Abstract
Late-acquired incomplete stent apposition (ISA) is frequently observed after drug-eluting stent (DES) implantation. Most incidences of late-acquired ISA induced by positive vascular remodeling were of the focal type and occurred in a single vessel. We present an unusual case of a 45-year-old male subject diagnosed with late-acquired ISA that occurred in multiple vessels.
Keywords: Drug-eluting stent; Ultrasonography, interventional
Introduction
Several reports have been published on late-acquired incomplete stent apposition (ISA) after drug-eluting stent (DES) implantation, particularly sirolimus-eluting stent (SES).1) Most incidences of late-acquired ISA induced by positive vascular remodeling were of the focal type and occurred in a single vessel. However, multivessel ISA with extensive forms have not been reported as yet.
In the present case study, extensive late-acquired ISA occurred throughout two vessels, namely the left anterior descending artery (LAD) and the right coronary artery (RCA).
Case
A 45-year-old male patient was admitted with effortinduced chest pain for a month. He presented no cardiovascular risk factors except for dyslipidemia. The electrocardiogram was sinus bradycardia without any ischemic changes such as changes in ST-T. Furthermore, the echocardiogram showed no regional wall motion abnormality with normal ejection fraction. However there was significant ST segment depression at Bruce protocol stage 1 during the treadmill test. A multidetector computed tomogram revealed total occlusion with positive vascular remodeling at proximal LAD and middle RCA.
Diagnostic coronary angiography (CAG) was performed. The CAG revealed a total occlusion in distal RCA and significant stenosis in mid RCA and proximal to mid LAD (Fig. 1). The patient underwent percutaneous coronary intervention (PCI) at the mid to distal RCA with a 3.0 by 33 mm Cypher (Cordis, Miami Lakes, FL, USA) with 20 atmospheres {minimal lumen diameter (MLD) 2.72 mm}.
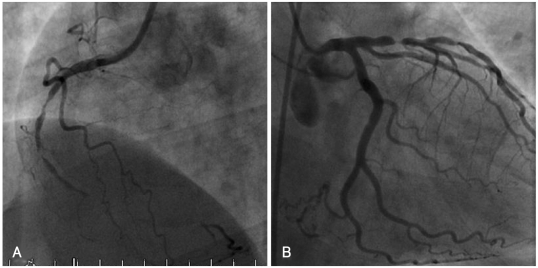
Fig. 1.
Coronary angiography at pre-intervention. A: right coronary artery. B: left coronary artery.
To revascularize the LAD lesion, DESs were successfully implanted with a 3.5 by 23 mm Cypher and 3.0 by 23 mm Cypher with 20 atmospheres covering proximal to mid LAD with overlapping technique (MLD 2.93 mm). Intravascular ultrasound (IVUS, Atlantis Plus 40 MHz; Boston Scientific, Natick, MA, USA) was then performed with a pullback speed of 0.5 mm/sec from distal to middle RCA and from middle to proximal LAD. Nine months later, a scheduled follow-up CAG was performed (Figs. 2 and 3).
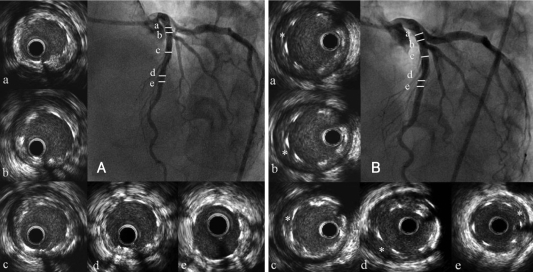
Fig. 2.
Intravascular ultrasound (IVUS) images of sirolimus-eluting stents in left anterior descending artery (LAD). A: post-stenting IVUS. The stent struts were well apposed to the vessel wall at the time of implantation. B: nine month follow-up IVUS. Incomplete stent apposition was found diffusely from proximal to distal LAD (a-e) at the follow-up. *incomplete stent apposition.
