Abstract
Introduction
The study aimed to quantify the preferences of young physicians for different attributes relevant to practice establishment in Germany.
Methods
Qualitative in-depth interviews of 22 physicians were conducted to identify relevant practice attributes. Based on this information, a questionnaire was developed containing a discrete choice experiment comprised of a “best–worst scaling” (BWS) task. It was mailed to a representative sample of 14,939 young physicians who were close to making a decision regarding practice establishment. Regression analysis was used to estimate utility weights quantifying physicians' preferences for practice attributes.
Results
Qualitative interviews identified six attributes: “professional cooperation,”“income,”“career opportunities of the partner,”“availability of child care,”“leisure activities,” and “on-call duties.” For the BWS task, 5,026 returned questionnaires were analyzed. Results indicated that a change in income led to the largest utility change compared with changes in other attributes. Additional net income to compensate the disutility of a rural practice as compared with an urban practice was 9,044€/months (U.S.$ 11,938). Yet, nonmonetary attributes such as on-site availability of childcare and fewer on-call duties would decrease the additional income required to compensate the disutility of a rural practice.
Discussion
The results offer quantifiable information about young physicians' preferences in establishing a practice. It can assist health policy makers in developing tailored incentive-based interventions addressing urban–rural inequalities in physician coverage.
Keywords: Physician shortage, stated preferences, discrete choice experiment
In Germany the looming shortage of physicians has been an important health policy issue in recent years. The German Federal Medical Association (GFMA), the joint association of the 17 state chambers of physicians in Germany, reports residents in some rural areas—particularly in eastern Germany—to be considered medically underserved (Kopetsch 2006). The GFMA expects a rising physician shortage, since 19 percent of the practicing physicians will retire within 5 years, and some study results show fewer medical school graduates intending to work in clinical medicine (Rieser 2005; Gensch 2007; Kopetsch 2008;). Several studies describe physicians' job satisfaction as presumably a key factor influencing remaining in the medical workforce. For example, “the level of remuneration,”“the general workload,”“the extent of administrative work,”“the collaboration with colleagues,”“the balance of work and family,”“the extent of responsibility in the decision making process,” and “continuing education” seem to impact job satisfaction (Gensch 2007; Janus et al. 2007, 2008; Laubach and Fischbeck 2007; Brähler, Alfermann, and Stiller 2008).
Concerning the physician shortage's effect on health care, the Association of Health Insurance Physicians (AHIP) of the federal state of Saxony-Anhalt, a less densely populated state in Eastern Germany, described rural areas with five general practitioners per 10,000 inhabitants, with 33 percent aged 60 or above (Kassenärztliche Vereinigung Sachsen-Anhalt 2009). Another indicator of limited health care access is waiting time for consultations, with up to 33 days on average in some rural areas of Eastern Germany compared with 12 days in urban areas of Berlin (Betriebskrankenkassen Ost 2008). Particularly in Eastern Germany the state AHIPs reported that patients' traveling distances for medical care and the use of nonphysician services like nurse practitioners has increased. In conclusion, the AHIPs have questioned whether ambulatory care can be secured in the future. Yet studies about whether, for example, nurse practitioners are a cost-effective alternative to physicians for treating simpler medical conditions and how much such nonphysician services affect the quality of care are still missing.
In contrast to these indications of physician shortage, the Organization for Economic Cooperation and Development (OECD) reported the total number of physicians per capita in Germany increased in the last years, averaging 3.4 practicing physicians per 1,000 population, compared with a 3.0 average in OECD countries (Simoens and Hurst 2004). Considering this, one could assume that the problem of physician shortage in Germany is not necessarily due to a lack of physicians in general but to an unequal distribution (Klose, Uhlemann, and Gutschmidt 2003; Simoens and Hurst 2004;). This means physicians tend to practice in urban or affluent rural areas, whereas other areas have difficulties attracting enough physicians to provide high-quality health care to the residents. This “maldistribution” of physicians is perceived in many countries, including the United States, the United Kingdom, Australia, and Canada (Joyce, McNeil, and Stoelwinder 2004; Rosenthal, Zaslavsky, and Newhouse 2005; Robertson et al. 2007;).
In Germany health policy makers have addressed the “maldistribution” of physicians with many interventions, tending to improve the diffusion of physicians either by regulation or by incentive-based programs. Monetary incentive-based programs were implemented, including improved remuneration plans or the donation of seed capital for practice establishment. Little evidence in the literature favors the long-term success of such programs (Sempowski 2004), and health policy makers are thinking about programs focusing more on physician life-style concerns, for example, the number of on-call duties. To date very few studies have explored the role of monetary and nonmonetary attributes in practice establishment. The present study aimed to provide information for health policy makers about the importance of different attributes and their combinations related to practice establishment.
