Abstract
We evaluated methods for assessing body temperature by comparing subjective assessment of fever by parents and doctors with objective axillary, tympanic, and rectal measurements of body temperature in 1000 children ≤ 10-years-old who presented at outpatient clinics with recent history of fever. Sensitivity of subjective assessment of fever were higher at thresholds of ≥ 38.3°C with specificity as low as 60%. Axillary methods showed better specificity at fever thresholds of > 38.0°C with maximum sensitivity of 63% at thresholds of ≥ 37.5°C. Bland-Altman analysis showed wide limits of agreement between objective methods of measurements: −1°C to 3°C for comparison of rectal and axillary, −1°C to 2°C for rectal and tympanic, and −1°C to 2°C for tympanic and axillary measurements. A choice of method to measure body temperature for diagnosis of fever in African children should be informed by a trade off between its specificity and sensitivity that considers thresholds > 38.0°C.
Introduction
The core temperature of the human body lies between 36.4 and 37.4°C, depending on the time and measurement.1,2 A universally accepted definition for fever is still elusive,3,4 and there are problems in measuring “true” body temperature in clinical situations, which include variations in body temperature of children with level of activity, meals, time of day, environmental conditions, even improper positioning of thermometers, and hurried measurements, amongst others.5–14 These factors are difficult and almost impossible to control or standardize, making the use of a single temperature measurement an unreliable indicator.
However, the Brighton Collaboration Fever Working Group recommends a body temperature ≥ 38°C as fever irrespective of device, anatomic site, age, or environmental conditions4 and a World Health Organization expert study group accepts fever as an axillary temperature measurement of ≥ 37.5°C.5 Apparently the choices of fever threshold in malarial trials are determined by intention to increase the sensitivity and specificity of primary study endpoints. We have evaluated by comparison subjective and objective methods of determining fever in African children.
Method
We carried out a study in Lambaréné, Gabon from March 2007 to March 2008, and we enrolled 1000 children aged 10 years and younger who presented at the outpatient department of the private hospital (HAS) and government hospital (HG), which serve Lambaréné community and its neighboring area. Every morning,15 irrespective of any other associated complaint, children presenting with complaints of fever within the past 14 days were recruited after obtaining an oral consent from their parents or guardians. Their age, sex, and brief medical history including drug intake in the preceding 6 hours were recorded. For each child, an investigator (SO or KP) asked parents/guardians if the child had a “fever” presently, noting their impression or the part(s) of the child's body palpated. The investigators also subjectively determined if the child had a “fever”. Parents were asked if they objectively measured the body temperature of their children at home because health care practice in this community encourage mothers to objectively measure body temperature whenever they felt their children had a fever. They were then asked to go ahead and measure the body temperature of their children in their usual or preferred manner. The parents read the mercury thermometers immediately after measuring and the doctors (SO or KP) verified their readings. Thereafter, the doctors measured the body temperature of eligible children in the following order: tympanic temperature with infrared tympanic thermometers (ThermoScan: BRAUN type: 6022, Kronberg, Germany) and axillary and rectal temperature with electronic thermometers (Thermoval Basic: Paul Hartmann AG, 89522, Heidenheim, Germany). SO and KP assessed equal number of children during this study, the above sequence of objective measurements was followed for every eligible child aged 6 years or younger and completed within 5 minutes. Children older than 6 years of age did not have a rectal temperature taken by the investigators. Microscopic parasitemia was the only parameter for diagnosis of malaria in this study, therefore 10 µL of capillary blood was taken to quantify malaria parasite.16 Ethical clearance for this study was obtained from the local ethics committee (Comité d’Ethique Regional Independent de Lambaréné).
Data was analyzed with Stata 10 for Mac OS X (Stata Corp., College Station, TX) using Spearman correlation and Bland-Altman bias methods.17 Sensitivity, specificity and predictive values were performed with rectal temperature as “gold standard”.
Results
We observed 1000 children with median age of 3 years; 51% of them were enrolled at HG and 49% at HAS. Twenty-one children (2.1%) had taken paracetamol within the 6 hours before enrollment and three children had taken amodiaquine plus artesunate combination. Malaria parasites were found in blood slides of 73 children. At presentation, parents of 70% (700 of 1000) of the children enrolled indicated that their children had fever by palpating the head or face and others by body contact, breathing pattern, rate of activity, oral warmth during breast-feeding, or unspecified subjective impressions. Doctors said 60% (596 of 1000) of these children had a fever by palpating their head and/or their face. The sensitivity of subjective assessment of fever by parents and doctors were above 95% at a tympanic and axillary fever threshold above 38.3°C or at a rectal fever threshold above 38.7°C. The specificity of subjective assessment of fever by parents and doctors were lower than 60% and 80%, respectively.
