Abstract
Background
Guidelines for the management of patients with acute myocardial infarction recommend the routine use of 4 effective cardiac medications: angiotensin converting enzyme (ACE) inhibitors, aspirin, β-blockers, and lipid lowering agents. Limited data are available, however, about the contemporary, and changing, use of these therapies, particularly from a population-based perspective. The study describes differences in the use of these medications during hospitalization for acute myocardial infarction according to age, sex, and period of hospitalization.
Methods
The study population consisted of 6,334 women and men treated at 11 hospitals in the Worcester (MA) metropolitan area for acute myocardial infarction in 6 annual periods between 1995 and 2005.
Results
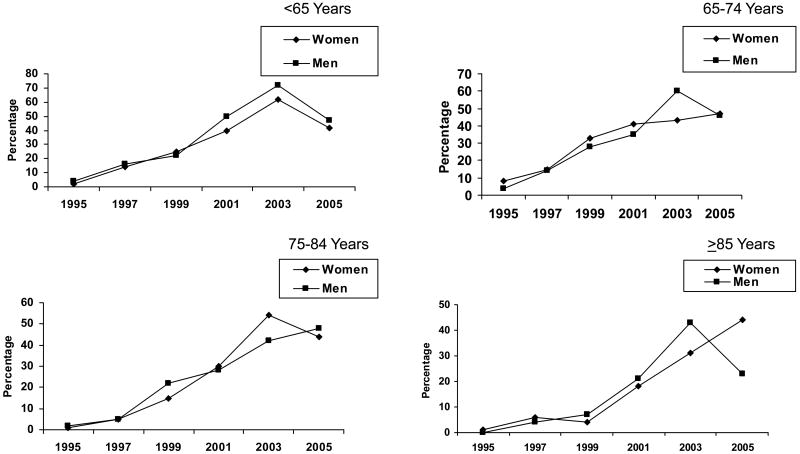
Increases in the use of all 4 cardiac medications during hospitalization for acute myocardial infarction were noted between 1995 and 2005 for all men as well as in those of different age strata (<65 years: 4% to 47%); 65-74 years (4% to 46%); 75-84 years (2% to 48%); and ≥85 years (0% to 23%). Increases in the use of all 4 cardiac medications were also observed in all women as well as in those of all ages over time (2% to 42%); 65-74 years (8% to 47%); 75-84 years (1% to 44%); and ≥85 years (1% to 44%).
Conclusions
The present results suggest marked increases over time in the use of evidence-based therapies in patients hospitalized with acute myocardial infarction. Educational efforts to augment the utilization of these effective cardiac therapies, as well as attempts to identify sub-optimally treated groups, remain warranted.
Keywords: management practices, acute myocardial infarction, changing trends, population-based investigation
Introduction
The treatment of patients with acute myocardial infarction has undergone dramatic changes over the past several decades due to the results of numerous large scale clinical trials which have shown the effectiveness of several cardiac medications including angiotensin converting enzyme (ACE) inhibitors, aspirin, β- blockers, and lipid lowering agents on the hospital and long-term outcomes of patients with acute myocardial infarction1,2. The use of these beneficial therapies is further supported by published guidelines that encourage the prescription of these medications for the vast majority of patients hospitalized with acute myocardial infarction3-6.
Despite age and sex related differences in the mode of presentation and outcomes associated with acute myocardial infarction, guidelines for the use of aspirin, β-blockers, ACE inhibitors, and lipid lowering medications do not differentiate treatment on the basis of age or sex3-6. Several studies have, however, shown that women and the elderly are, in general, treated less aggressively with evidence-based therapies in the setting of acute myocardial infarction than men and younger patients7-9.
The objectives of this study were to describe contemporary, as well as changing, age and sex specific decade long trends (1995-2005) in the use of multiple evidence-based cardiac therapies in patients from a large New England community hospitalized at all area medical centers with acute myocardial infarction. Data from the population-based Worcester Heart Attack Study were utilized for this investigation10-12.
