Abstract
Objectives
To determine the association between myocardial infarction and use of different types of oral contraception in young women.
Design
Community based case-control study. Data from interviews and general practice records.
Setting
England, Scotland, and Wales.
Participants
Cases (n=448) were recruited from women aged between 16 and 44 who had suffered an incident myocardial infarction between 1 October 1993 and 16 October 1995. Controls (n=1728) were women without a diagnosis of myocardial infarction matched for age and general practice.
Main outcome measures
Odds ratios for myocardial infarction in current users of all combined oral contraceptives stratified by their progestagen content compared with non-users; current users of third generation versus second generation oral contraceptives.
Results
The adjusted odds ratio for myocardial infarction was 1.40 (95% confidence interval 0.78 to 2.52) for all combined oral contraceptive users, 1.10 (0.52 to 2.30) for second generation users, and 1.96 (0.87 to 4.39) for third generation users. Subgroup analysis by progestagen content did not show any significant difference from 1, and there was no effect of duration of use. The adjusted odds ratio for third generation users versus second generation users was 1.78 (0.66 to 4.83). 87% of cases were not exposed to an oral contraceptive, and 88% had clinical cardiovascular risk factors or were smokers, or both. Smoking was strongly associated with myocardial infarction: adjusted odds ratio 12.5 (7.29 to 21.5) for smoking 20 or more cigarettes a day.
Conclusions
There was no significant association between the use of oral contraceptives and myocardial infarction. The modest and non-significant point estimates for this association have wide confidence intervals. There was no significant difference between second and third generation products.
Key message
There is no evidence of a difference between second and third generation oral contraceptives on risk of myocardial infarction
There is no significantly increased risk of myocardial infarction in users of oral contraceptives
Of women aged under 45 years who suffered a myocardial infarction, 87% were not taking any oral contraceptive
Of women who suffered myocardial infarction, 88% had one or more known cardiovascular risk factors
Young women who wish to preserve cardiovascular health should be advised to stop smoking, above all else
Introduction
Recent studies on the association between use of oral contraceptives and myocardial infarction have suggested that any risk is confined to women with known cardiovascular risk factors.1–3 Reported odds ratios vary between 1.67 and 5.01 for comparison of current users of all types of combined oral contraceptive versus non-users. Only one study, however, had sufficient power to report on the variation in risk between different types of oral contraceptive.3 This study found an odds ratio of 0.28 (95% confidence interval 0.09 to 0.86) for current users of third generation versus second generation oral contraceptives. Third generation oral contraceptives were defined as those containing the progestagens gestodene and desogestrel combined with ethinyloestradiol and second generation as containing the progestagens levonorgestrel and norethisterone combined with less than 50 μg of ethinyloestradiol. The MICA study was designed to investigate whether the risk of myocardial infarction was influenced by oral contraceptive use overall and to study in more detail the effect of different types of oral contraceptives among women in England, Scotland, and Wales.
Methods
The research protocol for this study has been published elsewhere.4 This was a community based, retrospective case-control study undertaken in the population of England, Scotland, and Wales.
Cases
—Women were eligible as cases if they were aged 16-44 and had suffered an incident myocardial infarction between 1 October 1993 and 16 October 1995. Exclusion criteria were a history of myocardial infarction, pregnancy in the 6 weeks before the date of the myocardial infarction, or a history of menopause, hysterectomy, oophorectomy, and breast or ovarian cancer. Cases were identified from hospital inpatient episode statistics and the deaths register of the Office for National Statistics for all England and Wales and from the Information and Statistics division of the Department of Health or the registrar general’s office in Scotland. International classification of diseases, 9th revision (ICD-9) code 410 or 10th revision (ICD-10) code 121 were used as identifiers of acute myocardial infarction. A validation study in Tayside, Scotland, showed 67% sensitivity and 100% specificity in using only these codes for identifying the cases.5 Diagnostic information for each potential case was extracted from the hospital notes, and these data were submitted to a panel of three cardiologists, blinded to exposure status, for confirmation of diagnosis. Criteria for diagnosis were according to the World Health Organisation, with inclusion of the case depending on a majority decision of the diagnosis as being “definite” or “possible.”6 Cases in which the woman died before reaching hospital or before investigations had been done were validated on the result of the necropsy findings. Those without necropsy were excluded. Women were interviewed in the community by using a structured questionnaire, after consent was obtained from the general practitioner and the patient. For women who died we interviewed a proxy (husband or a close relative).
