Abstract
Western equine encephalitis virus (WEEV) is a zoonotic alphavirus that circulates in western North America between passerine birds and mosquitoes, primarily Culex tarsalis. Since it was isolated in 1930, WEEV has caused tens of thousands of equine deaths in addition to thousands of human cases. In addition because WEEV is a virus of agricultural importance in addition to a public health threat, we developed two live-attenuated chimeric vaccine candidates that have been shown to be immunogenic and efficacious in mouse models. Vaccine candidate strains were developed by inserting the structural protein genes of WEEV strain McMillan (McM) or CO92-1356 into a Sindbis virus (SINV) strain AR339 backbone. The SIN/McM chimera also derived the N-terminal half of its capsid gene from a North American eastern equine encephalitis virus (EEEV) strain FL39-939 (henceforth referred to as SIN/EEE/McM). Although these vaccines do not generate viremia in mice, we further assessed their safety by exposing Cx. tarsalis to artificial blood meals containing high viral titers of each vaccine candidate. Both viruses exhibited a decreased rate of infection, dissemination, and transmission potential compared with the parental alphaviruses. Specifically, SIN/CO92 infected 37% of mosquitoes and disseminated in 8%, but failed to reach the saliva of the mosquitoes. In contrast, the SIN/EEE/McM virus was unable to infect, disseminate, or be transmitted in the saliva of any mosquitoes. These findings suggest that both vaccine candidates are less competent than the parental strains to be transmitted by the primary mosquito vector, Cx. tarsalis, and are unlikely to be reintroduced into a natural WEEV transmission cycle.
Introduction
Western equine encephalitis virus (WEEV: Togaviridae: Alphavirus) is a mosquito-borne pathogen that causes severe neurologic disease, which can be fatal and lead to mild to severe neurologic sequelae in survivors. Infections have an economic impact ranging from $21,000 to $3 million dollars per apparent human case.1 This virus is a New World recombinant alphavirus that is distributed throughout western North America and has also been isolated in Panama, Argentina, Brazil, and Cuba.2 Western equine encephalitis virus is a challenging public health risk because there is no licensed vaccine or treatment available for humans, the ecology of virus over-wintering remains to be elucidated, control measures are expensive, and there is little financial support for surveillance and prevention.1 Additionally, WEEV is classified as a category B select agent by the National Institute of Allergy and Infectious Disease because of its potential use as a biological weapon.3
Ecological studies of western equine encephalitis (WEE) in California indicate that in nature, WEEV primarily cycles between passerine birds such as sparrows and house finches, and the primary mosquito vector, Cx. tarsalis.4–8 A secondary cycle, which is less well understood, also exists between Aedes melanimon7,9,10 mosquitoes and hares (Lepus californicus).4,11 Vector competence studies have shown that Ae. dorsalis4,12,13 and Culiseta inornata8 are also able to transmit WEEV in North America. As the population of Cx. tarsalis females increases throughout the summer, the proportion of mosquitoes feeding on mammals increases, which leads to an increased risk of WEEV transmission to humans and domestic animals.14,15
Currently, there is no licensed WEEV vaccine for human immunization of high-risk persons (i.e., laboratory professionals, veterinarians). However, there are several commercial vaccines available for use in equids. These vaccines contain formalin-inactivated, wild-type WEEV prepared in chicken embryo fibroblast cultures and are typically delivered as a bivalent eastern equine encephalitis virus (EEEV)/WEEV formulation or even a trivalent Venezuelan equine encephalitis virus (VEEV)/EEEV/WEEV preparation.16 Effective immunization requires two initial doses followed by annual booster immunizations. Unfortunately, these kinds of inactivated vaccines are not ideal for public health after either a natural WEE outbreak or potential bioweapon exposure because of the two-dose requirement and the typically slow and short-lived immune responses that vaccinees generate.4
To develop a safer, more efficacious vaccine candidate, live-attenuated chimeric WEEV vaccine candidates have been developed.17 Alphaviruses contain a single-stranded, positive-sense RNA genome with four nonstructural proteins (NSP1–4) encoded by an open reading frame in the 5′ two-thirds of the genome, and a structural polyprotein that is translated from a subgenomic (26S) RNA and cleaved into three major structural proteins (capsid and envelope glycoproteins E2 and E1). The backbone of the first strain, SIN/CO92, consists of the 3′- and 5′-untranslated genome regions and nonstructural protein genes of Sindbis virus (SINV) strain AR339 (Figure 1A). The structural protein genes are derived from WEEV strain CO92-1356. The second strain, SIN/EEE/McM, has a similar genetic makeup with two exceptions: 1) the amino-terminal half of the capsid gene, including the 5′-untranslated region of the subgenomic RNA, is derived from EEEV strain FL93-939,18 and 2) the remainder of the structural protein genes is derived from the WEEV McMillan strain (Figure 1B). The amino-terminal half of the EEEV capsid gene was included to enhance virus packaging without the attenuating affects that would occur if a SINV or WEEV N-terminal capsid gene was present to interact with the NSP2 packaging signal.19 High replication efficiency observed previously with a SIN/EEEV chimeric virus indicated that the EEEV-specific capsid has strong RNA-binding activity during virus assembly.17,20,21 Both chimeric SIN/WEEV viruses replicated efficiently in African green monkey (Vero) cells and Ae. albopictus (C710) cells, and were highly attenuated, immunogenic, and efficacious in mouse models of WEE.17
Figure 1.
