Abstract
Coues rice rat (Oryzomys couesi), a species abundant throughout Central America, was evaluated experimentally for the ability to serve as an amplifying host for three arboviruses: Patois (Bunyaviridae, Orthobunyavirus), Nepuyo (Orthobunyavirus), and Venezuelan equine encephalitis virus subtype ID (Togaviridae, Alphavirus). These three viruses have similar ecologies and are known to co-circulate in nature. Animals from all three cohorts survived infection and developed viremia with no apparent signs of illness and long-lasting antibodies. Thus, O. couesi may play a role in the general maintenance of these viruses in nature.
During field studies in 2007, two orthobunyaviruses, Patois (PATV) and Nepuyo (NEPV), were isolated from mosquitoes collected in coastal Chiapas, Mexico, an area endemic for Venezuelan equine encephalitis virus subtype IE (VEEV-IE).1 These two orthobunyaviruses are known to cause fatal disease in sentinel hamsters, and NEPV is associated with non-specific febrile illness in humans.2,3 Little experimental work has been conducted with these orthobunyaviruses. However, because of their shared ecology with VEEV, we evaluated their ability to use one of the most abundant, sympatric rodents as an amplification or reservoir host.
Patois virus is the type member of the Patois group in the family Bunyaviridae and the genus Orthobunyavirus. Originally isolated in 1961 from the blood of a wild cotton rat (Sigmodon hispidus) in Panama, it has since been found in Mexico, Belize, and Guatemala.4,5 It has also been isolated from sentinel mice and hamsters and from wild rodents and several species of Culex (Melanoconion) and Culex (Culex) mosquitoes.5,6 In experimental infections, PATV kills newborn and weanling mice.7 Adult mice, guinea pigs, and rabbits survive infection and produce antibodies.7 Several instances of human seropositivty have been found. However PATV has not yet been isolated from humans and has not been associated with human disease.5
Nepuyo virus also is included in the genus Orthobunyavirus, although it is classified in the serogroup known as group C. This virus was originally isolated in 1957 in Trinidad from a pool of Culex (Aedinus) accelerans. Additional isolations have been made from multiple species of Culex mosquitoes, Artibeus bats, wild rodents, and sentinel mice and hamsters.8,9 It has been shown to cause illness and death in laboratory mice, and it has been experimentally transmitted from naturally infected Culex mosquitoes to mice (Travassos da Rosa AP, unpublished data). Nepuyo virus viremia and seropositivity were detected in a human patient on the Pacific coast of Guatemala, and it was associated with an acute illness consisting of generalized myalgia, headache, and fever.2,10
Oryzomys couesi (Coues’ rice rat) is a medium-sized rodent found abundantly throughout Central America and Mexico in wetlands, marshes, at the edges of rice and sugar cane fields, and along streams.11 Several viruses of the genus Hantavirus (Bunyaviridae), including Catacamas and Playa de Oro viruses, have been associated with O. couesi, as has VEEV.12–15 Because O. couesi is such a widespread and common species and tolerates infection by a broad range of viruses, we evaluated its potential as an amplification or reservoir host, by infecting wild-caught individuals from coastal Chiapas, Mexico with sympatric strains of PATV and NEPV.
Co-evolution between VEEV and its reservoir host is thought to select for resistance to disease caused by sympatric, enzootic VEEV.15–17 Consistent with this hypothesis, it has been shown that O. couesi from coastal Chiapas are susceptible to infection yet resistant to disease by a sympatric strain of VEEV subtype IE.15 To further confirm this resistance to disease and determine if it extends to other VEEV subtypes, we used the ID subtype of enzootic VEEV from Panama with which to infect the Mexican population of O. couesi.
