Abstract
Thoracic spine manipulation (TSM) is an intervention practiced by different professions, and recently an incursion of research using TSM has been published. The purpose of this review was to examine the effectiveness of TSM for the management of musculoskeletal conditions and the quality of trials that included TSM techniques. A comprehensive search of online databases was performed, and first authors of studies identified were contacted. Thirteen randomized clinical trials were included in the final review. The methodological quality of all studies was assessed using the 10-point PEDro scale. Seven of the 13 studies were of high quality. Three studies looked at TSM for treatment of shoulder conditions; however, there is limited evidence to support the use of TSM for shoulder conditions. Nine studies used TSM for the management of neck conditions. The meta-analysis identified a subset of homogeneous studies evaluating neck pain. The value of the pooled estimator (1.33) was statistically significant for the treatment effect of TSM in the studies with researcher effect removed (95 % confidence interval: 1.15, 1.52). This analysis suggests there is sufficient evidence to support the use of TSM for specific subgroups of patients with neck conditions. This review also identifies the need for further studies to examine the effectiveness of TSM to treat shoulder conditions and the effectiveness of TSM on neck conditions with long-term follow-up studies.
KEYWORDS: Meta-Analysis, Shoulder, Spinal Manipulation, Systematic Review, Thoracic Spine
Spinal manipulation is a treatment intervention practiced by a number of professions including physical therapists, who often utilize manipulation of the thoracic spine1. The Guide to Physical Therapist Practice2 defines “mobilization/manipulation” as “skilled passive movements to joints and/or related soft tissue that are applied at varying speeds and amplitudes, including small-amplitude/high-velocity therapeutic movements”. For the purpose of this paper, thoracic spine manipulation (TSM) is defined as a high-velocity/low-amplitude movement or “thrust” directed at any segment of the thoracic spine, including the cervicothoracic junction.
Since 2004, there has been an increase in published research investigating the effectiveness of thoracic spine manipulation using different techniques, mostly for treatment of musculoskeletal conditions3–23. This recent research includes the development of a clinical prediction rule (CPR) focused on the use of TSM for the treatment of mechanical neck pain12.
Much of this recent focus on TSM has evaluated the effects of TSM in regions of the body adjacent to the thoracic spine, such as the neck and shoulder, rather than the areas of the thoracic spine itself, a concept known as regional interdependence24. For example, there is evidence that reduced mobility of upper thoracic segments is related to neck-shoulder pain25–27. However, why relationships like this exist is not fully understood and is a topic of debate24,28,29. Bialosky et al28 asserted that the neurophysiological effects of manipulation (such as hypoalgesia) or other non-specific mechanisms (such as placebo or patient expectation) are possibly the cause of regional interdependence. Others have advocated that biomechanical effects associated with manipulation at one vertebral segment may influence adjacent vertebral segements30,31. Apart from what exactly is happening as a result of spinal manipulation/TSM, regional interdependence is a concept that experts agree occurs and that should be considered in clinical decision-making24,28,29.
The purpose of this review is to evaluate the effectiveness of TSM for the management of musculoskeletal conditions and examine the quality of trials that include any TSM technique. In particular, this study examines pooled estimates of the effect of TSM techniques on regions outside the parameters of the thoracic spine.
Methods
Search Strategy
A comprehensive online search was performed using the following databases: PubMed (1969-November 2008), the Cumulative Index of Nursing and Allied Health (CINAHL) (1997-November 2008), Physiotherapy Evidence Database (PEDro) (1995-November 2008), SportDiscus (1991-November 2008), and the Cochrane Central Register of Controlled Trials (1991-November 2008). Key phrases used in CINAHL, PEDro, SportDiscus, and Cochrane Database searches included: thoracic spine manipulation, thoracic spine mobilization, manual therapy, thoracic spine. The Boolean operator, AND, linked the latter two phrases. The same key phrases were used in PubMed searches; however, the results yielded an excessive number of unrelated studies with each search. Therefore, the following phrases were used in PubMed, which includes the previously mentioned Boolean operator: thoracic spine manipulation AND physical therapy, thoracic spine mobilization AND physical therapy.
All titles found in searches from the above databases were screened by one investigator (RW) to identify the articles that might meet eligibility criteria. Those articles were then retrieved to evaluate for inclusion. The reference lists of all retrieved articles were manually reviewed for other potentially eligible articles. Finally, in an attempt to include all pertinent articles in this review, the contact authors of articles that met the eligibility criteria were emailed and provided with a list of eligible articles identified, and asked if they were aware of other articles not listed, including those in press. Authors who did not respond to the first email within 6 days were emailed a second time with the same request. The articles obtained through manually searching references and from published manuscripts went through the same scrutiny as the articles initially found in database searches. All articles that met eligibility criteria were included in this review. No systematic reviews examining the effectiveness of TSM were identified during the database searches.
Selection Criteria
Articles selected met the following eligibility criteria:
Inclusion criteria
Randomized controlled/clinical trial
“Thrust” or “high-velocity/low-amplitude” manipulations of the thoracic spine or cervicothoracic junction was performed as at least part of one group's intervention
Outcomes focused on musculo-skeletal conditions
Exclusion criteria
Mobilizations were used instead of “manipulation” or “thrust” or “high-velocity/low-amplitude” movements
Articles in a language other than English
Subjects less than 18 years old
Only abstract available
For this review, outcomes focused on musculoskeletal conditions were those that could be inherently related to the musculoskeletal system. Such outcomes could include pain, range of motion (ROM), muscle tenderness, disability, strength, and perceived recovery.