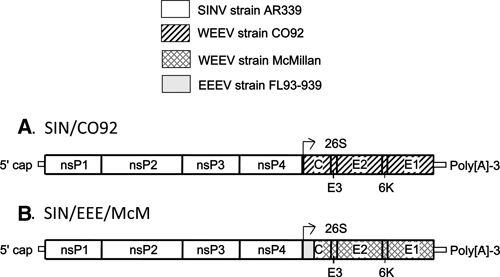
Schematic representation of SIN/CO92 and SIN/EEE/McM chimeric vaccine candidates. The SIN/CO92 chimera (A) includes the nonstructural protein gene regions of Sindbis virus (SINV) strain AR339 and the structural protein gene regions of western equine encephalitis virus (WEEV) strain CO92-1356. The SIN/EEE/McM chimera (B) includes the nonstructural protein gene regions of SINV strain AR339, the amino-terminal domain of the capsid of eastern equine encephalitis virus (EEEV) strain FL93-939, and the carboxy-terminal domain of the capsid and envelope glycoproteins of WEEV strain McMillan.
The large-scale use of live virus vaccines can include the risk of reversion to virulence and transmissibility, which could lead to outbreaks of disease as demonstrated by the live-attenuated poliovirus vaccine.22 This risk is of particular concern for genetically modified viruses that might evolve in unpredictable ways during natural circulation. For arthropod-borne viruses, transmission generally requires the generation of viremia sufficient for infection of the vector, followed by replication, dissemination, and shedding into the saliva. Although neither chimeric WEEV vaccine produces viremia in mice, it is nonetheless desirable to evaluate their ability to infect WEEV vectors as a measure of environmental safety. Any live virus vaccine, when administered on a large scale, has the potential to produce a viremia in a compromised host. However, if infection or transmission by the mosquito vector cannot occur, this risk would not extend beyond the occasional compromised vaccinee.
To evaluate the environmental safety of these chimeric WEEV vaccine candidates, we orally exposed the primary WEEV mosquito vector, Cx. tarsalis, to high-titered artificial blood meals to assess the ability of these chimeric viruses to infect, disseminate, and be transmitted to uninfected mice. Culex tarsalis was selected because it is the principal WEEV vector in North America,8 where these vaccine candidates would be used if approved for equids or humans.
Materials and Methods
Viruses.
Three wild-type alphavirus strains and two chimeric vaccine candidates were compared in this study. The wild-type strains included 1) SINV strain AR339, 2) WEEV strain CO92-1356, which was isolated in 1992 from Cx. tarsalis mosquitoes in Colorado, and 3) WEEV strain McMillan, which was isolated in 1941 from a human in Ontario, Canada. The first chimeric vaccine candidate (SIN/CO92) consisted of nonstructural protein genes derived from SINV strain AR339 and structural protein genes derived from WEEV strain CO92 (Figure 1A). The second vaccine candidate (SIN/EEE/McM) also contained SINV strain AR339 nonstructural protein genes, but derived the N-terminal half of its capsid gene from the North American EEEV strain FL93-93923 and the remainder of the capsid as well as the envelope glycoprotein genes from WEEV strain McMillan (Figure 1B). Cloning and electroporation of each chimeric virus were performed as described previously.17
Oral mosquito infections.
Culex tarsalis eggs from a colony generated at the University of California, Davis were hatched and reared using standard methods to generate a laboratory-based colony.24 Five cohorts of 50 adult females (1–3 replicates per virus) 5–6 days after emergence from the pupal state were allowed to feed for 45 minutes on an artificial blood meal containing 33% (v/v) defibrinated sheep erythrocytes (Colorado Serum Company, Denver, Co), 33% (v/v) heat-inactivated fetal bovine serum (FBS) (Omega Scientific, Inc., Tarzana, CA), 33% (v/v) of each individual virus in cell culture fluid (resulting in a final concentration of approximately 6 log10 plaque-forming units [PFU]/mL), and 1% (v/v) of 0.25 μM ATP. Artificial blood meals were encased in a collagen membrane and warmed in a Hemotek feeder (Discovery Workshops, Accrinton, United Kingdom) before being placed on the screened lids of 0.45-liter paper cartons. After feeding, mosquitoes were cold-anesthetized and engorged specimens were held at 27°C at a relative humidity of 70–75% for an extrinsic incubation period of 11–14 days.