Eighty-six percent (862 of 1000) of the parents said they objectively measured body temperature in their children when they felt their children had fever, and when asked to measure the body temperature of their children at enrollment, majority used a mercury thermometer, of which 81% (611 of 753) measured per rectum, 19% (141 of 753) in the axilla, and one child's temperature was measured orally. Only a tenth (109 of 1000) used digital thermometers (not considered in our analysis). We observed that 43% of parents participating from HG and 45% from HAS did not read the mercury thermometer correctly, plus there was another 12% in each group that could not read the mercury thermometer.
Mean ± SD of body temperatures of children aged 0–10 years was 37.9 ± 1°C with tympanic thermometers, 37.5 ± 1°C with axillary thermometers, and children 0–6 years was 38.1 ± 1°C with electronic rectal thermometer. The proportions of children with fever at various body temperature thresholds by method of measurement are shown on Table 1. Sensitivity, specificity, and predictive values of axillary and tympanic measurements of body temperature compared with electronic rectal measurements are shown on Table 2.
Table 1.
Proportions of children with objectively measured “fever” at various temperature thresholds
| Thermometry | Doctors | Parents | |||
|---|---|---|---|---|---|
| Tympanic | Axillary | Rectal | Axillary | Rectal | |
| Number of children | 1000 | 1000 | 835 | 141 | 611 |
| Temperature thresholds (°C) | n (%) | n (%) | n (%) | n (%) | n (%) |
| 37.5 | 615 (62) | 462 (47) | 594 (71) | 99 (70) | 434 (71) |
| 38.0 | 428 (42) | 315 (32) | 449 (54) | 75 (53) | 348 (57) |
| 38.3 | 348 (35) | 233 (24) | 338 (41) | 72 (51) | 238 (39) |
| 38.7 | 245 (25) | 139 (14) | 254 (30) | 56 (40) | 189 (31) |
Table 2.
Sensitivity, specificity, and predictive values of axillary and tympanic temperatures measured by doctors compared with “gold standard” electronic rectal temperatures measured by same doctors
| Site | Number of children | Temperature threshold °C | Sensitivity % | Specificity % | PPV* % | NPV† % |
|---|---|---|---|---|---|---|
| Axillary | 835 | ≥ 37.5 | 63 | 96 | 97 | 51 |
| ≥ 38.0 | 56 | 99 | 98 | 66 | ||
| ≥ 38.3 | 52 | 98 | 94 | 75 | ||
| ≥ 38.7 | 41 | 98 | 90 | 79 | ||
| Tympanic | 835 | ≥ 37.5 | 81 | 86 | 94 | 65 |
| ≥ 38.0 | 75 | 95 | 94 | 76 | ||
| ≥ 38.3 | 75 | 93 | 87 | 84 | ||
| ≥ 38.7 | 68 | 95 | 86 | 87 |
Positive predictive value.
Negative predictive value.
We found no correlation between age of children and objective measurements of fever using any of the three methods. Linear correlations of paired measurements were excellent, with Spearman rank correlation coefficients of 0.85 for the paired readings of tympanic and axillary temperatures, 0.83 for tympanic and rectal, 0.81 for axillary and rectal, and 0.81 for parents’ mercury and doctors’ electronic rectal thermometers (P < 0.001 for all pairs). Bland-Altman analysis showed that electronic rectal measurements were systematically higher than tympanic measurements, which were in turn higher than electronic axillary measurements. The mean differences were 0.9°C (95% confidence interval [CI] 0.7–0.9) with limits of agreement (LOA) of −1°C to 3°C for the comparison of rectal and axillary, 0.3°C (95% CI 0.2, 0.3) with LOA of −1°C to 2°C for rectal and tympanic, and 0.6°C (95% CI 0.5, 0.6) with LOA of −1°C to 2°C for tympanic and axillary measurements (Figure 1). Additionally the prevalence of malaria parasitemia at axillary temperature thresholds of ≥ 37.5°C, 38.0°C, 38.3°C, and 38.7°C were 3.4%, 2.9%, 2.6%, and 2.1%, respectively. Although we observed an association between presence of malaria parasites in blood smears and axillary measured temperature at thresholds of 38.3°C (odds ratio [OR] = 1.8, 95% CI 1.1–2.8, P = 0.02) and 38.7°C (OR = 2.4, 95% CI 1.5–3.9, P < 0.001), half of the children with more than 5000 parasite per microliter had an axillary temperature less than 37.5°C.18,19
Figure 1.
