Abstract
A temporomandibular disorder (TMD) is a very common problem affecting up to 33% of individuals within their lifetime. TMD is often viewed as a repetitive motion disorder of the masticatory structures and has many similarities to musculoskeletal disorders of other parts of the body. Treatment often involves similar principles as other regions as well. However, patients with TMD and concurrent cervical pain exhibit a complex symptomatic behavior that is more challenging than isolated TMD symptoms. Although routinely managed by medical and dental practitioners, TMD may be more effectively cared for when physical therapists are involved in the treatment process. Hence, a listing of situations when practitioners should consider referring TMD patients to a physical therapist can be provided to the practitioners in each physical therapist's region. This paper should assist physical therapists with evaluating, treating, insurance billing, and obtaining referrals for TMD patients.
KEYWORDS: Dentistry, Physical Therapy, Temporomandibular Disorders, Temporomandibular Joint
Atemporomandibular disorder (TMD) is a musculoskeletal disorder within the masticatory system. Many practitioners refer to TMD as a single disorder in spite of the fact that patients have various sub-diagnoses (e.g., myofascial pain, temporomandibular joint (TMJ) inflammation)1,2. TMD is a prevalent disorder most commonly observed in individuals between the ages of 20 and 40. Approximately 33% of the population has at least one TMD symptom and 3.6% to 7% of the population has TMD with sufficient severity to cause them to seek treatment1–3.
TMD is often viewed as a repetitive motion disorder of the masticatory structures. It has many similarities to musculoskeletal disorders of other parts of the body, and therapeutic approaches for other musculoskeletal disorders generally apply to this disorder as well1,2,4. Similar to other repetitive motion disorders, TMD self-management instructions routinely encourage patients to rest their masticatory muscles by voluntarily limiting their use, i.e., avoiding hard or chewy foods and restraining from activities that overuse the masticatory muscles (e.g., oral habits, clenching teeth, holding tension in the masticatory muscles, chewing gum, and yawning wide)1,2,5. The self-management instructions also encourage awareness and elimination of parafunctional habits (e.g., changing teeth clenching habit to lightly resting the tongue on top of the mouth or wherever the tongue is most comfortable) and keeping the teeth apart and masticatory muscles relaxed1,2,5.
As with other musculoskeletal disorders, pain during function and/or at rest is the primary reason patients seek treatment, and reduction in pain is generally the primary goal of therapy1,2. Less commonly, individuals seek TMD therapy for TMJ catching or locking, masticatory stiffness, limited mandibular range of motion, TMJ dislocation, and unexplained change in their occlusion (anterior or posterior open bite, or shift in their mandibular midline). However, TMJ noises are common among the general population, are generally not a concern for individuals or practitioners, are not commonly treated, and do not generally respond as well to therapy as pain1,2,6–9. The purpose of this clinical perspective is to describe the examination and treatment of TMD from both a dentist's and a physical therapist's perspective.
Dentist's TMD Examination
TMD pain is generally located in the masseter muscle, preauricular area, and/ or anterior temporalis muscle regions. The quality of this pain is generally an ache, pressure, and/or dull pain and may include a background burning sensation. There may also be episodes of sharp pain, and when the pain worsens, the primary pain quality may become a throbbing sensation. Patients with TMD tend to report that their pain is intensified by events such as stress, clenching, and eating, while it is relieved by relaxing, applying heat to the painful area, and taking over-the-counter analgesics1,4,5,10.
As practitioners obtain a patient's pain history, they must be alert for unusual pain locations, pain qualities, pain-aggravating and pain-relieving events, and other factors (e.g., unexplained fever) suggestive of disorders that may mimic TMD symptoms (e.g., infection, giant cell arteritis, meningitis, etc.)2,5. Practitioners must also inquire about other diseases or symptoms that may negatively impact the patient's response to the practitioner's therapies. For instance, studies suggest that TMD patients with cervical or widespread pain will not obtain the same degree of improvement as other TMD patients who do not have these pains11–13. Thus, practitioners may desire to refer these patients for treatment of these disorders. For example, the patient may be referred to a physical therapist primarily for treatment of the cervical region, but additionally for supplementary therapy for the masticatory region2,14.
