Abstract
Diabetes mellitus can affect ventricular repolarization, and we investigated the impact of diabetes on the risk for cardiac events in older patients with Long QT Syndrome (LQTS). The study population consisted of 1,152 patients with QTc≥450ms who were enrolled in the U.S. portion of the International LQTS Registry and survived beyond 40 years of age. Patients were categorized as having diabetes if they received oral diabetic medication or insulin. End points after age 40 included first cardiac event (syncope, aborted cardiac arrest, sudden cardiac death, whichever occurred first) and all-cause mortality. Follow-up extended from age 41 to 75 years. The risk factors for the end points were evaluated by the Cox model. During follow-up, 193 patients experienced a first cardiac event, and 99 patients died. Among LQTS patients, the development of diabetes in adult LQTS patients was not associated with an increased risk of first cardiac events dominated by syncope. The risk factors for mortality were syncope before age 41, QTc ≥500ms, heart rate >80bpm, and diabetes; there was no mortality interaction involving diabetes and QTc ≥500ms. In conclusion, diabetes and prolonged QTc contributed independent mortality risks in adult patients with LQTS, with no interaction between these two risk factors.
While many prior Long QT Syndrome (LQTS) studies have focused on pediatric and young adult patients with this disorder,1–6 a few recent studies have highlighted the association of LQTS with common co-morbidities in adults >40 years of age.7, 8 No study, however, has focused on the risk conferred by diabetes mellitus (DM) in LQTS patients despite the fact that QTc prolongation occurs in diabetic patients and contributes to increased risk in patients with DM.9 The current study examines whether the development of DM is associated with an increased risk for cardiac events in older adults with LQTS.
METHODS
We studied patients >40 years of age who were enrolled in the U.S. portion of the International Long QT Syndrome Registry. Baseline clinical data were obtained on all enrolled family members <41 years of age, and this included ECGs and history of LQTS-related syncope as previously reported.1 Patient selection criteria for this study required survival >40 years of age in LQTS Registry subjects who had an ECG with QTc ≥450ms and answered a prospective follow-up questionnaire regarding the age of non-LQTS related comorbidities related to coronary artery disease, hypertension, and diabetes mellitus during follow-up extending up to age 75 years of age. We did not collect information on hyperglycemia or degree of diabetic control. Patients were considered to have diabetes mellitus if they were taking oral diabetic medication or were receiving insulin during follow-up. The end points for patients over 40 years of age were first cardiac events (syncope, aborted cardiac arrest, or sudden cardiac death using a 1-hour definition for the terminal event, whichever occurred first) and all-cause mortality.
Patients were identified as having coronary artery disease (CAD) if they indicated on the medical questionnaire the date when they had been hospitalized for a myocardial infarction, coronary angioplasty, coronary artery bypass graft surgery, or were prescribed medication for the treatment of angina pectoris.
Clinical characteristics were compared using chi-square or Fisher’s exact tests for categorical variables and Student’s t test for continuous variables. Graphical display of the time to event before and after time-dependent diabetes was identified utilized the Byar-Mantel method.10 The contributions of relevant clinical variables including QTc, time-dependent diabetes mellitus, time-dependent beta-blocker therapy, and prespecified interactions to the risk of a first cardiac event and separately for mortality were determined using Cox proportional hazards regression models.11
Statistical significance was determined by p ≤ 0.05, and all tests were two-sided. SAS version 9.1.3 (SAS, Cary, North Carolina) was used to perform the statistical analyses.
RESULTS
The study population involved 1,152 LQTS patients who were followed past the age of 40 years. Diabetes mellitus was identified in 71 patients at some time during follow-up. The clinical characteristics of the study population are presented in Table 1. Overall, diabetic patients had faster heart rates and there was a trend towards an increased frequency of coronary disease compared to those unaffected with diabetes. During follow-up, 193 patients experienced a first cardiac event, and 99 patients died.
Table 1.