Methods
The Worcester Heart Attack Study is an ongoing observational study which is examining long term trends in the incidence rates, case-fatality rates, and management practices utilized in greater Worcester residents hospitalized at all metropolitan Worcester medical centers with validated acute myocardial infarction on an approximate alternate yearly basis10-12. We restricted our study sample to greater Worcester residents hospitalized with acute myocardial infarction during a recent 10 year period to provide contemporary insights into the use of various cardiac medications as well as to coincide with the more recent introduction of ACE inhibitors to clinical practice. The study population consisted of adult men and women of all ages hospitalized with acute myocardial infarction at any of 11 medical centers in the Worcester metropolitan area during 1995, 1997, 1999, 2001, 2003, and 2005.
The medical records of patients with a discharge diagnosis of acute myocardial infarction were individually reviewed and validated according to predefined diagnostic criteria10-12. All patients hospitalized with acute myocardial infarction, irrespective of their discharge status, were included in the study population. Information about hospital complications of acute myocardial infarction, including heart failure, atrial fibrillation, and cardiogenic shock, was collected from the review of clinical charts10-12. This study was approved by the Office of the Protection of Human Subjects Research at the University of Massachusetts Medical School.
Data Collection
Information about patient's demographic, medical history, and clinical data was collected through the review of hospital medical records by trained nurse and physician abstractors. Information was collected about patient's age, sex, race, comorbidities, acute myocardial infarction order (initial or prior) and type (Q wave or non-Q wave and ST segment elevation vs. non-ST segment elevation), and clinical complications developed during hospitalization10-12. Information about the use of cardiac medications, coronary revascularization procedures, do not resuscitate orders, and hospital discharge status was also reviewed. Major contraindications to the receipt of any of the 4 therapies under study were identified. Exclusion criteria for receipt of the cardiac medications included the following: adverse reaction to β-blockers, allergy to aspirin, asthma, liver disease, major hemorrhage, a positive history of gastrointestinal bleeding, 2nd and 3rd degree atrioventricular block, history of pacing, and current pregnancy. Information about adverse reactions or allergies to statins, or contraindications to the use of ACE inhibitors in patients with renal insufficiency or renal failure, was not collected.
Data Analysis
Differences in the characteristics of patients prescribed and not prescribed the medications under study were examined by use of the chi-square test for discrete variables and t-tests or analysis of variance (ANOVA) for continuous variables. Changes in the proportion of patients treated with different cardiac medications over time were examined through the use of chi-square tests for trends. Multivariable logistic regression models were constructed to examine changing trends in the use of combination drug therapies, separately in men and women of various age strata, while controlling for factors possibly affecting the prescribing of the medications studied. These factors included patient's history of selected comorbidities, acute myocardial infarction associated characteristics, hospital discharge status (alive vs dead), availability of do not resuscitate orders, and receipt of coronary revascularization procedures. We also controlled for patient's health insurance status in these regression analyses though we did not report findings on this factor due to confounding by age (e.g., Medicare status) as well as possible misclassification bias. Multivariable adjusted odds ratios (OR) and accompanying 95% confidence intervals (CIs) were calculated. Given the nonrandomized nature of this observational study, and potential confounding by drug indication and other unmeasured variables, we did not examine the relation between use of these medications and hospital outcomes such as mortality.
Results
Characteristics of Patients Hospitalized with Acute Myocardial Infarction
The study population consisted of 6,334 adult residents of the Worcester metropolitan area hospitalized with acute myocardial infarction during the 6 study years. The mean age of the study sample was 71 years and 56% were men. The average age of greater Worcester men hospitalized with acute myocardial infarction in 1995 was 65 years increasing to 68 years in 2005. The average age of women with confirmed acute myocardial infarction was 73 years in 1995 and 76 years in 2005.
Overall Use of All Effective Cardiac Medications
Among women, across all study years, all 4 cardiac medications were prescribed during hospitalization for acute myocardial infarction to 32.1% of those <65 years, 29.7% of those 65-74 years, 25.6% of patients 75-84 years, and to 20.2% of women 85 years and older (p <.001). Among men, the corresponding use of all 4 effective cardiac medications during the index hospitalization was 35.5%, 29.9%, 24.7%, and 19.8%, respectively (p <.001).