A thorough physical examination entails evaluating the mandibular range of motion (Figure 1); the minimum of normal is a 40 mm opening, 7 mm to the right and to the left movements, and a 6 mm protrusive movement2,5,15. If the patient has a restricted opening, the practitioner may be able to determine its origin by stretching the mouth wider. This is usually performed by placing the index finger over the incisal edges of the mandibular incisors and the thumb over the incisal edges of the maxillary incisors and pressing the teeth apart by moving the fingers in a scissor-type motion2. The patient will usually feel tightness or pain at the location of the restriction, and the patient is asked to point to this location. The location is confirmed by the practitioner palpating that location2.
FIGURE 1.

Measuring the opening mandibular range of motion.
In the thorough physical exam, the practitioner will also intensify or reproduce the patient's masticatory pain and then rule out structures outside the masticatory region as sources of the pain1,2,16. It is recommended that the masseter and anterior temporalis muscles (Figure 2) and the TMJs (Figure 3) be palpated to ensure that this intensifies or reproduces the patient's pain and to determine whether the primary pain source is muscle or TMJ1,2,14,17,18. It is also recommended that the thyroid, carotid arteries, and suboccipital and postural musculature be palpated to determine whether they cause or contribute to the pain complaint; if they do, a referral may be indicated2,17,18.
FIGURE 2.

Palpating the anterior temporalis muscles.
FIGURE 3.

Palpating the temporomandibular joints.
If the patient's pain was not intensified or reproduced with the palpatory examination, the practitioner may more intensely palpate the previously palpated structures, may locate and palpate the myofascial trigger points within the previous structures, or may attempt to reproduce the patient's pain from different locations19–21. The decision varies with the practitioner's suspicions and clinical experience. Figure 4 provides maps of palpation locations that have been shown to generate referred pain to the labeled anatomical areas of the head and face. Referred pain patterns tend to be consistent from patient to patient, so readers may find these maps beneficial for any patient with head or face pain when the true source of the patient's pain has not been identified19–21.
FIGURE 4.
Locations responsible for producing referred pain to the different regions of the head.*
*The superficial sites that have caused referred pain to the labeled regions of the head are highlighted on the drawing and the intraoral palpation locations are listed below the drawing.
When evaluating a patient for pain, first evaluate for local causes. For example, if an individual has ear pain, it is best if he or she is evaluated by a physician to determine if there is a local cause for this pain2,19,21. Similarly, it is common for dentists to receive a referral for patients with ear pain where a physician has ruled out a local cause for the pain (e.g., ear infection) and the physician suspects TMD16,19.
Studies confirm that about one-third of these patients have ear pain that is referred from TMD, one-third have pain that is referred from a cervical spine disorder (CSD), and one-third have pain referred from both TMD and CSD22,23. To determine the source(s), Figure 1 can be used to identify the locations to palpate that have been shown to cause ear pain. Based upon the identified tenderness and the ease of the various palpated structures in intensifying or reproducing the ear pain, the practitioner can more easily determine whether it would be most cost-effective to provide this patient with TMD therapy, refer the patient to a physical therapist for CSD therapy, or recommend both therapies2.
Another example of identifying the source of referred pain is a patient who complains of forehead pain when local structures (e.g., sinuses) have been ruled out as the cause of this pain. Practitioners may want to palpate the structures that have been found to commonly refer pain to the forehead (Figure 4). If palpation of cervical muscles reproduces the patient's forehead pain, this suggests that the cervical musculature could cause or contribute to this pain and it is generally worthwhile to conservatively treat (e.g., through physical therapy) the cervical musculature and see if this provides satisfactory relief of the forehead pain2.
As part of the clinical exam, it is recommended that dental practitioners visually perform an intraoral screening, evaluating for evidence of pathology, such as swelling, cavities, deflection of the soft palate when saying “ah,” etc. The patient's history will often have alerted the practitioner to oral disorders that may be causing or contributing to the symptoms and which may indicate that additional radiographs or tests are needed. Generally, only a screening radiograph, such as a panoramic radiograph, is needed in the evaluation of the majority of TMD patients2,5,17,18.
To varying degrees, practitioners are able to identify contributing factors that appear to be perpetuating the TMD symptoms and the magnitude to which they are contributing to the symptoms. Examples of commonly identified TMD perpetuating factors are nighttime parafunctional habits, gum chewing, daytime clenching, holding tension in the masticatory muscles, neck pain, excessive caffeine consumption, stress, tension, aggravations, frustrations, depression, poor sleep, poor posture, and widespread pain. It is recommended that the contributing factors that are the easiest to change and that are speculated to provide the greatest impact on the symptoms be initially changed1,2,4,17,24.