Wild O. couesi were collected from coastal Chiapas, Mexico during October 2007 in an overgrown field adjacent to a stream in Mapastepec Municipality, approximately two kilometers from the Pacific coast (N15.413°, W093.070°). Animals were captured at night using live-capture Sherman traps (H.B. Sherman Traps, Tallahassee, FL). Species identification was based on morphology and later confirmed genetically using cytochrome B gene sequences.11,18 Animals were collected under permit number SGPA/DGVS/03858/07 Julio 2 de 2007 issued to J.G.E.-F. and transported to the Animal BioSafety Level 3 Facility at the University of Texas Medical Branch in Galveston, Texas and allowed one week of acclimation. Before infection, baseline sera were collected for antibody assays. All studies were done using protocols reviewed and approved by the University of Texas Medical Branch Institutional Animal Care and Use Committee.
The PATV strain MP1078 was isolated from a pool of Psorophora varipes mosquitoes, and the NEPV strain MP0758 was isolated from a pool of Cx. (Melanoconion) taeniopus mosquitoes from coastal Chiapas in 2006. The viruses were passaged twice in Vero cells and identified by complement fixation.19 The Chiapas strain MP0758, identified as Nepuyo-like, was tested with a panel of control sera and yielded complement fixation patterns consistent with a strain of NEPV previously isolated from Mexico (63U11), yet slightly different than a strain previously isolated from Brazil (BeAn10709). Nunes and others20 confirmed that serologic techniques resolve Orthobunyavirus identification and relatedness comparably to genetic techniques. The VEEV subtype ID strain 213413 was isolated from the serum of a febrile human in Panama and was passaged once in suckling mouse brain.21 This strain was chosen because it is a low-passage strain of an enzootic subtype of VEEV that is non-sympatric with the population of O. couesi used in this experiment.
Adult, wild-caught animals and juvenile animals born in captivity (four weeks of age at the time of infection) were included in this study. The PATV cohort comprised four adults and one juvenile, the NEPV cohort comprised four adults and two juveniles, and the VEEV cohort comprised five adults. Juveniles were not included in the VEEV cohort because previous work with VEEV subtype IE found no obvious age-dependent differences in the process or outcome of infection.15 Animals were inoculated subcutaneously in the right thigh with 3.7, 4.5, and 3.0 log10 plaque-forming units (PFU) of PATV, NEPV, or VEEV subtype ID, respectively. Animals were weighed daily for one week and were observed for signs of illness, such as hunching, ruffled fur or lethargy, for two weeks after inoculation.
Sera were collected daily for the first 7 days after inoculation, then on days 15, 28, and 39. Animals were first anesthetized with inhaled isoflurane. Blood was then collected from the retro-orbital sinus in heparinized capillary tubes and transferred to five volumes of phosphate-buffered saline. Blood cells were removed by centrifugation to yield an approximate 1:10 dilution of plasma, which was stored at −80°C. Viremia titers were subsequently determined by plaque assay on Vero cells with a limit of detection of 1.5 log10 PFU/mL.19 To detect PATV-, NEPV-, and VEEV-ID-specific antibodies, hemagglutination inhibition (HI) assays were performed as described.19
No animal from any infection group showed weight loss or outward signs of illness (e.g., hunching, ruffled fur, lethargy, ataxia) after inoculation, and most survived until the end of the experiment at day 39 post-inoculation. However, one animal from each group died during anesthesia on day 5 (VEEV-ID) or day 28 (PATV and NEPV) without prior weight loss or signs of illness. The dead animal in the VEEV cohort had the lowest (2.11 log10 PFU/mL) and shortest (1 day) viremia of all viremic animals in that cohort. After necropsy, organs (brain, heart, lung, liver, spleen, kidney) were tested by plaque assay for live virus and none was detected. The other two animals, one from the PATV cohort and one from the NEPV cohort, exhibited no viremia and died on day 28, suggesting a cause of death unrelated to experimental infection.