In studies where “thrust” or “high-velocity/low-amplitude” was not indicated, but where “manipulation” was noted, the article was deemed to have met eligibility criteria. An exception occurred if “manipulation” was stated but further analysis showed that mobilizations (grades I-IV) were used; in that case, the article was excluded.
Data Extraction and Analysis
Information of interest was extracted from the articles that met eligibility criteria in a standardized form. The extracted information included sample size, age, sex, symptom duration, outcome measures, treatment performed (including manipulation technique or approach), treatment frequency, results, and follow-up. Information not available from articles was marked as “not stated.” Studies that examined the results of TSM on the same anatomical area of the body (such as neck or shoulder) were analyzed by comparing the findings of outcomes (such as pain or ROM).
Studies evaluating individuals with neck pain only were further analyzed for homogeneity. Studies focusing on different symptoms were not analyzed because there were simply too few such studies. The neck study effect size estimates were first corrected for bias32. A chi square test as described by Hedges and Olkin32 was then performed to determine homogeneity of the corrected effect size estimates across studies. Homogeneity confirmed, the corrected effect size estimates were then pooled according to the methods described by Hedges and Olkin32. The confidence interval (CI) for the pooled estimate uses Hedge's32 estimate of the variance of the pooled treatment estimate and a critical value from the standard normal distribution.
Methodological Quality Assessment
The methodological quality of the articles was assessed by using the Physiotherapy Evidence Database (PEDro) scale. The PEDro scale is possibly the most useful scale to assess the methodological quality of physical therapy trials33 and has been shown to have fair to good interrater reliability with an ICC of .55 (95% CI .41, .72) for individual raters34. The PEDro scale consists of 11 items to assess the methodological quality of trials. The first item in the scale deals with the external validity and items 2-11 assess the internal validity of an article. Each item in the scale was scored yes or no; a “1” was given for each yes and “0” for each no. The first item is not included in the total PEDro score of the article; therefore, a maximum of 10 points was possible to score the internal validity of each article, with a range of 0 to 10.
Maher et al34 found from 2 studies of randomized clinical trials that yes responses were common (greater than 50% of the time) for 5 of the 10 internal validity PEDro items; possibly indicating that articles with scores of 5 on the PEDro scale would be of average quality. In those same studies 7 of the 10 items were found to be noted in articles at least 18% of the time. Therefore, to more narrowly identify the articles of higher methodological quality in this review, articles with scores of 7 or higher were noted as high quality, 5-6 of fair quality, and 0-4 of poor quality. The studies were grouped according to the region of the body targeted. Due to some potential overlap, the shoulder group studies were those that primarily focused on mainly affecting the shoulder girdle region, while the neck group studies primarily focused on affecting the cervical region.
One author (RW) conducted all searches, determined eligibility of studies, and read and scored all eligible articles. One author (BM) extracted data for statistical analysis, and another author (TB) performed the meta-analysis of trials.
Results
Article Selection
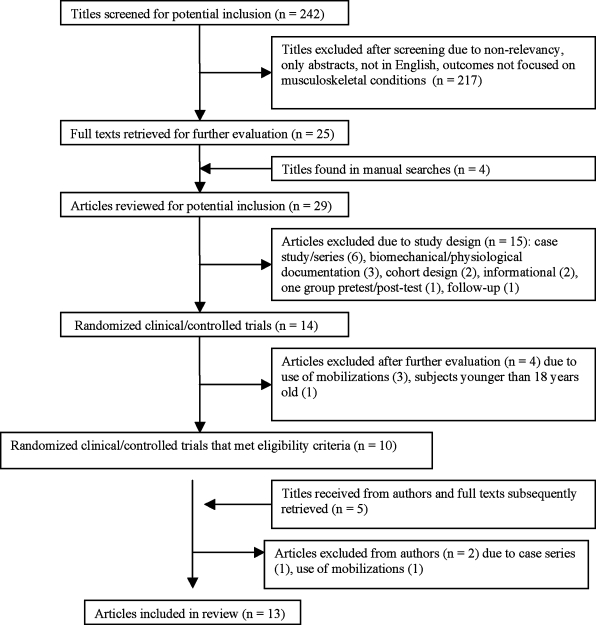
A total of 242 titles were identified in database searches and screened for relevancy and potential eligibility in this review. Four articles were identified from manually searching references of articles found in database searches, and an additional five articles were obtained from authors. Figure 1 illustrates the results of search strategy for potential articles. Following the initial exclusion of articles from database searches and after a review of potentially relevant articles obtained from database searches, manual searches, and authors, 21 obtained articles were excluded for the following reasons: case study/series3,6,9,15,20,23,35, use of mobilization instead of manipulation36–39, purpose being biomechanical/ physiological documentation30,40,41, cohort designs11,12, primarily informational42,43, one group pretest/post-test design5, follow-up of a previous RCT44, or subjects were younger than 18 years of age45.
FIGURE 1.
Flow chart of study selection.
Eight authors were identified and emailed to find out if they were aware of other articles on TSM. Two authors did not have email addresses listed on their articles. Emails were successfully sent to the other six authors and a response from three of them was received from the first email attempt. The other three were sent a second email and one responded. As noted above, this strategy yielded five potential articles. Through all search strategies, 13 studies met eligibility criteria and were included in this review.