Decade Long Trends in the Use of Multiple Cardiac Medications
The use of all 4 cardiac medications in patients hospitalized with acute myocardial infarction increased from 7.3% in our initial 2 study years of 1995/1997 to 49.3% in our 2 most recent study years of 2003 and 2005. Between 1995/97, and 2003/2005, the increased use of all 4 medications during hospitalization for acute myocardial infarction was similarly evident in men (from 7.9 to 52.2%) as well as in women (from 6.5 to 46.0%: p <.001 for both).
The rate of prescribing individual cardiac medications varied over time. Between 1995 and 2005, the use of ACE inhibitors nearly doubled in both men and women, while a 6 to 7 fold increase in the use of lipid lowering medication was observed. In contrast, in both men and women, the prescribing of aspirin and β-blockers increased less over time, mostly due to the high rate of prescription during the first year of observation for these medications (90-93% and 70-72% respectively).
During the decade long period under study, and during each study interval (Table 1), the use of all 4 beneficial cardiac medications increased significantly in men and women of all ages. These trends were also evident in patients of all races, in those with selected comorbidities, and acute myocardial infarction associated characteristics.
Table 1. Prescribing of Multiple (all four) Cardiac Medications in Patients Hospitalized With Acute Myocardial Infarction According to Patient Characteristics and Study Period.
| Characteristic | 1995/1997 (n= 2,006) (%) |
1999/2001 (n= 2,266) (%) |
2003/2005 (n= 2,060) (%) |
|---|---|---|---|
| Age (yrs) | |||
| <65 | 9.5 | 35.1 | 59.1 |
| 65-74 | 10.3 | 34.4 | 50.2 |
| 75-84 | 3.5 | 24.6 | 47.3 |
| ≥85 | 3.4 | 13.0 | 36.1 |
| Sex | |||
| Male | 7.9 | 30.3 | 52.2 |
| Female | 6.5 | 25.0 | 46.0 |
| Race | |||
| Caucasian | 7.2 | 28.1 | 49.1 |
| Non Caucasian | 8.0 | 27.7 | 50.9 |
| Co-morbidity | |||
| None | 3.8 | 26.8 | 49.8 |
| 1-2 | 6.4 | 27.8 | 49.6 |
| 3-4 | 10.8 | 28.4 | 49.3 |
| ≥5 | 12.5 | 33.7 | 45.8 |
| Acute myocardial infarction characteristics | |||
| Initial | 6.0 | 26.7 | 48.3 |
| Prior | 9.8 | 30.4 | 51.3 |
| Q wave | 9.1 | 35.4 | 63.1 |
| Non-Q wave | 6.3 | 25.5 | 46.1 |
| ST segment elevation | 11.5 | 33.0 | 60.6 |
| Non-ST segment elevation | 5.9 | 24.5 | 44.1 |
| Heart failure | |||
| Present | 6.3 | 25.4 | 46.9 |
| Absent | 7.8 | 29.6 | 51.0 |
| Cardiogenic shock | |||
| Present | 5.8 | 22.5 | 44.3 |
| Absent | 7.4 | 28.4 | 49.6 |
| Atrial fibrillation | |||
| Present | 7.5 | 23.7 | 46.1 |
| Absent | 7.2 | 29.0 | 50.3 |
| Procedures | |||
| Cardiac catheterization | 11.5 | 38.8 | 59.8 |
| Percutaneous coronary intervention | 12.7 | 43.1 | 63.1 |
| Coronary artery bypass grafting | 18.5 | 29.6 | 47.9 |
| Hospital discharge status | |||
| Alive | 8.0 | 30.3 | 52.0 |
| Dead | 2.0 | 11.3 | 22.5 |
Age and Sex Specific Trends in the Use of Multiple Cardiac Medications
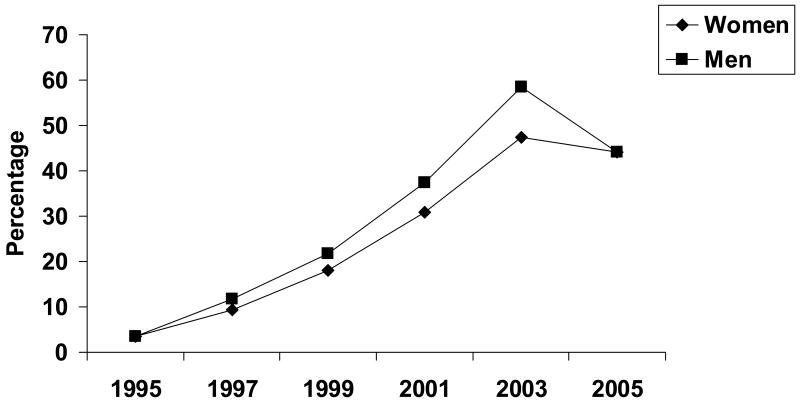
An increasing trend in the prescribing of all 4 cardiac medications was observed in both men and women between 1995 and 2003, followed by a slight decline in the use of all 4 therapies in both sexes during our most recent year under study (Figure 1).
