Abstract
Patellofemoral pain is a common knee disorders with a multi-factorial etiology related to abnormal patellar tracking. Our hypothesis was that the pattern of 3-dimensional rotation and translation of the patella induced by selective activation of individual quadriceps components would differ between subjects with patellofemoral pain and healthy subjects. Nine female subjects with patellofemoral pain and seven healthy female subjects underwent electrical stimulation to selectively activate individual quadriceps components (vastus medialis obliquus, VMO; vastus medialis lateralis, VML; vastus lateralis, VL) with the knee at 0° and 20° flexion, while three-dimensional patellar tracking was recorded. Normalized direction of rotation and direction of translation characterized the relative amplitudes of each component of patellar movement. VMO activation in patellofemoral pain caused greater medial patellar rotation (distal patellar pole rotates medially in frontal plane) at both knee positions (p<0.01), and both VMO and VML activation caused increased anterior patellar translation (p<0.001) in patellofemoral pain compared to healthy subjects at 20° knee flexion. VL activation caused more lateral patellar translation (p<0.001) in patellofemoral pain compared to healthy subjects. In healthy subjects the 3-D mechanical action of the VMO is actively modulated with knee flexion angle while such modulation was not observed in PFP subjects. This could be due to anatomical differences in the VMO insertion on the patella and medial quadriceps weakness. Quantitative evaluation of the influence of individual quadriceps components on patellar tracking will aid understanding of the knee extensor mechanism and provide insight into the etiology of patellofemoral pain.
Keywords: Patella, Tracking, In vivo, Kinematics, Patellofemoral Pain, Malalignment
INTRODUCTION
Patellofemoral pain (PFP) is one of the most common knee disorders seen in an orthopaedic practice (Fulkerson, 1997; Powers et al., 2004), with a reported incidence as high as 25% in the general population, and even higher among athletes (Devereaux and Lachmann, 1984; Insall, 1995). PFP syndrome is a serious problem because participation in sports and daily activities may be substantially affected by the pain, and chronic PFP may lead to joint degeneration (Fulkerson, 2002). Despite the high incidence, the pathophysiology of PFP is not clearly understood (Dye, 2005; Fulkerson, 2002).
Current literature suggests the etiology of PFP is multi-factorial (Csintalan et al., 2002; Schepsis and Watson, 2005), and closely related to static patellar malalignment and abnormal patellar tracking (Fitzgerald and McClure, 1995; Fulkerson, 2002; Grelsamer and Stein, 2005; Sheehan et al., 2009; Wilson et al., 2009). Patellar alignment and tracking have been evaluated using techniques such as x-ray, computed tomography, magnetic resonance imaging, and motion analysis at different knee flexion angles (Guzzanti et al., 1994; Hirokawa, 1992; McNally et al., 2000; Sheehan et al., 2009; Wilson et al., 2009). However, none of these methods provide quantitative information on the actions of the individual quadriceps on the patella.
Patellar tracking relies on the bony architecture of the knee, but is also dependent on the magnitudes and directions of forces from the soft tissue structures surrounding the patellofemoral joint (Amis et al., 2006). Reduced action of the medial stabilizers, especially the vastus medialis obliquus (VMO), is thought to be an important factor in patellofemoral kinematics (Goh et al., 1995; Koskinen and Kujala, 1992; Lieb and Perry, 1968; Sakai et al., 2000). The action of the VMO is believed to limit lateral shift and tilt due to its anatomical location (Goh et al., 1995; Heegaard et al., 1994; Koh et al., 1992; Lin et al., 2004; Sakai et al., 2000). Therefore, it is important to understand how patellar tracking is influenced by the mechanical actions of each individual quadriceps component.
Our purpose was to compare, in vivo and noninvasively, patellar tracking patterns induced by selective activation of individual quadriceps components in subjects with PFP syndrome to healthy subjects. More specifically, this study focused on the function of the VMO and VL in controlling patellar tracking. We hypothesized that PFP is associated with altered six degree-of-freedom (DOF) mechanical actions of the individual quadriceps components. Quantitative evaluation of the role individual quadriceps play in patellar tracking will aid understanding of the knee extensor mechanism and provide insight into the mechanisms underlying PFP.
MATERIALS AND METHODS
Nine female subjects with clinically-diagnosed idiopathic PFP syndrome participated in this study. None of these subjects had PFP initiated by a traumatic episode or arthritis. In general, patients did not indicate any improvement from physical therapy. Seven female healthy subjects with no prior history of knee injuries were used as a control group. Each subject’s activity level was documented and similar variation was seen in both groups, ranging from inactive to active athletes. The study protocol was approved by the Institutional Review Board, and all subjects provided informed consent prior to participation. There were no significant differences between the two groups for gender, age, height, or weight (Table 1).
Table 1.