Methodological Quality
The systematic assessment of the articles in this review revealed PEDro scores ranging from 4 to 9 out of 10, with a mean of 6.85 (SD, 1.77). The mean of 6.85 indicates that RCTs using TSM exhibited overall fair methodological quality. Seven of the studies were considered of high quality, four of fair quality, and two of poor quality. The most frequently satisfied PEDro criterion was subjects randomly allocated to groups (100%), because the inclusion criteria of this review required use of RCTs. Other PEDro criteria were also frequently satisfied; two criteria with 92%, and five criteria with 77%. One criterion, therapists who administered the treatment were blinded, was not met by any of the articles; and another criterion, subjects were blinded to treatment, was satisfied by 15% of articles. An official attempt was made in two of the articles17,18 to blind subjects to the treatment received and therefore satisfied that criterion. Table 1 shows a detailed breakdown of PEDro scores for individual articles.
TABLE 1.
Breakdown of PEDro scores.
| Author | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | PEDro scores |
|---|---|---|---|---|---|---|---|---|---|---|---|
| González-Iglesias et al18 | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | 9 |
| González-Iglesias et al17 | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | 9 |
| Bergman et al4 | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8 |
| Cleland et al13 | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8 |
| Cleland et al10 | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8 |
| Cleland et al8 | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8 |
| Fernández-de-las-Peñas et al16 | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8 |
| Fernández-de-las-Peñas et al14 | Y | N | Y | N | N | N | Y | Y | Y | Y | 6 |
| Krauss et al19 | Y | Y | Y | N | N | Y | N | N | Y | Y | 6 |
| Winters et al46 | Y | Y | N | N | N | Y | N | Y | Y | Y | 6 |
| Savolainen et al21 | Y | N | N | N | N | Y | Y | N | Y | Y | 5 |
| Parkin-Smith and Penter47 | Y | N | Y | N | N | N | N | N | Y | Y | 4 |
| Strunk and Hondras22 | Y | Y | N | N | N | N | Y | Y | N | N | 4 |
| Total “yes” scores and percentage (%) of “yes” scores in each criterion | 13 (100) | 10 (77) | 10 (77) | 2 (15) | 0 (0) | 10 (77) | 10 (77) | 10 (77) | 12 (92) | 12 (92) |
Y = Criterion was satisfied; N = Criterion was not satisfied
2 = Subjects were randomly allocated in groups
3 = Allocation was concealed
4 = Groups were similar at baseline
5 = Subjects were blinded
6 = Terapists who administered the treatment were blinded
7 = Assessors were blinded
8 = Measures of key outcomes were obtained from more than 85% of subjects
9 = Data analyzed by intention-to-treat
10 = Statistical comparisons between groups were conducted
11 = Point measures and measures of variability were provided
Study Characteristics
All 13 studies included male and female subjects with the number of subjects ranging from 622 to 19846. The average age of subjects was variable but ranged from 25 (SD, 5)16 to 53.5 (SD, 12.5)46. Symptom duration was also variable. Two studies8,16 included asymptomatic subjects and symptom duration was not stated in four studies19,21,22,47. Demographic data from eligible studies is in Table 2.
TABLE 2.
Demographic data from studies.
| Study | n | Male/Female | Average Age (SD) | Symptom Duration (SD) |
|---|---|---|---|---|
| Shoulder | ||||
| Bergman et al4 | 150 | 71/79 | 47.8 (11.8), 48.4 (12.4) | < 6 weeks to > 26 weeks |
| Winters et al46 | 198 | 87/111 | 43.9 (12.6), 46.4 (11.2), 53.5 (12.5), 46.7 (12.1), 53.1 (12.6) | 3,4,8,9,4* |
| Savolainen et al21 | 75 | 18/57 | 43 (7), 46 (6) | Not stated |
| Trunk | ||||
| Cleland et al8 | 40 | 19/21 | 34.7 (12), 31.4 (12) | Asymptomatic |
| Neck | ||||
| González-Iglesias et al18 | 45 | 24/21 | 34 (5) | 18.7 (3.9), 19.5 (4.5) days |
| González-Iglesias et al17 | 45 | 20/25 | 34 (4) | 17 (5), 18 (6) days |
| Cleland et al13 | 60 | 27/33 | 43.3 (12.7) | 56.1 (27.6), 54.9 (46) days |
| Cleland et al10 | 36 | 9/27 | 36 (9.8) | 12.2 (3.5), 13.2 (4.2) weeks |
| Fernández-de-las-Peñas et al16 | 30 | 13/17 | 25 (5), 27 (6), 25 (4.5) | Asymptomatic |
| Fernández-de-las-Peñas et al14 | 88 | 40/48 | 31.2 | 3 weeks to 3 months |
| Krauss et al19 | 32 | 6/26 | 34.2 (9.56), 35 (10.51) | Not stated |
| Parkin-Smith & Penter47 | 30 | 19/11 | 35.4 | Not stated |
| Strunk & Hondras22 | 6 | 1/5 | 48 (12) | Not stated |
Average ages (with standard deviations) of groups are separated by comma.
= Number of weeks before consultation.
The TSM technique used was not noted in three of the studies21,22,46. The most common TSM technique used was a supine anterior-to-posterior manipulation. Pain was the outcome measure most often used in the studies. Two studies did not use a pain scale as an outcome measure8,16, and the most common pain scale used was the visual analog scale.