Figure 1.
Trends in the use of multiple evidence-based cardiac therapies in men and women during hospitalization for acute myocardial infarction
Increases in the use of these 4 effective therapies during hospitalization for acute myocardial infarction were observed in men and women of different age strata during the years under study (Figure 2). While these trends were generally similar for men and women in each of the 4 age groups examined, slightly divergent trends were noted in the use of all 4 cardiac therapies during 2005 in elderly patients.
Figure 2.
Trends in the use of multiple evidence-based cardiac therapies during hospitalization for acute myocardial infarction according to age and sex
Factors Associated With the Use of Multiple Cardiac Medications
We examined the association between a variety of demographic and clinical factors with changing trends in the use of all 4 cardiac medications, separately in women (Table 2) and in men (Table 3) of varying ages in a series of regression analyses.
Table 2. Factors Associated With Receipt of All Four Beneficial Cardiac Medications in Women With Acute Myocardial Infarction According to Age (years).
| Clinical Characteristics | <65 | 65-74 | 75-84 | ≥85 | ||||
|---|---|---|---|---|---|---|---|---|
| O.R. | 95% CI | O.R. | 95% CI | O.R. | 95% CI | O.R. | 95% CI | |
| Comorbid conditions | ||||||||
| 0-1 | 0.73 | 0.39,1.37 | 0.65 | 0.37,1.13 | 0.84 | 0.53,1.34 | 0.80 | 0.43,1.48 |
| 2 | 1.18 | 0.62,2.24 | 0.81 | 0.48,1.35 | 1.27 | 0.84,1.93 | 0.91 | 0.54,1.52 |
| Acute myocardial infarction characteristics | ||||||||
| Initial | 1.44 | 0.80,2.59 | 1.56 | 0.97,2.51 | 1.53 | 1.03,2.27 | 1.40 | 0.84,2.34 |
| Q wave | 1.34 | 0.87,2.08 | 0.84 | 0.52,1.38 | 1.19 | 0.80,1.75 | 0.94 | 0.54,1.63 |
| Clinical complications | ||||||||
| Heart failure | 0.79 | 0.49,1.25 | 0.83 | 0.56,1.24 | 0.88 | 0.63,1.21 | 0.87 | 0.58,1.32 |
| Cardiogenic shock | 0.82 | 0.34,1.94 | 1.30 | 0.53,3.17 | 1.94 | 0.90,4.18 | 1.07 | 0.39,2.90 |
| Atrial fibrillation | 1.25 | 0.62,2.52 | 1.00 | 0.59,1.70 | 0.71 | 0.48,1.04 | 0.56 | 0.36,0.88 |
| Discharged alive | 1.76 | 0.62,4.98 | 2.08 | 0.86,5.02 | 2.54 | 1.38,4.70 | 3.96 | 1.85,8.49 |
| Revascularization procedures | 2.90 | 1.81,4.65 | 2.26 | 1.53,3.34 | 3.80 | 2.72,5.30 | 4.70 | 2.86,7.71 |
Referent categories: presence of ≥3 comorbidities, prior acute myocardial infarction, non-Q wave acute myocardial infarction, absence of selected hospital clinical complications, dead at discharge, and lack of receipt of revascularization procedures
Table 3. Factors Associated With Receipt of All Four Beneficial Cardiac Medications in Men According to Age (years).