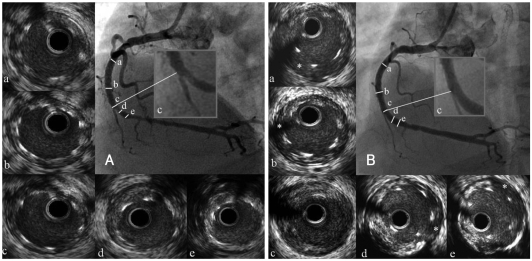
Fig. 3.
Intravascular ultrasound (IVUS) images of sirolimus-eluting stent in right coronary artery (RCA). A: post-stenting IVUS. The stent struts were well apposed to the vessel wall at the time of implantation. B: nine month follow-up IVUS. Incomplete stent apposition was found diffusely from proximal to distal RCA (a-e) with stent fracture (c) at the follow-up. *incomplete stent apposition.
A subsequent IVUS showed that there was remarkable separation between the stent struts and the vessel wall indicating the extensive development of the lateacquired ISA in the stented segments of both LAD and RCA. The maximum and mean depth of ISA in LAD was 0.89 mm and 0.5 mm respectively, while that of ISA in RCA was 1.09 mm and 0.63 mm respectively. The length of ISA in LAD and RCA was 34.2 mm and 26.2 mm respectively. Furthermore, focal stent fracture also existed within the stent body in RCA. The stent strut-free length was 1.42 mm. The patient received 100 mg of aspirin as well as 75 mg of clopidogrel as part of the antiplatelet therapy. There was no evidence of any major adverse cardiac events during a 25-month followup period, post detection of late-acquired ISA.
Discussion
ISA is the IVUS finding of lack of contact between stent struts, not overlying a side branch, and the underlying arterial wall. Late ISA may be due to either persistence of acute ISA occurring at the time of stent implantation or late-acquired ISA only being detected during a follow-up analysis.2)
Many cases have previously reported the incidence of late-acquired ISA after DES implantation.2-4) Such phenomena were more frequently observed after SES implantation.5) The present case study was also about the stent fracture and late-acquired ISA after SES implantation. However, this was a rare occurrence of extensive late-acquired ISA in multiple vessels with the evidence of stent fracture.
Several mechanisms of late-acquired ISA have been postulated, including: 1) positive vascular remodeling with or without an increase in plaque area, 2) plaque or thrombus dissolution primarily in patients presenting acute coronary syndromes, 3) chronic stent recoil, 4) decrease in plaque, and 5) ISA not being recognized at implantation and only being detected during followup analyses.2),3),6)
Hong et al.7) reported that the incidence of late-acquired ISA after DES implantation during a 6-month follow-up analysis was 12.1% and the average length of ISA was 3.9±1.4 mm. In their study, the majority of late-acquired ISA cases were focally distributed. Unlike the ISA pattern frequently observed, our case showed late-acquired ISA occurring throughout all treated segments, which conformed to the so-called "extensive ISA" pattern in both LAD and RCA. In the IVUS analysis of LAD, the mean external elastic membrane (EEM) volume was 13.9 mm3/mm at post stenting and 16.6 mm3/mm at follow-up. In RCA, the mean EEM volume was 12.9 mm3/mm at post stenting and 16.0 mm3/mm at follow-up. There was a significant interval change in the mean EEM volume but not in the mean stent volume in LAD (7.5 mm3/mm at post stenting vs. 8.0 mm3/mm at follow-up) and RCA (7.0 mm3/mm at post stenting vs. 6.8 mm3/mm at follow-up). As compared to the poststenting, the mean EEM volume at follow-up was increased in both LAD and RCA (19% and 24%, respectively). This suggested that positive vessel remodeling along with all treated segments was the main mechanism of our late-acquired ISA case. However, this is not a common phenomenon. The main cause of our extensive ISA remains unclear, but we postulate that hypersensitivity against the drug or polymer may contribute to this phenomenon.
Additional IVUS finding of the present case was that stent fracture occurred in mid to distal RCA segment, which had high angulations.8-11) We were unable to convincingly determine whether the stent fracture was associated with ISA or not. However, there was no difference in the lumen area between segments of ISA and stent fracture. We can assume that fracture occurred after the whole drug had been released since there was no in-stent restenosis found in fractured segments, and the lumen area in fractured segments was almost same with the overall lumen area.