Intrathoracic mosquito infections.
Two cohorts of 30 adult females were subjected to intrathoracic inoculation of approximately 1 μL of 6 log10 PFU/mL of SINV, SIN/EEE/McM, or wild-type WEEV strain McMillan (WEEV-McM). Mosquitoes were held for an extrinsic incubation period of 8 days at 27°C at a relative humidity of 70–75% before being presented to uninfected suckling mice for blood feeding.
Mosquito processing.
After extrinsic incubation, legs and wings were removed from cold-anesthetized mosquitoes and placed in an Eppendorf (Hamburg, Germany) tube with 350 μL of Dulbecco's modified Eagle's essential medium (DMEM) with 10% FBS, and amphotericin B (50 μg/mL). When salivation was performed, the proboscis of each immobilized mosquito was inserted into a 10-μL capillary tube containing immersion oil (Cargille Laboratories, Cedar Grove, NJ) to induce salivation for approximately 45 minutes. After salivation, mosquito bodies and legs/wings were triturated for 4 minutes in 350 μL of DMEM, 10% FBS, and amphotericin B using a Mixer Mill 300 (Retsch, Newton, PA). Collected saliva was added to an Eppendorf tube containing 100 μL of 10% FBS/DMEM and centrifuged before transfer of the supernatants. Collected supernatants from each sample were analyzed for virus content by the induction of cytopathic effects (CPE) on Vero cells.25
Transmission to mice.
Because artificial saliva collection assayed by cell culture CPE has limited sensitivity to detect transmission potential,26 we also exposed some mosquitoes to uninfected murine hosts. After completion of the extrinsic incubation period, mosquito cohorts were allowed to feed for 45 minutes on a group of five six-day-old mice placed on the screened lid of the incubation carton. For all experiments, it was noted that no mosquito engorged fully on the suckling mice, but probing was considered exposure because mosquitoes salivate while locating a blood vessel. In subsequent experiments, each individual mosquito was allowed to probe on an individual mouse to follow which mosquitoes probed on a particular mouse. Individual mosquitoes were cold-anesthetized and separated into individual wire-top tubes through which they could probe. Mice were placed adjacent to the wire top and mosquitoes were allowed to probe. As a control, an additional cohort of mice was exposed to uninfected mosquitoes. Mice were then returned to their cages and observed for survival for three weeks. Survivors were bled and analyzed for neutralizing antibodies to assess exposure to virus. Positive and negative control serum samples were included for all 80% plaque reduction neutralization tests (PRNT80).
Statistical analyses.
Initial body infection, dissemination into the hemocoel, and salivary infection as a measure of transmission potential were compared between virus groups using a 2 × 3 chi-square for independence test by using the software program InStat version 3.0 (GraphPad, San Diego, CA). Experimental replicates were combined for final analysis between groups. Results were considered significant if a P value < 0.05 was achieved.
Results
Orally exposed Cx. tarsalis infection and dissemination.
Overall, Cx. tarsalis body infection rates varied greatly among the parental virus strains (SINV, WEEV-CO92, and WEEV-McM: 92%, 73%, and 0%, respectively) (Table 1). The SIN/CO92 vaccine candidate strain showed a significantly decreased rate of body infection compared with its parents (P < 0.0025). Similarly, comparison of SINV, WEEV-CO92, and SIN/CO92 showed a significant difference in dissemination rates into the hemocoel (86%, 60%, and 8%, respectively) (P < 0.0001). The McMillan-derived vaccine candidate strain and the parental WEEV strain failed to infect or disseminate in Cx. tarsalis after oral exposure.
Table 1.