| Clinical Characteristics | <65 | 65-74 | 75-84 | ≥85 | ||||
|---|---|---|---|---|---|---|---|---|
| O.R. | 95% CI | O.R. | 95% CI | O.R. | 95% CI | O.R. | 95% CI | |
| Comorbid conditions | ||||||||
| 0-1 | 0.55 | 0.36,0.83 | 0.53 | 0.32,0.86 | 0.49 | 0.30,0.79 | 1.04 | 0.46,2.37 |
| 2 | 0.55 | 0.37,0.82 | 1.05 | 0.68,1.63 | 0.69 | 0.45,1.05 | 1.03 | 0.48,2.24 |
| Acute myocardial infarction characteristics | ||||||||
| Initial | 0.82 | 0.58,1.15 | 1.03 | 0.69,1.55 | 1.11 | 0.76,1.64 | 1.65 | 0.82,3.32 |
| Q wave | 1.41 | 1.11,1.78 | 0.96 | 0.67,1.37 | 0.89 | 0.57,1.39 | 0.74 | 0.30,1.87 |
| Clinical complications | ||||||||
| Heart failure | 0.91 | 0.67,1.25 | 0.96 | 0.68,1.36 | 0.93 | 0.66,1.32 | 0.74 | 0.40,1.37 |
| Cardiogenic shock | 1.41 | 0.77,2.57 | 1.73 | 0.83,3.59 | 1.27 | 0.57,2.83 | 6.26 | 0.68,57.65 |
| Atrial fibrillation | 0.73 | 0.47,1.13 | 0.91 | 0.62,1.34 | 0.73 | 0.51,1.06 | 1.18 | 0.61,2.30 |
| Discharged alive | 5.33 | 1.98,14.35 | 2.04 | 0.91,4.55 | 1.69 | 0.87,3.28 | 4.38 | 1.37,14.04 |
| Revascularization procedures | 3.88 | 2.84,5.29 | 2.48 | 1.75,3.51 | 2.57 | 1.81,3.64 | 8.20 | 4.23,15.89 |
Referent categories: presence of ≥3 comorbidities, prior acute myocardial infarction, non-Q wave acute myocardial infarction, absence of selected hospital clinical complications, dead at discharge, and lack of receipt of revascularization procedures
Among women, those with one or without any comorbidity present were significantly less likely to be treated with the 4 beneficial cardiac medications than patients with multiple comorbidities (Table 2). Patients with a non-Q wave acute myocardial infarction, those not treated with revascularization procedures, and those who died during hospitalization were less likely to have been prescribed all 4 beneficial cardiac medications during hospitalization than respective comparison groups (Table 2). Men with fewer comorbidities, those with developed atrial fibrillation or who died during hospitalization, and men who failed to receive a coronary reperfusion/revascularization procedure during their index hospitalization were significantly less likely to be prescribed all 4 beneficial cardiac medications compared to respective referent groups (Table 3). In both women and in men, the significance of factors that may be associated with the prescribing of the multiple cardiac therapies under study were either exaggerated, or attenuated, depending on the age group examined (Tables 2 and 3).
We carried out a secondary analysis in which patients with contraindications to any of these 4 therapies were excluded. After excluding these patients, trends in medication prescribing practices similar to those observed in our total study sample were observed. In 1995/97, 7.8% of all men and 6.1% of all women were prescribed all 4 cardiac therapies during hospitalization for acute myocardial infarction; these percentages increased to 59.3% and 48.5% in 2003/05, respectively.
Similar trends were observed in men and women without contraindications to any of the 4 medications studied in the different age strata examined. For example, in 1995/97, 10.2% of men <65 years, 8.6% of those 65-74 years, 2.9% of those 75-84 years, and 3.5% of those 85 years and older received all 4 cardiac therapies; these percentages increased to 65.2%, 61.3%, 49.6%, and 40.9% in 2003/05, respectively.
Discussion
The results of this community-wide study in residents of a large New England metropolitan area suggest improving trends in the use of 4 cardiac medications currently recommended for the effective management of patients hospitalized with acute myocardial infarction. Despite these encouraging trends, a large percentage of men and women of all ages failed to be treated with all 4 beneficial cardiac therapies.
The American College of Cardiology/American Heart Association guidelines for the use of cardiac medications in patients hospitalized with acute myocardial infarction have recommended the use of β-blockers and aspirin (1990), ACE inhibitors (1996), and the use of lipid lowering medications in the 2002 and 2004 guidelines for the management of patients with non-ST-segment elevation and ST-elevation MI, respectively3-6.