Demographic characteristics of the subject population (Mean ±SD)
| Healthy Subjects | PFP Subjects | p-value | |
|---|---|---|---|
| Number and Gender | 7 female | 9 female | 0.99 |
| Age (years) | 27.8 (±8.5) | 30.9 (±7.0) | 0.44 |
| Height (cm) | 165.8(±7.0) | 161.1 (±7.6) | 0.23 |
| Weight (kg) | 66.1 (±22.8) | 61.0 (±8.7) | 0.54 |
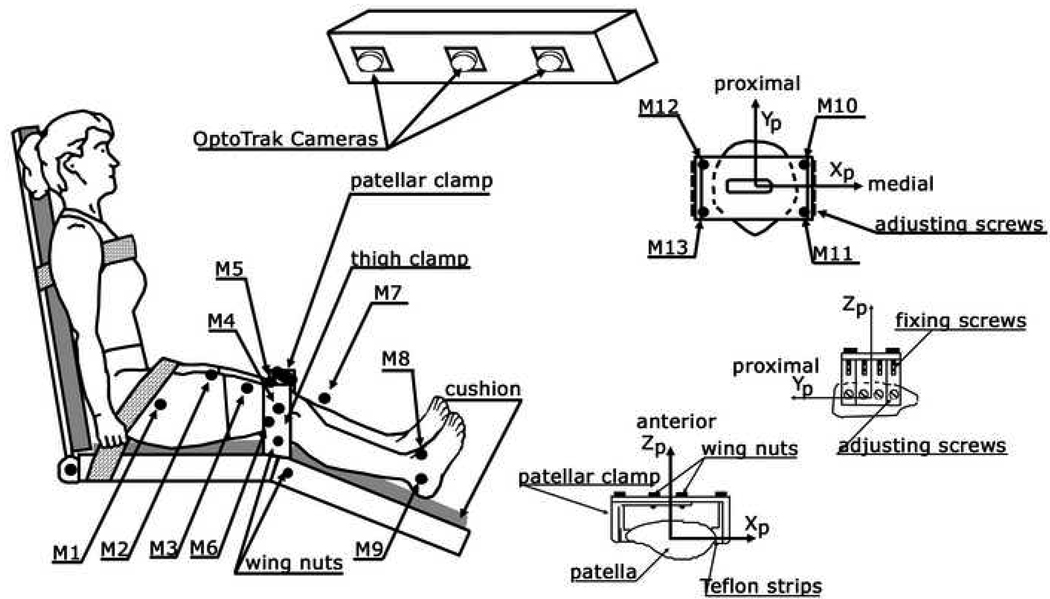
Before testing, patellar medial-lateral glide was manually tested to examine patellar mobility. Subjects sat upright with the back and thigh supported (Figure 1) (Lin et al., 2003). The femoral condyles were held tightly by a clamp which was fixed to the seat; the clamp forced the femur to remain stationary during testing. The heel was placed on a cushioned table which could be positioned such that the knee was at either 20° flexion or full extension. Patellar maltracking is more pronounced between full extension and 20° flexion when the patella is not in close articulation with the trochlear grove (Sheehan et al., 2009). In addition, the patellar clamp used to track patellar motion has been previously validated to move together with the patella during knee flexion-extension between 0°–20° (Lin et al., 2003).
Figure 1.
Experimental setup for in vivo and noninvasive patellar tracking. The subject was seated with the thigh and trunk strapped to the seat and backrest. The femoral condyles were fixed from both the medial and lateral sides with a thigh clamp. Two pairs of wing nuts were tightened from the medial and lateral sides to fix the femoral condyles. Three markers were placed on the thigh (M1, M2, M3). Three markers were attached to the thigh clamp (M4–M6) with M4 placed on the knee flexion axis and lateral to the lateral epicondyle. Three markers were attached to the lower leg (M7–M9), and three were fixed to the four corners of the patellar clamp (M10–M13).
Active infrared markers were placed on a custom-designed lightweight clamp mounted on the patella (Lin et al., 2003) and on the femoral condyle clamp (fixed to the chair). Three-dimensional patellar movements relative to the femur were measured using an optoelectronic motion capture system (OPTOTRAK™ 3020, Northern Digital, Inc., Waterloo, Canada). To minimize the effect of skin movement of the thigh associated with stimulation-induced muscle contraction, patellar movement was calculated relative to the femoral condyle clamp.
Patellofemoral movements were described by joint coordinate systems (JCS) embedded in the femur and patella as previously described (Grood and Suntay, 1983; Lin et al., 2003). The patellar flexion axis was the transepicondylar line of the femur. The Y-axis was the longitudinal axis of the patella and was the axis of patellar medial/lateral tilt. The third axis, perpendicular to the above axes, characterized medial/lateral rotation of the patella, with medial rotation defined as the distal pole of the patella moving medially in frontal plane. Linear shifts of the tibia and patella relative to the femur were described by translations along the three axes of the femoral coordinate system: medial-lateral translation along the femoral X-axis, proximal-distal translation along the femoral Y-axis, and anterior-posterior translation along the femoral Z-axis; where the positive directions of motion are listed first (for a right knee). The positive directions of patellar rotation for a right knee were flexion, medial tilt, and medial rotation. The zero position of the patella was defined as the position when the local patellar coordinate system and the local femoral coordinate system were parallel. Therefore, an initial patellar orientation with respect to the femur at full extension can be described. Translations and rotations of the patella and tibia relative to the femur were calculated from the measured infrared marker coordinates in six DOFs. For left knees appropriate sign changes were made to convert translations and rotations to the right-knee conventions.
To selectively activate an individual head of the quadriceps muscle, a pair of surface electrodes was placed on the skin above the targeted muscle component (VML, VMO, and VL) and constant-current electrical stimulation was delivered through the electrodes. The approximate location of the motor point (Warfel, 1993) for each muscle was located and marked with a skin marker. Starting with a low-intensity current, a pair of electrodes with conducting gel was placed on skin at the marked location and was moved around to locate the point where stimulation induced the strongest contraction with a constant current intensity. If no contraction was successfully induced, the intensity of the current was slightly increased and the procedure was repeated until an obvious muscle contraction was achieved.
Once the motor point was located, a train of constant current stimulation pulses was used to activate the muscle at 2-second intervals. The pulse width was 0.3 msec repeated at 25 pulses per second. The pulse train duration was 600 msec. The current amplitude was adjusted for each quadriceps component so that visually observable and palpable contraction of the target muscle was elicited without significant current overflow to the surrounding muscles (monitored by palpation of the quadriceps tendon and visual inspection). To evaluate the stimulation-elicited contraction at the target muscle and current overflow to neighboring muscles, the M-wave (compound muscular action potential) was recorded for each muscle component during electrical stimulation in selected subjects. When no measurable M-wave was detected in the surrounding muscles while obvious contraction of the targeted muscle was induced, the stimulation was considered valid with negligible current overflow. Practically, a muscle had to produce visible/palpable contraction to contribute measurably to patellar tracking.