Statistical Results
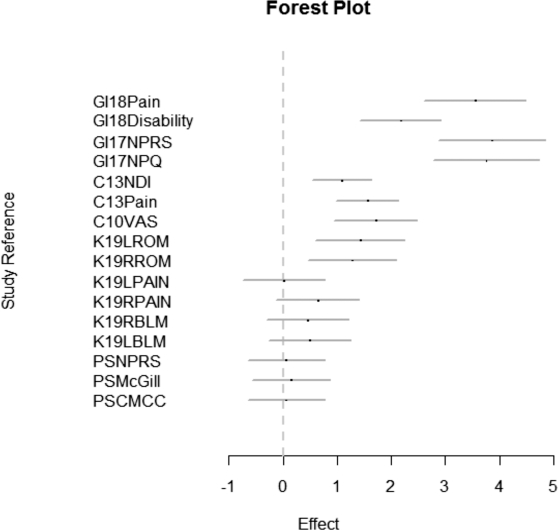
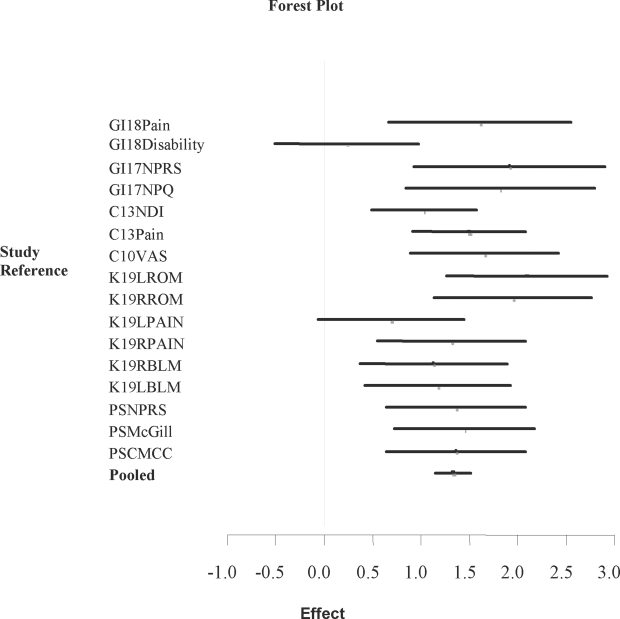
The chi square test statistic for homogeneity of all studies evaluating neck pain was 658.01 (95% chi-square cutoff: 30.14), indicating heterogeneity across studies. When one study evaluating only asymptomatic individuals16 and another outlier study that produced a significant researcher effect14 were removed, the chi square test statistic for homogeneity was 134.56 (95% chi-square cutoff: 24.99). The chi square test statistic for homogeneity without researcher effect was 22.25 (95% chi-square cutoff: 24.99). Figures 2 and 3 illustrate the forest plots of the effect-size CI from each study with and without researcher effects. Heterogeneity is apparent in the plot with researcher effects (Figure 2). Homogeneity was achieved by removing the researcher effect (Figure 3). Thus, a pooled estimator of all the effect sizes was possible. The value of the pooled estimator (1.33) was statistically significant for the treatment effect of TSM in the studies with researcher effect removed (95 % CI: 1.14, 1.52).
FIGURE 2.
Forest plot of the effect-size confidence intervals of all studies evaluating neck pain with researcher effect. Results are heterogeneous.
FIGURE 3.
Forest plot of the effect-size confidence intervals of all studies evaluating neck pain without researcher effect. Results are homogenous and the pooled estimate is statistically significant.
Abbreviations for Figures 2 and 3: C10 = Cleland10; C13 = Cleland13; CMCC = CMCC Neck Disability Index; GI17 = Gonzalez-Iglesias et al17; GI18 = Gonzalez-Iglesias et al18; K = Krauss et al19; LBLM = left cervical bilateral motion; LROM = left cervical range of motion; McGill = McGill Short-form Pain Questionnaire; NPQ = Northwick Neck Pain Questionnaire; NPRS = Numeric Pain Rating Scale; NDI = Neck Disability Index; PS = Parkin-Smith and Penter47; RBLM = right cervical bilateral motion; RROM = right cervical range of motion; VAS = visual analog scale for pain
Shoulder
Three studies used TSM in the treatment of shoulder conditions, one high-quality study4 and two fair quality studies21,46. Subject reported full recovery or being cured was used as an outcome measure in two studies4,46; both reported a notable difference in favor of groups who received TSM. However, Winters and colleagues46 reported that the group that received corticosteroid injections improved faster and a greater number of subjects considered themselves cured than those in the physiotherapy or manipulation groups. Savolainen et al21 noted in a fair study that there was no long-term difference in muscle tenderness or tender thoracic levels between subjects who received either a personal exercise program or TSM and those who dropped out of the study.
Trunk
One high quality study8 investigated the effects of TSM on lower trapezius muscle strength. Subjects who received TSM had significant changes in increased peak strength and percentage of increased strength over those who received a sham manipulation. Although this was a high quality study, the subjects were asymptomatic and hence the generalizability to a patient population is questionable.
Neck
Nine studies investigated the effects of TSM on cervical conditions, five studies were of high quality10,13,16–18, two of fair quality14,19, and two of poor quality22,47. Four studies of high quality10,13,17,18 showed significant improvement in pain from subjects who received TSM over those in comparison groups; similar results were found in one fair study14. Krauss et al19 reported in a fair study that significant improvement in end range pain during right and left cervical rotation occurred in the group that received TSM. Fernandez-de-las-Penas et al16 noted in a study with asymptomatic subjects that the group that received TSM had a significant difference in pressure pain threshold, with the right side (dominant side) having greater improvements than the left side. Again, the generalizability of this study to a patient population is questionable due to the use of asymptomatic subjects. In two high quality studies, Gonzalez-Iglesias and colleagues17,18 found cervical range of motion to be significantly improved in all directions in favor of TSM groups. One fair study19 and one poor study47 found significant within-group changes in bilateral cervical rotation in the groups that received TSM. In the same poor study47, there was also a significant within-group change in bilateral cervical rotation in subjects who received cervical manipulations. Two studies, one high quality13 and one poor quality22, looked at the Neck Disability Index (NDI) to consider improvement in disability. Cleland et al13 found significant improvement in disability in favor of the TSM group, while Strunk and Hondras22 found no significant changes in disability.