METHODS
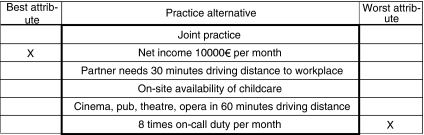
The study used a preference-based approach to derive information about attributes relevant for practice establishment: in a hypothetical scenario a practice alternative is described by several attributes at different levels, and respondents choose the most and the least preferred attributes at a respective level (see Figure 1). This choice task is repeated according to an experimental design plan for a set of practice alternatives and is called “best worst scaling” (BWS) (Finn and Louviere 1992; Flynn et al. 2007;).
Figure 1.
Example of a Best–Worst Scaling (BWS) Task
BWS belongs to the discrete choice experiments (DCE) applied to measure preferences in health care issues, like estimation of patient benefit in health technology assessment, analysis of patient or professional decision making, and developing prioritization frameworks (Ryan et al. 2001). Preferences derived from BWS tasks have strong roots in economic theory and design of experiments and have the advantage of giving preference information on the attribute's impact (attribute utility weight) and on its levels (level scale utility weight) (Flynn et al. 2007). This quantification informs about how the attributes and their levels are related to each other. For health policy makers, “level scale utility weights” are often more interesting—they illustrate implications of policy decisions by quantifying changes from one level to the other. Attribute utility weights indicate the impact of the attribute itself, but since attributes do not change across decision scenarios, their policy relevance is rather limited. Since all estimated level scale utilities lie on a common scale, marginal rates of substitution (MRS) can be calculated (Flynn et al. 2007). The MRS describe the rates for respondents willingly giving up one attribute in exchange for another, and the present study uses them to describe the relation of nonmonetary attributes to a monetary attribute. Thus, MRS provide health policy makers with information about the utility of different attributes and their combinations to develop tailored incentive-based programs.
The present study involved the following steps: (1) identifying a set of attributes relevant to the establishment of a practice, (2) generating the BWS task using an experimental design plan, (3) determining the sampling procedure, and (4) estimating the utility of the attributes and their respective levels.
Identifying the Attributes
Attributes relevant to the establishment of a practice were identified, described and labeled to ensure the BWS task encompassed the most relevant attributes by executing a qualitative study interviewing 22 physician in-depth. All physicians were randomly selected at two university hospital campuses, one in Eastern Germany (Leipzig) and the other in Western Germany (Münster). The interviewed physicians had not yet established a practice but intended to. Briefly, the qualitative process identifying relevant attributes was a multistep funnel-shaped process. At first a brainstorming task was conducted, collecting all potentially relevant attributes. In the following process the number of attributes was reduced stepwise based on interviewees' attitudes concerning the relevance of practice establishment. This was achieved with the repertory grid technique (Fransella, Bell, and Bannister 2004) and the laddering technique (Gutman and Reynolds 1988) during the in-depth interviews; both techniques helped the interviewee distinguish between attributes concerning relevance to establish a practice. In addition to the attributes, interviewed physicians determined discrete observable levels in sufficient detail, allowing to distinguish in the BWS task between attributes related more to a rural practice or to an urban practice. In the last step, all attributes and their levels were evaluated by two established physicians, selected at the authors' convenience, to be realistic concerning development of policy (Coast and Horrocks 2007).
Experimental Design
The number of attributes and their levels identified during the qualitative process determined the total set of possible practice alternatives. Using the complete set, that is a full factorial design, the number of choices required from each respondent soon becomes enormous as the number of attributes and/or levels increases. To minimize respondents' burdens, an orthogonal main effects plan (OMEP) was used, reducing the number of practice alternatives shown in the experiment (Burgess and Street 1994). The appropriate experimental design plan was developed with the software SAS and the macro Mktex. The final questionnaire had 24 different practice alternatives, allowing estimation of all main effects of the attributes and their levels (Flynn et al. 2007). Using the BWS task utility, weights of the attributes and their respective levels were estimated.
Sampling Procedure
With databases of five state chambers of physicians, we identified physicians who had not yet established their own practice. Since this information was not directly specified in the database, all physicians with (1) no completed training in any specialty and (2) younger than 40 years were sampled. The first sample criterion was based on specialization as a prerequisite for licensing by the AHIP when establishing a practice. Consequently, this criterion ensured that sampled physicians had not yet established an AHIP-licensed practice. The second criterion was chosen because most physicians not completing specialty training by age 40 never do so, mainly because specialization is not required for their work, for example, in industry or health service administration. Thus, both criteria should ensure that the survey went only to physicians likely to face a future decision on practice establishment.