Each quadriceps component was stimulated at the motor point with the knee at full extension and at 20° of flexion, while 6 degree-of-freedom patellar tracking was simultaneously recorded. For each muscle at each knee angle, four trials were recorded and the mean value of the four trials used for further analysis. To minimize muscle fatigue, all sequential trials were separated by rest periods.
To compare patellar tracking across different subjects, the normalized direction of translation (DOT) and direction of rotation (DOR) were used to characterize the relative amplitude of the components of 3-D patellar movement as follows (Zhang et al., 1998):
| (1) |
| (2) |
where R1, R2 and R3 were rotations about the three JCS axes of the patellofemoral coordinate systems. Tx, Ty and Tz were translations, which were normalized to the knee width at the level of the femoral epicondyles for each subject, along the X, Y and Z axes of the femur, respectively.
Differences in patellofemoral kinematics between groups were analyzed for each muscle using two-way ANOVA with repeated measures (group had two levels: healthy and PFP, and knee flexion angle had two levels: 0° and 20°). If an overall significant difference was detected, the Tukey’s HSD post-hoc test was used to test for differences at specific knee flexion angles. Alpha and beta were preset to 0.05 and 0.20, respectively. The number of male and female subjects in each group was compared using the Fisher’s exact test, and subject age, height, and weight were compared between groups using the Student’s t-test.
RESULTS
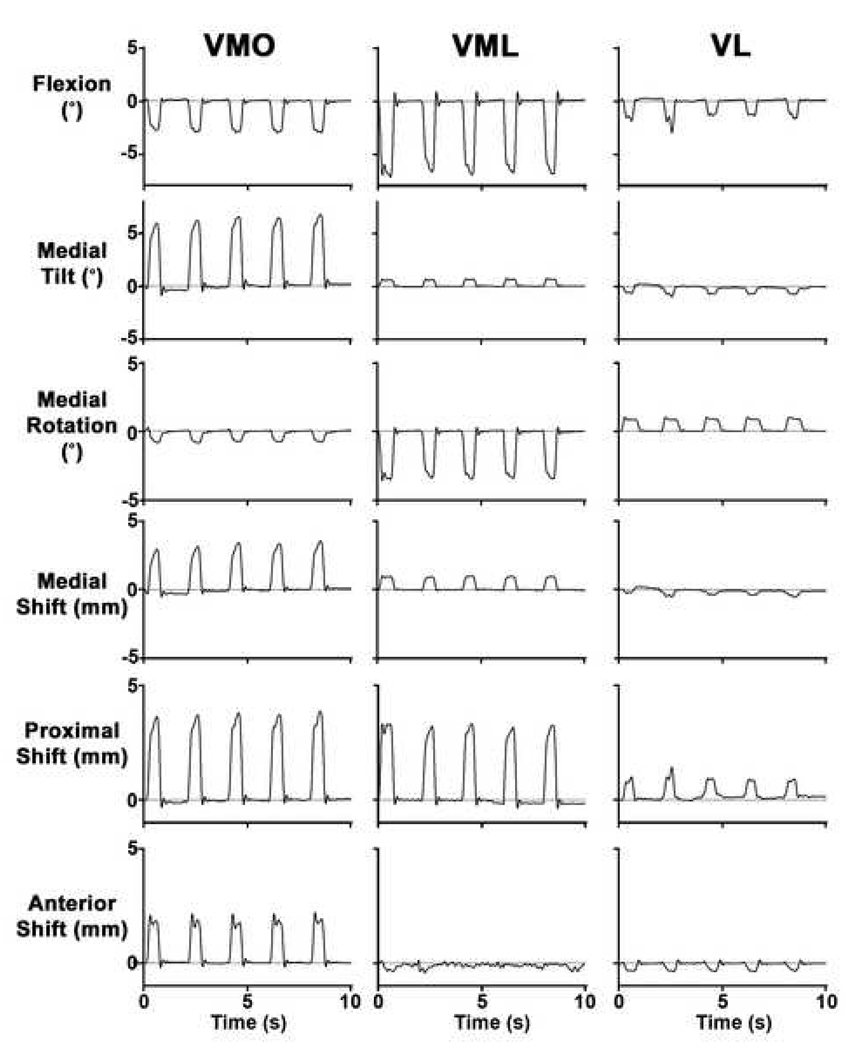
There was no obvious resistance to manual medial or lateral patellar translation for the entire PFP group, except a single subject who exhibited noticeable tightness of the lateral parapatellar structures resulting in resistance to medial patellar glide. For each subject, consistent patellar movement was induced through electrical stimulation of an individual quadriceps component (Figure 2). Typical results from healthy subjects show that selective VMO activation caused patellar extension, medial tilt, lateral rotation, and medial, proximal, and anterior translation (Figure 2). VML activation induced patellar extension, medial tilt, and lateral rotation and medial, proximal, and posterior translation. VL activation induced patellar extension, lateral tilt, medial rotation, and lateral, proximal, and posterior translation.
Figure 2.
Typical result for patellar tracking in healthy subjects induced through selective activation of individual quadriceps components with the knee at full extension, neutral tibial rotation, and neutral tibial abduction. The stimulation train (and thus the contraction) was repeated at 2-second intervals. From top to bottom, the six rows correspond to patellar flexion, medial tilt, medial rotation, medial shift, proximal shift, and anterior shift, respectively. The positive direction of each DOF is given for the ordinate. The zero position corresponded to the patellar position prior to stimulation.