Management Protocol
Many therapies have been advocated for treating TMD, and many health professionals have found that they are able to help patients improve TMD symptoms. The practitioner managing the patient's therapy should decide which therapies are most cost-effective and evidence-based, and which have the greatest potential to provide the patient with long-term symptom relief. The most cost-effective therapies are the TMD self-management therapies, specifically when use is continuous and adhered to1,2,24.
A therapy that is commonly provided by dentists is an occlusal orthotic, also called a dental or occlusal appliance or a splint (see Figure 5). The appliance can be made to cover the occlusal surfaces of maxillary or mandibular teeth and can be fabricated from many different materials, giving it a hard, soft, or intermediate feel. It is generally preferred that the appliance be worn only at night and possibly a few hours during the day when the patient has not yet broken the habit of heavy clenching activity (e.g., while driving a car). It is rare for patients to be willing to wear the orthotic in public because it generally interferes with speech and is somewhat unattractive1,2,5,17,25.
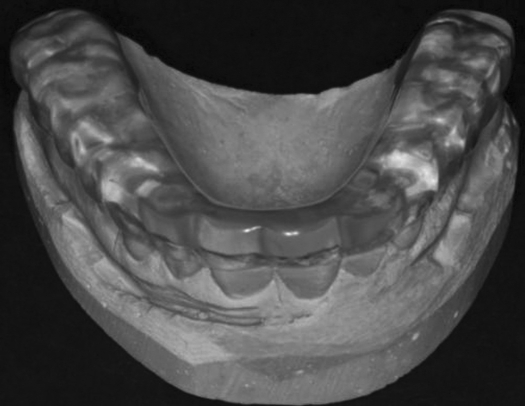
FIGURE 5.
An occlusal orthotic on a cast of the patient's teeth.
Occlusal orthotics are beneficial for masticatory muscle pain, TMJ pain, TMJ noises, restricted jaw mobility, and TMJ dislocation1,2,5,25. If the appliance is worn at night, it has its most dramatic effect on the TMD symptoms that patients have upon awaking. Therefore, an occlusal orthotic can be fabricated primarily to relieve symptoms in patients who have TMD symptoms on waking1,3,5,26,27. It is our impression that if a patient's pain is limited to the masticatory system and the patient has minimal psychosocial contributors, we can satisfactorily reduce the symptoms without referral. If the patient has a CSD that is worthy of treatment, he or she should usually be referred to a physical therapist for treatment2,14.
The dentist author has, to date, recommended a physical therapy referral for approximately 50% of his TMD patients28. He would generally like the physical therapist to treat the cervical component and help resolve the masticatory component1,2,5,12. The situations in which it is recommended that practitioners consider referring TMD patients to a physical therapist are listed in Table 1. Conversely, there are situations in which it is recommended that physical therapists consider referring a TMD patient to a dentist (Table 2). For example, if a TMD patient is waking with TMD pain, this suggests nocturnal factors are contributing to the symptoms. If stomach sleeping has been corrected or ruled out, it is recommended that the patient be provided with an occlusal orthotic to decrease pain on waking1,3,26,27.
TABLE 1.
Situations when it is recommended that dental practitioners consider referring TMD patients to a physical therapist.
| Mechanism | Situation |
|---|---|
| Cervical | The patient has neck pain worthy of treatment. |
| The patient has cervicogenic headaches (headaches that can be reproduced by palpating the neck). | |
| Postural | The patient has moderate to severe forward head posture; a study suggests these patients may obtain significant TMD symptom improvement from posture exercises in combination with TMD self-management instructions. |
| The patient's TMD symptoms increase with abnormal postural activities. | |
| The patient desires help in changing poor sleep posture (e.g., stomach sleeping). | |
| Outcome-Oriented | The patient did not obtain adequate TMD symptom relief from initial therapies that did not include physical therapy. |
| The patient is to have TMJ surgery; patients who receive physical therapy after TMJ surgery may have significantly better results. It is appropriate for these patients to be referred for physical therapy prior to surgery in order that they may learn about and possibly start the postsurgical exercises, schedule the recommended postsurgical appointments, and receive prior authorization from their insurance carrier. |
TABLE 2.