Controls
—Control women were selected from the general practice with which the index woman was registered at the time of her myocardial infarction. They were closely matched by age: each general practitioner provided a list of women with date of birth closest to the index woman’s (six older and six younger), and we interviewed the four controls with closest date of birth (two older and two younger) from among those who consented.
Interview data
—The interview included questions on medical history of cardiovascular risk factors, obstetric history (including history of high blood pressure), use of contraception in the 5 years before the myocardial infarction (recorded in a calendar), drug history, family history of premature cardiovascular disease, and socioeconomic status (by employment history of interviewee and partner). Current use of oral contraceptives was defined as use within 3 months of the date of myocardial infarction to enable direct comparisons with results from WHO and transnational studies.1,3 Interviews were carried out between December 1996 and February 1998 and thus the length of recall varied between 14 months and 51 months.
Risk factors
—Risk factors and exposure data (oral contraceptive use, blood pressure, smoking, lipid concentrations, and family history) were validated by checking against the interviewee’s general practitioner record or occasionally against records from family planning clinics. We calculated odds ratios using three different measures of exposure: interview data, general practitioner record data, and a compromise with exposure data taken from general practitioner records when the two sources disagreed on the type of oral contraceptive and interview data when there was disagreement on whether or not there was any current exposure to oral contraception.
Control of observer bias
—All research assistants were trained in a standardised technique and were issued with a standard field manual. They were quality controlled throughout the study by means of accompanied and taped interviews.
Statistical power
—With data from 448 cases and 1728 controls available for statistical evaluation and a prevalence of exposure to third generation oral contraceptives of 3.7% in the controls the power of this study to detect an odds ratio of 2 for third generation users versus no use was 81% at the 5% significance level. The power for second generation oral contraceptive users (exposure 7.2%) versus no use was 96%.
Statistical analysis
—We fitted conditional logistic regression models with STATA (StataCorp, Texas, release 5, 1997) with outcome (case-control status) as the dependent variable. Unadjusted univariate odds ratios were estimated for category of contraceptive use and for all potential confounding variables. In a first, planned, multivariate analysis a stepwise backward elimination procedure was carried out to identify those potential confounding variables which were independently related to outcome by using an arbitrary significance level for expulsion from the model of P<0.05. The odds ratios for category of contraceptive use were then adjusted for those confounding factors which entered the stepwise regression model. These are referred to as “select.” In a second multivariate analysis we adjusted the odds ratios for contraceptive use category for all potential confounding factors. These are referred to as “full.” Both analyses are presented. Finally, unconditional logistic regression models were fitted to selected subgroups of cases and controls, again with STATA.
Results
Incidence rate
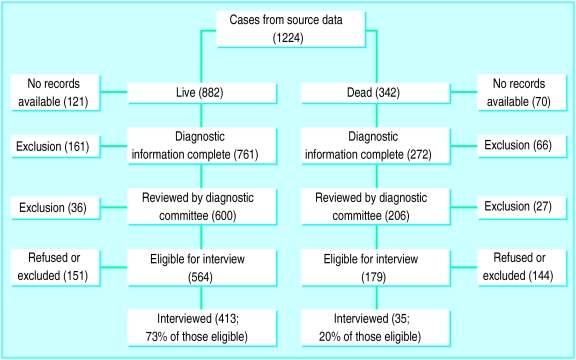
On the basis of 1224 cases identified from source data (see figure), the incidence rate of myocardial infarction was 0.5 per 1000 women years.
Cases and controls
We interviewed 413 women who had experienced myocardial infarction (index women) and 35 surrogates in cases when the index woman had died, representing 60.4% of the total eligible cases. There was a large difference in the interview rate between surviving index women and surrogates (figure). A total of 1728 control women were interviewed, giving a mean of 3.86 controls per case. Age matching between cases and controls was good, the median age difference being only 18 days (table 1). We validated the data from 436 (97%) cases and 1716 (99%) controls with general practitioner or family planning records.
Table 1.