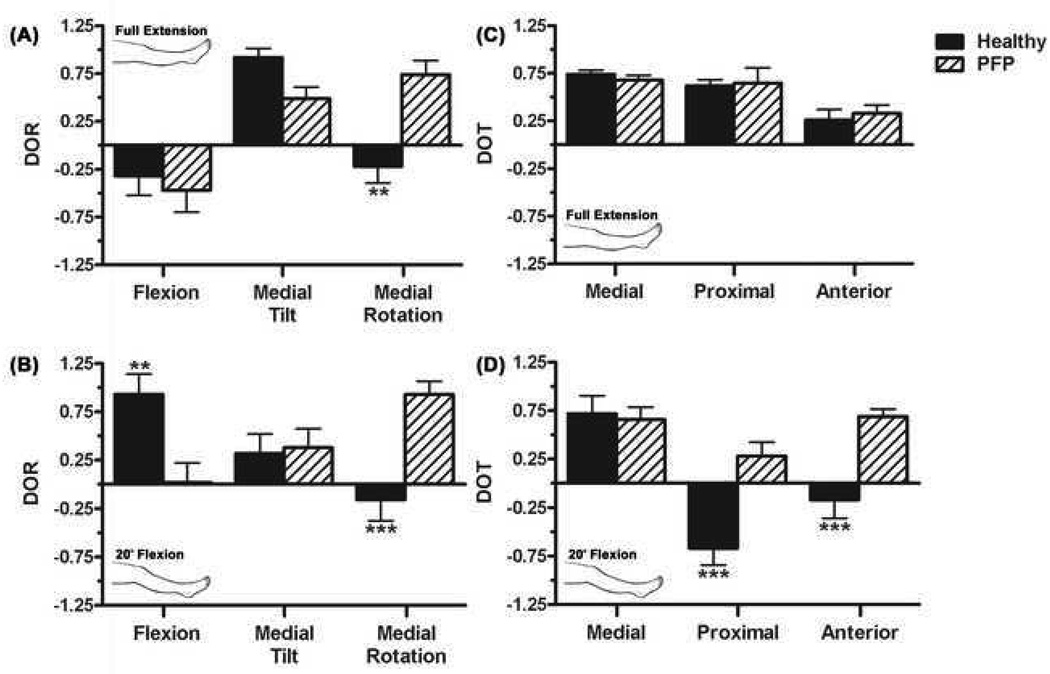
The normalized DOR and DOT varied with knee angle and varied between healthy and subjects with PFP. In healthy subjects, the primary DOR during selective VMO activation was medial tilt at full extension and patellar flexion at 20° of knee flexion (Table 2). In PFP subjects at both knee positions VMO activation caused medial patellar rotation compared to lateral rotation in healthy subjects (p<0.01, p<0.001 respectively; Figure 3). VMO activation also caused less patellar flexion in PFP subjects with the knee in 20° flexion (p<0.01). Finally, VMO activation caused proximal and anterior patellar translation in subjects with PFP compared to distal and posterior translation in healthy subjects at 20° flexion (p<0.001, p<0.001, respectively; Table 3).
Table 2.
Patellar Tracking DORs for Selective Activation of the Individual Quadriceps Components (Mean ±SD).
| 0° | 20° | ||||||
|---|---|---|---|---|---|---|---|
| Flexion | Medial Tilt | Medial Rotation |
Flexion | Medial Tilt | Medial Rotation |
||
| VMO |
PFP Healthy |
−0.47 (±0.69) | 0.49 (±0.35) | 0.74 (±0.44) ** | 0.02 (±0.60) ** | 0.38 (±0.58) | 0.93 (±0.41) *** |
| −0.32 (±0.54) | 0.92 (±0.24) | −0.22 (±0.46) | 0.93 (±0.56) | 0.32 (±0.53) | −0.16 (±0.57) | ||
| VML |
PFP Healthy |
−0.91 (±0.14) | 0.06 (±0.44) | −0.40 (±0.34) | −0.84 (±0.49) | 0.51 (±0.48) | −0.16 (±0.47) |
| −0.41 (±0.69) | 0.36 (±0.40) | −0.84 (±0.30) | −0.49 (±0.47) | 0.76 (±0.25) | −0.43 (±0.40) | ||
| VL |
PFP Healthy |
−0.71 (±0.72) | −0.51 (±0.36) | 0.48 (±0.55) | 0.30 (±0.67) | −0.82 (±0.19) | 0.49 (±0.42) |
| −0.79 (±0.26) | −0.54 (±0.36) | 0.29 (±0.50) | 0.02 (±0.43) | −0.72 (±0.49) | 0.70 (±0.59) | ||
p<0.01,
p<0.001
Figure 3.
Patellar tracking induced by selective activation of the VMO resulted in significantly more flexion, medial rotation and more anterior and proximal translation in subjects with PFP compared to healthy subjects. (A) Mean DOR for all subjects in each group with the knee in full extension. (B) Mean DOR for all subjects in each group with the knee at 20° flexion. (C) Mean DOT for all subjects in each group with the knee at full extension (D) Mean DOT for all subjects in each group with the knee at 20° flexion. Error bars represent standard error of the mean, ** p<0.01, *** p<0.001.
Table 3.
