Abstract
Shoulder pain is a common orthopedic condition seen by physical therapists, with many potential contributing factors and proposed treatments. Although manual physical therapy interventions for the cervicothoracic spine and ribs have been investigated for this patient population, the specific effects of these treatments have not been reported. The purpose of this investigational study is to report the immediate effects of thoracic spine and rib manipulation in patients with primary complaints of shoulder pain. Using a test-retest design, 21 subjects with shoulder pain were treated during a single treatment session with high-velocity thrust manipulation to the thoracic spine or upper ribs. Post-treatment effects demonstrated a 51% (32mm) reduction in shoulder pain, a corresponding increase in shoulder range of motion (30°-38°), and a mean patient-perceived global rating of change of 4.2 (median 5). These immediate post-treatment results suggest that thoracic and rib manipulative therapy is associated with improved shoulder pain and motion in patients with shoulder pain, and further these interventions support the concept of a regional interdependence between the thoracic spine, upper ribs, and shoulder.
KEYWORDS: Manipulation, Manual Therapy, Shoulder Pain, Thoracic Spine
Regional interdependence, as described by Wainner and col-leagues1,2, “refers to the concept that seemingly unrelated impairments in a remote anatomical region may contribute to, or be associated with, the patient's primary complaint”. This model suggests that many musculoskeletal disorders may respond more favorably to a regional examination and treatment approach that, in addition to localized treatment, encourages physical therapists to examine and treat distant dysfunctions that may be influencing the patient's symptoms. Although the specific mechanism (whether neurophysiologic, biomechanical, or other) has yet to be elucidated, several high-quality clinical trials have demonstrated the effective use of this regional examination and treatment approach in achieving positive functional outcomes for patients with a variety of musculoskeletal disorders3–10.
Three of these studies3–5 have investigated the effects of including cervicothoracic spine and rib manual physical therapy into an overall treatment approach for patients with shoulder pain. Winters et al5 found that manipulative therapy applied throughout the shoulder girdle was more effective than physiotherapy in reducing the duration of shoulder pain in a subgroup of 58 patients whose shoulder pain was attributed to dysfunctions within the cervical spine, upper thoracic spine, or upper ribs. Bang and Deyle3 reported improved outcomes in strength, function, and pain when manual physical therapy techniques for the shoulder, cervical spine, and thoracic spine were added to an exercise program for patients with shoulder impingement syndrome. In a more recent clinical trial, Bergman et al4 assessed the added benefit of applying cervicothoracic and rib manipulations and mobilizations to a standardized treatment regimen of anti-inflammatory and analgesic medications, corticosteroid injections, and physical therapy (exercises, massage, and modalities) for patients with shoulder pain and dysfunction. The addition of manipulative therapy to this usual medical care resulted in significant improvements in short- and long-term recovery rates and symptom severity for these subjects.
Although the overall treatment effect of manual physical therapy has been demonstrated in these studies, the relative contribution of specific manipulative techniques applied to the cervical spine, thoracic spine, and/or ribs towards the improvement in functional outcomes for patients with shoulder pain cannot be determined. The purpose of this preliminary study is to report the immediate effects of thoracic and rib manipulation on subjects with primary complaints of shoulder pain. Exploratory studies of this nature are needed to help define the potential interdependence between anatomic regions such as the thoracic spine, upper ribs, and shoulder.
Methodology
Subjects
Consecutive patients referred to physical therapy by their primary care managers with a primary complaint of unilateral shoulder pain were considered for participation in this study. Inclusion criteria were a primary complaint of unilateral shoulder pain, age between 18 and 65 years, decreased shoulder range of motion (ROM), and pain reproduction with either the Hawkins-Kennedy test or Neer impingement test. These special tests and their diagnostic properties have been previously described11,12 and are widely used in clinical practice to detect musculoskeletal shoulder disorders. Subjects were excluded from the study if they presented with any shoulder pain resulting from an active systemic disease or serious pathology (e.g. rheumatoid arthritis, infection, tumors, fracture, etc.), a rotator cuff tear confirmed with diagnostic imaging, physical examination findings consistent with shoulder adhesive capsulitis (defined as active and passive physiologic motion limitations in multiple planes, to include those with a suggested capsular pattern), or cervical nerve root pathology diagnosed using a cluster of the following positive tests: Upper Limb Tension Test A (median nerve bias), Spurling A Test, Distraction Test, or cervical rotation < 60° to the ipsilateral side13. Subjects with any serious spinal pathology (e.g., infections, osteoporosis, spinal fracture, or tumors) or exhibiting a fear or unwillingness to undergo spinal manipulative treatment were also excluded.