Two of the five animals inoculated with PATV had measurable viremia, with a mean (SE) peak titer of 2.41 ± 0.59 log10 PFU/mL on day one (Figure 1). Only one animal had detectable viremia on day two (2.59 log10 PFU/mL), and no animals had measurable viremia thereafter. Five of the 6 animals inoculated with NEPV had measurable viremia, with a mean (SE) peak titer of 3.88 ± 0.68 log10 PFU/mL on day 1 post-inoculation (Figure 1). Three animals had measurable viremia on day 2, with a mean (SE) of 3.44 ± 0.94 log10 PFU/mL, and only one animal had measurable viremia on day 3 (1.82 log10 PFU/mL). None of the NEPV cohort had detectable viremia after day 3 post-inoculation. Four of the 5 animals inoculated with VEEV-ID had measurable viremia, with a mean (SE) peak titer of 2.60 ± 0.71 log10 PFU/mL on day 1 (Figure 1). Three animals had measurable viremia on day 2 post-inoculation with a mean (SE) of 2.54 ± 0.76 log10 PFU/mL, and only one animal remained viremic on day 3, with viremia measuring 2.90 log10 PFU/mL. None of the VEEV-ID cohort had measurable viremia after day three. The only animal from this cohort that did not become detectably viremic was the only one with pre-existing antibodies against VEEV. In neutralization tests, serum from this animal exhibited a four-fold higher titer against VEEV-IE than against VEEV-ID, indicating natural exposure to VEEV-IE.
Figure 1.
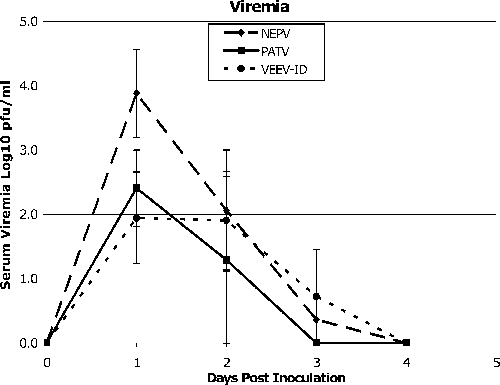
Viremia profiles for Oryzomys couesi inoculated with arboviruses from Mexico. NEPV = Nepuyo virus (n = 6); PATV = Patois virus (n = 5); VEEV-ID = Venezuelan equine encephalitis virus type ID (n = 5). Bars indicate standard errors.
Three of the 4 adult animals in the PATV cohort developed detectable PATV-specific HI antibodies within the first two weeks, with a geometric mean (SE) day 15 titer of 1:32 ± 13 (Figure 2). By day 28, one of these three animals had died and the remaining two had a two-fold decrease in antibody titer with a geometric mean (SE) titer of 1:15 ± 7. Three of the four adults and both of the juveniles in the NEPV cohort developed NEPV-specific HI antibodies within the first two weeks, with a geometric mean (SE) day 15 titer of 1:88 ± 20 (Figure 2). Antibodies in all five animals persisted through the end of the experiment, with a mean (SE) day 39 titer of 1:704 ± 250. As described above, one animal from the VEEV cohort had pre-existing antibodies against VEEV. One additional animal died on day 5 during anesthesia and handling. The remaining three animals in the cohort all developed antibodies with a mean (SE) day 7 titer of 1:133 ± 12 and a mean (SE) day 15 titer of 1:133 ± 40 (Figure 2). No sera from this cohort were collected beyond day 15. However, previous experiments with O. couesi and VEEV-IE indicate that peak HI titers are reached by day 15 and do not significantly change over the next two months.15
Figure 2.