Fourteen thousand nine hundred and thirty-nine questionnaires were mailed to 4,689 physicians from the state chamber of Lower Saxony, 3,287 physicians from the state chamber of Saxony, 3,212 physicians from Westphalia-Lippe, 1,887 physicians from Mecklenburg Western Pomeranian, and 1,864 physicians from Saxony-Anhalt. All samples were full samples except for Westphalia-Lippe, which consisted of a random subsample of all 4,812 identified physicians. With Westphalia-Lippe and Lower Saxony, two chambers of Western Germany and with Saxony, Saxony-Anhalt, Mecklenburg Western Pomeranian three chambers of Eastern Germany participated in the study. Within the context of the study, one should know the struggle of the Eastern German economy since unification in 1989, and large subsidies still go from west to east mainly to support the infrastructure policy.
The present study based sample size calculation on a simulation study (Flynn et al. 2007). Considering that further subgroup analysis stratified by sociodemographic characteristics in each state chamber would be performed, each subgroup should have at least 150 physicians to achieve an R2 of 0.95 in the regression analysis of up to eight attributes. A questionnaire pretest was conducted with 15 physicians not already having their own practice. These were selected at the authors' convenience; all physicians were completing training for speciality at the University of Leipzig. Questionnaires were sent out in August 2007; a reminder followed after 14 days.
Statistical Analysis
As suggested by Flynn (Flynn et al. 2007), inferences about the utility scale based on the BWS tasks were made with the “paired model approach,” aggregating the choice frequencies of all possible best–worst pairs at a sample level followed by an adjustment eliminating sampling zeros. According to the experimental design plan, the levels of attributes with fewer levels appeared more often in the BWS task than in attributes with more levels. This influences the probability of a particular best–worst pair being chosen (Flynn et al. 2007). Therefore, the frequency of choosing a best–worst pair was adjusted by its availability in the BWS task.
The utility weights of the attributes and their levels were estimated by weighted least square regression. The weights used in regression analysis were the frequencies of the choice totals adjusted to eliminate zeros. Since the natural log of the frequency of a best–worst pair chosen is a linear function of the difference in utilities, the dependent variable (cf) in the regression model was represented by the logarithm of the adjusted choice frequencies. The explanatory variables were formed by a set of dummy-coded variables representing the weight of attributes (AT1–AT6) and a set of effect-coded variables representing the level scale utilities of the attributes (AT1_level1–AT6_level4). Formally, the regression model is described by
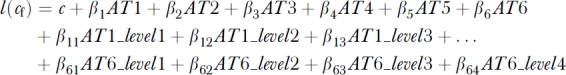 |
The regression model shows the simple difference in the number of best/worst frequencies explained by two different components, the attribute utility weights and the level scale utility weights (Lanscar, Louviere, and Flynn 2007). Assuming a linear range span by all levels, MRS in terms of income resulted as follows: the range in β of the level scale utility of the attribute income was adjusted by the range of its scale unit (Δβ/Δ€). The same was done for all other attributes of interest. Finally, the latter was divided by the former, giving the respective MRS. They are used to describe the relation of nonmonetary attributes to a monetary attribute.
Following the BWS task, physicians were asked for their attitude towards each attribute concerning the decision to establish a practice. This was done with Likert items ranging from 1, reflecting “no impact at all,” to 5, reflecting “very high impact” on the decision to establish a practice. This study focused on the information of the Likert item “income,” regressed by an ordinary least square regression model on several sociodemographic characteristics (“gender,”“having children,”“having a partner,” and “grown up in a rural/urban area”). The regression analysis aimed to identify a subgroup of physicians differing in their attitude in such a way that monetary aspects are most important to them. This step was required, since BWS data were aggregated at a sample level and, therefore, it was not possible to incorporate individual covariates in the BWS regression model.
All calculations were preformed by using the software STATA 10.2 (STATA Corp., College Station, TE, USA).
RESULTS
Qualitative Study
Fifty-four percent of the interviewed physicians were female and the group mean age was 33.4 [standard deviation (SD)=2.5]. About 41 percent grew up in an urban area and about 91 percent of respondents intended to establish a practice, in about 4 years on average.
Briefly, the analysis of the in-depth interviews revealed the following concepts relevant to the establishment of a practice: professional cooperation, income, family, leisure, and workload. In detail, the interviewed physicians stated feeling a lack of experience in conducting a practice, both in urban and in rural areas. The possibility to reassure diagnostic decisions in the treatment of patients was also very important. Additionally, almost all interviewed physicians were concerned about the economic risks related to the financial investment of practice establishment. The attribute “professional cooperation” addressed these concerns with different types of practices reflecting the level of cooperation.