Subjects that met all criteria provided written informed consent prior to participation. The Navajo Nation Institutional Review Board and Chinle Service Unit Health Board approved this study.
Procedures
History and Physical Examination
A physical therapist performed a standardized history and examination of the shoulder girdle region, to include the shoulder, cervical spine, thoracic spine, and upper ribs. Demographic data were collected on each subject to include age, gender, hand dominance, and the location, nature, and duration of symptoms. Shoulder physical exam measures included active and passive ROM measurements using a bubble inclinometer, manual muscle testing, and a series of diagnostic and provocative special tests commonly used to identify shoulder pathology11,14. The Hawkins-Kennedy test and Neer's impingement test were performed on all subjects. Pain scores were recorded immediately following these pain provocation tests and used as a standardized outcome measure. The cervical spine examination consisted of ROM measurement, passive accessory motion testing, and special tests to rule out a cervical origin for the subject's shoulder pain complaint.
The physical examination concluded with an assessment of the upper thoracic spine and ribs. Motion restrictions and symptom responses were assessed during active ROM and overpressure testing for thoracic flexion, extension, and bilateral rotation. Thoracic segmental mobility testing was performed using central and unilateral postero-anterior passive accessory in-tervertebral motions (PAIVMs) applied to the spinous and transverse processes. Segmental rib dysfunctions were identified using postero-anterior PAIVMs of the costovertebral joints and direct palpation of rib angles. These thoracic and rib physical exam techniques are thoroughly described by Greenman15 and Maitland16. The reliability of thoracic segmental testing for assessing joint mobility is slight to fair for intrarater reliability (kappa = .17 to .33) and slight for interrater reliability (kappa = .03 to .15). When assessing pain provocation, intra-rater reliability increases to fair to good (kappa = .28 to .66) and interrater reliability increases to fair (kappa = .24 to .38)17,18. Similarly, segmental testing of the rib cage yields fair intrarater reliability for mobility (kappa = .26 to .29), no to moderate intrarater reliability for pain (kappa = .00 to .49), no to moderate intrarater reliability for mobility (kappa = .00 to .49), and no to good interrater reliability for pain (kappa = .00 to .66)17,19. Despite this variability in reliability data, these techniques are widely used by manual physical therapists in clinical practice. In a recent survey, Abbott et al20 reported that 66% of manual physical therapists believed PAIVMs were valid for assessing quantity of segmental motion and 98% of respondents based treatment decisions at least in part on the results of this testing
Manual Physical Therapy Interventions
The primary investigator (JS), a residency-trained orthopedic manual physical therapist and a Fellow of the American Academy of Orthopaedic Manual Physical Therapists (FAAOMPT) examined and treated all subjects. Following the physical examination, all subjects received high-velocity thrust manipulative therapy to the upper thoracic spine and/or ribs. The type and number of manipulative techniques performed during the treatment session were based on the presence or absence of specific thoracic and/or rib impairments. Subjects with stiffness in the cervicothoracic junction were treated with a seated cervicothoracic junction distraction manipulation (Figure 1)21. Subjects with a thoracic flexion/opening restriction or a unilateral rib dysfunction were treated with a supine technique that facilitated seg-mental thoracic flexion (Figure 2)21 or rib mobility (Figure 3)21. Subjects with a thoracic extension/closing restriction were treated with a prone technique to facilitate segmental thoracic extension (Figure 4)21. Subjects with no identifiable thoracic or rib restrictions were to receive a nonspecific “general” seated manipulation performed in a longitudinal direction to produce a distraction or unloading of the thoracic spine.
FIGURE 1.

Seated distraction manipulation for the cervicothoracic junction.
FIGURE 2.

