as it is the closest hospital. Farther away, less severe injuries may instead go to closer hospitals or clinics; thus, only the most severe injuries will be seen at the trauma center, making estimation of the denominator population unfeasible. A major challenge associated with the trauma registry was data completeness and accuracy. The county in which the injury occurred was missing in 65% of records. Zip code of residence was used as a proxy, but it is possible that this variable does not adequately represent location of injury. False information is a possibility as well; for instance, false SSNs may have been used. Undocumented workers may use false SSNs out of fear of legal consequences of being discovered, such as loss of employment or deportation. It is possible that a portion of the cases identified as having SSNs actually used false numbers.
Additional challenges encountered during the process of chart abstraction included data accuracy and consistency. Race and ethnicity were not coded consistently across the registry and charts. “Hispanic” was listed as the race in some medical records, while in the registry, Hispanic origin was coded as a separate variable, ethnicity. Lack of work-related information in the medical records was another major challenge to the identification of Employment Type and Day Labor Status. Although some cases had medical records with detailed information on occupation, about half of the cases abstracted contained none. The work-related variable was also found to be miscoded in some instances. Information in the medical records revealed that 5 of the 160 cases selected for chart abstraction had been miscoded as work-related, such as a “systems analyst” injured while doing maintenance on his home. While sensitivity of the work-related variable cannot be estimated without knowing the true number of work-related cases, an approximate positive predictive value of this variable, using the medical records as a gold standard, would be 155/160 = 97%. The actual value is likely to be lower, given the lack of work-related information in many of the medical records.
Missed work-related cases may be of greater concern; two studies have reported that 14% and 25% of work-related trauma registry cases, respectively, were miscoded as not work-related [Azaroff et al., 2003; Friedman and Forst, 2007]. An additional investigation of injuries not coded as work-related in this trauma registry was carried out to address this question. An abbreviated chart abstraction looking specifically for work information was performed on 40 cases of any ethnicity and SSN status, and another 40 specifically of Hispanic ethnicity and lacking SSN, all between the ages of 15 and 65, from 2001 to 2006, and coded as not work-related. (Forty cases per group were chosen to be consistent with the size of the initial four groups, and due to feasibility considerations.) As work relatedness is coded based on information in the emergency room notes and the discharge notes, chart abstraction would catch miscoded cases which only had work information in other medical records, such as social work notes, in addition to any that were accidentally miscoded despite work information present in emergency room and discharge notes. It would not catch work-related cases which had no work information in the medical records. In fact, 0 of the 80 cases were confirmed as miscoded, and the lack of work information was, not surprisingly, an even greater challenge among this group. Twenty-eight (70%) of the cases of any ethnicity and SSN, and 19 (48%) of the Hispanic cases lacking SSN, were confirmed as not work-related.
The failure to find miscoded work-related cases could potentially be attributed to (a) the absence of miscoding; (b) missing information due to language, injury severity, or other factors; and (c) a relatively low frequency of miscoded work-related injuries. Injuries coded as work-related constitute approximately 12% of all injuries in the trauma registry. If 25% of work-related injuries were miscoded, then the 12% coded as work-related would represent 75% of true work-related cases, with an additional 4% of cases miscoded as not work-related. Another way to estimate this figure would be to check for workers’ compensation coverage among those coded as not work-related, as carried out in other studies [Friedman and Forst, 2007].
Another major challenge in chart abstraction was subjectivity, particularly in assigning employment types and levels of certainty. In order to maximize consistency, one researcher abstracted charts for all 160 cases. After all relevant work information was extracted and values were tentatively assigned, all cases and relevant employment information were discussed between multiple researchers. Despite challenges inherent in choosing between the subtle differences of “probable” versus “tentative,” this method allowed maximum use of the limited information given; a tentative assignment was still more valuable than classifying a case as “unknown.” Additionally, “probable” and “tentative” cases were ultimately not distinguished from each other in the analysis.
It is not certain why the “Hispanic, no SSN” group had less information than the other three groups; possible explanations include a language barrier which prevented both SSN and other information from being collected, or more severe injury with the same result. Injury severity as represented by ISS does not appear to explain the differences, as similar mean ISSs were seen across groups (Table II).
Cases lacking SSN were much more likely to have died in or before arrival to the hospital; 15% of cases lacking SSN died in the hospital, whereas less than 2% of cases with SSN died. As this did not seem to be entirely explained by differences in injury severity between the two groups, it may be that in the case of a death, SSN was less likely to be recorded, whether because it was more difficult to obtain or for some other reason. It appears that there were some differences in the number of deaths across race and ethnicity categories, but further analysis of the distribution of deaths in this population is uncertain because many fatalities would not be seen at the trauma center and thus would not even make it into the database.