The results of the present study suggest that slightly less than one half of patients hospitalized with acute myocardial infarction were administered all 4 medications during the 2 most recent years under study. This is especially relevant considering that similar prescribing rates were observed when we restricted our analyses to patients without known drug contraindications. While medication utilization patterns increased markedly over time, the less than optimal treatment of these patients continued into our most recent study year which coincided with the more contemporary publication of these treatment guidelines. A recent publication from the multinational Global Registry of Acute Coronary Events (GRACE) suggested relatively similar increases in the use of aspirin, β-blockers, ACE inhibitors, and lipid lowering agents in patients discharged after hospitalization for acute myocardial infarction between 2000 (23%) and 2005 (58%)13.
In previous studies, advanced age and female sex have been associated with the under-prescribing of effective cardiac therapies in patients with acute coronary disease7-9,13-15. Typically, elderly patients are more likely to have a variety of additional comorbidities present, and a greater intolerance to medications, that has likely contributed to the lower utilization of different therapies in elderly as compared to younger patients and to complexities in their more effective management. In agreement with the findings from prior investigations, while age was associated with the receipt of all 4 cardiac medications during hospitalization for acute myocardial infarction in the overall study sample, patients of all ages experienced marked increases in the receipt of evidence-based cardiac therapies over time. Women are typically nearly a decade older than men at the time that they present with acute myocardial infarction and it is believed that this interaction between age and sex is partially attributable to the less than optimal use of effective cardiac medications in women16,17.
Encouragingly, previously observed differences in the use of all 4 cardiac medications examined in men and women during early study years narrowed over time. Our findings also parallel recent observations from the GRACE registry which documented a narrowing of differences over time in the therapeutic management of men and women hospitalized with acute myocardial infarction in 14 countries13.
The use of each of the 4 cardiac therapies examined increased during the 10 year period under study; however, there were significant differences in the magnitude of increases in individual agents overall as well as according to age and sex. Particularly marked increases were observed in the use of ACE inhibitors and lipid lowering agents between 1995 and 2005.
In our 2 most recently hospitalized study cohorts, there were modest differences in the use of ACE inhibitors, aspirin, β-blockers and lipid lowering drugs according to sex. In the GRACE registry, differences in the use of combination medical therapy in men and women hospitalized with an acute syndrome in 2005 were unchanged from those observed in prior study years, showing that men were more likely to be treated with these effective therapies than women13.
Factors Associated With Receipt of Multiple Cardiac Therapies
We identified a number of factors associated with a reduced likelihood of being prescribed the 4 beneficial cardiac medications examined. Patients with fewer comorbid conditions were less likely to be prescribed all 4 cardiac medications as compared to patients with multiple comorbidities. It is likely that patients with a specific comorbidity were more likely to be on selected medications prior to their acute myocardial infarction and that patients with multiple comorbidities were more likely to be continued on their prior therapeutic regimen.
In our study, failure to undergo a coronary reperfusion or revascularization procedure during hospitalization for acute myocardial infarction was associated with a reduced likelihood of receiving combination medical therapy. Other studies have also suggested that patients with acute coronary disease who receive interventional procedures are more likely to be treated with more intensive medical therapies than patients who do not undergo these coronary reperfusion/revascularization approaches19-21.
Study Strengths and Limitations
The inclusion of all patients hospitalized with acute myocardial infarction in a community-wide setting provides a unique opportunity to examine trends in the therapeutic management of an unselected population of men and women of all ages. An additional strength of this community-based study is the inclusion of “real world” patients with acute myocardial infarction treated in the community in contrast to patients that receive a prescribed therapeutic regimen as occurs in the context of randomized clinical trials with their more narrowly defined inclusion/exclusion criteria. In terms of study limitations, we were unable to systematically determine the number of patients eligible to receive the 4 cardiac medications examined; similarly, we did not collect information about the adverse effects related to the use of these medications, reasons by patients as well as by their physicians for not using these medications, as well as timing/dosages of the medications prescribed. We did not examine the relation of medication prescribing practices to hospital outcomes given the nonrandomized nature of the present study and potential for confounding by drug indication.