The qualitative analysis identified “income” as a significant attribute influencing the decision to establish a practice. Here, income was the monthly net income after tax in Euro (1€=U.S.$1.32). The lowest level reflected the average income of a young physician working as an assistant in hospital. The highest level reflected an above-average income compared with a typical general practitioner in Germany (Statistisches Bundesamt 2003).
Issues about the “career opportunities of the partner” and the “availability of child care” were considered important in most interviews with particular focus on establishing a practice in rural areas. Interviewed physicians stated that the partner's workplace or child care should not be far from practice location. Ideally, the workplace of the partner or the child care should be on-site, it should never be further than 60 minutes driving time. Briefly, physicians tended to combine aspects of private life with professional life, for example, interviewed physicians viewed the choice of practice location against the background of childcare availability, since it is seen as an advantage to pick up the children directly after work.
Although interviewed physicians mentioned different “leisure activities,” for example, theatre, opera, cinema, or restaurants, most agreed that “leisure activities” should ideally be located on-site; they should not be further away than 60 minutes driving time.
The workload expressed by the amount of “on-call duty” was still an important issue through most interviews. The amount of “on-call duty” stated by the interviewed physicians ranged from two to eight per month. The interviewed physicians viewed more than eight times of “on-call duty” per month as a very heavy workload. The workload attributed to administration had an apparently minor role, since most interviewed physicians see administration today as a usual part of a practice.
Table 1 shows the final set of attributes and their levels used for the BWS task.
Table 1.
Attributes and Their Levels Developed in the Qualitative Study for Use in the Best–Worst-Scaling (BWS) Task
| Attributes | Levels | Description of the Level |
|---|---|---|
| Professional cooperation | 0 | Individual practice |
| 1 | Joint practice | |
| 2 | Individual practice in a medical center | |
| Income (net after tax) | 0 | 2,500€ (U.S.$3,30)* |
| 1 | 5,000€ (U.S.$6,600) | |
| 2 | 7,500€ (U.S.$9,900) | |
| 3 | 10,000€ (U.S.$13,200) | |
| Career opportunities for the partner | 0 | On-site |
| 1 | 30 minutes driving distance | |
| 2 | 60 minutes driving distance | |
| Availability of childcare | 0 | On-site |
| 1 | 30 minutes bus ride | |
| 2 | 60 minutes bus ride | |
| Leisure activities | 0 | On-site |
| 1 | 30 minutes driving distance | |
| 2 | 60 minutes driving distance | |
| On-call duty | 0 | 2 on-call times per month |
| 1 | 4 on-call times per month | |
| 2 | 6 on-call times per month | |
| 3 | 8 on-call times per month |
1€=U.S.$1.32.
Quantitative Study
Of 14,939 mailed questionnaires, 5,381 were returned—a response rate of 36 percent. Only complete BWS tasks were chosen for the analysis. Thus, 5,026 physicians provided sufficient data for analyzing the BWS task. The mean age of the respondents was 31 (SD=3.3), and about 60 percent were female. The same proportion was married or had a long-standing relationship, and 36 percent of respondents had at least one child. Most respondents grew up in an urban area (60 percent) and were living in Western Germany (55 percent). At survey time almost all responding physicians were practicing medicine (93 percent). About 53 percent of the respondents stated the intention to establish a practice, in about 6 years time on average.
Sociodemographic information on nonresponders was not available. Comparing the responders' age and gender with data registered by the state chambers of physicians showed no considerable differences, implying that the respondents seemed to be representative concerning age and gender, according to the study population.
Regression analysis of sociodemographic characteristics on the Likert item “income” showed income was significantly more important to male physicians without children and without a partner having grown up in an urban area. The explanatory power of the regression model was R2=0.23. The data of this subgroup and the total sample were used in the analysis of the BWS task.
Table 2 shows BWS results from the regression analysis describing the attribute utility weights for the two samples. The explanatory power of the regression model was R2=0.84. The attribute with the greatest utility weight relative to the reference category “on-call duty” was the attribute “income.” This attribute showed the highest utility weight in the total sample and in the subgroup compared with the remaining attributes. Although the attribute utility weights differed in detail, the rank order of all attributes was similar in the two samples.
Table 2.