Oral mosquito infection and dissemination in Culex tarsalis*
| Virus | Blood meal titer (log10 PFU/mL) | No. engorged | No. (%) infected | ||
|---|---|---|---|---|---|
| Body | Legs/wings | Saliva | |||
| SINV | 6.9 | 22 | 22 (100) | 21 (95) | 2 (20)† |
| 7.0 | 7 | 5 (71) | 5 (71) | 0 (0) | |
| 6.2 | 7‡ | 6 (85) | 5 (71) | – | |
| Total | 36 | 33 (92) | 31/36 (86) | 2/17 (12)§ | |
| SIN/CO92 | 6.1 | 20 | 9 (45) | 2 (10) | 0 (0)¶ |
| 6.3 | 10 | 4 (40) | 1 (10) | 0 (0) | |
| 6.2 | 7‡ | 1 (14) | 0 (0) | – | |
| Total | 37 | 14 (37) | 3 (8) | 0/20 (0)# | |
| WEEV CO92 | 6.2 | 20 | 17 (85) | 14 (70) | 0 (0)** |
| 6.0 | 16 | 9 (56) | 8 (50) | 4 (25) | |
| 5.6 | 2‡ | 2 (100) | 1 (50) | – | |
| Total | 38 | 28 (73) | 23 (60) | 4/26 (15)†† | |
| SIN/EEE/McM | 6.6 | 27 | 0 (0) | 0 (0) | 0 (0) |
| WEEV McM | 5.9 | 26 | 0 (0) | 0 (0) | 0 (0) |
PFU = plaque-forming units; SINV = Sindbis virus; WEEV = western equine encephalitis virus; EEE = eastern equine encephalitis; McM = McMillan.
Ten mosquitoes were selected for salivary analysis at the time of processing, and upon analysis, it was found that all 10 had disseminated infection.
Number engorged in these groups indicates the number of orally exposed mosquitoes that were later presented to suckling mice.
Total represents the number of the sample of 17 tested for salivary infection.
Ten mosquitoes were selected for salivary analysis at the time of processing, and upon analysis, it was found that only 2 of the 10 chosen had disseminated infection.
Total represents the number of the sample of 20 tested for salivary infection.
Ten mosquitoes were selected for salivary analysis at the time of processing, and upon analysis, it was found that only 6 of the 10 chosen had disseminated infection.
Total represents the number of the sample of 26 tested for salivary infection.
Intrathoracic exposure to WEEV-McM and SIN/EEE/McM.
To determine whether McMillan-derived viruses can replicate within Cx. tarsalis mosquitoes, intrathoracic inoculations bypassing the midgut were also performed. Bodies of all surviving inoculated mosquitoes inoculated with SINV, WEEV-McM, and SIN/EEE/McM were examined for infection (Table 2). In contrast to oral exposure to WEEV-McM and SIN/EEE/McM (Table 1), the intrathoracic route infected all mosquitoes. As expected, all SINV mosquitoes were also infected.
Table 2.
Intrathoracic infection of Culex tarsalis mosquito cohorts*
| Virus | Inoculum titer (log10 PFU/mL) | No. inoculated | No. (%) infected |
|---|---|---|---|
| SINV | 7.3 | 9 | 9 (100) |
| SIN/EEE/McM | 6.7 | 10 | 10 (100) |
| WEEV McM | 6.3 | 8 | 8 (100) |
PFU = plaque-forming units; SINV = Sindbis virus; EEE = eastern equine encephalitis; McM = McMillan; WEEV = western equine encephalitis virus.
Mosquito transmission of virus after oral exposure.
SIN/CO92 and its parental virus strains were evaluated for transmission potential by examining the saliva of exposed mosquitoes using the capillary method. When the SIN/CO92 vaccine candidate strain was compared with SINV and WEEV-CO92, there were no statistically significant differences in transmission potential based on infectious saliva content. SINV, SIN/CO92, and WEEV-CO92 had 12%, 0%, and 15%, salivary infection rates, respectively. However, because of the known insensitivity of saliva assays for transmission potential,26 other cohorts of orally exposed mosquitoes were allowed to feed on groups of five uninfected six-day-old mice, which were followed-up for three weeks for survival (Figure 2) and seroconversion. The parental WEEV-CO92 produced rapid mortality in mice; all mice succumbed to infection by three days after exposure to infected mosquitoes. SINV strain AR339 was also transmitted by Cx. tarsalis to mice, resulting in 40% mortality by day six post-exposure. The mice exposed to mosquitoes that fed on the vaccine candidate SIN/CO92 showed no mortality up to three weeks after exposure to infected mosquitoes. Similarly, mice exposed to mosquitoes that fed on WEEV McM and vaccine candidate SIN/EEE/McM also showed no mortality (Figure 2). However, none of the exposed mosquitoes acquired either of these two vaccines, further supporting the results shown in Table 1.
Figure 2.
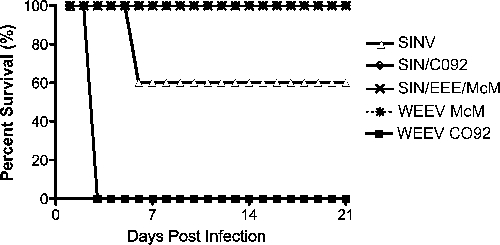
Survival of six-old mice after probing and/or blood feeding by orally exposed mosquitoes.