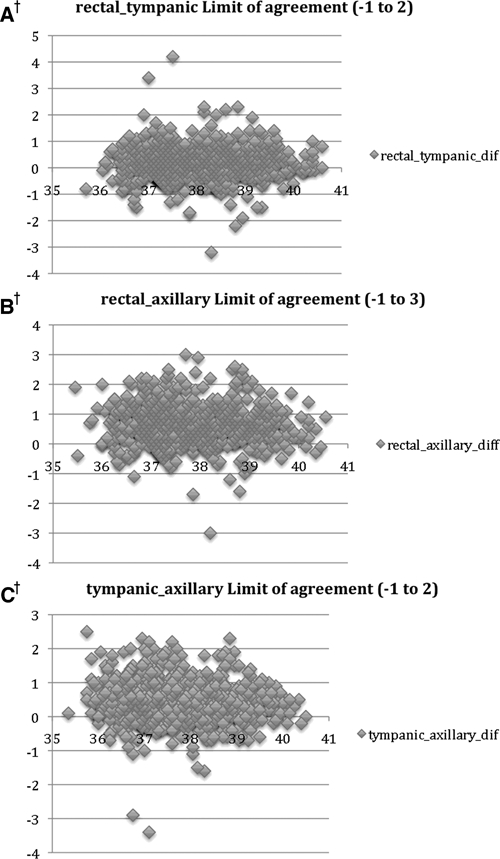
Bland-Altman plots of pairwise comparisons between different temperature measurement methods showing differences in means and upper and lower 95% limits of agreement. A, agreement of rectal with the tympanic thermometer; B, agreement of the rectal with the axillary thermometer; C, agreement of the tympanic and the axillary. † The difference between paired temperature measurements on y-axis and the mean of corresponding temperature on x-axis.
Discussion
Results of this study showed wide limits of agreement between body temperatures measured by axillary, tympanic, or rectal route. Limits of agreement correspond to 95% confidence intervals of the difference between two measurements. The range of these limits was as large as 4°C between rectal and axillary measurement, which implies that fever threshold should be considered specific for the site of measurement used.
During the course of this study we came across some practical limitations, most of which had previously been reported,20–27 including the inherent limitations and variations in individual thermometry that are difficult to reconcile, particularly individual techniques of measurement coupled with the environmental influence on body temperature. Moreover, it was cumbersome maintaining a thermometer appropriately in the axilla of very young children, who were also startled with infrared tympanic probes,28 and older children resented the rectal method.
However, the findings in this study underpin the fact that there are significant inaccuracies in subjective assessment of body temperature,24,28,29 and using either axillary or tympanic or rectal methods as “benchmark” for the assessment of body temperature for fever diagnosis in all circumstances is misleading.30–36
We conclude that when fever is of primary concern especially in large interventional trials, a standard objective measurement of body temperature is required for the diagnosis of fever taking into account possible physiological variations. The choice of method should be informed by a trade off between its specificity and sensitivity that considers thresholds higher than 38.0°C.
Footnotes
Authors’ addresses: Sunny Oyakhirome and Katharina Profanter, Medical Research Unit, Albert Schweitzer Hospital, Lambaréné, Gabon, E-mails: drsunnysmcn@hotmail.com and katharinaprofanter@yahoo.de. Peter G. Kremsner, Department of Parasitology, Institute of Tropical Medicine, University of Tubingen, Tubingen, Germany, E-mail: peter.kremsner@uni-tuebingen.de.