Supine flexion/opening manipulation.
FIGURE 3.

Supine unilateral rib manipulation.
FIGURE 4.

Prone extension/closing manipulation.
Outcome Measures
The primary outcome measures for this study were shoulder pain and active ROM. As this was an investigational study, all baseline and immediate post-treatment outcome measurements were collected by a single unblinded physical therapist.
Shoulder ROM was assessed using a bubble inclinometer, with measurements taken at the patient's maximum active ROM. As described by Green et al22, active shoulder flexion and abduction were measured in the seated position and combined total internal and external rotation was measured in the supine position with the shoulder abducted to 90° and the humerus supported by the plinth. One movement was performed and measured for each direction. Using these techniques, the intrarater reliability for measuring shoulder ROM has been reported to be 0.75 to 0.8222.
Pain was assessed using the 100mm visual analog scale (VAS), where a score of 0 represented no pain and 100mm represented the worst pain imaginable. The pre-treatment pain score was taken immediately following baseline shoulder active ROM measurements and provocative special testing and included the Hawkin's-Kennedy, Neer's, and Drop Arm tests. Post-treatment pain was assessed after shoulder active ROM was re-measured and all positive provocative tests from the initial examination were repeated. The VAS has been shown to be a reliable and valid instrument to assess immediate changes in pain intensity. The test-retest reliability has been reported between 0.95 to 0.9723,24 and the minimal clinically important difference (MCID) of 12mm (+/− 3 mm at a 95% CI), regardless of the severity of pain initially reported25.
A 15-point global rating of change (GRC) scale was used as a secondary outcome measure to assess patient-perceived improvement or deterioration following treatment. The GRC requires subjects to select an appropriate phrase to describe their pre- to post-treatment change in symptoms from −7 (a very great deal worse) to +7 (a very great deal better) where a score of 0 represents no change26,27. The intent of this outcome measure was to assess the patient's overall perceived change in shoulder pain, stiffness, and motion immediately following spinal manipulative intervention.
Data Analysis
The data was analyzed using SPSS for Windows software, version 12.0 (SPSS, Inc., Chicago, IL). Statistical significance was set at P = 0.05. Paired t-tests were performed to detect any differences between baseline and post-treatment shoulder ROM measurements and VAS pain scores.
Results
Twenty-two consecutive subjects with primary complaints of shoulder pain were considered for inclusion in this study from February 2004 to February 2005. One subject was excluded due to diagnostic evidence of rotator cuff tear. The 21 subjects (10 male and 11 female) included in this study ranged in age from 21 to 62, with a mean age of 47 (SD = 12.6) years. Symptom duration ranged from 1 to 18 months, with a mean duration of 4.2 (SD = 4.8) months. Thirteen subjects (62%) presented with primary pain complaints in their dominant shoulder.
Physical examination revealed one or more thoracic spine and/or upper rib impairments in every subject, to include CT junction restrictions (71%), upper thoracic flexion restrictions (100%), thoracic extension restrictions (7%), and unilateral rib restrictions (79%). Manipulative therapy techniques, as shown in Figures 1 through 4, were performed based on these segmental impairments. No subjects received the general seated distraction manipulation.
Statistically and clinically important improvements for the entire group were demonstrated in post-treatment shoulder ROM measurements and VAS pain scores immediately following manipulative therapy (Table 1). Shoulder active ROM improved by 38° flexion, 38° abduction, and 30° total rotation (p<0.01). VAS pain intensity scores decreased by 32mm post-treatment (p<0.01), thus surpassing the MCID of 12mm25.
TABLE 1.