An alternate method of day labor injury surveillance which we attempted is worth mentioning in considering the challenges and possibilities of this task. An active surveillance reporting system was implemented for 3 months at two day labor hiring centers, in which reports of injuries occurring within the past 2 years were solicited at weekly safety trainings. An injury report form was used to interview workers and collect data on cause and type of injury and personal and job characteristics. Of the 12 reports collected, the majority were muscle or joint injuries, were caused by falls, and occurred on construction jobs. Frequency of reporting depended on the method used to solicit participation, thus there were challenges in maintaining a systematic approach. For example, approaching workers individually while they were awaiting work was more effective than making an announcement to a large group. This one-on-one approach made it easier and less threatening for workers to respond and to discuss their injury experiences within the past 2 years. A lack of strong incentives for participation, as well as differences in perceptions of injuries, also may have influenced reporting. Injury surveillance among day laborers remains a very challenging problem, and we have not identified an effective way to address this. Solicitation of injury reports among a population in this way is not sufficiently systematic; to ascertain injuries more systematically a survey would probably be more effective.
CONCLUSION
Medical chart abstraction from a trauma registry is not well suited as a means of identifying work contingency or employment type, due to inconsistencies in the availability of employment information in the records. However, a few improvements in the injury surveillance system could greatly increase its utility. Requiring the collection of work-related information in the registry and charts, such as employment and employer characteristics, and length of time at current job, would be a valuable addition. Inclusion of cases with at least a 12-hr stay (instead of a 48-hr stay) at the trauma center might permit a broader, more inclusive representation of severe occupational injuries. Additionally, this study has demonstrated that chart abstraction has the potential to provide a level of information for some cases not seen in other sources of injury data. This data source would be valuable for qualitative investigation and generation of hypotheses around social and other factors related to occupational injury in day laborers, precarious workers, and other high-risk groups, as well as inquiries into the nature of severe work-related injuries in general.
Another consideration is that the Employment Type variable, with its two values contingent and formal, may fail to meaningfully explain risk of injury or other negative outcomes related to health care, job security, or financial repercussions. For example, in the following summary of one case, Employment Type failed to capture what might be called “work precariousness”:
A Spanish-speaking laborer/roofer worked for a local company for two years illegally, and the company now refuses to pay the medical expenses and time loss, and denies that he works for them.
Despite the precariousness of this employment situation, this case was coded as formal, given the duration of the employment. Perhaps formal and contingent work should be defined differently; does a self-employed business owner belong in the same category as a short-term precarious worker? Or perhaps employment type should be replaced with another variable or set of variables that might more effectively capture this “precariousness.”
These attempts at occupational injury surveillance in day laborers have highlighted the need for continued efforts toward better surveillance systems. In order to most successfully conduct injury surveillance, and ultimately to inform and implement injury prevention strategies, it is necessary to gain a better understanding of the injury experience of day laborers. Both the chart abstraction process and the workers’ injury reports have raised new questions, such as where workers seek medical care. Social and personal factors including homelessness, lack of support networks, pre-existing medical conditions, and poor access to preventive services may play a significant role in workers’ injury experiences as well as their likelihood to report injuries, particularly in more marginalized populations such as day laborers. In order to improve injury surveillance of this population, both the injury count and the estimation of the denominator of workers must be improved. In addition to previously mentioned suggestions for improving the trauma registry’s ability to detect injuries, worker centers may also have potential, particularly in monitoring less severe injuries missed by trauma registries. Relevant measures for estimating the denominator include the number of day laborers seeking work on a given day, and the number actually dispatched to jobs daily, with some estimation of the approximate length of the job. Injury counts could be improved by prioritization of injury reporting within the centers, through more direct involvement of hiring center staff in report recruitment, and by creating outcomes of reporting which more directly affect the workers. Limitations of using a trauma registry or solicitation of injury reports through a worker center underscore the challenges and the importance of injury surveillance in this highly vulnerable population. Workers, regardless of type of employment and documentation status, are entitled to a jobsite which is free of unnecessary risk of injury, and they are entitled to receive medical care for any injuries without fear of legal consequences.
ACKNOWLEDGMENTS
The authors would like to thank the staff at the Seattle day labor hiring centers for their generous assistance with this study. Funding was provided by the Department of Environmental and Occupational Health Sciences and Northwest Center for Occupational Safety and Health, under training grant, T42 OH008433 from the National Institute for Occupational Safety and Health of the Centers for Disease Control and Prevention.