References
- 1.Mackowiak PA, Wasserman SS, Levine MM. A critical appraisal of 98.6 degrees F, the upper limit of the normal body temperature, and other legacies of Carl Reinhold August Wunderlich. JAMA. 1992;268:1578–1580. [PubMed] [Google Scholar]
- 2.Fischler MP, Reinhart WH. Fever: friend or enemy? Schweiz Med Wochenschr. 1997;127:864–870. [PubMed] [Google Scholar]
- 3.Baraff LJ, Bass JW, Fleisher GR. Practice guideline for the management of infants and children 0 to 36 months of age with fever without source. Pediatrics. 1993;92:1–12. doi: 10.1016/s0196-0644(05)80991-6. [DOI] [PubMed] [Google Scholar]
- 4.Marcy SM, Kohl KS, Daganc R, Nalin D, Blume M, Jones MC, Hansen J, Labadie J, Lee L, Martin BL, O’Brien K, Rothstein E, Vermeerm P, The Brighton Collaboration Fever Working Group Fever as an adverse event following immunization: case definition and guidelines of data collection, analysis, and presentation. Vaccine. 2004;22:551–556. doi: 10.1016/j.vaccine.2003.09.007. [DOI] [PubMed] [Google Scholar]
- 5.Moorthy V, Reed Z, Smith PG. Measurement of malaria vaccine efficacy in phase III trials: report of a WHO consultation. Vaccine. 2007;25:5115–5123. doi: 10.1016/j.vaccine.2007.01.085. [DOI] [PubMed] [Google Scholar]
- 6.Wailoo MP, Petersen SA, Whittaker H, Goodenough P. Sleeping body temperatures in 3–4 month old infants. Arch Dis Child. 1989;64:596–599. doi: 10.1136/adc.64.4.596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Anderson ES, Petersen SA, Wailoo MP. Factors influencing the body temperature of 3–4 month old infants at home during the day. Arch Dis Child. 1990;65:1308–1310. doi: 10.1136/adc.65.12.1308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rabinowitz RP, Cookson ST, Wasserman SS, Mackowiak PA. Effects of anatomic site, oral stimulation, and body position on estimates of body temperature. Arch Intern Med. 1996;156:777–780. [PubMed] [Google Scholar]
- 9.Anagnostakis D, Matsaniotis N, Grafakos S, Sarafidou E. Rectal-axillary temperature difference in febrile and afebrile infants and children. Clin Pediatr. 1993;32:268–272. doi: 10.1177/000992289303200503. [DOI] [PubMed] [Google Scholar]
- 10.Terndrup TE, Allegra JR, Kealy JA. A comparison of oral, rectal, and tympanic membrane-derived temperature changes after ingestion of liquids and smoking. Am J Emerg Med. 1989;7:150–154. doi: 10.1016/0735-6757(89)90127-7. [DOI] [PubMed] [Google Scholar]
- 11.Cone TE., Jr Diagnosis and treatment: children with fevers. Pediatrics. 1989;43:290–293. [PubMed] [Google Scholar]
- 12.Herzog LW, Coyne LJ. What is fever? Normal temperature in infants less than 3 months old. Clin Pediatr. 1993;32:1452–1456. doi: 10.1177/000992289303200303. [DOI] [PubMed] [Google Scholar]
- 13.Sequin J, Terry K. Neonatal infrared axillary thermometry. Clin Pediatr. 1999;38:35–40. doi: 10.1177/000992289903800105. [DOI] [PubMed] [Google Scholar]
- 14.Zehner JW, Terndrup TE. The impact of moderate ambient temperature variance on the relationship between oral, rectal, and tympanic membrane temperatures. Clin Pediatr. 1991;30:61–64. doi: 10.1177/0009922891030004S19. [DOI] [PubMed] [Google Scholar]
- 15.Schellenberg JR, Greenwood BM, Gomez P, Menendez C, Alonso PL. Diurnal variation in body temperature of Gambian children. Trans R Soc Trop Med Hyg. 1994;88:429–431. doi: 10.1016/0035-9203(94)90416-2. [DOI] [PubMed] [Google Scholar]
- 16.Planche T, Krishna S, Kombila M, Engel K, Faucher JF, Ngou-Milama E, Kremsner PG. Comparison of methods for the rapid laboratory assessment of children with malaria. Am J Trop Med Hyg. 2001;65:599–602. doi: 10.4269/ajtmh.2001.65.599. [DOI] [PubMed] [Google Scholar]
- 17.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. [PubMed] [Google Scholar]