Discussion
Evidence for TSM for shoulder conditions is limited, but the studies included in this review4,21,46 do indicate that TSM may accelerate improvement in conditions treated, at least in the short term. Winters and colleagues46 performed a long-term follow-up study44 that showed no significant differences between groups when there were differences at the short term. Subject reported improvement such as full recovery or being cured was the main outcome measure for two studies4,46. Cleland and Durall48 noted that the Winters et al46 article was not clear on the meaning of cured, whether it meant complete symptom reduction or satisfying predetermined criteria. Whatever the case, there is sufficient information provided in these randomized clinical/controlled trials to encourage pursuit of future studies on the effect of TSM on various shoulder conditions.
Four high quality studies10,13,17,18 used TSM as part of a treatment regimen for neck conditions. The four studies showed significant short-term improvement in pain, and three of the studies13,17,18 showed significant short-term improvement in disability. The longest follow-up from all neck studies was 4 weeks18. A CPR developed by Cleland et al12 also indicated effective short-term treatment management for a subgroup of patients with neck pain. Together, the high-quality studies, the CPR, and the pooled data of the meta-analysis, which included each of the high quality neck studies along with one fair study19 and one poor study47, indicate there is sufficient evidence for the use of TSM for short-term results in specific subgroups of patients, and practitioners can confidently use the results of these articles to support their treatment rationale. Research is needed to investigate the long-term results of the effectiveness of these treatment regimens in similar subgroups of subjects.
Krauss et al19 in a fair study found significant within-group changes in pain at end range of right rotation. This result is different from what was found in the high quality studies in this review because pain was rated at end range instead of at rest19. This is an intriguing manner of assessment that associates pain with cervical rotation and, subsequently, indirectly assesses activities such as driving. Several studies17–19,47 reported significant changes in cervical range of motion, including cervical rotation, when TSM was used as a treatment. Obtaining the increased range of cervical motion could, for example, improve the ability to effectively perform the aforementioned activity.
Although the neurophysiological effects are not definitively known, there are several theories that explain what may be occurring as a result of spinal manipulation. In a comprehensive review of the neurophysiological effects of spinal manipulation, Picker49 found that current evidence supports the following mechanisms as contributory to the effects of spinal manipulation: changes in group Ia and group II mechanoreceptor discharge, sensory processing facilitation in the spinal cord, and control of skeletal muscle reflexes. In addition, it has been hypothesized that serotonergic and noradrenergic receptors use descending inhibitory pathways to mediate an analgesic response from spinal manipulation50. Electromyographical studies have suggested that thrust manipulations may elicit muscle activation in muscles adjacent to and opposite of the manipulation site51,52, with muscle activation possibly originating from type II articular mechanoreceptors in the spine51. In a later study, Herzog et al53 did not note the origin of reflex responses but did report specific EMG responses in distinct areas of the body in response to spinal manipulation. The results included clear EMG responses from TSM in back muscles extending to the deltoid of the upper extremity of the side of the spine that was manipulated.
Although the evidence is abundant that some type of neurophysiological effect occurs following spinal manipulation, the placebo effect must also be considered. If a subject in a study is informed of the potential benefits of spinal manipulation, the expectation of the benefits could contribute to placebo analgesia from the treatment54. This manifests the importance of carefully informing subjects of necessary and required information relating to treatment procedures, which will minimize expectation bias in studies.
In the past, the risks of adverse events when performing spinal manipulation have influenced the use of manipulation in physical therapist practice1. However, it can be assumed that due to the increased research including TSM in recent years, spinal manipulation may be used more frequently in practice by physical therapists. The risk of adverse events is a concern that may be encountered in practice and research as the documentation of adverse events associated with spinal manipulation is plentiful55; but adverse events associated with TSM appear to be much less frequent than those associated with cervical and lumbar manipulations1,56,57.
Limitations
There are several limitations to this review. First, the methodological scoring of the studies was performed by one person. Although scoring by one person could potentially be a strong point of the review as all articles were scored using the same critical evaluation process, a method described in other systematic reviews58,59 that uses at least two scorers and a mediator for any unresolved differences in scoring could be a more effective method of methodological scoring. Second, limitations associated with the search strategy were the inclusion of articles only in English and the linking of physical therapy to the key phrases. Studies were found in searches that may have been appropriate for this review, but they were not in English. Other potential studies may have been found without the addition of physical therapy in the key phrases; however, as noted in the methods section, this yielded an excessive amount of unrelated results. Third, the author who selected and scored articles was not blinded to author names.
Conclusion
There is limited evidence to support the use of TSM for shoulder conditions, but there is enough evidence to encourage the pursuit of additional research to determine if TSM is effective for such treatment. There is currently sufficient evidence to support the use of TSM for the management of neck conditions in specific subgroups of patients for short-term outcomes. Long-term follow-up studies should now be done to determine the effectiveness of TSM past the short term for subjects with neck conditions. Additionally, symptomatic subjects should be used in future studies using TSM to increase the generalizability of the results. Considering the studies in this review and the meta-analysis performed, the future appears promising for the use of TSM for the management of certain musculoskeletal conditions.