Clinical Characteristics of the Study Population
| QTc ≥ 450ms (n=1152) | P- value | ||
|---|---|---|---|
| Variable | Diabetes Mellitus | ||
| No (n=1081) | Yes (n=71) | ||
| Female | 753 (70%) | 43 (61%) | 0.11 |
| Caucasian | 1047 (97%) | 67 (94%) | 0.28 |
| Age at ECG recording, years | 48 ± 15 | 53 ± 13 | 0.001 |
| ECG data | |||
| QTc baseline (msec) | 488 ± 42 | 484 ± 47 | 0.04 |
| RR baseline (msec) | 874 ± 186 | 791 ±158 | <0.001 |
| Beta-blockers | 517 (48%) | 31 (44%) | 0.50 |
| LQTS Mutations | n=318 | ||
| LQT1 | 149 (49%) | 4 (27%) | 0.09 |
| LQT2 | 124 (41%) | 10 (67%) | 0.04 |
| Other/Multiple | 30 (10%) | 1 (7%) | 0.99 |
| Non-LQTS comorbidities* | n = 191 | ||
| Coronary artery disease | 13 (54%) | 61 (37%) | 0.10 |
| Hypertension | 129 (77%) | 17 (71%) | 0.49 |
| Stroke | 17 (10) | 2 (8) | 0.99 |
| End points | |||
| 1st cardiac events† | 181 (17%) | 12 (20%) | 0.49 |
| Mortality | 89 (8%) | 10 (17%) | 0.02 |
Values are mean ± SD where indicated.
Number of patients with available information.
Syncope, aborted cardiac arrest or sudden death, whichever occurred first.
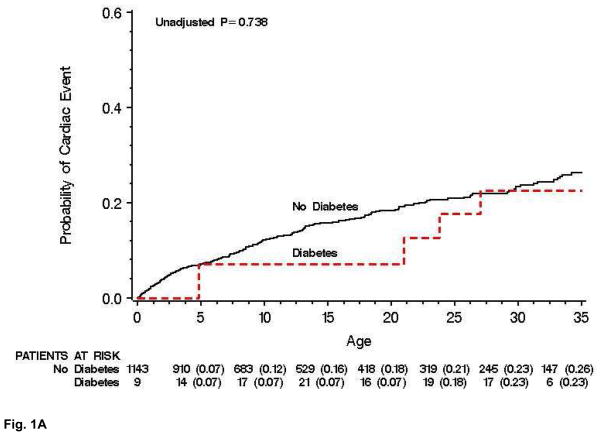
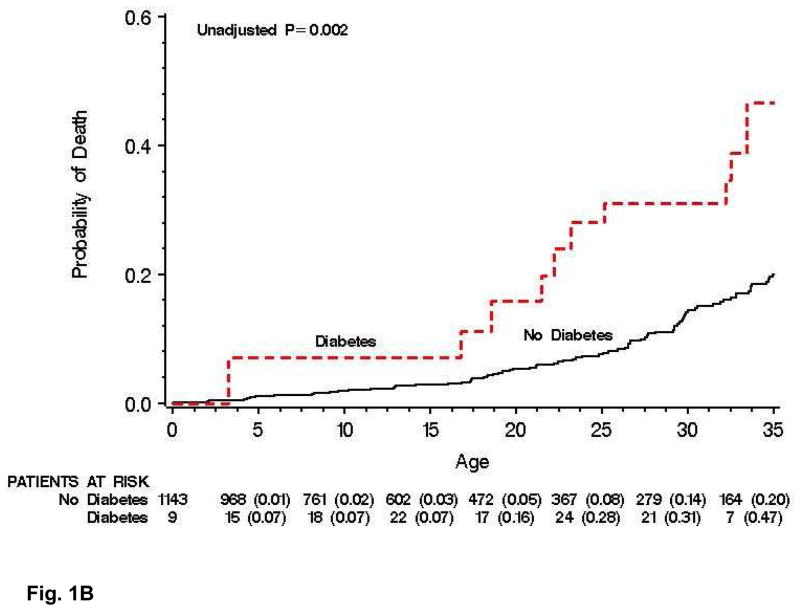
The probabilities of experiencing a first cardiac event or all-cause mortality before and after the development of DM in patients affected with LQTS are shown in Figures 1A and 1B, respectively. The probability of a first cardiac event was similar in diabetics and non-diabetics (Fig. 1A), but death was more frequent in diabetics than non-diabetics (Fig. 1B).