Conclusions
The results of the present study suggest encouraging increases in the use of combination medical therapy in patients of both sexes and across all ages hospitalized with acute myocardial infarction in accord with recently published guidelines. Our results also suggest that previously observed inequalities in management practices between men and women have been attenuated during recent study years. Nevertheless, the proportion of eligible patients who were prescribed all 4 therapies during recent years remained less than 60% for men and for women and for patients of different ages.
While academic detailing, continuing medical education seminars, quality assurance initiatives, and other educational approaches remain needed to encourage physicians to treat these high risk patients in a more optimal manner22-24, further gains in the utilization of all evidence-based cardiac therapies in patients hospitalized with acute myocardial infarction may be harder to realize. Recent efforts to tie quality of care benchmarks to hospital reimbursement may prove to be effective in the future. Continued surveillance of the therapeutic management of patients hospitalized with acute myocardial infarction remains important to ensure that the proportion of eligible patients receiving effective cardiac therapies continues to increase.
Acknowledgments
This research was made possible through funding support provided by the National Institutes of Health (RO1 HL35434).
Footnotes
All authors had access to the data and a role in writing this manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.American Heart Association. Heart Disease and Stroke Statistics – 2007 Update. Dallas, Texas: American Heart Association; 2007. [Google Scholar]
- 2.Yusuf S, Sleight P, Held P, McMahon S. Routine medical management of acute myocardial infarction: lessons from overviews of recent randomized controlled trials. Circulation. 1990;82(Suppl II):II117–II134. [PubMed] [Google Scholar]
- 3.Gunnar RM, Passamani ER, Bourdillon PD, et al. Guidelines for the early management of patients with acute myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Assessment of Diagnostic and Therapeutic Cardiovascular Procedures (Subcommittee to Develop Guidelines for the Early Management of Patients With Acute myocardial infarction) J Am Coll Cardiol. 1990;16:249–292. doi: 10.1016/0735-1097(90)90575-a. [DOI] [PubMed] [Google Scholar]
- 4.Ryan TJ, Anderson JL, Antman EM, et al. ACC/AHA guidelines for the management of patients with acute myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute myocardial infarction) J Am Coll Cardiol. 1996;28:1328–1428. doi: 10.1016/s0735-1097(96)00392-0. [DOI] [PubMed] [Google Scholar]
- 5.Braunwald E, Antman EM, Beasley JW, et al. ACC/AHA 2002 guideline update for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on the Management of Patients With Unstable Angina) Circulation. 2002;106:1893–1900. doi: 10.1161/01.cir.0000037106.76139.53. [DOI] [PubMed] [Google Scholar]
- 6.Antman EM, Anbe DT, Armstrong PW, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction; A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of patients with acute myocardial infarction) J Am Coll Cardiol. 2004;44:E1–E211. doi: 10.1016/j.jacc.2004.07.014. [DOI] [PubMed] [Google Scholar]
- 7.Maynard C, Litwin PE, Martin JS, Weaver WD. Gender differences in the treatment and outcome of acute myocardial infarction: results from the Myocardial Infarction Triage and Intervention Registry. Arch Intern Med. 1992;152:972–976. [PubMed] [Google Scholar]
- 8.Spencer FA, Lessard D, Yarzebski J, et al. Decade-long changes in the use of combination evidence-based medical therapy at discharge for patients surviving acute myocardial infarction. Am Heart J. 2005;150:838–844. doi: 10.1016/j.ahj.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 9.McLaughlin TJ, Soumerai SB, Willison DJ, et al. Adherence to national guidelines for drug treatment of suspected acute myocardial infarction: evidence for undertreatment in women and the elderly. Arch Intern Med. 1996;156:799–805. [PubMed] [Google Scholar]