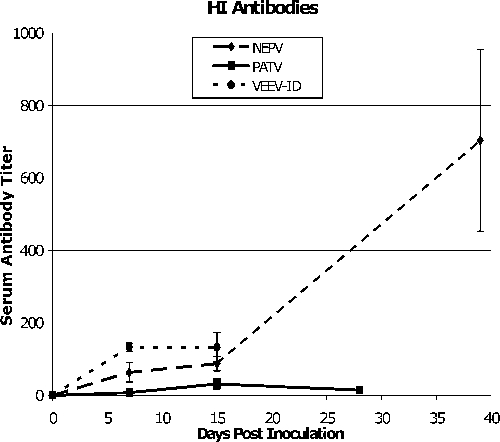
Hemagglutination inhibition (HI) antibody profiles for Oryzomys couesi animals inoculated with arboviruses from Mexico. Titers are geometric mean reciprocal of the highest serum dilution with a positive HI result. NEPV = Nepuyo virus (n = 6); PATV = Patois virus (n = 5); VEEV-ID = Venezuelan equine encephalitis virus type ID (n = 5). Bars indicate standard errors.
No indication of age dependence with respect to externally visible disease manifestation or survival was observed in any of the cohorts. The one juvenile and two of the four adults inoculated with PATV showed no viremia. The two juveniles inoculated with NEPV showed higher levels and longer viremia than the three viremic adults. The juvenile mean (SE) peak viremia titer was 5.06 ± 0.06 log10 PFU/mL with a maximum duration of three days, and the adult mean (SE) peak titer was 2.33 ± 1.00 log10 PFU/mL with a maximum duration of two days. However, no difference among age groups was seen in antibody response or survival. Previous work suggests no age-dependent effects in O. couesi animals after infection with a sympatric VEEV subtype IE strain.15
Because NEPV and PATV were found to be lethal to sentinel hamsters during field studies of VEEV in Guatemala, a bivalent vaccine was developed against these two orthobunyaviruses to facilitate VEEV isolations. However, the efficacy of such vaccination is uncertain because Scherer and others reported that a hamster that had been immunized against NEPV nonetheless yielded a field isolate.2 Thus, it is possible that the immune response to these viruses is variable between animals, which could explain the one animal in our NEPV cohort that did not seroconvert despite having a brief viremia.
Co-circulation of PATV, NEPV, and VEEV has been previously reported for foci in Central America, indicating that they may have similar ecology.2,5 Co-infection of one hamster by VEEV and PATV occurred during a field study in Guatemala,2 suggesting that these alphaviruses and bunyaviruses, although not closely related, share a similar niche. Oryzomys couesi is one of the most abundant rodents in the areas where these viruses are found. Thus, we evaluated its suitability as an amplifying and/or reservoir host. The ability of this rodent to produce viremia yet survive infection with no signs of disease suggests the evolution of resistance after co-evolution. The threshold of infection for uninfected Cx. taeniopus, a known vector of all three viruses, is approximately 2.0–2.5 log10 PFU/mL for VEEV.22 Although the threshold for NEPV and PATV is unknown, if it is similar to that of VEEV, then the viremias observed in this study would be sufficient to initiate vector infection. Further examination of transmission thresholds and mosquito and rodent co-infection experiments would complement the findings of the current study. If competition exists between viruses within the mosquito vector or the rodent amplifying host, it could affect the success of these viruses in their natural transmission cycle. This knowledge could shed new light on our understanding of arboviral dynamics in nature.
Acknowledgments
We thank Justin Darwin and Estella Abadia-Cruz for help in collecting the rodents, Nicole Arrigo and Paige Adams for help with sampling, and Judy Barnett and Don Bouyer for access assistance to BioSafety Level 3 facilities.
Footnotes
Financial support: This study was supported by contract N01-AI25489 from the National Institutes of Health (NIH) and from grants provided to Jose G. Estrada-Franco by the Interamerican Institute for Cooperation on Agriculture and the Pan American Health Organization in Washington, DC and Mexico. Eleanor R. Deardorff was supported by a James W. McLaughlin predoctoral fellowship award and by the Biodefense Training Program, NIH grant T32-AI060549.