Results of Weighted Least Square Regression Estimating Attribute Utility Weights of the Total Sample (n=5,026) and of the Subgroup† (n=409)
| Full Sample | Subgroup | |
|---|---|---|
| β [95%-CI] | β [95%-CI] | |
| Professional cooperation | 1.530* [1.396; 1.664] | 1.178* [1.028; 1.328] |
| Income | 1.586* [1.488; 1.683] | 1.247* [1.144; 1.349] |
| Career opportunities of the partner | 0.521* [0.394; 0.649] | 0.469* [0.330; 0.609] |
| Availability of child care | 0.227* [0.139; 0.314] | 0.277* [0.171; 0.383] |
| Leisure activities | 0.845* [0.722; 0.967] | 0.542* [0.421; 0.663] |
| On-call duty‡ | — | — |
p<.05.
Male physicians without children, living without partner, and grown up in urban area.
Reference category.
95%-CI, 95%-confidence interval.
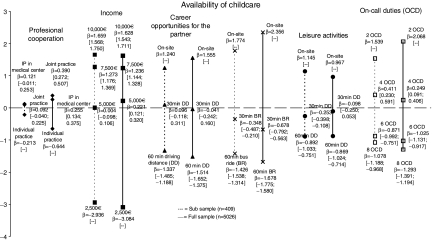
Figure 2 shows utility weights from the same analysis concerning the levels of each attribute. These level scale utilities reveal information on the most beneficial changes when establishing a practice. The results indicated that a change in income from 2,500€ (U.S.$3,300) to 10,000€ (U.S.$13,200) would produce a larger utility than, for example, a change in availability of leisure activities from 60 minutes driving time to on-site. The range of level scale utility for “income” was largest, followed by “availability of childcare,” and “on-call duty.” Level scale utility weights for “professional cooperation” showed a small range, although the attribute utility weight indicated its importance. This means that the change in levels of “professional cooperation” produces only a small change in the overall utility of the practice alternative. Comparing the total sample results with the subgroup, level scale utility weights of income were similar in both samples, although regression analysis of the sociodemographic characteristics on the Likert item “income” showed the impact of income higher in the subgroup.
Figure 2.
Results of Weighted Least Square Regression Estimating Level Scale Utility Weights for the Attributes in the Full Sample (n=5,026) and in the Subgroup of Male Physicians without Children, Living without Partner, and Grown up in an Urban Area (n=409). The Vertical Axis Describes the Level Scale Utility Weights on the Common Scale. (10,000€=U.S.$13,200, 7,500€=U.S.$9,900, 5,000€=U.S.$6,600, 2,500€=U.S.$3,300; 1€=U.S.$1.32; BR, Bus Ride; DD, Driving Distance; IP, Individual Practice; OCD, On-Call Duties)
The level scale utility weight of 2,500€ (U.S.$3,300) income was associated with the largest negative utility, whereas the level scale utility of on-site availability of childcare was associated with the largest positive utility. The practice with lowest level scale utility weights for all attribute produced an overall utility of −9.1, whereas the practice with the highest level scale utility weights for all attributes produced an overall utility of 9.0. In the subgroup, the respective overall utility ranged from −7.9 to 7.4. In both samples, a practice where childcare is <30 minutes bus ride away, the partner's work and leisure activities are <30 minutes driving time away, the number of on-call services is less than four per month, and the net income is above 5,000€ (U.S.$6,600) per month is generally associated with a positive utility.
Calculated MRS for the total sample for income showed that, for example, one on-call service was associated with an additional income of 892€ (U.S.$1,177), or 1-minute bus ride to childcare was associated with an additional income of 109€ (U.S.$144). The corresponding MRS for the subgroup were 712€ (U.S.$940) and 88€ (U.S.$116), respectively. Table 3 shows further MRS for income for the total sample and the subgroup.
Table 3.
Marginal Rates of Substitution (MRS) with Respect to Income for the Full Sample (n=5,026) and Subgroup* (n=409)
| Substituted by Income |
||
|---|---|---|
| Attribute | Full Sample | Subgroup |
| Professional cooperation | —† | —† |
| Career opportunities for the partner | 83€ (U.S.$110)‡ per minute driving time to workplace | 71€ (U.S.$94) per minute driving time to workplace |
| Availability of childcare | 109€ (U.S.$144) per minute bus ride to childcare | 88€ (U.S.$116) per minute bus ride to childcare |
| Leisure activities | 50€ (U.S.$66) per minute driving time to leisure activity | 56€ (U.S.$74) per minute driving time to leisure activity |
| On-call duty | 892€ (U.S.$1,177) per on-call duty | 712€ (U.S.$940) per on-call duty |
Male physicians without children, living without partner, and grown up in urban area.
No substitution since attribute is nominal scaled.