Figure 1.
Figure 1A. Byar-Mantel graphic display of the probability of first cardiac event in diabetic and non-diabetic patients with Long QT Syndrome from age 41 to 75 years.
Figure 1B. Byar-Mantel graphic display of the probability of all-cause mortality in diabetic and non-diabetic patients with Long QT Syndrome from age 41 to 75 years.
As shown in Table 2, risk factors for a first cardiac event (syncope or mortality, whichever occurred first) after age 40 years included history of a cardiac event before age 41, QTc ≥500 ms, and female gender. Beta-blocker therapy was associated with a reduced probability of cardiac events with a hazard ratio of 0.59. Time-dependent development of diabetes did not make a significant contribution to the cardiac event risk model. .
Table 2.
Cox model for first cardiac events* after 40 years of age in Patients with Long QT Syndrome (QTc ≥ 450 ms).
| HR | 95% CI | P-value | |
|---|---|---|---|
| Factor | |||
| Time-dependent diabetes | 0.77 | 0.28–2.08 | 0.60 |
| Cardiac event before age 41 years | 2.96 | 2.14–4.11 | <0.001 |
| QTc ≥ 500ms | 1.79 | 1.34–2.40 | <0.001 |
| Female Gender | 1.41 | 1.00–1.98 | 0.05 |
| Treatment with beta blockers | 0.59 | 0.40–0.87 | <0.01 |
Cardiac events include syncope, aborted cardiac arrest, or sudden cardiac death, whichever occurred first.
The risk factors for all-cause mortality included, time-dependent DM, time-dependent syncope, heart rate >80bpm, and QTc≥500ms (Table 3). There was no meaningful or significant interaction between QTc and diabetes on mortality. The efficacy of beta-blocker therapy could not be evaluated because only a small number of diabetic patients who died had been treated with beta-blockers.
Table 3.
Cox model for mortality after 40 years of age in patients with Long QT Syndrome (QTc≥ 450ms).
| Factor | HR | 95% CI | P Value |
|---|---|---|---|
| Time-dependent diabetes | 2.31 | 1.21–4.72 | <0.01 |
| Time-dependent syncope | 1.69 | 1.03–2.87 | <0.05 |
| QTc ≥500 ms | 1.52 | 1.00–2.30 | <0.05 |
| RR<740ms | 1.63 | 1.07–2.49 | <0.05 |
DISCUSSION
The development of DM in LQTS patients over 40 years of age was associated with an increased mortality risk. This DM risk was independent of increased QTc and syncopal events before age 41, both known risk factor in LQTS, and there was no significant interaction between QTc and DM on mortality. This lack of QTc – DM interaction indicates that patients with both QTc≥500ms and DM had a mortality risk equivalent to the multiplicative risk of the two factors, a finding suggesting the absence of an exacerbating mechanism on mortality when these two factors co-exist. Interestingly, the development of DM in LQTS patients was not associated with a higher risk for first cardiac events, an end point dominated by syncope.
Diabetes mellitus is a strong risk factor for acquired cardiac disease, specifically coronary artery disease and diabetic cardiomyopathy.12, 13 A meta-analysis of several studies found that both males and females with DM had increased risk of developing fatal CAD, with the effect more pronounced in women than men.14 In patients with CAD, diabetics experience more cardiac complications than non-diabetics.15 Our current study shows that DM poses a serious health risk for LQTS patients just as it does in non-LQTS patients.