Authors’ address: Eleanor R. Deardorff, Naomi L. Forrester, Amelia P. Travassos da Rosa, Jose G. Estrada-Franco, Roberto Navarro-Lopez, Robert B. Tesh, and Scott C. Weaver, Department of Pathology, University of Texas Medical Branch, Galveston, TX, E-mail: sweaver@utmb.edu.
References
- 1.Estrada-Franco JG, Navarro-Lopez R, Freier JE, Cordova D, Clements T, Moncayo A, Kang W, Gomez-Hernandez C, Rodriguez-Dominguez G, Ludwig GV, Weaver SC. Venezuelan equine encephalitis virus, southern Mexico. Emerg Infect Dis. 2004;10:2113–2121. doi: 10.3201/eid1012.040393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Scherer WF, Dickerman RW, Ordonez JV, Seymour C III, Kramer LD, Jahrling PB, Powers CD. Ecologic studies of Venezuelan encephalitis virus and isolations of Nepuyo and Patois viruses during 1968–1973 at a marsh habitat near the epicenter of the 1969 outbreak in Guatemala. Am J Trop Med Hyg. 1976;25:151–162. doi: 10.4269/ajtmh.1976.25.151. [DOI] [PubMed] [Google Scholar]
- 3.Scherer WF, Dickerman RW, Cupp EW, Ordonez JV. Ecologic observations of Venezuelan encephalitis virus in vertebrates and isolations of Nepuyo and Patois viruses from sentinel hamsters at Pacific and Atlantic habitats in Guatemala, 1968–1980. Am J Trop Med Hyg. 1985;34:790–798. doi: 10.4269/ajtmh.1985.34.790. [DOI] [PubMed] [Google Scholar]
- 4.Srihongse S, Galindo P, Grayson MA. Isolation of group C arboviruses in Panama including two new members, Patois and Zegla. Am J Trop Med Hyg. 1966;15:379–384. doi: 10.4269/ajtmh.1966.15.379. [DOI] [PubMed] [Google Scholar]
- 5.Scherer WF, Anderson K, Dickerman RW, Ordonez JV. Studies of Patois group arboviruses in Mexico, Guatemala, Honduras, and British Honduras. Am J Trop Med Hyg. 1972;21:194–200. doi: 10.4269/ajtmh.1972.21.194. [DOI] [PubMed] [Google Scholar]
- 6.Galindo P, Srihongse S. Transmission of arboviruses to hamsters by the bite of naturally infected Culex (Melanoconion) mosquitoes. Am J Trop Med Hyg. 1967;16:525–530. doi: 10.4269/ajtmh.1967.16.525. [DOI] [PubMed] [Google Scholar]
- 7.Zarate ML, Geiger RH, Shope RE, Scherer WF. Intergroup antigenic relationships among Arboviruses manifested by a Mexican strain of Patois virus and viruses of the Bunyamwera, C, California, Capim and Guama groups. Am J Epidemiol. 1968;88:273–286. doi: 10.1093/oxfordjournals.aje.a120886. [DOI] [PubMed] [Google Scholar]
- 8.Scherer WF, Zarate ML, Dickerman RW. Discovery and identification of group C, Nepuyo arbovirus in Mexico. Bol Oficina Sanit Panam. 1969;66:325–338. [PubMed] [Google Scholar]
- 9.Calisher CH, Chappell WA, Maness KS, Lord RD, Sudia WD. Isolations of Nepuyo virus strains from Honduras, 1967. Am J Trop Med Hyg. 1971;20:331–337. doi: 10.4269/ajtmh.1971.20.331. [DOI] [PubMed] [Google Scholar]
- 10.Scherer WF, Dickerman RW, Ordonez JV. Human disease caused by Nepuyo virus, a Central American bunyavirus transmitted by mosquitoes [in Spanish] Bol Oficina Sanit Panam. 1983;95:111–117. [PubMed] [Google Scholar]
- 11.Reid FA. A Field Guide to the Mammals of Central America and Southeast Mexico. New York: Oxford University Press; 1997. [Google Scholar]