- 10.Goldberg RJ, Gore JM, Alpert JS, Dalen JE. Recent changes in attack and survival rates of acute myocardial infarction (1975 through 1981). The Worcester Heart Attack Study. JAMA. 1986;255:2774–2779. [PubMed] [Google Scholar]
- 11.Goldberg RJ, Yarzebski J, Lessard D, Gore JM. A two-decades (1975 to 1995) long experience in the incidence, in-hospital and long-term case-fatality rates of acute myocardial infarction: a community-wide perspective. J Am Coll Cardiol. 1999;33:1533–1539. doi: 10.1016/s0735-1097(99)00040-6. [DOI] [PubMed] [Google Scholar]
- 12.Floyd KC, Yarzebski J, Spencer FA, Lessard D, Dalen JE, Alpert JS, Gore JM, Goldberg RJ. A 30 year perspective (1975-2005) into the changing landscape of patients hospitalized with initial acute myocardial infarction: Worcester Heart Attack Study. Circ Cardiovasc Qual Outcomes. 2009;2:88–95. doi: 10.1161/CIRCOUTCOMES.108.811828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goldberg RJ, Spencer FA, Steg PG, et al. for the Global Registry of Acute Coronary Events Investigators Increasing use of single and combination medical therapy in patients hospitalized for acute myocardial infarction in the 21st century. Arch Intern Med. 2007;167:1766–1773. doi: 10.1001/archinte.167.16.1766. [DOI] [PubMed] [Google Scholar]
- 14.Vaccarino V, Krumholz HM, Berkman LF, Horwitz RI. Sex differences in mortality after myocardial infarction. Circulation. 1995;91:1861–1871. doi: 10.1161/01.cir.91.6.1861. [DOI] [PubMed] [Google Scholar]
- 15.Spencer FA, Frederick PD, Goldberg RJ, et al. for the National Registry of Myocardial Infarction-4 Investigators Use of combination evidence-based medical therapy prior to acute myocardial infarction (from the National Registry of Myocardial Infarction-4) Am J Cardiol. 2005;96:922–926. doi: 10.1016/j.amjcard.2005.05.048. [DOI] [PubMed] [Google Scholar]
- 16.Vaccarino V, Horwitz RI, Meehan TP, et al. Sex differences in mortality after acute myocardial infarction: evidence for a sex-age interaction. Arch Intern Med. 1998;158:2054–2062. doi: 10.1001/archinte.158.18.2054. [DOI] [PubMed] [Google Scholar]
- 17.Harrold LR, Lessard D, Yarzebski J, et al. Age and sex differences in the treatment of patients with initial acute myocardial infarction: a community-wide perspective. Cardiology. 2003;99:39–46. doi: 10.1159/000068445. [DOI] [PubMed] [Google Scholar]
- 18.Wald NJ, Law MR. A strategy to reduce cardiovascular disease by more than 80% Br Med J. 2003;326:1419–1424. doi: 10.1136/bmj.326.7404.1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Spencer FA, Scleparis G, Goldberg RJ, et al. Decade long trends (1986 to 1997) in the medical management of patients with acute myocardial infarction: a community-wide perspective. Am Heart J. 2001;142:594–603. doi: 10.1067/mhj.2001.117776. [DOI] [PubMed] [Google Scholar]
- 20.Spencer FA, Goldberg RJ, Frederick PD, et al. Age and the utilization of cardiac catheterization following uncomplicated first acute myocardial infarction treated with thrombolytic therapy (The Second National Registry of Myocardial Infarction [NRMI-2]) Am J Cardiol. 2001;88:107–111. doi: 10.1016/s0002-9149(01)01602-2. [DOI] [PubMed] [Google Scholar]
- 21.Stafford RS, Radley DC. The underutilization of cardiac medications of proven benefit, 1990 to 2002. J Am Coll Cardiol. 2003;41:56–61. doi: 10.1016/s0735-1097(02)02670-0. [DOI] [PubMed] [Google Scholar]
- 22.Mehta RH, Montoye CK, Gallogly M, et al. Improving quality of care for acute myocardial infarction: the guidelines applied in practice (GAP) initiative. JAMA. 2002;287:1269–1276. doi: 10.1001/jama.287.10.1269. [DOI] [PubMed] [Google Scholar]
- 23.Lewis WR, Peterson ED, Cannon CP, et al. An organized approach to the improvement in guideline adherence for acute myocardial infarction. Results with the Get With The Guidelines Quality Improvement Program. Arch Intern Med. 2008;168:1813–1819. doi: 10.1001/archinte.168.16.1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mehta RH, Roe MT, Chen AY, et al. Recent trends in the care of patients with non-ST-segment elevation acute coronary syndromes: insights from the CRUSADE initiative. Arch Intern Med. 2006;166:2027–2034. doi: 10.1001/archinte.166.18.2027. [DOI] [PubMed] [Google Scholar]