REFERENCES
- 1.Adams G, Sim J. A survey of UK manual therapists' practice of and attitudes toward manipulation and its complications. Physio-ther Res Int. 1998;3:206–227. doi: 10.1002/pri.141. [DOI] [PubMed] [Google Scholar]
- 2.American Physical Therapy Association Guide to Physical Therapist Practice. Phys Ther. 2001;81:9–746. 2nd ed. [PubMed] [Google Scholar]
- 3.Aspegren D, Hyde T, Miller M. Conservative treatment of a female collegiate volleyball player with costochondritis. J Manipulative Physiol Ther. 2007;30:321–325. doi: 10.1016/j.jmpt.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 4.Bergman GJD, Winters JC, Groenier KH, et al. Manipulative therapy in addition to usual medical care for patients with shoulder dysfunction and pain. Ann Intern Med. 2004;141:432–439. doi: 10.7326/0003-4819-141-6-200409210-00008. [DOI] [PubMed] [Google Scholar]
- 5.Boyles RE, Ritland BM, Miracle BM, et al. The short-term effects of thoracic spine thrust manipulation on patients with shoulder impingement syndrome. Man Ther. 2009;14:375–380. doi: 10.1016/j.math.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 6.Browder DA, Erhard RE, Piva SR. Intermittent cervical traction and thoracic manipulation for management of mild cervical compressive myelopathy attributed to cervical herniated disc: A case series. J Orthop Sports Phys Ther. 2004;34:701–712. doi: 10.2519/jospt.2004.34.11.701. [DOI] [PubMed] [Google Scholar]
- 7.Budgell B, Polus B. The effects of thoracic manipulation on heart rate variability: A controlled crossover trial. J Manipulative Physiol Ther. 2006;29:603–610. doi: 10.1016/j.jmpt.2006.08.011. [DOI] [PubMed] [Google Scholar]
- 8.Cleland J, Selleck B, Stowell T, et al. Short-term effects of thoracic manipulation on lower trapezius muscle strength. J Man Ma-nip Ther. 2004;12:82–90. [Google Scholar]
- 9.Cleland JA, Whitman JM, Fritz JM, Palmer J. Manual physical therapy, cervical traction and strengthening exercises in patients with cervical radiculopathy: A case series. J Or-thop Sports Phys Ther. 2005;35:802–811. doi: 10.2519/jospt.2005.35.12.802. [DOI] [PubMed] [Google Scholar]
- 10.Cleland JA, Childs JD, McRae M, Palmer JA, Stowell T. Immediate effects of thoracic spine manipulation in patients with neck pain: A randomized clinical trial. Man Ther. 2005;10:127–135. doi: 10.1016/j.math.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 11.Cleland JA, Flynn TW, Childs JD, Eberhart S. The audible pop from thoracic spine thrust manipulation and its relation to short-term outcomes in patients with neck pain. J Man Manip Ther. 2007;15:143–154. doi: 10.1179/106698107790819828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cleland JA, Childs JD, Fritz JM, Whitman JM, Eberhart S. Development of a clinical prediction rule for guiding treatment of a subgroup of patients with neck pain: Use of thoracic spine manipulation, exercise, and patient education. Phys Ther. 2007;87:9–23. doi: 10.2522/ptj.20060155. [DOI] [PubMed] [Google Scholar]
- 13.Cleland JA, Glynn P, Whitman JM, Eberhart S, MacDonald C, Childs JD. Short-term effects of thrust versus nonthrust mobilization/manipulation directed at the thoracic spine in patients with neck pain: A randomized clinical trial. Phys Ther. 2007;87:431–440. doi: 10.2522/ptj.20060217. [DOI] [PubMed] [Google Scholar]
- 14.Fernandez-de-las-Penas C, Fernandez-Carnero J, Fernandez AP, Lomas-Varga R, Miangolarra-Page JC. Dorsal manipulation in whiplash injury treatment: A randomized controlled trial. J Whiplash Rel Disord. 2004;3:55–72. [Google Scholar]
- 15.Fernandez-de-las-Penas C, Palomeque-del-Cerro L, Rodríguez-Blanco C, Gímez-Conesa A, Miangolarra-Page JC. Changes in neck pain and active range of motion after a single thoracic spine manipulation in subjects presenting with mechanical neck pain: A case series. J Manipulative Physiol Ther. 2007;30:312–320. doi: 10.1016/j.jmpt.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 16.Fernández-de-las-Penas C, Alonso-Blanco C, Cleland JA, Rodríguez-Blanco C, Albuquerque-Sendin F. Changes in pressure pain thresholds over C5-C6 zygapophyseal joint after a cervicothoracic junction manipulation in healthy subjects. J Manipulative Physiol Ther. 2008;31:332–337. doi: 10.1016/j.jmpt.2008.04.006. [DOI] [PubMed] [Google Scholar]
- 17.Gonzáles-Iglesias J, Fernández-de-las-Penas C, Cleland JA, Albuquerque-Sendín F, Palomeque-del-Cerro L, Míndez-Sánchez R. Inclusion of thoracic spine thrust manipulation into an electrotherapy/thermal program for the management of patients with acute mechanical neck pain: A randomized clinical trial. Man Ther. 2009;14:306–313. doi: 10.1016/j.math.2008.04.006. [DOI] [PubMed] [Google Scholar]