Till now, the manifest guideline of antiplatelet therapy for ISA is still controversial. However, according to recent findings, this therapy may exert potential benefits if it is continued for longer than one year in patients with DES.12) Thus, we assume that dual antiplatelet therapy over a one-year duration should be considered in the case of ISA.
The present case study calls for more attention to late-acquired ISA after DES implantation. As DES is frequently used for coronary heart disease, more careful long-term follow-up studies are required to assess the significance of late-acquired ISA and to establish reasonable therapeutic guidelines that may include antiplatelet therapy.
References
- 1.Degertekin M, Serruys PW, Tanabe K, et al. Long-term follow-up of incomplete stent apposition in patients who received sirolimus-eluting stent for de novo coronary lesions: an intravascular ultrasound analysis. Circulation. 2003;108:2747–2750. doi: 10.1161/01.CIR.0000103666.25660.77. [DOI] [PubMed] [Google Scholar]
- 2.Colombo A, Latib A. Late incomplete stent apposition after drugeluting stent implantation: a true risk factor or "an innocent bystander"? Heart. 2008;94:253–254. doi: 10.1136/hrt.2007.126375. [DOI] [PubMed] [Google Scholar]
- 3.Mintz GS. What to do about late incomplete stent apposition? Circulation. 2007;115:2379–2381. doi: 10.1161/CIRCULATIONAHA.107.697136. [DOI] [PubMed] [Google Scholar]
- 4.Zhang RY, DU R, Zhu ZB, et al. Acute coronary syndrome is an independent risk factor for late incomplete stent apposition after sirolimus-eluting stent implantation. Chin Med J. 2008;121:2504–2508. [PubMed] [Google Scholar]
- 5.Hoffmann R, Morice MC, Moses JW, et al. Impact of late incomplete stent apposition after sirolimus-eluting stent implantation on 4-year clinical events: intravascular ultrasound analysis from the multicentre, randomised, RAVEL, E-SIRIUS and SIRIUS trials. Heart. 2008;94:322–328. doi: 10.1136/hrt.2007.120154. [DOI] [PubMed] [Google Scholar]
- 6.Mintz GS, Shah VM, Weissman NJ. Regional remodeling as the cause of late stent malapposition. Circulation. 2003;107:2660–2663. doi: 10.1161/01.CIR.0000074778.46065.24. [DOI] [PubMed] [Google Scholar]
- 7.Hong MK, Mintz GS, Lee CW, et al. Late stent malapposition after drug-eluting stent implantation: an intravascular ultrasound analysis with long-term follow-up. Circulation. 2006;113:414–419. doi: 10.1161/CIRCULATIONAHA.105.563403. [DOI] [PubMed] [Google Scholar]
- 8.Shaikh F, Maddikunta R, Djelmami-Hani M, Solis J, Allaqaaband S, Bajwa T. Stent fracture, an incidental finding or a significant marker of clinical in-stent restenosis? Catheter Cardiovasc Interv. 2008;71:614–618. doi: 10.1002/ccd.21371. [DOI] [PubMed] [Google Scholar]
- 9.Aoki J, Nakazawa G, Tanabe K, et al. Incidence and clinical impact of coronary stent fracture after sirolimus-eluting stent implantation. Catheter Cardiovasc Interv. 2007;69:380–386. doi: 10.1002/ccd.20950. [DOI] [PubMed] [Google Scholar]
- 10.Okumura M, Ozaki Y, Ishii J, et al. Restenosis and stent fracture following sirolimus-eluting stent (SES) implantation. Circ J. 2007;71:1669–1677. doi: 10.1253/circj.71.1669. [DOI] [PubMed] [Google Scholar]
- 11.Kim JS, Yoon YW, Hong BK, et al. Delayed stent fracture after successful sirolimus-eluting stent (Cypher®) implantation. Korean Circ J. 2006;36:443–449. [Google Scholar]
- 12.Bhatt DL. Role of antiplatelet therapy across the spectrum of patients with coronary artery disease. Am J Cardiol. 2009;103(3 Suppl):11A–19A. doi: 10.1016/j.amjcard.2008.11.018. [DOI] [PubMed] [Google Scholar]