Conditional odds ratios for characteristics of women who suffered myocardial infarction (cases) and control women. Figures are numbers (percentage) of women unless stated otherwise
| Variable | Cases (n=448) | Controls (n=1728) | Univariate odds ratio (95% CI) |
|---|---|---|---|
| Median (interquartile range) age (years) | 40.6 (37.4-42.9) | 40.7 (37.4-42.9) | |
| Medical history: | |||
| Hypertension | 81 (18.1) | 88 (5.1) | 4.23 (3.03 to 5.89) |
| Chronic bronchitis | 34 (7.6) | 36 (2.1) | 4.26 (2.57 to 7.07) |
| Stroke | 10 (2.2) | 7 (0.4) | 5.14 (1.92 to 13.8) |
| Heart disease | 11 (2.5) | 31 (1.8) | 1.24 (0.59 to 2.58) |
| Angina | 22 (4.9) | 10 (0.6) | 9.27 (4.26 to 20.2) |
| Hyperlipidaemia | 34 (7.6) | 51 (3.0) | 2.68 (1.70 to 4.23) |
| Diabetes mellitus | 52 (11.6) | 17 (1.0) | 14.1 (7.82 to 25.5) |
| Cardinal risk factors* | 147 (32.8) | 140 (8.1) | 5.80 (4.38 to 7.67) |
| Blood pressure measured: | |||
| In past year | 263 (58.7) | 985 (57.0) | 0.97 (0.77 to 1.23) |
| Not known | 47 (10.5) | 239 (13.8) | 0.71 (0.49 to 1.03) |
| Obstetric history: | |||
| Ever pregnant | 399 (89.1) | 1521 (88.0) | 1.17 (0.82 to 1.66) |
| Multiparity (>4 live births) | 22 (4.9) | 39 (2.3) | 2.46 (1.33 to 4.54) |
| Pre-eclampsia | 146 (32.6) | 396 (22.9) | 1.64 (1.30 to 2.06) |
| Sterilisation | 129 (28.8) | 355 (20.5) | 1.63 (1.27 to 2.08) |
| Other medications: | |||
| Steroids (oral/inhaler/topical) | 45 (10.0) | 85 (4.9) | 2.19 (1.49 to 3.22) |
| Other hormones | 23 (5.1) | 71 (4.1) | 1.25 (0.76 to 2.07) |
| Psychotropic drugs | 56 (12.5) | 117 (6.8) | 2.03 (1.43 to 2.88) |
| Other, non-cardiovascular drugs | 157 (35.0) | 252 (14.6) | 3.18 (2.49 to 4.06) |
| Family history: | |||
| Ischaemic heart disease | 243 (54.2) | 494 (28.6) | 3.04 (2.44 to 3.79) |
| Hypertension | 140 (31.3) | 486 (28.1) | 1.17 (0.94 to 1.47) |
| Hyperlipidaemia | 63 (14.1) | 151 (8.7) | 1.74 (1.27 to 2.39) |
| Personal history: | |||
| Mean (SD) body mass index kg/m2 | 28.13 (6.57) | 25.37 (4.99) | 1.09 (1.07 to 1.11)† |
| Smoked in past year | 360 (80.4) | 520 (30.1) | 9.99 (7.58 to 13.2) |
| Ever smoked cigarettes | 394 (87.9) | 899 (52.0) | 6.88 (5.05 to 9.36) |
| Cigarettes/day smoked in past year: | |||
| 1-9 | 14 (3.1) | 58 (3.4) | 2.54 (1.30 to 4.94) |
| 10-19 | 93 (20.8) | 214 (12.4) | 6.27 (4.40 to 8.94) |
| ⩾20 | 253 (56.5) | 247 (14.3) | 16.5 (12.0 to 22.8) |
| Alcohol intake (days/week): | |||
| 1 | 85 (19.0) | 414 (24.0) | 0.60 (0.45 to 0.80) |
| 2-3 | 88 (19.6) | 467 (27.1) | 0.54 (0.41 to 0.72) |
| 4-7 | 45 (10.0) | 161 (9.3) | 0.79 (0.54 to 1.14) |
| Takes exercise to keep fit (hours/week): | |||
| ⩾1 | 46 (10.3) | 273 (15.8) | 0.45 (0.32 to 0.64) |
| >1-2 | 35 (7.8) | 291 (16.8) | 0.33 (0.22 to 0.48) |
| >2-3 | 38 (8.5) | 173 (10.1) | 0.55 (0.37 to 0.81) |
| >3 | 64 (14.3) | 269 (15.6) | 0.60 (0.43 to 0.82) |
| Subject employed in past year | 287 (64.1) | 1372 (79.4) | 0.46 (0.36 to 0.57) |
Any one of hypertension, hyperlipidaemia, angina, or diabetes mellitus.