Although cardiac arrhythmias frequently occur in diabetics with CAD and heart failure, a recent study has shown that DM is associated with an increased risk for ventricular fibrillation independent of these comorbidities.16 Several studies in animal models have demonstrated QT prolongation and ventricular arrhythmias following induction of DM, possibly due to inhibition of expression of the HERG K+ channel, important in the repolarization of cardiac myocytes.17 Furthermore, insulin treatment restored expression of HERG in diabetic myocardium.18 In our adult LQTS population, DM and prolonged QTc were independent risk factor for mortality, and there was no significant interaction involving these 2 risk variables.
There are several limitations in this observational, retrospective study. This study defined LQTS by QTc≥ 450 msec on a baseline ECG. This leaves the potential for misclassification of study subjects as some patients with LQTS-related symptoms may have QTc intervals <450 ms and some genetically unaffected patients may have QTc ≥450 ms. Only 27% of the patients with QTc≥450ms were genotyped. Although all diabetics included in the analysis were treated with either insulin or oral hypoglycemics, the dosages of the therapies were not available.
Acknowledgments
This work was supported in part by research grants HL-33843 (Moss) and HL-51618 (Moss) from the National Institutes of Health, Bethesda, Maryland and by an unrestricted research grant from BioReference Labs, Inc., Elmwood Park, New Jersey.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Moss AJ, Schwartz PJ, Crampton RS, Tzivoni D, Locati EH, MacCluer J, Hall WJ, Weitkamp L, Vincent GM, Garson A, Jr, Robinson JL, Benhorin J, Choi S. The long QT syndrome. Prospective longitudinal study of 328 families. Circulation. 1991;84:1136–1144. doi: 10.1161/01.cir.84.3.1136. [DOI] [PubMed] [Google Scholar]
- 2.Goldenberg I, Moss AJ. Long QT syndrome. J Am Coll Cardiol. 2008;51:2291–2300. doi: 10.1016/j.jacc.2008.02.068. [DOI] [PubMed] [Google Scholar]
- 3.Priori SG, Schwartz PJ, Napolitano C, Bloise R, Ronchetti E, Grillo M, Vicentini A, Spazzolini C, Nastoli J, Bottelli G, Folli R, Cappelletti D. Risk stratification in the long-QT syndrome. N Engl J Med. 2003;348:1866–1874. doi: 10.1056/NEJMoa022147. [DOI] [PubMed] [Google Scholar]
- 4.Goldenberg I, Moss AJ, Peterson DR, McNitt S, Zareba W, Andrews ML, Robinson JL, Locati EH, Ackerman MJ, Benhorin J, Kaufman ES, Napolitano C, Priori SG, Qi M, Schwartz PJ, Towbin JA, Vincent GM, Zhang L. Risk factors for aborted cardiac arrest and sudden cardiac death in children with the congenital long-QT syndrome. Circulation. 2008;117:2184–2191. doi: 10.1161/CIRCULATIONAHA.107.701243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hobbs JB, Peterson DR, Moss AJ, McNitt S, Zareba W, Goldenberg I, Qi M, Robinson JL, Sauer AJ, Ackerman MJ, Benhorin J, Kaufman ES, Locati EH, Napolitano C, Priori SG, Towbin JA, Vincent GM, Zhang L. Risk of aborted cardiac arrest or sudden cardiac death during adolescence in the long-QT syndrome. JAMA. 2006;296:1249–1254. doi: 10.1001/jama.296.10.1249. [DOI] [PubMed] [Google Scholar]