Contract grant sponsor: National Institute for Occupational Safety and Health of the Centers for Disease Control and Prevention; Contract grant number: T42 OH008433; Contract grant sponsor: Department of Environmental and Occupational Health Sciences.
REFERENCES
- Azaroff LS, Levenstein C, Wegman DH. Occupational health of Southeast Asian immigrants in a US city: A comparison of data sources. Am J Public Health. 2003;93(4):593–598. doi: 10.2105/ajph.93.4.593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC. US Department of Health and Human Services National Center for Health Statistics ICD-9-CM List of Three Digit Categories (FY09) 2008 ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Publications/ICD9-CM/2008/
- Friedman LS, Forst L. Occupational injury surveillance of traumatic injuries in Illinois, using the Illinois trauma registry: 1995–2003. J Occup Environ Med. 2007;49(4):401–410. doi: 10.1097/JOM.0b013e31803b9527. [DOI] [PubMed] [Google Scholar]
- Guice KS, Cassidy LD, Mann NC. State trauma registries: Survey and update—2004. J Trauma. 2007;62(2):424–435. doi: 10.1097/01.ta.0000200862.93527.1c. [DOI] [PubMed] [Google Scholar]
- Husberg BJ, Fosbroke DE, Conway GA, Mode NA. Hospitalized nonfatal injuries in the Alaskan construction industry. Am J Ind Med. 2005;47(5):428–433. doi: 10.1002/ajim.20158. [DOI] [PubMed] [Google Scholar]
- Layde PM, Stueland DT, Nordstrom DL. Representativeness of trauma center registries for farm injury surveillance. Accid Anal Prev. 1996;28(5):581–586. doi: 10.1016/0001-4575(96)00028-0. [DOI] [PubMed] [Google Scholar]
- Mann NC, Guice K, Cassidy L, Wright D, Koury J. Are statewide trauma registries comparable? Reaching for a national trauma dataset. Acad Emerg Med. 2006;13(9):946–953. doi: 10.1197/j.aem.2006.04.019. [DOI] [PubMed] [Google Scholar]
- Mode NA, Hackett EJ, Conway GA. Unique occupational hazards of Alaska: Animal-related injuries. Wilderness Environ Med. 2005;16(4):185–191. doi: 10.1580/1080-6032(2005)16[185:uohoaa]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Quinn MM, Sembajwe G, Stoddard AM, Kriebel D, Krieger N, Sorensen G, Hartman C, Naishadham D, Barbeau EM. Social disparities in the burden of occupational exposures: Results of a cross-sectional study. Am J Ind Med. 2007;50(12):861–875. doi: 10.1002/ajim.20529. [DOI] [PubMed] [Google Scholar]
- Seixas NS, Blecker H, Camp J, Neitzel R. Occupational health and safety experience of day laborers in Seattle, WA. Am J Ind Med. 2008;51(6):399–406. doi: 10.1002/ajim.20577. [DOI] [PubMed] [Google Scholar]
- Theodore N, Valenzuela A, Meléndez E. La esquina (the corner): Day laborers on the margins of New York’s formal economy. Labor USA: J Labor Soc. 2006;9(4):407–423. [Google Scholar]
- Thomas TK, Lincoln JM, Husberg BJ, Conway GA. Is it safe on deck? Fatal and non-fatal workplace injuries among Alaskan commercial fishermen. Am J Ind Med. 2001;40(6):693–702. doi: 10.1002/ajim.10010. [DOI] [PubMed] [Google Scholar]
- Valenzuela A, Theodore N, Meléndez E, Luz Gonzalez A. On the corner: Day labor in the United States. UCLA; 2006. http://www.sscnet.ucla.edu/issr/csup/index.php. [Google Scholar]
- Walter N, Bourgois P, Margarita Loinaz H, Schillinger D. Social context of work injury among undocumented day laborers in San Francisco. J Gen Intern Med. 2002;17:221–229. doi: 10.1046/j.1525-1497.2002.10501.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams JM, Higgins D, Furbee PM, Prescott JE. Work-related injuries in a rural emergency department population. Acad Emerg Med. 1997;4(4):277–281. doi: 10.1111/j.1553-2712.1997.tb03548.x. [DOI] [PubMed] [Google Scholar]
- Wong SS, Leung GK. Injury severity score (ISS) vs. ICD-derived injury severity score (ICISS) in a patient population treated in a designated Hong Kong trauma centre. Mcgill J Med. 2008;11(1):9–13. [PMC free article] [PubMed] [Google Scholar]
- Washington State Department of Health . Washington state trauma registry inclusion criteria. Washington State Department of Health; 2002. http://www.doh.wa.gov/hsqa/emstrauma/download/inclusion_criteria.pdf. [Google Scholar]