For 1 unit increase in body mass index.
Risk factors
Table 1 shows the distribution of the potential confounders between the cases and controls. Most of these covariates were shown to be associated with an increased risk of myocardial infarction: smoking, diabetes mellitus, and history of angina having the largest effects. In 88% of cases (versus 36% of controls) we found one or more cardiovascular risk factors. In particular, 80% (360) of the index women were smokers compared with 30% (520) of controls, and there was a clear gradient of risk with increasing number of cigarettes smoked per day. The population attributable fraction for smoking in the year before the myocardial infarction was 73%. Consumption of alcohol, taking regular exercise to keep fit, and being in paid work in the past year were all associated with a decreased risk of myocardial infarction.
Exposure to oral contraceptives
Table 2 shows the data on exposure to oral contraceptives in the 3 months before the date of the myocardial infarction. From the subject interviews, 87% of index women were not taking an oral contraceptive in this time period.
Table 2.
Unadjusted conditional odds ratios by source of information on oral contraceptive use in women who suffered myocardial infarction (cases) and control women
| Progestagen group | No (%) of cases (n=448*) | No (%) of controls (n=1728*) | Unadjusted odds ratios by interview data (95% CI) | Unadjusted odds ratios by GP record data (95% CI) | Unadjusted odds ratios by data combined (95% CI)† |
|---|---|---|---|---|---|
| No oral contraception | 386 (86.7) | 1467 (85.0) | 1.00 | 1.00 | 1.00 |
| 2nd and 3rd generation | 40 (9.2) | 180 (10.7) | 0.79 (0.53 to 1.16) | 0.75 (0.50 to 1.11) | 0.78 (0.52 to 1.18) |
| 2nd generation | 20 (4.5) | 119 (7.1) | 0.58 (0.35 to 0.98) | 0.78 (0.47 to 1.29) | 0.73 (0.43 to 1.25) |
| Norethisterone | 2 (0.4) | 14 (0.8) | 0.49 (0.11 to 2.23) | 1.53 (0.39 to 5.97) | 1.25 (0.25 to 6.19) |
| Levonorgestrel | 18 (4.0) | 105 (6.1) | 0.59 (0.34 to 1.03) | 0.72 (0.42 to 1.23) | 0.69 (0.39 to 1.22) |
| 3rd generation | 20 (4.5) | 61 (3.5) | 1.20 (0.7. to 2.06) | 0.71 (0.40 to 1.24) | 0.85 (0.48 to 1.51) |
| Gestodene | 11 (2.5) | 24 (1.4) | 1.72 (0.82 to 3.62) | 1.10 (0.51 to 2.35) | 1.33 (0.61 to 2.89) |
| Desogestrel | 9 (2.0) | 37 (2.1) | 0.86 (0.41 to 1.84) | 0.48 (0.22 to 1.09) | 0.58 (0.25 to 1.31) |
| Progestagen only | 9 (2.0) | 49 (2.8) | 0.69 (0.34 to 1.43) | 0.80 (0.44 to 1.43) | 0.80 (0.41 to 1.55) |
No information on oral contraceptive use obtained from three cases and two controls. There were 10 index women and 30 controls taking other oral contraceptives: type unknown, norgestimate, high dose oestrogen (50 mg mestranol), or cyproterone (interview data).
With interview data when disagreement on current exposure or not, GP record data when disagreement on type of oral contraceptive.
Univariate analysis
Although most of the point estimates of the unadjusted odds ratios were below 1, the 95% confidence intervals predominantly include 1 (table 2). We further subdivided the third generation oral contraceptives that contain desogestrel into two classes: those with low dose (20 μg) and those with standard dose (30 μg) ethinyloestradiol. The odds ratio for low dose was 0.46 (95% confidence interval 0.13 to 1.55) and that for standard dose was 1.57 (0.59 to 4.17), but these were based on only three and six cases, respectively.
Stratification by current smoking habit (non-smokers, all smokers, and smoking >20 cigarettes a day) produced odds ratios which were not significantly different from 1 for any classification of oral contraceptive.