To determine whether mice that survived mosquito probing or feeding had been infected with either SINV or SIN/CO92, serum was collected from the mice three weeks post-mosquito exposure and assayed for neutralizing antibodies. There were no antibodies detected in the surviving mice, suggesting these mice were never exposed to virus during mosquito probing or feeding. Alternatively, it was also possible that the mosquitoes that contained infectious saliva were not the individuals that probed on the mice. Therefore, the SIN/CO92 mouse transmission experiment was repeated to expose each individual mosquito to an individual suckling mouse. In this experiment, seven SIN/CO92 orally exposed mosquitoes that survived the extrinsic incubation period were each exposed to one suckling mouse and probing was observed. Although it was noted that each of the seven mosquitoes probed, all of the suckling mice survived, and subsequent tests indicated that none of the seven mosquitoes had disseminated infections with SIN/CO92.
Mosquito transmission of virus after intrathoracic inoculation.
Mosquitoes that were intrathoracically inoculated with either SIN/EEE/McM, SINV, or McM were examined for the ability to transmit virus. Suckling mice were exposed to individual mosquitoes and probing/feeding behavior was noted. Subsequent CPE assays indicated that all mosquitoes in each virus group were infected. As observed in the previous experiments with orally exposed mosquitoes, SINV was transmitted to suckling mice. Of the nine mice presented to individual mosquitoes in the SINV group, seven (78%) were probed. Six of the seven SINV-exposed mice (86%) succumbed to disease by day five post-exposure (Figure 3), and the single surviving mouse was seropositive (antibody titer = 1:20). Of 10 SIN/EEE/McM-infected mosquitoes, nine (90%) probed on individual mice. Of these nine SIN/EEE/McM-exposed mice, six succumbed to disease (67%) by day five post-infection (Figure 3). Of the three surviving SIN/EEE/McM-exposed mice, two were seropositive (1:20 and 1:40) and one was seronegative. In the McM group, three of the seven infected mosquitoes (43%) probed on individual mice. Two of the three mice succumbed to disease (67%) by day three post-infection (Figure 3). The single surviving mouse was killed by its mother at day 10 post-infection. However, this mouse never displayed signs of disease and was seronegative.
Figure 3.
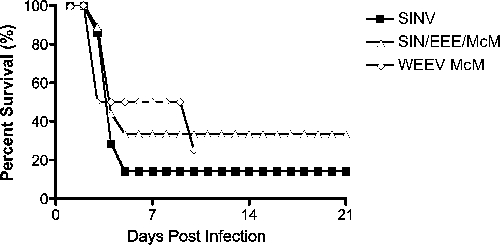
Survival of six-day-old mice after probing and/or blood feeding by intrathoracically infected mosquitoes. Transmission rates from mosquitoes to mice for Sindbis virus (SINV), SIN/EEE/McM, and western equine encephalitis virus McMillan (McM) were 77%, 89%, and 100%, respectively. EEE = eastern equine encephalitis.
Discussion
All currently available WEEV vaccines are inactivated strains that are only licensed for veterinary use (i.e., horses), are poorly immunogenic, not consistently efficacious, and require multiple doses to achieve seroconversion.4,27 Therefore, recent efforts have focused on developing live-attenuated vaccine strains that will be highly immunogenic and efficacious after a single dose. The purpose of our study was to assess whether, in the event that a human or equid became viremic after vaccination, these recently developed chimeric WEEV strains have the potential to be introduced into a mosquito-borne transmission cycle. Using the primary WEEV mosquito vector, Cx. tarsalis, we evaluated the potential for each chimeric vaccine candidate strain (SIN/CO92 and SIN/EEE/McM) to infect, disseminate, and be transmitted when compared with parental virus strains (SINV and WEEV).
We found that the parental SINV strain AR339, WEEV strain CO92, and the chimeric vaccine candidate strain SIN/CO92 were infectious for Cx. tarsalis after exposure to large oral doses. Similarly, SIN/CO92 was able to disseminate in mosquitoes, albeit at a much lower rate, when compared with the parental strains. Interestingly, Cx. tarsalis was refractory to WEEV strain McMillan and the McMillan-derived chimeric vaccine candidate strain. This finding is likely because of unaccounted mouse brain passages since its isolation in 1941. We speculate that this strain was selected for neurovirulence in rodents, and as a result, lost its ability to efficiently infect mosquitoes. Further studies should attempt to identify sequence variations in the structural protein regions of the McMillan strain that may be responsible for the loss of the Cx. tarsalis infection phenotype. These determinants could be used to reduce the ability of other SIN/WEEV strains to infect this vector.