Patellar Tracking DOTs for Selective Activation of the Individual Quadriceps Components (Mean ±SD).
| 0° | 20° | ||||||
|---|---|---|---|---|---|---|---|
| Medial | Proximal | Anterior | Medial | Proximal | Anterior | ||
| VMO |
PFP Healthy |
0.68 (±0.15) | 0.65 (±0.48) | 0.33 (±0.26) | 0.66 (±0.38) | 0.28 (±0.43) *** | 0.69 (±0.23) *** |
| 0.74 (±0.12) | 0.62 (±0.17) | 0.26 (±0.29) | 0.72 (±0.49) | −0.67 (±0.46) | −0.17 (±0.50) | ||
| VML |
PFP Healthy |
0.37 (±0.30) | 0.83 (±0.14) | 0.42 (±0.33) * | 0.63 (±0.22) | 0.52 (±0.23) | 0.57 (±0.55) *** |
| 0.56 (±0.30) | 0.83 (±0.21) | −0.01 (±0.50) | 0.85 (±0.26) | 0.39 (±0.36) | −0.35 (±0.51) | ||
| VL |
PFP Healthy |
−0.71 (±0.28) | 0.69 (±0.55) | 0.17 (±0.37) | −0.68 (±0.50) *** | 0.59 (±0.49) | −0.44 (±0.56) |
| − 0.46 (±0.12) | 0.88 (±0.09) | 0.10 (±0.28) | 0.22 (±0.46) | 0.69 (±0.21) | − 0.68 (±0.29) | ||
p<0.05,
p<0.001
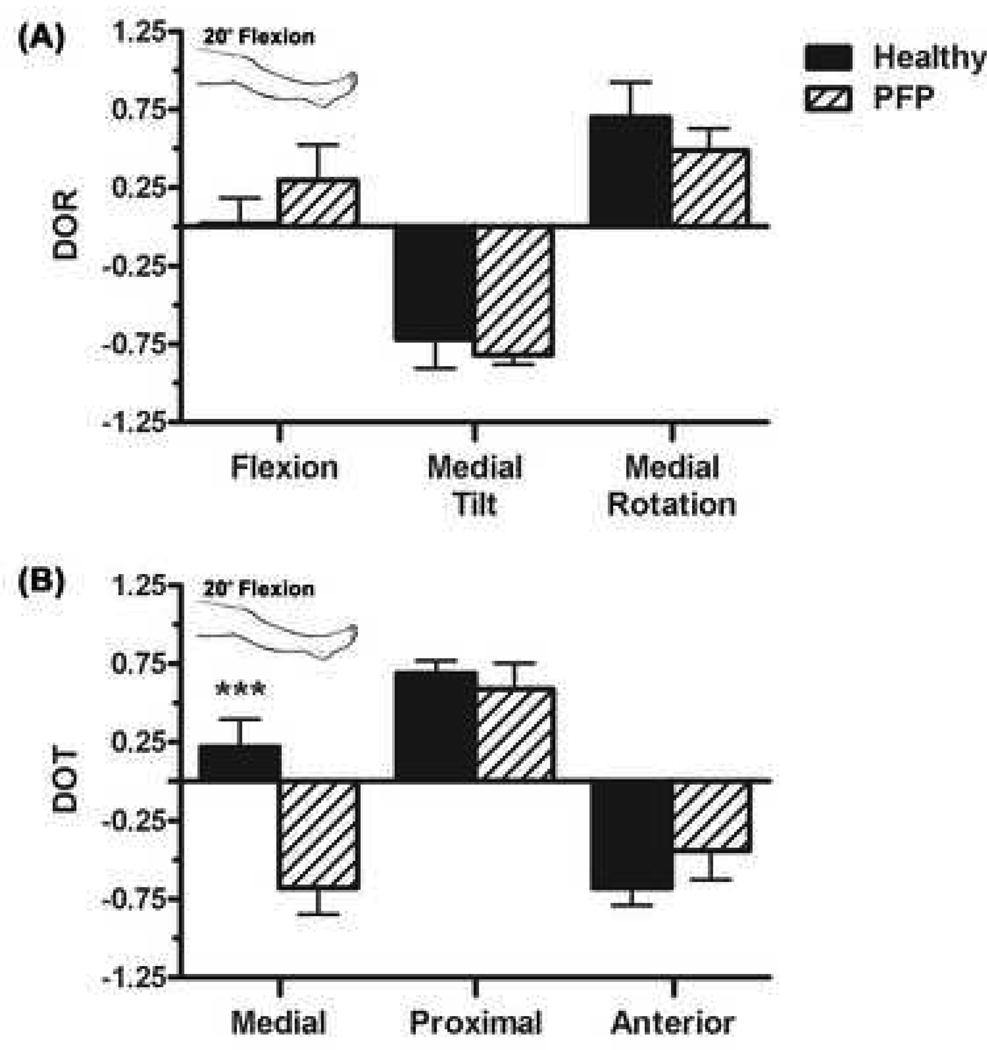
There were no significant differences in patellar rotations between healthy and subjects with PFP during VML activation (Table 2). However in subjects with PFP at both knee positions, VML activation caused anterior patellar translation compared to posterior translation in healthy subjects (p<0.05, p<0.001, respectively; Table 3). At 20° flexion, VL activation caused lateral patellar translation compared to medial patellar translation in healthy subjects (p<0.001, Figure 4B).
Figure 4.
(A) Selective activation of the VL generated less medial rotation and more lateral tilt in PFP subjects when the knee was at 20° flexion. (B) VL activation also generated lateral patellar translation in PFP subjects when the knee was at 20° flexion. Error bars represent standard error of the mean, *** p<0.001.