Situations when it is recommended that physical therapy practioners refer TMD patients to a dentist and appropriate treatment mechanisms.
| Time Factor | Event | Treatment |
|---|---|---|
| Nocturnal | The patient awakes with TMD pain. |
|
| Daytime | The patient has symptoms associated with tooth-related pain such as:
|
Comprehensive dental examination and treatment. |
Patients who have tooth pain generally also have facial pain5,29. As with other referred pains, patients occasionally perceive the site of their pain as the source of the referred pain and attempt to have the site treated rather than the source5. Consequently, a physical therapist may target treatment for TMD when the true pain source is actually a tooth. Some situations that suggest that a tooth, rather than TMD, is the source of the patient's pain include the patient relating that 1) the pain occurs or intensifies upon drinking hot or cold beverages, 2) throbbing pain occurs spontaneously, or 3) throbbing pain wakes him or her up from sleep (there can be other causes for this symptom, e.g., neck pain). In about 3% of the patients referred to the dentist author for “TMD,” after thorough examination, a tooth is found to be the true source of the pain. The tooth may need to receive root canal therapy or to be extracted5,16,30.
Treatment Approaches for TMD
There are several theories on best therapies for TMD. None of these theories is perfect, but the one that appears to best target the various patients and their contributing factors correlates treatment strategies with patients' daily variations in symptoms31,32. For example, some TMD patients awake with TMD pain that only last minutes to hours, suggesting that nocturnal factors are the primary contributors to these symptoms2,3,5,26,27. Other TMD patients awake symptom-free and their TMD symptoms develop later in the day, suggesting that daytime factors are the primary contributors to these symptoms (e.g., daytime muscle tensing or clenching habits). TMD patients in a third group may report that they awake with TMD pain that never goes away, suggesting that both nocturnal and daytime factors are contributing to their symptoms. In this third patient group, patients generally report that either their awaking or daytime symptoms are worse, suggesting that the nocturnal or daytime factors are more significantly contributing to their symptoms2,5,31,32.
Therapies shown to be beneficial for TMD symptoms that patients awake with are provided in Table 2. Therapies shown to be beneficial for daytime TMD symptoms are provided in Table 3. There are also therapies that appear beneficial for both awaking and daytime TMD symptoms; they are provided in Table 4. Some TMD therapies are not listed because the authors do not routinely use them; these methods have no demonstrated evidence within the literature or there is inconsistent clinical sense for their effect on symptom patterns2,5,10.
For a patient who awakes with TMD symptoms, decide which therapies in Tables 2 and 4 have the greatest potential to provide the most cost-effective, long-term symptom relief. For a patient who awakes symptom-free and the TMD symptoms develop later in the day, similarly consider therapies in Tables 3 and 4. For a patient who awakes with symptoms and has them throughout the day, consider all the therapies (Tables 2, 3, and 4), keeping in mind the predominant category2.
TABLE 4.
Therapies that appear beneficial for both awaking and daytime TMD symptoms.
| Orientation | Treatment |
|---|---|
| Medicative | Prescribing NSAIDs and/or steroids. |
| Passive Approach | Performing physiotherapy modalities (heat, ice, ultrasound, iontophoresis, etc.). |
| Performing jaw-stretching exercises. | |
| Active Approach | Performing head and neck posture improvement exercises. |
| Indirect Approach | Performing cervical therapies (manual techniques, neuromuscular re-education, etc.). |
TABLE 3.
Therapies that have been shown to be beneficial for daytime TMD symptoms.
| Orientation | Treatment |
|---|---|
| Relaxation/Stress Management |
|
| Orthotic |
|
| Medicative |
|
Some treatment effects generally carry over to the other portion of the day, so patients who have mild daytime pain may find that nocturnal wear of occlusal orthotic provides satisfactory symptom relief.
It is recommended that these therapies be modulated with the symptom severity, anticipated compliance, abilities of providers (dentist, physical therapist, psychologist, etc.), impact on the patient's lifestyle (for both symptoms and treatments), and cost (in terms of price, time, adverse sequelae, etc.). It is recommended that the least invasive procedures be used first and if this adequately resolves the pain, no other treatment is needed. It is appropriate for patients to wear an occlusal orthotic at night for as long as it is beneficial1,2.