Multivariate analysis
Table 3 shows the odds ratios from the “select” model adjusted for number of cigarettes smoked a day, diabetes mellitus, family history of ischaemic heart disease, other drugs taken in past year, body mass index, history of hypertension, history of angina, and whether or not blood pressure was taken in past year. Adjustment tended to increase the odds ratios, but none was significant. There was no effect of duration of use of oral contraceptives. There were some differences in the point estimates of odds ratios derived from the two data sources (interview and general practitioner record data), but the 95% confidence intervals overlapped.
Table 3.
Adjusted conditional odds ratios (95% confidence intervals) by source of information on oral contraceptive use in women who suffered myocardial infarction (cases) and control women
| Progestogen group | Select
model*
|
Full model
|
|||||
|---|---|---|---|---|---|---|---|
| Subject interview | GP record form | Interview and GP† | Subject interview | GP record form | Interview and GP† | ||
| No oral contraception | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |
| 2nd and 3rd generation | 1.23 (0.70 to 2.16) | 1.30 (0.75 to 2.25) | 1.22 (0.69 to 2.14) | 1.50 (0.83 to 2.70) | 1.50 (0.85 to 2.65) | 1.40 (0.78 to 2.52) | |
| 2nd generation | 0.94 (0.47 to 1.90) | 1.16 (0.59 to 2.26) | 0.98 (0.49 to 1.99) | 1.12 (0.54 to 2.32) | 1.30 (0.64 to 2.63) | 1.10 (0.52 to 2.30) | |
| Norethisterone | 0.75 (0.06 to 9.03) | 2.56 (0.39 to 16.9) | 1.83 (0.15 to 22.7) | 0.92 (0.07 to 11.7) | 3.14 (0.44 to 22.6) | 2.26 (0.16 to 32.2) | |
| Levonorgestrel | 0.95 (0.46 to 1.97) | 1.06 (0.52 to 2.17) | 0.93 (0.45 to 1.95) | 1.13 (0.53 to 2.41) | 1.18 (0.56 to 2.48) | 1.03 (0.48 to 2.23) | |
| 3rd generation | 1.82 (0.83 to 4.00) | 1.56 (0.72 to 3.40) | 1.66 (0.75 to 3.67) | 2.30 (1.02 to 5.19) | 1.84 (0.83 to 4.05) | 1.96 (0.87 to 4.39) | |
| Gestodene | 2.06 (0.66 to 6.44) | 2.32 (0.78 to 6.92) | 2.41 (0.80 to 7.30) | 2.71 (0.79 to 9.27) | 2.54 (0.84 to 7.73) | 2.62 (0.85 to 8.08) | |
| Desogestrel | 1.57 (0.55 to 4.47) | 1.11 (0.38 to 3.23) | 1.20 (0.40 to 3.57) | 1.98 (0.70 to 5.57) | 1.37 (0.47 to 4.06) | 1.51 (0.50 to 4.57) | |
| Progestogen only | 0.57 (0.21 to 1.58) | 1.15 (0.54 to 2.49) | 1.23 (0.52 to 2.91) | 0.68 (0.23 to 2.04) | 1.36 (0.60 to 3.05) | 1.48 (0.60 to 3.65) | |
Adjusted for current cigarette smoking, body mass index, blood pressure measured in previous year, diabetes mellitus, angina, hypertension, family history of ischaemic heart disease, and use of other drugs.
Interview data used when disagreement on current exposure or not, GP record data used when disagreement on type of oral contraceptive.
Table 3 also shows the odds ratios from the “full” model—that is, adjusted for all the factors in the “select” model, plus all additional variables examined in the univariate analysis (table 1). The odds ratios are all higher than for the select model but with wider confidence intervals. Adjusted odds ratios for third generation versus second generation users were as follows: from patient interview data 2.06 (0.77 to 5.50), from general practitioner record data 1.41 (0.54 to 3.70), and from interview and general practitioner data combined 1.78 (0.66 to 4.83).
Discussion
Myocardial infarction is rare in this age group of women. The point estimates suggest that the risk of myocardial infarction is increased slightly by the use of oral contraceptives, although adjustment for a large number of confounders introduced some uncertainty in the risk estimates, as shown by wide 95% confidence intervals. The point estimates were greater for third than for second generation oral contraceptives, but the differences observed were not significant.