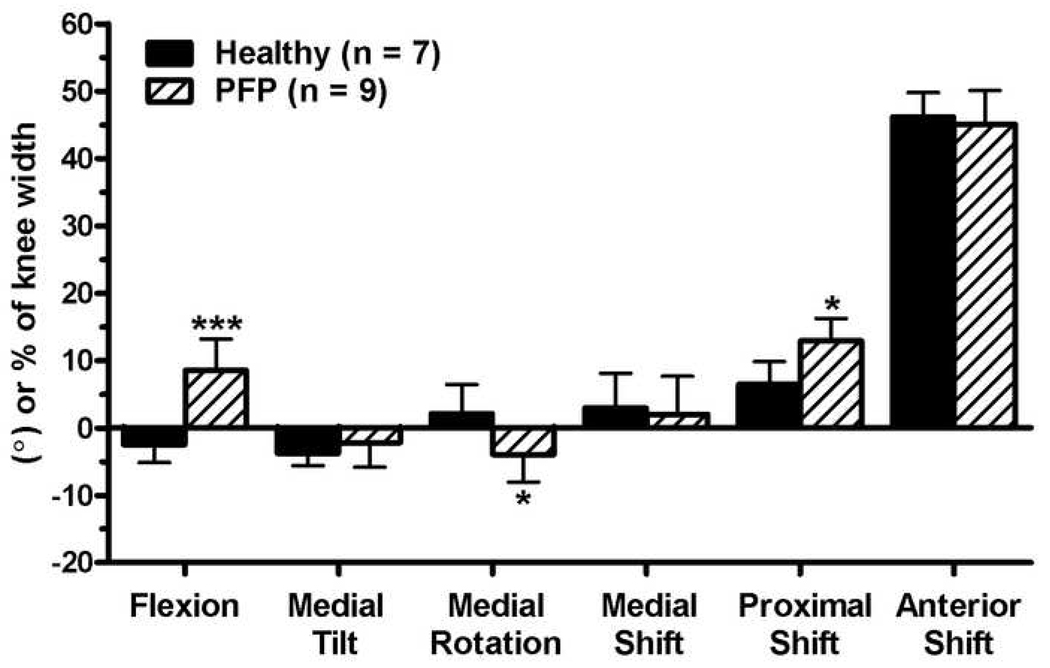
In subjects with PFP, the initial static patellar position at full extension was extended (p<0.001), more laterally rotated (p<0.05), and shifted in the proximal direction (patella alta, p<0.05) compared to healthy subjects (p<0.001, Figure 5).
Figure 5.
The mean static position of the patella at full knee extension for healthy and subjects with PFP. Error bars represent one standard deviation, * p<0.05, *** p<0.001.
DISCUSSION
It has been shown that each quadriceps component is responsible for different portions of patellar movement during knee flexion-extension (Goh et al., 1995; Heegaard et al., 1994; Lin et al., 2004; Sakai et al., 2000). The action of the VMO component has been studied extensively (Goh et al., 1995; Heegaard et al., 1994; Koh et al., 1992; Lin et al., 2004; Sakai et al., 2000; Zhang et al., 2003) because the VMO is thought to be the most important quadriceps component for preventing abnormal patellar tracking (Fulkerson, 2002; MacIntyre et al., 2006). In healthy subjects in the current study contraction of the VMO produced lateral patellar rotation. This counterintuitive finding is likely due to the specific anatomy of the obliquus portion of the vastus medialis muscle. Anatomical studies have shown that the muscle fibers of the VMO are more obliquely oriented than the fibers of the VML (Farahmand et al., 1998), and it has been shown that the tendon associated with the VMO inserts on the medial side rather than the superior edge of the patella (Holt et al., 2008). This oblique orientation and the medial location of the tendon insertion on the patella would produce medial patellar tilt and lateral rotation (inferior pole moving laterally in the frontal plane) with VMO contraction. In subjects with PFP, contraction of the VMO produced medial patellar rotation. This may be due to anatomical differences between healthy subjects and subjects with PFP (i.e. PFP subjects may have more superiorly-oriented VMO muscle fibers or a different tendon insertion site). Weakness in the oblique muscle fibers of the VMO in subjects with PFP could also contribute to this finding (Amis et al., 2006; Thomee et al., 1995; Young et al., 1987).
In the healthy knee, the presence of obliquely oriented muscle fibers and a medial tendon insertion site also explains the modulation from extension to flexion and from proximal and anterior patellar translation to distal and posterior patellar translation as the knee moves from full extension to 20°. As the patella flexes, a medially oriented (as opposed to superiorly oriented) pull would cause the patella to flex further and translate in the medial, distal, and posterior directions. This modulation of action is consistent with the hypothesis that in the healthy knee the VMO stabilizes the patella at or near terminal extension (Goh et al., 1995; Lieb and Perry, 1968).
In a recent study, Lin et al. (2004) found that VML activation produced patellar extension, medial tilt, and lateral rotation. Results from the current study show a similar patellar rotation patterns in both study populations. However, in subjects with PFP, VML activation produced anterior patellar translation compared to posterior patellar translation in healthy subjects. Posterior patellar translation in healthy subjects suggests the VML also plays a role in stabilizing the patella during knee flexion by causing the patella to have a more firm articulation with the trochlear groove. The decrease in posterior stabilization force from the medial quadriceps components may suggest the presence of moment arm dysfunction (i.e. the line of action of the medial quadriceps muscle is altered in subjects with PFP syndrome) (Wilson and Sheehan, 2009).
In healthy subjects, VL activation produced lateral patellar translation at full extension and medial patellar translation at 20° flexion. At 20° of knee flexion the patella begins to articulate with the trochlear groove and VL contraction causes the patella to have a firm articulation with the trochlear groove. The proximal portion of the trochlear groove is oriented medially, and tends to guide the patella medially, so an increased articulation with the groove will cause a medial shift as the patella slides into the groove. These results are further supported by a recent in vivo study which found that in healthy subjects the patella translated laterally during the first 15° of knee flexion, but after 15° medial patellar translation occurred throughout the range of knee flexion during squatting (Wilson et al., 2009). In the current study, VL activation produced lateral patellar translation at both knee positions in subjects with PFP. Similarly, the aforementioned study found consistent lateral patellar translation throughout knee flexion in subjects with PFP (Wilson et al., 2009).