1€=U.S.$1.32.
Considering a change from a rather typical practice in an urban area—usually an individual practice with 5,000€ (U.S.$6,600) income, two times of on-call duty, on-site career opportunities for the partner, on-site availability of childcare, and on-site leisure activities—to a typical practice in rural areas—differing in two supplementary on-call duty times and 30 minutes driving time to workplace for the partner, leisure activities, and childcare—the additional income compensating this change was 9,044€ (U.S.$11,938) for the total sample and 7,874€ (U.S.$10,394) for the subgroup.
DISCUSSION
This study quantified the utility of monetary and nonmonetary attributes for establishing a practice. The BWS task results showed the utility of a practice alternative primarily associated with a large change in level scale utility weights of some attributes. For example, income was the attribute with the largest change in level scale utility weights to young physicians, and a change in monthly net income from 2,500€ (U.S.$3,300) to 10,000€ (U.S.$13,200) provides the largest single increase in utility to young physicians. A monthly net income of 2,500€ (U.S.$3,300) is associated with the lowest utility value of all. Indeed, the MRS of the remaining attributes to income showed a considerable rise in income necessary to compensate the disadvantage in utility of a practice characterized by attributes related to typical rural areas. Yet young physicians associated the change to on-site availability of childcare or to two on-call duties per month with a high utility value, even higher than a monthly net income of 10,000€ (U.S.$13,200). From a health policy maker's perspective, future programs should also focus on nonmonetary incentives, like a move to closer childcare or to a lower number of on-call duties. Both attributes also showed a large range in level scale utility weights with a high absolute value in utility at the best level. In real life some attributes like on-site availability of childcare are hard to change, but its substantial impact on the establishment of a practice should be considered in health policy discussions, particularly in Germany with its increasing number of young female physicians (Kassenärztliche Bundesvereinigung 2007).
From a health policy maker's perspective, it is important to identify certain subgroups of physicians differing considerably in their preferences in such a way that they are more susceptible to attributes related to a practice in rural areas. For example, studies indicate that physicians who grew up in a rural area tend to practice in a rural area more than their urban counterparts and that female physicians differ in choosing the best and the worst attribute (Owen et al. 2007). Incorporating person-specific covariates into the BWS regression analysis makes analyzing such research questions easier. Unfortunately, this study analyzed data on aggregated sample level, meaning person-specific covariates could not be included into the regression model. Instead, we analyzed the preferences of a subgroup identified by regressing sociodemographic characteristics on the Likert item “income.” This approach to identify subgroups showed rather low explanatory power in terms of potential differences in preferences. Future research should be on methods to analyze BWS data on respondent level, enabling it to incorporate person-specific covariates directly into the BWS regression model to show physicians needed to deliver care in rural areas.
Published DCE analyzing the preferences of already established general practitioners in the United Kingdom on practice and job characteristics show that high income, workload, list size of patients, the use of guidelines, professional cooperation, and the social status of the patients play an important role (Scott and Shiell 1997; Scott, Watson, and Ross 2003; Wordsworth et al. 2004;). Some of these attributes were also important in the present study. This suggests that various DCE methods lead to similar results. Yet the impact of monetary attributes compared with nonmonetary attributes tended to be smaller in the studies already published. But a systematic comparison with the present study in terms of the impact of income concerning nonmonetary attributes is difficult, since studies differ considerably in design, and the published DCE did not explicitly discriminate between the impact of “attribute utility weight” and “level scale utility weight” on preferences (Flynn et al. 2007).
There were some limitations related to the study. The BWS task was based on the attributes and their corresponding levels identified in the qualitative part of the study. Yet one cannot know whether other qualitative approaches produce the same six attributes and their levels, as identified by the four-step iterative process. Indeed, how closely the identified attributes are “truly” related to establishing a practice needs further research. Comparative qualitative approaches identifying attributes and levels for the same study would be important for determining the significance of the attributes found. Yet all attributes derived in the qualitative part of the study were conceptually similar with the factors related to job satisfaction found in literature. Moreover, the attributes explained a significant part of the respondent's preferences for establishing a practice possibly supporting the quantitative results in terms of their validity for health policy makers.
Literature reports that the range in levels impact the estimation of the utility (Verlegh, Schifferstein, and Wittink 2002), meaning the magnitude of utility is associated with the width of level range. Summed up, it is recommended to use realistic attribute level ranges and to be cautious when estimating utility of out-ranged levels. The present study identified attributes, and levels were verified by two established physicians as realistic. Data analysis showed that the attribute “income” indicated a diminishing marginal utility. This implies that the levels of income were well defined.