The SIN/EEE/McM vaccine candidate exhibited the same inability to orally infect Cx. tarsalis as the parental WEEV McM strain, which is a promising safety characteristic of this vaccine candidate. Further examination indicated that WEEV strain McMillan and SIN/EEE/McM can replicate in Cx. tarsalis when the midgut is bypassed by an intrathoracic inoculation. Previous studies have shown that there is a dose-dependent midgut infection barrier within Cx. tarsalis as it relates to strains of WEEV.28 However, in our studies, oral doses as high as 6.0 log10 PFU/mL were unable to overcome this putative threshold barrier.
The enhancement of alphavirus dissemination in mosquitoes co-infected with filarial worms has been reported and could enable transmission of the chimeric vaccine candidates we studied.29 However, the Brugia spp. that are known to enhance dissemination do not circulate in the same geographic regions as WEEV and have not been found in equids.30 To our knowledge, no studies have been performed indicating WEEV viral dissemination enhancement in horses (the most likely non-human vaccine host) co-infected with filarial worms. However, this concern could be easily alleviated by a simple blood smear to determine the parasitic status of an equid before WEEV vaccination or treatment with a dewormer before vaccination. Additionally, because horses do not become viremic from wild-type WEEV,4 the risk of an equid developing viremia sufficient for transmission with an attenuated vaccine candidate strain is further decreased. Therefore, it is highly unlikely that Cx. tarsalis could acquire infection from a host vaccinated with either a McMillan- or CO92-derived vaccine candidate strain.
Next, we examined the transmissibility of each vaccine candidate when compared with parental strains by using three measures: 1) presence of virus in Cx. tarsalis saliva as measured by cell culture assay, 2) survival of neonatal mice after exposure to infected Cx. tarsalis, and 3) seroconversion of surviving mice after exposure to infected mosquitoes. Rates of salivary gland infection with certain vaccine candidates were lower than expected when compared with wild-type viruses. For example, transmission potential measured by capillary method for mosquitoes exposed to SINV showed that only 13% of mosquitoes with disseminated infection had virus in the salivary glands. However, 77% of SINV intrathoracically infected mosquitoes were able to transmit virus to uninfected mice.
Previous studies have shown that viral transmission detection from newborn mice is more sensitive than capillary saliva collection followed by cell culture-based assays, and our findings support these observations.26 The mouse assay is a true measure of transmission, but detection of virus in the salivary glands is only a predictor of transmission potential. Thus, capillary salivary assays were used minimally throughout the study. Exposure of the WEEV CO92-fed mosquito group to uninfected suckling mice resulted in rapid mortality of all mice by day three post-exposure, indicating transmission. Forty percent of mice succumbed to SINV after exposure to orally infected mosquitoes. At the time of exposure, the number of infected mosquitoes was unknown because assays were performed only after mosquitoes were killed. Therefore, we deemed it necessary to distinguish if the 60% of surviving mice had been infected by evaluating their serum for neutralizing antibodies three weeks post-exposure. The PRNT80 results indicated that none of the surviving mice in this cohort had been infected with SINV. Similarly, all surviving mice from the SIN/CO92 exposure group were seronegative. Whether this was because these mice were only exposed to uninfected mosquitoes, or whether the mosquitoes were infected but unable to transmit, was not clear. Thus, additional experiments were performed to resolve this uncertainty.
In the subsequent experiments, individual mosquitoes were allowed to feed on an individual uninfected suckling mouse to correlate mosquito infection status with mouse exposure. None of the mosquitoes in the SIN/CO92 oral exposure group acquired a disseminated infection. Although we demonstrated that SIN/CO92 is able to disseminate in Cx. tarsalis mosquitoes in previous studies, we observed these rates to be very low, even at relatively high oral doses (³ 6 log10 PFU/mL). Because of these low rates of dissemination, we were unable to generate a cohort of mosquitoes with the potential to transmit to uninfected mice.
In summary, although both vaccine WEE candidate strains do not appear to be transmitted by the primary WEEV mosquito vector, Cx. tarsalis, only the SIN/EEE/McM strain was completely unable to infect this species after oral exposure. Therefore, this vaccine candidate should be regarded as having superior environmental safety. These results corroborate previous findings that chimeric alphaviruses have reduced infectivity in mosquito vectors,31 further supporting their safety as vaccine candidates.
Acknowledgments
We thank Jing Huang for help in rearing and preparing mosquitoes for experimental infections, Bill Reisen for providing viable Cx. tarsalis eggs, and Naomi Forrester for valuable advice throughout the process.
Footnotes
Financial support: This study was supported by a grant from the National Institute of Allergy and Infectious Disease through the Western Regional Center of Excellence for Biodefense and Emerging Infectious Disease Research, National Institutes of Health (NIH) grant U54 AIO57156. Joan L. Kenney was supported by a Centers for Disease Control and Prevention fellowship for training in vector-borne infectious diseases (TO1/CCT622892) and by the NIH-sponsored Emerging Infectious Diseases Training Program (T32-AI07536). A. Paige Adams was supported by the James W. McLaughlin Fellowship Fund.