- 18.González-Iglesias J, Fernández-de-las-Peñas C, Cleland JA, Gutiírrez-Vega MR. Thoracic spine manipulation for the management of patients with neck pain: A randomized clinical trial. J Orthop Sports Phys Ther. 2009;39:20–27. doi: 10.2519/jospt.2009.2914. [DOI] [PubMed] [Google Scholar]
- 19.Krauss J, Creighton D, Ely JD, Podlewska-Ely J. The immediate effects of upper thoracic translatoric spinal manipulation on cervical pain and range of motion: A randomized clinical trial. J Man Manip Ther. 2008;16:93–99. doi: 10.1179/106698108790818530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pho C, Godges J. Management of whiplashassociated disorder addressing thoracic and cervical spine impairments: A case report. J Orthop Sports Phys Ther. 2004;34:511–519. doi: 10.2519/jospt.2004.34.9.511. [DOI] [PubMed] [Google Scholar]
- 21.Savolainen A, Ahlberg J, Nummila H, Nissinen M. Active or passive treatment for neck-shoulder pain in occupational health care? A randomized controlled trial. Occup Med. 2004;54:422–424. doi: 10.1093/occmed/kqh070. [DOI] [PubMed] [Google Scholar]
- 22.Strunk RG, Hondras MA. A feasibility study assessing manual therapies to different regions of the spine for patients with subacute or chronic neck pain. J Chiropr Med. 2008;7:1–8. doi: 10.1016/j.jcme.2007.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Waldrop MA. Diagnosis and treatment of cervical radiculopathy using a clinical prediction rule and a multimodal intervention approach: A case series. J Orthop Sports Phys Ther. 2006;36:152–159. doi: 10.2519/jospt.2006.36.3.152. [DOI] [PubMed] [Google Scholar]
- 24.Wainner RS, Whitman JM, Cleland JA, Flynn TW. Regional interdependence: A musculoskeletal examination model whose time has come [guest editorial] J Orthop Sports Phys Ther. 2007;37:658–660. doi: 10.2519/jospt.2007.0110. [DOI] [PubMed] [Google Scholar]
- 25.Norlander S, Gustavsson B-A, Lindell J, Nordgren B. Reduced mobility in the cervico-thoracic motion segment-a risk factor for musculoskeletal neck-shoulder pain: A two-year prospective follow-up study. Scand J Rehab Med. 1997;29:167–174. [PubMed] [Google Scholar]
- 26.Norlander S, Aste-Norlander U, Nordgren B, Sahlstedt B. Mobility in the cervico-thoracic motion segment: An indicative factor of musculoskeletal neck-shoulder pain. Scand J Rehab Med. 1996;28:183–192. [PubMed] [Google Scholar]
- 27.Norlander S, Nordgren B. Clinical symptoms related to musculoskeletal neck-shoulder pain and mobility in the cervico-tho-racic spine. Scand J Rehab Med. 1998;30:243–251. doi: 10.1080/003655098443995. [DOI] [PubMed] [Google Scholar]
- 28.Bialosky JE, Bishop MD, George SZ. Regional interdependence: A musculoskeletal examination whose time has come [letters to the editor-in-chief] J Orthop Sports Phys Ther. 2008;38:159–160. doi: 10.2519/jospt.2008.38.3.159. [DOI] [PubMed] [Google Scholar]
- 29.Wainner RS, Whitman JM, Cleland JA, Flynn TW. Authors' response [letters to the editor-in-chief] J Orthop Sports Phys Ther. 2008;38:160. [Google Scholar]
- 30.Ross JK, Bereznick DE, McGill SM. Determining cavitation location during lumbar and thoracic spinal manipulation. Spine. 2004;29:1452–1457. doi: 10.1097/01.brs.0000129024.95630.57. [DOI] [PubMed] [Google Scholar]
- 31.Herzog W, Kats M, Symons B. The effective forces transmitted by high-speed, low-amplitude thoracic manipulation. Spine. 2001;26:2105–2111. doi: 10.1097/00007632-200110010-00012. [DOI] [PubMed] [Google Scholar]
- 32.Hedges LV, Olkin I. Statistical Methods for Meta-Analysis. FL: Academic Press: Orlando; 1985. [Google Scholar]
- 33.Olivo SA, Macedo LG, Gadotti IC, Fuentes J, Stanton T, Magee DJ. Scales to assess the quality of randomized controlled trials: A systematic review. Phys Ther. 2008;88:156–175. doi: 10.2522/ptj.20070147. [DOI] [PubMed] [Google Scholar]
- 34.Maher CG, Sherrigton C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro Scale for rating quality of randomized controlled trials. Phys Ther. 2003;83:713–721. [PubMed] [Google Scholar]
- 35.Horton SJ. Acute locked thoracic spine: Treatment with a modified SNAG. Man Ther. 2002;7:103–107. doi: 10.1054/math.2002.0456. [DOI] [PubMed] [Google Scholar]
- 36.Allison GT, Nagy BM, Hall T. A randomized clinical trial of manual therapy for cervico-brachial pain syndrome: A pilot study. Man Ther. 2002;7:95–102. doi: 10.1054/math.2002.0453. [DOI] [PubMed] [Google Scholar]
- 37.Cleland JA, Flynn TW, Palmer JA. Incorporation of manual therapy directed at the cervicothoracic spine in patients with lateral epicondylalgia: A pilot clinical trial. J Man Manip Ther. 2005;13:143–151. [Google Scholar]
- 38.Ferreira ML, Ferreira PH, Hodges PW. Changes in postural activity of the truck muscles following spinal manipulative therapy. Man Ther. 2007;12:240–248. doi: 10.1016/j.math.2006.06.015. [DOI] [PubMed] [Google Scholar]