Additionally, consider non-TMD disorders that may negatively impact the patient's TMD symptoms, such as neck pain, widespread pain, rheumatic disorders, sinus pain, poor sleep, and depression. Failure to obtain adequate improvement of these non-TMD contributors decreases the probability of patients achieving satisfactory TMD symptom improvement1,2. A significant number of TMD patients have a cervical component contributing to or perpetuating the TMD symptoms.
Surgery is rarely needed for TMD patients. One study that tracked over 2,000 TMD patients from many practices found that only 2.5% underwent TMJ surgery (1.4% arthrocentesis, 1.0% arthroscopy, and 0.1% open joint procedures)33. Other than for the obvious reasons (e.g., infection, fracture, or neo-plastic growth), there are primarily three TMD disorders for which patients are referred to a surgeon: 1) TMJ inflammation, 2) acute TMJ disc displacement without reduction (closed lock), and 3) TMJ ankylosis (painless severe limited opening)2.
Current Best Evidence in Physical Therapy Treatment
For many years, physical therapy has been used to treat TMD symptoms; however, the evidence supporting its use is limited. In this article, physical therapy treatments are assumed to include manual techniques (i.e., stretching, mobilizations, and manipulations of the TMJ and cervical spine); exercise instruction (i.e., self stretching and mobility strategies for the TMJ and cervical spine); patient education (i.e., postural instruction, relaxation techniques, and parafunctional awareness); and modalities that improve tissue health.
One recent systematic review of the literature on the efficacy of physical therapy interventions for TMD patients found 36 relevant articles, of which 12 met their selection criteria. Only 3 were found “to be of strong methodological quality”34, and 4 of the 12 were dedicated to exercise and manual interventions, and only one did not demonstrate significant benefit from the chosen treatment strategy (an oral exerciser device). The remaining 3 studies evaluated postural training, manual therapy, and exercise, and all demonstrated significant benefit34. The best Jadad score35 obtained for the 4 studies was a 234. This systematic review concluded that “active and passive oral exercises and exercises to improve posture are effective interventions to reduce symptoms associated with TMD”34.
A second recent systematic review that evaluated the literature on the efficacy of physical therapy interventions for TMD patients concluded that active exercise and manual mobilizations may be effective as well as postural training in combination with other TMD interventions36. This review favored the use of multifaceted TMD treatment strategies, which coincided the with review authors' opinions. According to Sackett's rules of evidence37, in general, the study quality was level II for 22 of the 36 studies reviewed36.
Further validation for physical therapy's effectiveness with TMD patients has been published since these two systematic reviews. In general, validity and strength of the studies were weak; however, continued evidence supports that physical therapy may be effectively used as a stand-alone and/or, more effectively, used in a team approach with other conservative TMD therapies38–41. One study suggested that Osteopathic Manipulative Treatment can induce changes in the stomatognathic dynamics, offering a valid support in the clinical approach to TMD”38. A second concluded that “physical therapy seems to have a positive effect on treatment outcomes of patients with TMD”39. A third found that “the combination of orofacial myofunctional therapy and an occlusal splint can be beneficial for patients with TMD-hypermobility”40. An additional study compared four treatment strategies for TMJ close-lock: medical management (education, counseling, self-help, and NSAIDS); rehabilitation (occlusal orthotic, physical therapy, and cognitive-behavioral therapy); arthroscopy with post-operative rehabilitation; and arthroplasty with post-operative rehabilitation (i.e., physical therapy). The results demonstrated that “the four treatment strategies did not differ in magnitude or timing of improved function or pain relief”41. Since the four treatment strategies had similar efficacy, the authors of this article believed that the most cost-effective and conservative methods should be explored prior to progression to more costly, invasive procedures.
Some studies have correlated cervical dysfunction and TMD14,42,43. One found that following a motor vehicle accident, chiropractic treatment alone for cervical spine pain was ineffective; however, providing the patient with an occlusal orthotic relieved the pain with continued chiropractic care14. Although this study evaluated chiropractor intervention, it appears there would be a similar correlation with physical therapy treatment for cervical pain following a motor vehicle accident. There is significant research supporting the use of physical therapy for cervical dysfunction, but more definitive research needs to objectively assess the effectiveness of cervical treatment for TMD pain and the reciprocal relationship.