In conclusion, the preference structure of both the complete sample and the subgroup suggests that one needs considerably high monetary incentives to improve the diffusion of physicians. Health policy makers should also act on optimal availability of childcare and very few on-call duties. In view of several federal states in the United States stepping up programs on incentive-based recruitment of physicians in rural areas, this study provides information about the potential role of monetary and nonmonetary incentives in such programs. However, since preferences of young physicians may differ from country to country, transferability of the results to U.S. settings may be limited. For example, in the U.S. relevant practice attributes and/or their levels may be different due to the country's huge geographic dimension. Practice establishment in rural areas may be associated with enormous distances that could separate the physician from family and friends. This could also result in very long driving time to reach schools, leisure activities, retail shops and limit career opportunities for the partner. Furthermore, regional differences in climate and population ethnicity may be relevant in the United States. Studies improving our understanding about the role of monetary and nonmonetary incentives should be encouraged, also taking into account other attributes than those identified in the present study.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This study was funded by the German Medical Association (Bundesärztekammer, grant no. 06-16).
Disclosures: None.
Disclaimers: None.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
REFERENCES
- Betriebskrankenkassen Ost. “Pressearchiv 06/2008” [accessed on August 5, 2009]. Available at http://www.bkk-ost.de/index.php?id=1393&von=Jun.+2006&bis=Jun.+2009&land=Landesverband+Ost.
- Brähler E, Alfermann D, Stiller J. Karriereentwicklung und berufliche Belastung im Arztberuf. Göttingen: Vandenhoeck & Ruprecht; 2008. [Google Scholar]
- Burgess LB, Street D. Algorithms for Constructing Orthogonal Main Effect Plans. Utilitas Mathematica. 1994;46:33–48. [Google Scholar]
- Coast J, Horrocks S. Developing Attributes and Levels for Discrete Choice Experiments Using Qualitative Methods. Journal of Health Services Research & Policy. 2007;12(1):25–30. doi: 10.1258/135581907779497602. [DOI] [PubMed] [Google Scholar]
- Finn A, Louviere JJ. Determining the Appropriate Response to Evidence of Public Concern: The Case of Food Safety. Journal of Public Policy and Marketing. 1992;11(1):12–25. [Google Scholar]
- Flynn TN, Louviere JJ, Peters TJ, Coast J. Best-Worst Scaling: What It Can Do for Health Care Research and How to Do It. Journal of Health Economics. 2007;26(1):171–89. doi: 10.1016/j.jhealeco.2006.04.002. [DOI] [PubMed] [Google Scholar]
- Fransella F, Bell R, Bannister D. A Manual for Repertory Grid Technique. 2nd Edition. Chichester, England: John Wiley & Sons; 2004. [Google Scholar]
- Gensch K. Veränderte Berufsentscheidung junger Ärzte und mögliche Konsequenzen für das zukünftige ärztliche Versorgungsangebot. Ergebnisse einer anonymen Befragung. Gesundheitswesen. 2007;69(6):359–70. doi: 10.1055/s-2007-981677. [DOI] [PubMed] [Google Scholar]
- Gutman J, Reynolds TJ. Laddering Theory, Method, Analysis and Interpretation. Journal of Advertising. 1988;28(1):11–31. [Google Scholar]
- Janus K, Amelung VE, Baker LC, Gaitanides M, Schwartz FW, Rundall TG. Job Satisfaction and Motivation among Physicians in Academic Medical Centers: Insights from a Cross-National Study. Journal of Health Politics, Policy and Law. 2008;33(6):1133–67. doi: 10.1215/03616878-2008-035. [DOI] [PubMed] [Google Scholar]
- Janus K, Amelung VE, Gaitanides M, Schwartz FW. German Physicians “On Strike”—Shedding Light on the Roots of Physician Dissatisfaction. Health Policy. 2007;82(3):357–65. doi: 10.1016/j.healthpol.2006.11.003. [DOI] [PubMed] [Google Scholar]
- Joyce CM, McNeil JJ, Stoelwinder JU. Time for a New Approach to Medical Workforce Planning. Medical Journal of Australia. 2004;180(7):343–6. doi: 10.5694/j.1326-5377.2004.tb05972.x. [DOI] [PubMed] [Google Scholar]
- Kassenärztliche Bundesvereinigung, 2007 [accessed on February 3, 2009]. Available at http://www.kbv.de/presse/7479.html.
- Kassenärztliche Vereinigung Sachsen-Anhalt [accessed on February 3, 2009]. Available at http://online.kvsa.braincms.de/media/artikel/medien_1/05f5bd49725723e28cbd494c56289fc2.pdf.