- 12.Milazzo ML, Cajimat MN, Hanson JD, Bradley RD, Quintana M, Sherman C, Velasquez RT, Fulhorst CF. Catacamas virus, a hantaviral species naturally associated with Oryzomys couesi (Coues’ oryzomys) in Honduras. Am J Trop Med Hyg. 2006;75:1003–1010. [PMC free article] [PubMed] [Google Scholar]
- 13.Chu YK, Owen RD, Sanchez-Hernandez C, Romero-Almaraz Mde L, Jonsson CB. Genetic characterization and phylogeny of a hantavirus from western Mexico. Virus Res. 2008;131:180–188. doi: 10.1016/j.virusres.2007.09.007. [DOI] [PubMed] [Google Scholar]
- 14.Estrada-Franco JG, Navarro-Lopez R, Freier JE, Cordova D, Clements T, Moncayo A, Kang W, Gomez-Hernandez C, Rodriguez-Dominguez G, Ludwig GV, Weaver SC. Venezuelan equine encephalitis virus, southern Mexico. Emerg Infect Dis. 2004;10:2113–2121. doi: 10.3201/eid1012.040393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Deardorff ER, Forrester NL, Travassos da Rosa AP, Estrada-Franco JG, Navarro-Lopez R, Tesh RB, Weaver SC. Experimental infections of potential Mexican reservoir hosts with Venezuelan equine encephalitis virus. Emerg Infect Dis. 2009;15:519–525. doi: 10.3201/eid1504.081008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carrara AS, Coffey LL, Aguilar PV, Moncayo AC, Da Rosa AP, Nunes MR, Tesh RB, Weaver SC. Venezuelan equine encephalitis virus infection of cotton rats. Emerg Infect Dis. 2007;13:1158–1165. doi: 10.3201/eid1308.061157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Young NA, Johnson KM, Gauld LW. Viruses of the Venezuelan equine encephalomyelitis complex: experimental infection of Panamanian rodents. Am J Trop Med Hyg. 1969;18:290–296. [PubMed] [Google Scholar]
- 18.Boakye DA, Tang J, Truc P, Merriweather A, Unnasch TR. Identification of bloodmeals in haematophagous Diptera by cytochrome B heteroduplex analysis. Med Vet Entomol. 1999;13:282–287. doi: 10.1046/j.1365-2915.1999.00193.x. [DOI] [PubMed] [Google Scholar]
- 19.Beaty BJ, Calisher CH, Shope RE. In: Diagnostic Procedures for Viral, Rickettsial and Chlamydial Infections. Sixth edition. Schmidt NJ, Emmons RW, editors. Washington, DC: American Public Health Association; 1989. pp. 797–855. (Arboviruses). [Google Scholar]
- 20.Nunes MR, Travassos da Rosa AP, Weaver SC, Tesh RB, Vasconcelos PF. Molecular epidemiology of group C viruses (Bunyaviridae, Orthobunyavirus) isolated in the Americas. J Virol. 2005;79:10561–10570. doi: 10.1128/JVI.79.16.10561-10570.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Quiroz E, Aguilar PV, Cisneros J, Tesh RB, Weaver SC. Venezuelan equine encephalitis in Panama: fatal endemic disease and genetic diversity of etiologic viral strains. PLoS Negl Trop Dis. 2009;3:e472. doi: 10.1371/journal.pntd.0000472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Scherer WF, Cupp EW, Dziem GM, Breener RJ, Ordonez JV. Mesenteronal infection threshold of an epizootic strain of Venezuelan encephalitis virus in Culex (Melanoconion) taeniopus mosquitoes and its implication to the apparent disappearance of this virus strain from an enzootic habitat in Guatemala. Am J Trop Med Hyg. 1982;31:1030–1037. doi: 10.4269/ajtmh.1982.31.1030. [DOI] [PubMed] [Google Scholar]