Pre-treatment versus post-treatment analysis of visual analog pain scores and shoulder range of motion data.
| Pre-treatment | Post-treatment | Change score | P-value | |
|---|---|---|---|---|
| VAS mean (SD) | 63.1 (22.8) | 31.2 (24.4) | 31.9 | <0.01* |
| Flexion ROM mean (SD) | 106.8° (30.0) | 145.2° (26.4) | 38.4° | <0.01* |
| Abduction ROM mean (SD) | 98° (32.1) | 135.7° (32.5) | 37.7° | <0.01* |
| Rotation ROM mean (SD) | 128.3° (32.1) | 157.8° (22.7) | 29.5° | <0.01* |
VAS = Visual analog scale
ROM = Range of motion
Statistically significant difference using paired t-test (P = 0.05)
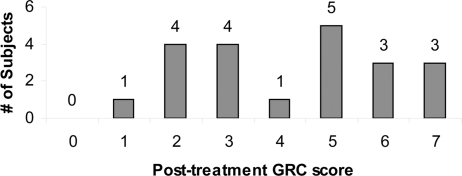
Post-treatment GRC scores (Figure 5) demonstrated a mean score of 4.2 and a median score of 5. Based on the GRC classifications proposed by Juniper et al27, one subject demonstrated no change in symptoms (GRC = 0 or 1), 8 had minimal improvement (GRC = 2 or 3), 6 had moderate improvement (GRC = 4 or 5), and 6 had a large improvement in their condition (GRC = 6 or 7).
FIGURE 5.
Post-treatment patient perceived improvement.
There were no reported adverse effects following treatment with thoracic spine or upper rib manipulations. No patient reported a worsening of symptoms with an increase in VAS, decrease in ROM, or a negative value on the GRC following thoracic or rib manipulative therapy.
Discussion
Several studies have used a regional interdependence examination and treatment approach to demonstrate the effectiveness of including cervicothoracic and upper rib manual physical therapy interventions into the treatment plan for subjects with a primary complaint of shoulder pain3–5. The RCT research design used in these studies precludes the ability to assess immediate within-treat-ment changes, the relative contribution of each independent manipulative technique, or the specific effects of treating a particular region on the subject's symptoms and functional status.
This preliminary exploratory study assessed the immediate effects of four thoracic and rib manipulative therapy techniques on subjects with shoulder pain and limited motion. Although no direct cause-and-effect relationship can be determined in this study, our data suggest that statistically and clinically significant changes in shoulder pain and ROM may occur immediately following thoracic or rib manipulative therapy (Table 1). These results support the concept and current evidence that suggests that a clinically relevant relationship exists between the thoracic spine, ribs, and shoulder regions, and that clinically important improvements in pain and motion can be achieved when this concept is used to guide the physical therapist's examination, evaluation, and treatment processes.
Several possible mechanisms can be offered for our observed treatment effects and this proposed thoracic-rib-shoulder interdependence; however, it is outside the scope and ability of this study to determine which of these may be contributing to our results. First, improving thoracic and rib segmental mobility following manipulation may provide biomechanical contributions towards improved shoulder range of motion, particularly for overhead movements. Norlander et al28–30 have previously reported on the relationship between reduced cervicothoracic mobility and the presence of neck-shoulder pain. This study is unable to report any specific biomechanical effects of thoracic and rib manipulation since spinal motion was not reassessed and the palpatory diagnosis of spinal dysfunctions has poor reliability18,19. A second proposed mechanism for increased shoulder motion is the restoration of neurophysio-logic motor control for the scapular and shoulder musculature as a result of decreased muscle inhibition. Cleland et al31 have demonstrated an increase in lower trapezius muscle strength immediately following thoracic manipulation. Suter et al32–34 have also demonstrated decreased biceps muscle inhibition following cervical manipulation32 and decreased quadriceps inhibition following sacroiliac manipulation33,34. Finally, the hypoalgesic effect of manipulation may contribute to the reduction of shoulder pain and a resultant increase in shoulder motion in this study. Several authors have reported a hypoalgesic effect in distal extremities following bouts of spinal manipulative interventions. Vicenzino et al35 and Fernandez-Carnero et al36 both demonstrated this rapid hypoalge-sic effect following cervical manipulative therapy in patients with lateral epicondylalgia. Iverson et al37 also demonstrated this effect following lumbar manipulation in patients with anterior knee pain. A recently proposed mechanism for this immediate hypoalgesia is an inhibition of C-fiber input as mediated by the local dorsal horn38. Again, while our study is unable to assess the true mechanism for the pain and motion changes observed in these subjects, the results of this study and these proposed mechanisms provide direction for future research.