- 6.Locati EH, Zareba W, Moss AJ, Schwartz PJ, Vincent GM, Lehmann MH, Towbin JA, Priori SG, Napolitano C, Robinson JL, Andrews M, Timothy K, Hall WJ. Age- and sex-related differences in clinical manifestations in patients with congenital long-QT syndrome: findings from the International LQTS Registry. Circulation. 1998;97:2237–2244. doi: 10.1161/01.cir.97.22.2237. [DOI] [PubMed] [Google Scholar]
- 7.Goldenberg I, Moss AJ, Bradley J, Polonsky S, Peterson DR, McNitt S, Zareba W, Andrews ML, Robinson JL, Ackerman MJ, Benhorin J, Kaufman ES, Locati EH, Napolitano C, Priori SG, Qi M, Schwartz PJ, Towbin JA, Vincent GM, Zhang L. Long-QT syndrome after age 40. Circulation. 2008;117:2192–2201. doi: 10.1161/CIRCULATIONAHA.107.729368. [DOI] [PubMed] [Google Scholar]
- 8.Sze E, Moss AJ, Goldenberg I, McNitt S, Jons C, Zareba W, Qi M, Robinson JL. Long QT syndrome in patients over 40 years of age: increased risk for LQTS-related cardiac events in patients with coronary disease. Ann Noninvasive Electrocardiol. 2008;13:327–331. doi: 10.1111/j.1542-474X.2008.00250.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rana BS, Lim PO, Naas AA, Ogston SA, Newton RW, Jung RT, Morris AD, Struthers AD. QT interval abnormalities are often present at diagnosis in diabetes and are better predictors of cardiac death than ankle brachial pressure index and autonomic function tests. Heart. 2005;91(1):44–50. doi: 10.1136/hrt.2003.017632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Byar DP, Mantel N. Some interrelationships among the regression coefficient estimates arising in a class of models appropriate to response-time data. Biometrics. 1975;31:943–947. [PubMed] [Google Scholar]
- 11.Cox DR. Regression models and life-tables. J Stat Soc [B] 1972;34:187–220. [Google Scholar]
- 12.Boudina S, Abel ED. Diabetic cardiomyopathy revisited. Circulation. 2007;115:3213–3223. doi: 10.1161/CIRCULATIONAHA.106.679597. [DOI] [PubMed] [Google Scholar]
- 13.Kannel WB, McGee DL. Diabetes and cardiovascular disease. The Framingham study. JAMA. 1979;241:2035–2038. doi: 10.1001/jama.241.19.2035. [DOI] [PubMed] [Google Scholar]
- 14.Huxley R, Barzi F, Woodward M. Excess risk of fatal coronary heart disease associated with diabetes in men and women: meta-analysis of 37 prospective cohort studies. BMJ. 2006;332:73–78. doi: 10.1136/bmj.38678.389583.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ahmed S, Cannon CP, Murphy SA, Braunwald E. Acute coronary syndromes and diabetes: Is intensive lipid lowering beneficial? Results of the PROVE IT-TIMI 22 trial. Eur Heart J. 2006;27(19):2323–2329. doi: 10.1093/eurheartj/ehl220. [DOI] [PubMed] [Google Scholar]
- 16.Movahed MR, Hashemzadeh M, Jamal M. Increased prevalence of ventricular fibrillation in patients with type 2 diabetes mellitus. Heart Vessels. 2007;22(4):251–253. doi: 10.1007/s00380-006-0962-9. [DOI] [PubMed] [Google Scholar]
- 17.Xiao J, Luo X, Lin H, Zhang Y, Lu Y, Wang N, Zhang Y, Yang B, Wang Z. MicroRNA miR-133 represses HERG K+ channel expression contributing to QT prolongation in diabetic hearts. J Biol Che. 2007;282(17):12363–12367. doi: 10.1074/jbc.C700015200. [DOI] [PubMed] [Google Scholar]
- 18.Zhang Y, Xiao J, Wang H, Luo X, Wang J, Villeneuve LR, Zhang H, Bai Y, Yang B, Wang Z. Restoring depressed HERG K+ channel function as a mechanism for insulin treatment of abnormal QT prolongation and associated arrhythmias in diabetic rabbits. Am J Physiol Heart Circ Physio. 2006;291(3):H1446–1455. doi: 10.1152/ajpheart.01356.2005. [DOI] [PubMed] [Google Scholar]