Excess lateral patellar translation in subjects with PFP syndrome has been shown in numerous previous studies (Brossmann et al., 1993; MacIntyre et al., 2006; Powers, 2000; Wilson et al., 2009) and it is commonly thought to be related to medial quadriceps weakness. Weakness of the VMO quadriceps component may cause the extensor mechanism to be incapable of generating effective forces in opposition to the action of the VL. Ineffective opposition of the force from the VL may lead to an imbalance in the extensor mechanism and overloading of the lateral compartment of the patellofemoral joint, which may ultimately lead to pain (Fulkerson, 1997). Since patellar tracking is also affected by other factors such as the shape of the trochlear groove and the pattern of the joint contact, tracking patterns found in this study cannot be fully explained by the action of the quadriceps muscles.
A limitation of this study is the relatively small sample size as the sample was limited to unilateral limbs from only female subjects in our larger PFP patient population. VL activation caused trends toward increased lateral tilt and decreased medial rotation in subjects with PFP compared to healthy subjects, which did not achieve statistical significance, likely due to power considerations. However, inclusion of a homogeneous, non-paired population was deemed a more important consideration as the lack of significance for these two trends did not substantially impact the findings of this study. Due to the limited sample size caution must be taken when extrapolating findings from this study to a larger population.
In conclusion, this study provides an in vivo and noninvasive tool to characterize 3-D patellar tracking induced by individual quadriceps components in PFP. Results suggest that in healthy subjects the mechanical actions of some of the quadriceps are actively modulated with knee flexion angle. However, this modulation of action was not demonstrated in subjects with PFP. Lack of active modulation may result in decreased patellar stabilization during knee flexion leading to abnormal patellar tracking. In addition, the 3-D mechanical action of the VL is altered in subjects with PFP, which may lead to increased lateral patellar translation. Excess lateral patellar translation in PFP syndrome may be related to VMO weakness which may cause ineffective forces in opposition to the action of the VL.
ACKNOWLEDGEMENTS
We would like to acknowledge the support of National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CONFLICT OF INTEREST
The authors report no conflicts of interest associated with this study.
References
- Amis AA, Senavongse W, Bull AM. Patellofemoral kinematics during knee flexion-extension: an in vitro study. Journal of Orthopaedic Research. 2006;24:2201–2211. doi: 10.1002/jor.20268. [DOI] [PubMed] [Google Scholar]
- Brossmann J, Muhle C, Schroder C, Melchert UH, Bull CC, Spielmann RP, Heller M. Patellar tracking patterns during active and passive knee extension: evaluation with motion-triggered cine MR imaging. Radiology. 1993;187:205–212. doi: 10.1148/radiology.187.1.8451415. [DOI] [PubMed] [Google Scholar]
- Csintalan RP, Schulz MM, Woo J, McMahon PJ, Lee TQ. Gender differences in patellofemoral joint biomechanics. Clinical Orthopaedics and Related Research. 2002:260–269. doi: 10.1097/00003086-200209000-00026. [DOI] [PubMed] [Google Scholar]
- Devereaux MD, Lachmann SM. Patello-femoral arthralgia in athletes attending a Sports Injury Clinic. British Journal of Sports Medicine. 1984;18:18–21. doi: 10.1136/bjsm.18.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dye SF. The pathophysiology of patellofemoral pain: a tissue homeostasis perspective. Clinical Orthopaedics and Related Research. 2005;436:100–110. doi: 10.1097/01.blo.0000172303.74414.7d. [DOI] [PubMed] [Google Scholar]
- Farahmand F, Senavongse W, Amis AA. Quantitative study of the quadriceps muscles and trochlear groove geometry related to instability of the patellofemoral joint. Journal of Orthopaedic Research. 1998;16:136–143. doi: 10.1002/jor.1100160123. [DOI] [PubMed] [Google Scholar]
- Fitzgerald GK, McClure PW. Reliability of measurements obtained with four tests for patellofemoral alignment. Physical Therapy. 1995;75:84–90. doi: 10.1093/ptj/75.2.84. [DOI] [PubMed] [Google Scholar]
- Fulkerson JP. Disorders of the patellofemoral joint. Williams & Wilkins: Baltimore; 1997. [Google Scholar]
- Fulkerson JP. Diagnosis and treatment of patients with patellofemoral pain. American Journal of Sports Medicine. 2002;30:447–456. doi: 10.1177/03635465020300032501. [DOI] [PubMed] [Google Scholar]
- Goh JC, Lee PY, Bose K. A cadaver study of the function of the oblique part of vastus medialis. Journal of Bone and Joint Surgery [Br] 1995;77:225–231. [PubMed] [Google Scholar]
- Grelsamer RP, Stein DA. Rotational Malalignment of the Patella. In: Fulkerson JP, editor. Common Patellofemoral Problems. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2005. pp. 19–28. [Google Scholar]
- Grood ES, Suntay WJ. A Joint Coordinate System for the Clinical Description of 3-Dimensional Motions - Application to the Knee. Journal of Biomechanical Engineering-Transactions of the Asme. 1983;105:136–144. doi: 10.1115/1.3138397. [DOI] [PubMed] [Google Scholar]
- Guzzanti V, Gigante A, Dilazzaro A, Fabbriciani C. Patellofemoral Malalignment in Adolescents - Computerized Tomographic Assessment with Or Without Quadriceps Contraction. American Journal of Sports Medicine. 1994;22:55–60. doi: 10.1177/036354659402200110. [DOI] [PubMed] [Google Scholar]