As previously alluded to, there are several inherent limitations with this preliminary study. We recognize that the lack of researcher blinding, control group usage and randomization, and longer follow-up intervals limit the clinical application of this study. We are unable to ascertain a true cause-and-effect relationship between the thoracic manipulative therapy and the observed changes in shoulder pain and motion among this patient sample. Additionally, these are immediate results only and may only constitute a temporary change in these observed findings. Despite these limitations, this exploratory study suggests that a positive treatment effect may be achieved immediately following thoracic and rib manipulation for subjects with shoulder pain. Further research is needed to determine the short- and long-term effects of thoracic and rib manipulation in subjects with shoulder pain, to develop a clinical prediction rule that identifies those patients likely to respond to this intervention, and to investigate the possible mechanisms involved in achieving these treatment outcomes.
Conclusion
This study demonstrated that thoracic spine and upper rib manipulative therapy is associated with improvement in shoulder pain and ROM immediately following intervention in patients with a primary complaint of shoulder pain. No patients reported adverse effects or a worsening of shoulder symptoms following treatment with thoracic spine or upper rib manipulations. Although further research is necessary, this preliminary study supports the concept of a regional interdependence between the thoracic spine, upper ribs, and shoulder in patients with shoulder pain.
Disclaimer
The opinions or assertions contained herein are the private views of the authors and are not to be construed as official or reflecting the views of the U.S. Public Health Service, U.S. Army, U.S. Air Force, or the Department of Defense.
Footnotes
Work should be attributed to Physical Therapy and Rehabilitation Department, Chinle Comprehensive Healthcare Facility, Chinle, AZ
REFERENCES
- 1.Wainner RS, Flynn TW, Whitman JM. Spinal and Extremity Manipulation: The Basic Skill Set for Physical Therapists. San Antonio, TX: Manipulations; 2001. [Google Scholar]
- 2.Wainner RS, Whitman JM, Cleland JA, Flynn TW. Regional interdependence: A musculoskeletal examination model whose time has come. J Orthop Sports Phys Ther. 2007;37:658–660. doi: 10.2519/jospt.2007.0110. [DOI] [PubMed] [Google Scholar]
- 3.Bang MD, Deyle GD. Comparison of supervised exercise with and without manual physical therapy for patients with shoulder impingement syndrome. J Orthop Sports Phys Ther. 2000;30:126–137. doi: 10.2519/jospt.2000.30.3.126. [DOI] [PubMed] [Google Scholar]
- 4.Bergman GJ, Winters JC, Groenier KH, et al. Manipulative therapy in addition to usual medical care for patients with shoulder dysfunction and pain: A randomized controlled trial. Ann Intern Med. 2004;141:432–439. doi: 10.7326/0003-4819-141-6-200409210-00008. [DOI] [PubMed] [Google Scholar]
- 5.Winters JC, Sobel JS, Groenier KH, Arendzen HJ, Meyboom-de Jong B. Comparison of physiotherapy, manipulation, and corticosteroid injection for treating shoulder complaints in general practice: Randomised, single blind study. BMJ. 1997;314:1320–1325. doi: 10.1136/bmj.314.7090.1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bronfort G, Evans R, Nelson B, Aker PD, Goldsmith CH, Vernon H. A randomized clinical trial of exercise and spinal manipulation for patients with chronic neck pain. Spine. 2001;26:788–797. doi: 10.1097/00007632-200104010-00020. discussion 798789. [DOI] [PubMed] [Google Scholar]