Smoking was an important risk factor (the population attributable fraction being 73%), and other cardiovascular risk factors were also important. In line with the results from the WHO study1 and the transnational study,3 among those who were current users of oral contraceptives the absence of a blood pressure check in the year preceding the index woman’s myocardial infarction showed a positive association with myocardial infarction, although this was not significant (odds ratio 2.07; 0.81 to 5.30). The positive association between multiparity and myocardial infarction has been reported before7 as has that with pre-eclampsia.1 The beneficial effect of consumption of alcohol is in keeping with results of other studies,8 as is the benefit of exercise and being in employment in the past year.9
Potential bias
Possible weaknesses of this study were low interview rates, misclassification of exposure, and selection bias. We interviewed 73% of the women who survived myocardial infarction but achieved proxy interviews for only 20% of those who died, which may have introduced a bias if, for example, certain types of oral contraceptive were particularly liable to cause sudden death from myocardial infarction. This does not seem likely as oral contraceptives were not found to be a significant risk factor in this study, but it cannot be entirely discounted. Recall bias may have occurred because we asked interviewees to recall contraceptive habits. The adverse publicity about third generation oral contraceptives generated by the “Dear Doctor” letter from the United Kingdom Committee on Safety of Medicines in October 1995 may have biased responses to our questions, although, whenever possible, interviewees were blinded to the main objective of the study. Also, we provided photographs of all marketed oral contraceptives to increase the accuracy of recall. Furthermore, we validated the exposure data from written records, and the κ score for agreement in exposure data between the two sources was 0.8 for both cases and controls. As shown in tables 2 and 3 there were some differences in odds ratios with the two different sources, but overall the measures of effect were similar, and the “compromise” odds ratios represent our best estimate of the true effect. Some effect of selection bias is possible because controls were women who responded to a request to participate, and such women may not be representative of the population, but on average it was necessary to approach only 6.6 (range 4-26) of the closest age matched controls.
Relevance of results
The importance of the MICA study is that it had sufficient power to examine the effects of oral contraceptives with differing progestagen content on the incidence of myocardial infarction with very close age matching between cases and controls. Our results do not agree with those of the European transnational study,3 although the United Kingdom results from that study and the present study show considerable overlap and are compatible within the bounds of random error. Other studies have been hampered by small numbers of participants exposed to oral contraceptives but generally their results also suggest that there is no difference in risk of myocardial infarction between different preparations.1,2,10 Although the WHO study reported an adjusted odds ratio of 5.01 (2.54 to 9.90) for European oral contraceptive users overall compared with non-users,1 and this contrasts with an odds ratio of 1.40 in this study, the populations studied were quite different. The WHO study recruited 55% of their cases from Eastern Europe, where there may be inadequate screening for risk factors among oral contraceptive users, and it is pertinent that the odds ratio for the subset of United Kingdom users was 2.10 (0.63 to 7.07), which is similar to our results. Comparison of the MICA study with similar studies carried out in the 1980s, which found odds ratios for current use of oral contraceptives varying between 1.2 and 3.5,11,12 is difficult because of changes in the formulations of the pills and because of probable improvements in routine medical care. The fact that most women with myocardial infarction in the present study were not taking any oral contraception suggests that doctors were cautious in their prescribing habits for older women who might be at risk. Our results for smoking and other cardiovascular risk factors agree with those of all the recent studies on this topic. These factors are of overriding importance in the aetiology of myocardial infarction in this age group and in comparison the use of oral contraception makes little or no difference.
Figure.
Case accrual and interview rates (*30 women died at time of myocardial infarction and five died subsequently)
Acknowledgments
We thank all the women and next of kin who agreed to be interviewed, hospital records staff, general practitioners and surgery staff, and those who worked on the MICA project as follows: National Centre staff: Ann Arscott (national project manager), Jan Phillips (administrator), Susan Jay (quality control officer), Greg Gallagher and Caroline Keal (data entry clerks), Annette Kinsella (data programmer), Gretl McHugh (epidemiological support), Gill Mein and Deborah Curle (study advisors); Southampton Centre staff: Penny Nettelfield, Julie Pring, Rachael Green, Lesley Foulkest, Julie Richardson, Shona Burman-Roy, Jo Lockett, Liz Bale, and Yvonne Egan-Davidson (research assistants), Dr Derek Waller (local diagnostic committee); Manchester Centre staff: Mr Harvey Chant (medical coordinator), Jane Richardson (project manager), Jill Carley, Linda Robinson, Helen Shea, Tamsin Warner, Joanne Watson, and Heather Youngson (research assistants), Jane Booth (secretary), Dr Nicholas Brooks (local diagnostic committee); Glasgow Centre staff: Hilary Davison (project manager), Edith Hamilton, Sheena Mitchell, Susan Brogan, and Margaret Carlin (research assistants), Anne Currie (secretary), Professor Ross Lorimer (local diagnostic committee). Newcastle Centre staff: Judy Bland and Lyn Cassidy (research assistants), Dr Gary Ford (local diagnostic committee); National Diagnostic Committee: Dr Richard Jones, Professor David de Bono; Scientific Review Board: Miss Angela Mills, Professor Martin Vessey, Professor Michael Langman, Dr Kenneth MacRae, Professor David de Bono.