- 39.Liebler EJ, Tufano-Coors L, Douris P, et al. The effect of thoracic spine mobilization on lower trapezius strength testing. J Man Manip Ther. 2001;9:207–212. [Google Scholar]
- 40.Bereznick DE, Ross JK, McGill SM. The frictional properties at the thoracic skin-fascia interface: Implications in spine manipulation. Clin Biomech. 2002;17:297–303. doi: 10.1016/s0021-9290(02)00014-3. [DOI] [PubMed] [Google Scholar]
- 41.Keating L, Lubke C, Powell V, Young T, Souvlis T, Jull G. Mid-thoracic tenderness: A comparison of pressure pain threshold between spinal regions, in asymptomatic subjects. Man Ther. 2001;6:34–39. doi: 10.1054/math.2000.0377. [DOI] [PubMed] [Google Scholar]
- 42.Fernandez de las Penas C, Palomeque del Cerro L, Fernandez Carnero J. Manual treatment of post-whiplash injury. J Bodywork Movement Ther. 2005;9:109–119. [Google Scholar]
- 43.Lee DG. Rotational instability of the mid-thoracic spine: Assessment and management. Man Ther. 1996;1:234–241. doi: 10.1054/math.1996.0273. [DOI] [PubMed] [Google Scholar]
- 44.Winters JC, Jorritsma W, Groenier KH, So-bel JS, Meyboom-de Jong B, Arendzen HJ. Treatment of shoulder complaints in general practice: Long-term results of a randomized, single-blind study comparing physiotherapy, manipulation, and corticosteroid injection. BMJ. 1999;318:1395–1396. doi: 10.1136/bmj.318.7195.1395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Schiller L. Effectiveness of spinal manipulative therapy in the treatment of mechanical thoracic spine pain: A pilot randomized clinical trial. J Manipulative Physiol Ther. 2001;24:394–401. doi: 10.1067/mmt.2001.116420. [DOI] [PubMed] [Google Scholar]
- 46.Winters JC, Sobel JS, Groenier KH, Arendzen HJ, Meyboom-de Jong B. Comparison of physiotherapy, manipulation, and corticosteroid injection for treating shoulder complaints in general practice: Randomized, single-blind study. BMJ. 1997;314:1320–1325. doi: 10.1136/bmj.314.7090.1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Parkin-Smith GF, Penter CS. A clinical trial investigating the effect of two manipulative approaches in the treatment of mechanical neck pain: A pilot study. JNMS. 1998;6:6–16. [Google Scholar]
- 48.Cleland J, Durall CJ. Physical therapy for adhesive capsulitis. Physiotherapy. 2002;88:450–457. [Google Scholar]
- 49.Pickar JG. Neurophysiological effects of spinal manipulation. Spine J. 2002;2:357–371. doi: 10.1016/s1529-9430(02)00400-x. [DOI] [PubMed] [Google Scholar]
- 50.Skyba DA, Radhakrishnan R, Rohlwing JJ, Wright A, Sluka KA. Joint manipulation reduces hyperalgesia by activation of mono-amine receptors but not opioid or GABA receptors in the spinal cord. Pain. 2003;106:159–168. doi: 10.1016/s0304-3959(03)00320-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Suter E, Herzog W, Conway PJ, Zhang YT. Reflex response associated with manipulative treatment of the thoracic spine. JNMS. 1994;2:124–130. [Google Scholar]
- 52.Herzog W, Conway PJ, Zhang YT, Gal J, Guimaraes ACS. Reflex response associated with manipulative treatments on the thoracic spine: A pilot study. J Manipulative Physiol Ther. 1995;18:233–236. [PubMed] [Google Scholar]
- 53.Herzog W, Scheele D, Conway PJ. Electromyographic responses of back and limb muscles associated with spinal manipulative therapy. Spine. 1999;24:146–153. doi: 10.1097/00007632-199901150-00012. [DOI] [PubMed] [Google Scholar]
- 54.Price DD, Milling LS, Kirsch I, Duff A, Montgomery GH, Nicholls SS. An analysis of factors that contribute to the magnitude of placebo analgesia in an experimental paradigm. Pain. 1999;83:147–156. doi: 10.1016/s0304-3959(99)00081-0. [DOI] [PubMed] [Google Scholar]
- 55.Ernst E. Adverse effects of spinal manipulation: A systematic review. J R Soc Med. 2007;100:330–338. doi: 10.1258/jrsm.100.7.330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dvorak J, Loustalot D, Baumgartner H, Antinnes JA. Frequency of complications of manipulation of the spine: A survey among the members of the Swiss Medical Society of Manual Medicine. Eur Spine J. 1993;2:136–139. doi: 10.1007/BF00301410. [DOI] [PubMed] [Google Scholar]
- 57.Oppenheim JS, Spitzer DE, Segal DH. Non-vascular complications following spinal manipulation. Spine J. 2005;5:660–667. doi: 10.1016/j.spinee.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 58.Decoster LC, Cleland J, Altieri C, Russell P. The effects of hamstring stretching on range of motion: A systematic literature review. J Orthop Sports Phys Ther. 2005;35:377–387. doi: 10.2519/jospt.2005.35.6.377. [DOI] [PubMed] [Google Scholar]
- 59.Coppola SM, Collins SM. Is physical therapy more beneficial than unsupervised home exercise in treatment of post-surgical knee disorders? A systematic review. Knee. 2009;16:171–175. doi: 10.1016/j.knee.2008.09.001. [DOI] [PubMed] [Google Scholar]