- 7.Walker MJ, Boyles RE, Young BA, et al. The effectiveness of manual physical therapy and exercise for mechanical neck pain: A randomized clinical trial. Spine. 2008;33:2371–2378. doi: 10.1097/BRS.0b013e318183391e. [DOI] [PubMed] [Google Scholar]
- 8.Deyle GD, Allison SC, Matekel RL, et al. Physical therapy treatment effectiveness for osteoarthritis of the knee: A randomized comparison of supervised clinical exercise and manual therapy procedures versus a home exercise program. Phys Ther. 2005;85:1301–1317. [PubMed] [Google Scholar]
- 9.Deyle GD, Henderson NE, Matekel RL, Ryder MG, Garber MB, Allison SC. Effectiveness of manual physical therapy and exercise in osteoarthritis of the knee: A randomized, controlled trial. Ann Intern Med. 2000;132:173–181. doi: 10.7326/0003-4819-132-3-200002010-00002. [DOI] [PubMed] [Google Scholar]
- 10.Whitman JM, Flynn TW, Childs JD, et al. A comparison between two physical therapy treatment programs for patients with lumbar spinal stenosis: A randomized clinical trial. Spine. 2006;31:2541–2549. doi: 10.1097/01.brs.0000241136.98159.8c. [DOI] [PubMed] [Google Scholar]
- 11.Cleland J. Orthopaedic Clinical Examination: An Evidence-Based Approach for Physical Therapists. Yardley, PA: Icon Learning Systems; 2005. [Google Scholar]
- 12.Johansson K, Ivarson S. Intra- and interexaminer reliability of four manual shoulder maneuvers used to identify subacromial pain. Man Ther. 2009;14:231–239. doi: 10.1016/j.math.2008.03.003. [DOI] [PubMed] [Google Scholar]
- 13.Wainner RS, Fritz JM, Irrgang JJ, Boninger ML, Delitto A, Allison S. Reliability and diagnostic accuracy of the clinical examination and patient self-report measures for cervical radiculopathy. Spine. 2003;28:52–62. doi: 10.1097/00007632-200301010-00014. [DOI] [PubMed] [Google Scholar]
- 14.Magee DJ. Orthopedic Physical Assessment, 4th ed. Toronto, Canada: Elsevier Sciences; 2006. [Google Scholar]
- 15.Greenman PE. Principles of Manual Medicine, 2nd ed. Baltimore, MD: Williams & Wilkins; 1996. [Google Scholar]
- 16.Maitland G. Maitland's Vertebral Manipulation, 7th ed. Oxford. UK: Butterworth Heinemann; 2005. [Google Scholar]
- 17.Heiderscheit B, Boissonnault W. Reliability of joint mobility and pain assessment of the thoracic spine and rib cage in asymptomatic individuals. J Man Manip Ther. 2008;16:210–216. doi: 10.1179/106698108790818369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Christensen HW, Vach W, Vach K, et al. Palpation of the upper thoracic spine: An observer reliability study. J Manipulative Physiol Ther. 2002;25:285–292. doi: 10.1067/mmt.2002.124424. [DOI] [PubMed] [Google Scholar]
- 19.Nomden JG, Slagers AJ, Bergman GJ, Winters JC, Kropmans TJ, Dijkstra PU. Interobserver reliability of physical examination of shoulder girdle. Man Ther. 2009;14:152–159. doi: 10.1016/j.math.2008.01.005. [DOI] [PubMed] [Google Scholar]
- 20.Abbott JH, Flynn TW, Fritz JM, Hing WA, Reid D, Whitman JM. Manual physical assessment of spinal segmental motion: Intent and validity. Man Ther. 2009;14:36–44. doi: 10.1016/j.math.2007.09.011. [DOI] [PubMed] [Google Scholar]
- 21.Flynn T. Orthopaedic Manual Physical Therapy Management of the Cervical-Thoracic Spine and Ribcage. Minneapolis, MN: OPTP; 2005. [Google Scholar]
- 22.Green S, Buchbinder R, Forbes A, Bellamy N. A standardized protocol for measurement of range of movement of the shoulder using the Plurimeter-V inclinometer and assessment of its intrarater and interrater reliability. Arthritis Care Res. 1998;11:43–52. doi: 10.1002/art.1790110108. [DOI] [PubMed] [Google Scholar]
- 23.Bijur PE, Silver W, Gallagher EJ. Reliability of the visual analog scale for measurement of acute pain. Acad Emerg Med. 2001;8:1153–1157. doi: 10.1111/j.1553-2712.2001.tb01132.x. [DOI] [PubMed] [Google Scholar]