Footnotes
Funding: Unconditional grant from NV Organon and Schering AG.
Competing interests: None declared.
References
- 1.WHO Collaborative Study of Cardiovascular Disease and Steroid Hormone Contraception. Acute myocardial infarction and combined oral contraceptives: results of an international case-control study. Lancet. 1997;349:1202–1209. [PubMed] [Google Scholar]
- 2.Sydney S, Pettiti DB, Quesenbery CP, Klatsky AL, Ziel HK, Wolf S. Myocardial infarction in users of low dose oral contraceptives. Obstet Gynecol. 1996;88:939–944. doi: 10.1016/s0029-7844(96)00351-1. [DOI] [PubMed] [Google Scholar]
- 3.Lewis MA, Heinemann LAJ, Spitzer WO, MacRae KD, Bruppacher R.on behalf of Trans-National Research Group on Oral Contraceptives and the Health of Young Women. The use of oral contraceptives and the occurrence of acute myocardial infarction in young women Contraception 199756129–140. [DOI] [PubMed] [Google Scholar]
- 4.Dunn NR, Thorogood M, de Caestecker L, Mann RD. Myocardial infarction and oral contraceptives, a retrospective case-control study in England and Scotland (MICA study) Pharmacoepidemiol Drug Safety. 1997;6:283–289. doi: 10.1002/(SICI)1099-1557(199707)6:4<283::AID-PDS270>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 5.McAlpine R, Pringle S, Pringle T, Lorimer R, MacDonald T. A study to determine the sensitivity and specificity of hospital discharge diagnosis data used in the MICA study. Pharmacoepid Drug Safety. 1998;7:311–318. doi: 10.1002/(SICI)1099-1557(199809/10)7:5<311::AID-PDS371>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 6.WHO Collaborative Study of Cardiovascular Disease and Steroid Hormone Contraception. A multinational case-control study of cardiovascular disease and steroid hormone contraceptives. J Clin Epidemiol. 1995;48:1513–1547. doi: 10.1016/0895-4356(95)00516-1. [DOI] [PubMed] [Google Scholar]
- 7.Oliver MF. What is the difference between men and women? In: Oliver MF, Vedin A, Wilhelmsson C, editors. Myocardial infarction in women. Edinburgh: Churchill Livingstone; 1986. pp. 215–221. [Google Scholar]
- 8.Tunstall-Pedoe H, Woodward M, Tavendale R, A’Brook R, McCluskey MK. Comparison of the prediction by 27 different factors of coronary heart disease and death in men and women of the Scottish heart health study: cohort study. BMJ. 1997;315:722–729. doi: 10.1136/bmj.315.7110.722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rich-Edwards JW, Manson JE, Hennekens CH, Buring JE. The primary prevention of coronary heart disease in women. N Engl J Med. 1995;332:1758–1766. doi: 10.1056/NEJM199506293322607. [DOI] [PubMed] [Google Scholar]
- 10.Jick H, Jick SS, Myers MW. Risk of acute myocardial infarction and low dose combined oral contraceptives. Lancet. 1996;347:627–628. doi: 10.1016/s0140-6736(96)91334-3. [DOI] [PubMed] [Google Scholar]
- 11.Rosenberg L, Palmer JR, Lesko SM, Shapiro S. Oral contraceptive use and the risk of myocardial infarction. Am J Epidemiol. 1990;131:1009–1016. doi: 10.1093/oxfordjournals.aje.a115592. [DOI] [PubMed] [Google Scholar]
- 12.La Vecchia C, Fransceschi S, De Carli A, Pampallona S, Tognoni G. Risk factors for myocardial infarction in young women. Am J Epidemiol. 1987;125:832–843. doi: 10.1093/oxfordjournals.aje.a114599. [DOI] [PubMed] [Google Scholar]