Current evidence supports the use of physical therapy for TMD patients, but more evidence-based research is needed to firmly establish the role of the physical therapist. Both authors here encourage well-trained physical therapists to inform the dentists in their community about their interest and education in providing TMD treatments for the dentist's TMD patients, enabling the dentist to establish an effective team approach for these patients.
Summary
TMD is similar to musculoskeletal disorders in other parts of the body, and similar therapeutic approaches can generally be used. It is important for dentists to rule out disorders that mimic TMD, to identify non-TMD disorders that may negatively impact the patient's TMD symptoms, and to offer the patient therapies that will provide the most cost-effective long-term symptom relief.
Physical therapists may find the maps in Figure 4 helpful for identifying the true source of referred pain. They may want to provide the dentists who treat TMD patients in their community with a copy of Table 1 (situations when it is recommended that practitioners consider referring TMD patients to a physical therapist)2. They should also be cognizant of potential situations when it may be prudent to refer a TMD patient to a dentist (Table 2)30. Physical therapists may also want to improve their skills in treating TMD patients (see below).
Sources for Physical Therapists to Obtain Additional TMD Training
There are two known physical therapy certifying programs for TMD. The first is the Certified Cervical and Temporomandibular Therapists (CCTT) from the American Academy of Orofacial Pain website (visit http://www.aaop.org/ and select Physical Therapists-PTBCCT). The other is the Cranio-Facial Certification (CFC) from the University of St. Augustine (http://www.usa.edu/ and select Continuing Education/ Certification Programs/Cranio-mandibular Head, Neck, and Facial Pain (CFC).
How Physical Therapists Can Find TMD-Trained Dentists
Dentists' abilities to evaluate and treat TMD vary greatly with their experience and training. Many postgraduate presentations, courses, and fellowship programs are available. Most fellowship programs have physical therapist and psychologist faculty members, so these graduates are well versed in working with these therapists and in referring patients to medical colleagues.
The American Dental Association does not recognize TMD or orofacial pain as a dental specialty, so dentists are not permitted to advertise themselves as a “specialist” in this area. To find a dentist with TMD expertise near your office, visit www.abop.net and select Diplomate Directory.
REFERENCES
- 1.American Academy of Orofacial Pain . In: Orofacial Pain: Guidelines for Assessment, Diagnosis and Management, 4th ed. de Leeuw R, editor. Chicago: Quintessence; 2008. [Google Scholar]
- 2.Wright EF. Manual of Temporomandibular Disorders. Ames, IA: Blackwell; 2005. [Google Scholar]
- 3.Okeson JP. Management of Temporomandibular Disorders and Occlusion, 6th ed. St. Louis, MO: CV Mosby; 2008. [Google Scholar]
- 4.Fricton J. Myogenous temporomandibular disorders: Diagnostic and management considerations. Dent Clin North Am. 2007;51:61–83. doi: 10.1016/j.cden.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 5.Murphy E. Managing Orofacial Pain in Practice. Chicago: Quintessence; 2008. [Google Scholar]
- 6.Ribeiro RF, Tallents RH, Katzberg RW, et al. The prevalence of disc displacement in symptomatic and asymptomatic volunteers aged 6 to 25 years. J Orofac Pain. 1997;11:37–47. [PubMed] [Google Scholar]
- 7.Egermark I, Carlsson GE, Magnusson T. A 20-year longitudinal study of subjective symptoms of temporomandibular disorders from childhood to adulthood. Acta Odontol Scand. 2001;59:40–48. doi: 10.1080/000163501300035788. [DOI] [PubMed] [Google Scholar]