- 24.McCormack HM, Horne DJ, Sheather S. Clinical applications of visual analogue scales: A critical review. Psych Med. 1988;18:1007–1019. doi: 10.1017/s0033291700009934. [DOI] [PubMed] [Google Scholar]
- 25.Kelly AM. The minimum clinically significant difference in visual analogue scale pain score does not differ with severity of pain. Emerg Med J. 2001;18:205–207. doi: 10.1136/emj.18.3.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jaeschke R, Singer J, Guyatt GH. Measurement of health status: Ascertaining the minimal clinically important difference. Control Clin Trials. 1989;10:407–415. doi: 10.1016/0197-2456(89)90005-6. [DOI] [PubMed] [Google Scholar]
- 27.Juniper EF, Guyatt GH, Willan A, Griffith LE. Determining a minimal important change in a disease-specific Quality of Life Questionnaire. J Clin Epidemiol. 1994;47:81–87. doi: 10.1016/0895-4356(94)90036-1. [DOI] [PubMed] [Google Scholar]
- 28.Norlander S, Aste-Norlander U, Nordgren B, Sahlstedt B. Mobility in the cervico-thoracic motion segment: An indicative factor of musculo-skeletal neck-shoulder pain. Scand J Rehabil Med. 1996;28:183–192. [PubMed] [Google Scholar]
- 29.Norlander S, Gustavsson BA, Lindell J, Nor-dgren B. Reduced mobility in the cervico-thoracic motion segment: A risk factor for musculoskeletal neck-shoulder pain: A two-year prospective follow-up study. Scand J Rehabil Med. 1997;29:167–174. [PubMed] [Google Scholar]
- 30.Norlander S, Nordgren B. Clinical symptoms related to musculoskeletal neck-shoulder pain and mobility in the cervico-thoracic spine. Scand J Rehabil Med. 1998;30:243–251. doi: 10.1080/003655098443995. [DOI] [PubMed] [Google Scholar]
- 31.Cleland JA, Selleck B, Stowell T, et al. Shortterm effects of thoracic manipulation on lower trapezius strength. J Man Manip Ther. 2004;12:82–90. [Google Scholar]
- 32.Suter E, McMorland G. Decrease in elbow flexor inhibition after cervical spine manipulation in patients with chronic neck pain. Clin Biomech. 2002;17:541–544. doi: 10.1016/s0268-0033(02)00025-6. [DOI] [PubMed] [Google Scholar]
- 33.Suter E, McMorland G, Herzog W, Bray R. Decrease in quadriceps inhibition after sac-roiliac joint manipulation in patients with anterior knee pain. J Manipulative Physiol Ther. 1999;22:149–153. doi: 10.1016/S0161-4754(99)70128-4. [DOI] [PubMed] [Google Scholar]
- 34.Suter E, McMorland G, Herzog W, Bray R. Conservative lower back treatment reduces inhibition in knee-extensor muscles: A randomized controlled trial. J Manipulative Physiol Ther. 2000;23:76–80. [PubMed] [Google Scholar]
- 35.Vicenzino B, Collins D, Wright A. The initial effects of a cervical spine manipulative physiotherapy treatment on the pain and dysfunction of lateral epicondylalgia. Pain. 1996;68:69–74. doi: 10.1016/S0304-3959(96)03221-6. [DOI] [PubMed] [Google Scholar]
- 36.Fernandez-Carnero J, Fernandez-de-las-Penas C, Cleland JA. Immediate hypoalgesic and motor effects after a single cervical spine manipulation in subjects with lateral epicondylalgia. J Manipulative Physiol Ther. 2008;31:675–681. doi: 10.1016/j.jmpt.2008.10.005. [DOI] [PubMed] [Google Scholar]
- 37.Iverson CA, Sutlive TG, Crowell MS, et al. Lumbopelvic manipulation for the treatment of patients with patellofemoral pain syndrome: Development of a clinical prediction rule. J Orthop Sports Phys Ther. 2008;38:297–309. doi: 10.2519/jospt.2008.2669. discussion 309-212. [DOI] [PubMed] [Google Scholar]
- 38.George SZ, Bishop MD, Bialosky JE, Zeppieri G, Jr., Robinson ME. Immediate effects of spinal manipulation on thermal pain sensitivity: An experimental study. BMC Musculoskelet Disord. 2006;7:68. doi: 10.1186/1471-2474-7-68. [DOI] [PMC free article] [PubMed] [Google Scholar]