- Klose J, Uhlemann T, Gutschmidt S. Ärztemangel –Ärzteschwemme. Auswirkungen der Altersstruktur von Ärzten auf die vertragsärztliche Versorgung. Bonn: Wissenschaftliches Institut der AOK; 2003. [Google Scholar]
- Kopetsch T. Bundesärztekammer-Statistik: Ärztemangel trotz Zuwachsraten. Deutsches Ärzteblatt. 2006;103:A-588. [Google Scholar]
- Kopetsch T. Entwicklung der Arztzahlen: Zahl der angestellten Ärzte im ambulanten Bereich steigt. Deutsches Ärzteblatt. 2008;208:A-985. [Google Scholar]
- Laubach W, Fischbeck S. Job Satisfaction and the Work Situation of Physicians: A Survey at a German University Hospital. International Journal of Public Health. 2007;52(1):54–59. doi: 10.1007/s00038-006-5021-x. [DOI] [PubMed] [Google Scholar]
- Lanscar E, Louviere JJ, Flynn TN. Several Methods to Investigate Relative Attribute Impact in Stated Preference Experiments. Social Science and Medicine. 2007;64(8):1738–53. doi: 10.1016/j.socscimed.2006.12.007. [DOI] [PubMed] [Google Scholar]
- Owen JA, Conaway MR, Bailey BA, Hayden GF. Predicting Rural Practice Using Different Definitions to Classify Medical School Applicants as Having a Rural Upbringing. Journal of Rural Health. 2007;23(2):133–40. doi: 10.1111/j.1748-0361.2007.00080.x. [DOI] [PubMed] [Google Scholar]
- Rieser S. Ärztemangel: Arbeitsbedingungen Schrecken Viele ab. Deutsches Ärzteblatt. 2005;102:797. [Google Scholar]
- Robertson JE, Jr., Boyd J, Hedges JR, Keenan EJ. Strategies for Increasing the Physician Workforce: The Oregon Model for Expansion. Academic Medicine. 2007;82(12):1158–62. doi: 10.1097/ACM.0b013e318159cf7e. [DOI] [PubMed] [Google Scholar]
- Rosenthal MB, Zaslavsky A, Newhouse JP. The Geographic Distribution of Physicians Revisited. Health Services Research. 2005;40(6):1931–52. doi: 10.1111/j.1475-6773.2005.00440.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan M, Scott DA, Reeves C, Bate A, van Teijlingen ER, Russell EM, Napper M, Robb CM. Eliciting Public Preferences for Healthcare: A Systematic Review of Techniques. Health Technology Assessment. 2001;5(5):1–186. doi: 10.3310/hta5050. [DOI] [PubMed] [Google Scholar]
- Scott A, Shiell A. Do Fee Descriptors Influence Treatment Choices in General Practice? A Multilevel Discrete Choice Model. Journal of Health Economics. 1997;16(3):323–42. doi: 10.1016/s0167-6296(96)00520-6. [DOI] [PubMed] [Google Scholar]
- Scott A, Watson MS, Ross S. Eliciting Preferences of the Community for Out of Hours Care Provided by General Practitioners: A Stated Preference Discrete Choice Experiment. Social Science and Medicine. 2003;56(4):803–14. doi: 10.1016/s0277-9536(02)00079-5. [DOI] [PubMed] [Google Scholar]
- Sempowski IP. Effectiveness of Financial Incentives in Exchange for Rural and Underserved Area Return-of-Service Commitments: Systematic Review of the Literature. Canadian Journal of Rural Medicine. 2004;9(2):82–8. [PubMed] [Google Scholar]
- Simoens S, Hurst J. Towards High-Performing Health Systems. Policy Studies. Paris: Organization for Economic Cooperation and Development; 2004. Matching Supply and Demand for the Services of Physicians and Nurses; pp. 167–206. [Google Scholar]
- Statistisches Bundesamt. Kostenstruktur Arztpraxen, Fachserie 2 [accessed on August 5, 2009]. Available at https://www-ec.destatis.de/csp/shop/sfg/bpm.html.cms.cBroker.cls?cmspath=struktur,vollanzeige.csp&ID=1018854.
- Verlegh PWJ, Schifferstein HNJ, Wittink DR. Range and Number-of-Levels Effects in Derived and Stated Measures of Attribute Importance. Marketing Letters. 2002;13(1):41–52. [Google Scholar]
- Wordsworth S, Skatun D, Scott A, French F. Preferences for General Practice Jobs: A Survey of Principals and Sessional GPs. British Journal of General Practice. 2004;54(507):740–6. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.