- 8.Magnusson T, Egermark I, Carlsson GE. A longitudinal epidemiologic study of signs and symptoms of temporomandibular disorders from 15 to 35 years of age. J Orofac Pain. 2000;14:310–319. [PubMed] [Google Scholar]
- 9.Wassell RW, Adams N, Kelly PJ. The treatment of temporomandibular disorders with stabilizing splints in general dental practice: One-year follow-up. J Am Dent Assoc. 2006;137:1089–1098. doi: 10.14219/jada.archive.2006.0347. [DOI] [PubMed] [Google Scholar]
- 10.Fricton JR, Schiffman EL. Management of masticatory myalgia and arthralgia. In: Sessle BJ, Lavigne GJ, Lund JP, Dubner R, editors. Orofacial Pain: From Basic Science to Clinical Management. Chicago: Quintessence; 2008. [Google Scholar]
- 11.Rammelsberg P, LeResche L, Dworkin S, Mancl L. Longitudinal outcome of tem-poromandibular disorders: A 5-year epidemiologic study of muscle disorders defined by research diagnostic criteria for temporomandibular disorders. J Orofac Pain. 2003;17:9–20. [PubMed] [Google Scholar]
- 12.Raphael KG, Marbach JJ, Klausner J. Myofascial face pain: Clinical characteristics of those with regional vs. widespread pain. J Am Dent Assoc. 2000;131:161–171. doi: 10.14219/jada.archive.2000.0143. [DOI] [PubMed] [Google Scholar]
- 13.Raphael KG, Marbach JJ. Widespread pain and the effectiveness of oral splints in myofascial face pain. J Am Dent Assoc. 2001;132:305–316. doi: 10.14219/jada.archive.2001.0173. [DOI] [PubMed] [Google Scholar]
- 14.Kraus S. Temporomandibular disorders, head and orofacial pain: Cervical spine considerations. Dent Clin North Am. 2007;51:161–193. doi: 10.1016/j.cden.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 15.Dawson PE. Functional Occlusion: From TMJ to Smile Design. St Louis. MO: Mosby; 2007. [Google Scholar]
- 16.Wright EF. Pulpalgia contributing to temporomandibular disorder-like pain: A literature review and case report. J Am Dent Assoc. 2008;139:436–440. doi: 10.14219/jada.archive.2008.0186. [DOI] [PubMed] [Google Scholar]
- 17.Abdel-Fattah RA. Evaluating and Managing Temporomandibular Injuries, 3rd ed. Boca Raton, FL: Radiance; 2008. [DOI] [PubMed] [Google Scholar]
- 18.Reimam EK. The ABC's of TMJ/TMD Diagnosis & Treatment. Alberta, Canada: Medical Scope; 2005. [Google Scholar]
- 19.Wright EF. Referred craniofacial pain patterns in patients with temporomandibular disorders. J Am Dent Assoc. 2000;131:1307–1315. doi: 10.14219/jada.archive.2000.0384. [DOI] [PubMed] [Google Scholar]
- 20.Simons DG, Travell JG, Simons LS. Travel! & Simons' Myofascial Pain and Dysfunction: The Trigger Point Manual, 2nd ed. I. Baltimore, MD: Williams & Wilkins; 1999. [Google Scholar]
- 21.Fricton JR, Kroening R, Haley D, Siegert R. Myofascial pain syndrome of the head and neck: A review of clinical characteristics of 164 patients. Oral Surg Oral Med Oral Pathol. 1985;60:615–623. doi: 10.1016/0030-4220(85)90364-0. [DOI] [PubMed] [Google Scholar]
- 22.Jaber JJ, Leonetti JP, Lawrason AE, Feustel PJ. Cervical spine causes for referred otalgia. Otolaryngol Head Neck Surg. 2008;138:479–485. doi: 10.1016/j.otohns.2007.12.043. [DOI] [PubMed] [Google Scholar]
- 23.Kuttila S, Kuttila M, Le Bell Y, Alanen P, Suonpaa J. Characteristics of subjects with secondary otalgia. J Orofac Pain. 2004;18:226–234. [PubMed] [Google Scholar]
- 24.Fricton JR, Chung SC. Contributing factors: A key to chronic pain. In: Fricton JR, Kroening RJ, Hathaway KM, editors. TMJ and Craniofacial Pain: Diagnosis and Management. MO: Ishiyaku EuroAmerica: St Louis; 1988. [Google Scholar]
- 25.Clark GT, Minakuchi H. Oral appliances. In: Laskin DM, Greene CS, Hylander WL, editors. Temporomandibular Disorders: An Evidenced-Based Approach to Diagnosis and Treatment. Hanover Park, IL: Quintessence; 2006. [Google Scholar]