Authors’ addresses: Joan L. Kenney, A. Paige Adams, and Scott C. Weaver, Department of Pathology, University of Texas Medical Branch, Galveston, TX 77555-0428, E-mails: jlkenney@utmb.edu, apadams@utmb.edu, and sweaver@utmb.edu.
References
- 1.Centers for Disease Control and Prevention Arboviral Encephalitides. Disease DoV-BI, ed. Fact Sheet: Western Equine Encephalitis. 2005. http://www.cdc.gov/ncidod/dvbid/Arbor/weefact.htm Available at.
- 2.Weaver SC, Kang W, Shirako Y, Rumenapf T, Strauss EG, Strauss JH. Recombinational history and molecular evolution of western equine encephalomyelitis complex alphaviruses. J Virol. 1997;71:613–623. doi: 10.1128/jvi.71.1.613-623.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Institute of Allergy and Infectious Diseases . Biodefense Research Agenda for Category B and C Priority Pathogens. Bethesda, MD: NIAID Biodefense Research; 2003. [Google Scholar]
- 4.Reisen WK, Monath TP. In: Western Equine Encephalomyelitis. Monath TP, editor. Boca Raton, FL: CRC Press; 1988. pp. 89–137. (Western equine encephalomyelitis). [Google Scholar]
- 5.Chamberlain RW. Vector relationships of the arthropod-borne encephalitides in North America. Ann NY Acad Sci. 1962;76:61–81. doi: 10.1111/j.1749-6632.1958.tb35390.x. [DOI] [PubMed] [Google Scholar]
- 6.Hess A, Hayes R. Seasonal dynamics of western encephalitis virus. Am J Med Sci. 1967;253:333–348. doi: 10.1097/00000441-196703000-00011. [DOI] [PubMed] [Google Scholar]
- 7.Reeves WC, Hammon WM, Longshore WA, Jr, McClure HE, Geib AF. Epidemiology of the arthropod-borne viral encephalitides in Kern County, California, 1943–1952. Public Health Univ Calif. 1962;4:1–257. [PubMed] [Google Scholar]
- 8.Hammon WM, Reeves WC, Gray M. Mosquito vectors and inapparent animal reservoirs of St. Louis and western equine encephalitis viruses. Am J Public Health Nations Health. 1943;33:201–207. doi: 10.2105/ajph.33.3.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jensen T, Washino RK. An assessment of the biological capacity of a Sacramento Valley population of Aedes melanimon to vector arboviruses. Am J Trop Med Hyg. 1991;44:355–363. doi: 10.4269/ajtmh.1991.44.355. [DOI] [PubMed] [Google Scholar]
- 10.Hardy J, Reeves WC, Bruen JP, Presser SB. Vector competence of Culex tarsalis and other mosquito species for western equine encephalomyelitis virus. Arctic Tropical Arboviruses. 1979;10:157–171. [Google Scholar]
- 11.Hardy JL, Bruen JP. Aedes melanimon as a vector of WEE virus in California. Proceedings of the California Mosquito Control Association. 1974;42:36. [Google Scholar]
- 12.Kramer LD, Reisen WK, Chiles RE. Vector competence of Aedes dorsalis (Diptera: Culicidae) from Morro Bay, California, for western equine encephalomyelitis virus. J Med Entomol. 1998;35:1020–1024. doi: 10.1093/jmedent/35.6.1020. [DOI] [PubMed] [Google Scholar]
- 13.Reisen WK, Lothrop HD, Chiles RE. Ecology of Aedes dorsalis (Diptera: Culicidae) in relation to western equine encephalomyelitis virus in the Coachella Valley of California. J Med Entomol. 1998;35:561–566. doi: 10.1093/jmedent/35.4.561. [DOI] [PubMed] [Google Scholar]
- 14.Hardy JL. The ecology of western equine encephalomyelitis virus in the Central Valley of California, 1945–1985. Am J Trop Med Hyg. 1987;37:18S–32S. doi: 10.4269/ajtmh.1987.37.18s. [DOI] [PubMed] [Google Scholar]
- 15.Olson JG, Reeves WC, Emmons RW, Milby MM. Correlation of Culex tarsalis population indices with the incidence of St. Louis encephalitis and western equine encephalomyelitis in California. Am J Trop Med Hyg. 1979;28:335–343. doi: 10.4269/ajtmh.1979.28.335. [DOI] [PubMed] [Google Scholar]
- 16.U.S. Department of Agriculture . Veterinary Biologic Products. Ames, IA: Center for Veterinary Biologics, U.S. Department of Agriculture; 2007. [Google Scholar]