- Heegaard J, Leyvraz P, Vankampen A, Rakotomanana L, Rubin PJ, Blankevoort L. Influence of Soft Structures on Patellar 3-Dimensional Tracking. Clinical Orthopaedics and Related Research. 1994;299:235–243. [PubMed] [Google Scholar]
- Hirokawa S. Effects of Variation on Extensor Elements and Operative Procedures in Patellofemoral Disorders. Journal of Biomechanics. 1992;25:1393–1401. doi: 10.1016/0021-9290(92)90053-4. [DOI] [PubMed] [Google Scholar]
- Holt G, Nunn T, Allen RA, Forrester AW, Gregori A. Variation of the vastus medialis obliquus insertion and its relevance to minimally invasive total knee arthroplasty. Journal of Arthroplasty. 2008;23:600–604. doi: 10.1016/j.arth.2007.05.053. [DOI] [PubMed] [Google Scholar]
- Insall JN. Foreword. In: Scuderi GR, editor. The Patella. New York: Springer-Verlag; 1995. [Google Scholar]
- Koh TJ, Grabiner MD, Deswart RJ. In vivo Tracking of the Human Patella. Journal of Biomechanics. 1992;25:637. doi: 10.1016/0021-9290(92)90105-a. [DOI] [PubMed] [Google Scholar]
- Koskinen SK, Kujala UM. Patellofemoral Relationships and Distal Insertion of the Vastus Medialis Muscle - A Magnetic-Resonance-Imaging Study in Nonsymptomatic Subjects and in Patients with Patellar Dislocation. Arthroscopy. 1992;8:465–468. doi: 10.1016/0749-8063(92)90009-z. [DOI] [PubMed] [Google Scholar]
- Lieb FJ, Perry J. Quadriceps Function - An Anatomical and Mechanical Study Using Amputated Limbs. Journal of Bone and Joint Surgery [Am] A. 1968;50:1535. [PubMed] [Google Scholar]
- Lin F, Makhsous M, Chang AH, Hendrix RW, Zhang LQ. In vivo and noninvasive six degrees of freedom patellar tracking during voluntary knee movement. Clinical Biomechanics. 2003;18:401–409. doi: 10.1016/s0268-0033(03)00050-0. [DOI] [PubMed] [Google Scholar]
- Lin F, Wang GZ, Koh J, Hendrix RW, Zhang LQ. In vivo and noninvasive three-dimensional patellar tracking induced by individual heads of quadriceps. Medicine and Science in Sports and Exercise. 2004;36:93–101. doi: 10.1249/01.MSS.0000106260.45656.CC. [DOI] [PubMed] [Google Scholar]
- MacIntyre NJ, Hill NA, Fellows RA, Ellis RE, Wilson DR. Patellofemoral joint kinematics in individuals with and without patellofemoral pain syndrome. Journal of Bone and Joint Surgery [Am] 2006;88:2596–2605. doi: 10.2106/JBJS.E.00674. [DOI] [PubMed] [Google Scholar]
- McNally EG, Ostlere SJ, Pal C, Phillips A, Reid H, Dodd C. Assessment of patellar maltracking using combined static and dynamic MRI. European Radiology. 2000;10:1051–1055. doi: 10.1007/s003300000358. [DOI] [PubMed] [Google Scholar]
- Powers CM. Patellar kinematics, part I: the influence of vastus muscle activity in subjects with and without patellofemoral pain. Physical Therapy. 2000;80:956–964. [PubMed] [Google Scholar]
- Powers CM, Ward SR, Chan LD, Chen YJ, Terk MR. The effect of bracing on patella alignment and patellofemoral joint contact area. Medicine and Science in Sports and Exercise. 2004;36:1226–1232. doi: 10.1249/01.mss.0000132376.50984.27. [DOI] [PubMed] [Google Scholar]
- Sakai N, Luo ZP, Rand JA, An KN. The influence of weakness in the vastus medialis oblique muscle on the patellofemoral joint: an in vitro biomechanical study. Clinical Biomechanics. 2000;15:335–339. doi: 10.1016/s0268-0033(99)00089-3. [DOI] [PubMed] [Google Scholar]
- Schepsis AA, Watson FJ. Patellofemoral Arthritis with Malalignment. In: Fulkerson J, editor. Common Patellofemoral Problems. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2005. [Google Scholar]
- Sheehan FT, Derasari A, Brindle TJ, Alter KE. Understanding patellofemoral pain with maltracking in the presence of joint laxity: complete 3D in vivo patellofemoral and tibiofemoral kinematics. Journal of Orthopaedic Research. 2009;27:561–570. doi: 10.1002/jor.20783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomee R, Renstrom P, Karlsson J, Grimby G. Patellofemoral pain syndrome in young women. II. Muscle function in patients and healthy controls. Scandinavian Journal of Medicine & Science in Sports. 1995;5:245–251. [PubMed] [Google Scholar]
- Warfel JH. The Extremities: Muscles and Motor Points. Baltimore: Williams & Wilkins; 1993. [Google Scholar]
- Wilson NA, Press JM, Koh JL, Hendrix RW, Zhang L. In Vivo Noninvasive Evaluation of Abnormal Patellar Tracking During Squatting in Patients with Patellofemoral Pain. Journal of Bone and Joint Surgery [Am] 2009;91:558–566. doi: 10.2106/JBJS.G.00572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson NA, Sheehan FT. Dynamic in vivo 3-dimensional moment arms of the individual quadriceps components. Journal of Biomechanics. 2009;42:1891–1897. doi: 10.1016/j.jbiomech.2009.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young A, Stokes M, Iles JF. Effects of Joint Pathology on Muscle. Clinical Orthopaedics and Related Research. 1987;219:21–27. [PubMed] [Google Scholar]
- Zhang L, Butler J, Nishida T, Nuber G, Huang H, Rymer WZ. In vivo determination of the direction of rotation and moment-angle relationship of individual elbow muscles. Journal of Biomechanical Engineering-Transactions of the ASME. 1998;120:625–633. doi: 10.1115/1.2834754. [DOI] [PubMed] [Google Scholar]
- Zhang LQ, Wang GZ, Nuber GW, Press JM, Koh JL. In vivo load sharing among the quadriceps components. Journal of Orthopaedic Research. 2003;21:565–571. doi: 10.1016/S0736-0266(02)00196-1. [DOI] [PubMed] [Google Scholar]