- 26.Rossetti LM, Pereira de Araujo Cdos R, Rossetti PH, Conti PC. Association between rhythmic masticatory muscle activity during sleep and masticatory myofascial pain: A polysomnographic study. J Orofac Pain. 2008;22:190–200. [PubMed] [Google Scholar]
- 27.Camparis CM, Siqueira JT. Sleep bruxism: Clinical aspects and characteristics in patients with and without chronic orofacial pain. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:188–193. doi: 10.1016/j.tripleo.2005.01.014. [DOI] [PubMed] [Google Scholar]
- 28.Cooper BC, Kleinberg I. Examination of a large patient population for the presence of symptoms and signs of temporomandibular disorders. Cranio. 2007;25:114–126. doi: 10.1179/crn.2007.018. [DOI] [PubMed] [Google Scholar]
- 29.Falace DA, Reid K, Rayens MK. The influence of deep (odontogenic) pain intensity, quality, and duration on the incidence and characteristics of referred orofacial pain. J Orofac Pain. 1996;10:232–239. [PubMed] [Google Scholar]
- 30.Wright EF, Gullickson DC. Identifying acute pulpalgia as a factor in TMD pain. J Am Dent Assoc. 1996;127:773–780. doi: 10.14219/jada.archive.1996.0313. [DOI] [PubMed] [Google Scholar]
- 31.Orlando B, Manfredini D, Salvetti G, Bosco M. Evaluation of the effectiveness of biobehavioral therapy in the treatment of tem-poromandibular disorders: A literature review. Behav Med. 2007;33:101–118. doi: 10.3200/BMED.33.3.101-118. [DOI] [PubMed] [Google Scholar]
- 32.Chen CY, Palla S, Erni S, Sieber M, Gallo LM. Nonfunctional tooth contact in healthy controls and patients with myogenous facial pain. J Orofac Pain. 2007;21:185–193. [PubMed] [Google Scholar]
- 33.Brown DT, Gaudet EL., Jr Temporomandibular disorder treatment outcomes: Second report of a large-scale prospective clinical study. Cranio. 2002;20:244–253. doi: 10.1080/08869634.2002.11746216. [DOI] [PubMed] [Google Scholar]
- 34.McNeely ML, Armijo Olivo S, Magee DJ. A systematic review of the effectiveness of physical therapy interventions for temporomandibular disorders. Phys Ther. 2006;86:710–725. [PubMed] [Google Scholar]
- 35.Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 36.Medlicott MS, Harris SR. A systematic review of the effectiveness of exercise, manual therapy, electrotherapy, relaxation training, and biofeedback in the management of temporomandibular disorder. Phys Ther. 2006;86:955–973. [PubMed] [Google Scholar]
- 37.Sackett DL. Rules of evidence and clinical recommendations for the use of antithrombic agents. J Chest. 1986;89(2 suppl):2S–3S. [PubMed] [Google Scholar]
- 38.Monaco A, Cozzolino V, Catteneo R, Cutilli T, Spadaro A. Osteopathic manipulative treatment (OMT) effects on mandibular kinetics: Kinesiographic study. Eur J Paediatr Dent. 2008;9:37–42. [PubMed] [Google Scholar]
- 39.de Felicio CM, Freitas RL, Bataglion C. The effects of orofacial myofunctional therapy combined with an occlusal splint on signs and symptoms in a man with TMD-hypermobility: Case study. Int J Orofacial Myology. 2007;33:21–29. [PubMed] [Google Scholar]
- 40.Schiffman EL, Look JO, Hodges JS, et al. Randomized effectiveness study of four therapeutic strategies for TMJ closed-lock. J Dent Res. 2007;86:58–63. doi: 10.1177/154405910708600109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ismail F, Demling A, Hessling K, Fink M, Stiesch-Scholz M. Short-term efficacy of physical therapy compared to splint therapy in treatment of arthrogenous TMD. J Oral Rehabil. 2007;34:807–817. doi: 10.1111/j.1365-2842.2007.01748.x. [DOI] [PubMed] [Google Scholar]
- 42.Vernon LF, Ehrenfeld DC. Treatment of temporomandibular joint syndrome for relief of cervical spine pain: Case report. J Manipulative Physiol Ther. 1982;2:9–81. [PubMed] [Google Scholar]
- 43.Kondo E. Nonextraction and nonsurgical treatment of an adult with skeletal Class II open bite with severe retrognathic mandible and temporomandibular disorders. World J Orthod. 2007;8:261–276. [PubMed] [Google Scholar]