- 17.Atasheva S, Wang E, Adams AP, Plante KS, Ni S, Taylor K, Miller ME, Frolov I, Weaver SC. Chimeric alphavirus vaccine candidates protect mice from intranasal challenge with western equine encephalitis virus. Vaccine. 2009;27:4309–4319. doi: 10.1016/j.vaccine.2009.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Aguilar PV, Paessler S, Carrara AS, Baron S, Poast J, Wang E, Moncayo AC, Anishchenko M, Watts D, Tesh RB, Weaver SC. Variation in interferon sensitivity and induction among strains of eastern equine encephalitis virus. J Virol. 2005;79:11300–11310. doi: 10.1128/JVI.79.17.11300-11310.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Frolova E, Frolov I, Schlesinger S. Packaging signals in alphaviruses. J Virol. 1997;71:248–258. doi: 10.1128/jvi.71.1.248-258.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Atasheva S, Wang E, Adams AP, Plant KS, Ni S, Taylor K, Miller ME, Frolov I, Weaver SC. Chimeric alphavirus vaccine candidates protect mice from intranasal challenge with western equine encephalitis virus. Vaccine. 2009;27:4309–4319. doi: 10.1016/j.vaccine.2009.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang E, Petrakova O, Adams AP, Aguilar PV, Kang W, Paessler S, Volk SM, Frolov I, Weaver SC. Chimeric Sindbis/eastern equine encephalitis vaccine candidates are highly attenuated and immunogenic in mice. Vaccine. 2007;25:7573–7581. doi: 10.1016/j.vaccine.2007.07.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fine PEM, Carneiro IA. Transmissibility and persistence of oral polio vaccine viruses: implications for the Global Poliomyelitis Eradication Initiative. Am J Epidemiol. 1999;150:1001–1021. doi: 10.1093/oxfordjournals.aje.a009924. [DOI] [PubMed] [Google Scholar]
- 23.Aguilar PV, Adams AP, Wang E, Kang W, Carrara AS, Anishchenko M, Frolov I, Weaver SC. Structural and nonstructural protein genome regions of eastern equine encephalitis virus are determinants of interferon sensitivity and murine virulence. J Virol. 2008;82:4920–4930. doi: 10.1128/JVI.02514-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gerberg EJ, Barnard DR, Ward RA. Manual for Mosquito Rearing and Experimental Techniques. Bulletin No. 5. Lake Charles, LA: American Mosquito Control Association; 1994. [Google Scholar]
- 25.Beaty BJ, Calisher CH, Shope RE. In: Diagnostic Procedures for Viral, Rickettsial and Chlamydial Infections. Sixth edition. Schmidt NJ, Emmons RW, editors. Washington, DC: American Public Health Association; 1989. pp. 797–855. (Arboviruses). [Google Scholar]
- 26.Smith DR, Carrara AS, Aguilar PV, Weaver SC. Evaluation of methods to assess transmission potential of Venezuelan equine encephalitis virus by mosquitoes and estimation of mosquito saliva titers. Am J Trop Med Hyg. 2005;73:33–39. [PubMed] [Google Scholar]
- 27.Waldridge BM, Wenzel JG, Ellis AC, Rowe-Morton SE, Bridges ER, D’Andrea G, Wint R. Serologic responses to eastern and western equine encephalomyelitis vaccination in previously vaccinated horses. Vet Ther. 2003;4:242–248. [PubMed] [Google Scholar]
- 28.Kramer LD, Hardy JL, Presser SB, Houk EJ. Dissemination barriers for western equine encephalomyelitis virus in Culex tarsalis infected after ingestion of low viral doses. Am J Trop Med Hyg. 1981;30:190–197. doi: 10.4269/ajtmh.1981.30.190. [DOI] [PubMed] [Google Scholar]
- 29.Vaughan JA, Turell MJ. Dual host infections: enhanced infectivity of eastern equine encephalitis virus to Aedes mosquitoes mediated by Brugia microfilariae. Am J Trop Med Hyg. 1996;54:105–109. doi: 10.4269/ajtmh.1996.54.105. [DOI] [PubMed] [Google Scholar]
- 30.Meyers WM, Neafie RC, Marty AM, Wear DJ. Pathology of Infectious Diseases, vol 1. Helminthiases. Washington, DC: Armed Forces Institute of Pathology; pp. 245–306. [Google Scholar]
- 31.Arrigo NC, Watts DM, Frolov I, Weaver SC. Experimental infection of Aedes sollicitans and Aedes taeniorhynchus with two chimeric Sindbis/eastern equine encephalitis virus vaccine candidates. Am J Trop Med Hyg. 2008;78:93–97. [PMC free article] [PubMed] [Google Scholar]