- 18.Lell B, Brandts CH, Graninger W, Kremsner PG. The circadian rhythm of body temperature is preserved during malarial fever. Wien Klin Wochenschr. 2000;112:1014–1015. [PubMed] [Google Scholar]
- 19.Sowunmi A. Body temperature and malaria parasitaemia in rural African children. East Afr Med J. 1995;72:427–430. [PubMed] [Google Scholar]
- 20.Blainey CG. Site selection in taking body temperature. Am J Nurs. 1974;74:1859–1861. [PubMed] [Google Scholar]
- 21.Kenney RD, Fortenberry JD, Surratt SS, Ribbeck BM, Thomas WJ. Evaluation of an infrared tympanic membrane thermometer in pediatric patients. Pediatrics. 1990;85:854–858. [PubMed] [Google Scholar]
- 22.Romano MJ, Fortenberry JD, Autrey E, Harris S, Heyroth T, Parmeter P, Stein F. Infrared tympanic thermometry in the pediatric intensive care unit. Crit Care Med. 1993;21:1181–1185. doi: 10.1097/00003246-199308000-00018. [DOI] [PubMed] [Google Scholar]
- 23.Erickson RS, Woo TM. Accuracy of infrared thermometry and traditional temperature methods in young children. Heart Lung. 1994;23:181–195. [PubMed] [Google Scholar]
- 24.Chamberlain JM, Terndrup TE, Alexander DT, Silverstone FA, Wolf-Klein G, O’Donnell R, Grandner J. Determination of normal ear temperature with an infrared emission detection thermometer. Ann Emerg Med. 1995;25:15–20. doi: 10.1016/s0196-0644(95)70349-7. [DOI] [PubMed] [Google Scholar]
- 25.Craig J, Lancaster G, Taylor S, Williamson P, Smyth R. Infrared ear thermometry compared with rectal thermometry in children: a systematic review. Lancet. 2002;360:603. doi: 10.1016/S0140-6736(02)09783-0. [DOI] [PubMed] [Google Scholar]
- 26.Craig JV, Lancaster GA, Williamson PR, Smyth RL. Temperature measured at the axilla compared with rectum in children and young people: systematic review. BMJ. 2000;320:1174–1178. doi: 10.1136/bmj.320.7243.1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Robinson JL, Seal RF, Spady DW, Joffres MR. Comparison of esophageal, rectal, axillary, bladder, tympanic, and pulmonary artery temperatures in children. J Pediatr. 1998;133:553–556. doi: 10.1016/s0022-3476(98)70067-8. [DOI] [PubMed] [Google Scholar]
- 28.Canadian Task Force on Preventive Health Care New grades for recommendations from the Canadian Task Force on Preventive Health Care. CMAJ. 2003;169:207–208. [PMC free article] [PubMed] [Google Scholar]
- 29.Singhi S, Sood V. Reliability of subjective assessment of fever by mothers. Indian J Pediatr. 1990;27:811–815. [PubMed] [Google Scholar]
- 30.Whybrew K, Murray M, Morley C. Diagnosing fever by touch: observational study. BMJ. 1998;317:321–322. doi: 10.1136/bmj.317.7154.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bergeson PS, Steinfeld HJ. How dependable is palpation as a screening method for fever. Can touch substitute for thermometer readings? Clin Pediatr (Phila) 1974;13:350–351. doi: 10.1177/000992287401300416. [DOI] [PubMed] [Google Scholar]
- 32.Einterz EM, Bates ME. Fever in Africa: do patients know when they are hot? Lancet. 1997;350:781. doi: 10.1016/S0140-6736(97)24037-7. [DOI] [PubMed] [Google Scholar]
- 33.Ernst TN, Philip M. Temperature assessment by parental palpation. Am J Dis Child. 1985;139:546. doi: 10.1001/archpedi.1985.02140080016015. [DOI] [PubMed] [Google Scholar]
- 34.Graneto JW, Soglin DF. Maternal screening of childhood fever by palpation. Pediatr Emerg Care. 1996;12:183–184. doi: 10.1097/00006565-199606000-00009. [DOI] [PubMed] [Google Scholar]
- 35.Hooker EA, Smith SW, Miles T, King L. Subjective assessment of fever by parents: comparison with measurement by noncontact tympanic thermometer and calibrated rectal glass mercury thermometer. Ann Emerg Med. 1996;28:313–317. doi: 10.1016/s0196-0644(96)70031-8. [DOI] [PubMed] [Google Scholar]
- 36.Jaffe DM. what's hot and what's not: the gold standard for thermometry in emergency medicine. Ann Emerg Med. 1995;25:97–99. [PubMed] [Google Scholar]


