Abstract
RFID technology shows significant potential for transforming healthcare, yet few studies assess this potential. Our study measured the effectiveness of using RFID as a bed trigger: a tool to accelerate identification of empty beds. We made a small alteration in the discharge process to associate RFID tags with patients and created an RFID-based system that automatically determined discharge time. For each patient, we evaluated the difference in the discharge times recorded manually by the current process and the RFID-based system. The study was conducted on 86 patients over 2 months in 2 physically separate multi-specialty units. Compared to the preexisting process, the RFID-based system identified empty beds >20 minutes earlier 67% of the time with an average of 25 minutes and median of 9 minutes earlier. Hospital leadership defined an improvement of ~10 minutes as significant. With minimal investment, our small-scale study lead hospital leadership to begin planning RFID deployment.
Introduction†,‡
Radio-Frequency Identification (RFID) has dramatically transformed industries outside of healthcare by providing for tracking materials and supplies from production to distribution to stock on shelves1. Not surprisingly the promise of RFID has excited many hospital executives with the potential of RFID to track both supplies and patients in real time2, 3. Yet, at the time of our study we were able to find only three peer reviewed studies on RFID. These studies looked at using RFID for mass casualty disaster/disaster recovery, nursing shift exchange and linking patients to test results in emergency room with a reduction of time to ICU admission4–6. We were unable to find any other studies examining workflows required to integrate and support the technology, demonstrations of increased efficiencies in tracking patients or supplies or specific uses that RFID might excel at, such as patient location. One potential reason for the limited number of peer reviewed RFID studies may be cost. An extensive investment is required to have the system in place for evaluation. Commercial RFID systems for patient, bed and supply tracking cost in the millions due to software, interfaces, reader deployment and the like. In addition, it is hard to test something that will cost millions to install1.
At Mount Sinai, the Chief Operating Officer had previously expressed a great deal of interest in RFID but felt the cost was prohibitive and was particularly concerned with workflow integration. He specifically challenged us to demonstrate that RFID could be integrated into an existing workflow and selectively deployed to solve previously identified critical problems at Mount Sinai Hospital†
Mount Sinai, like many hospitals, is faced with the challenge of bed turn around time, the period of time from discharge to new admission7. Prolonged turn around times have caused emergency rooms to become congested, created patient safety issues with sick patients being cared for in the emergency room when they need to be on a hospital floor, and patient dissatisfaction8–10.
Bed turn around time is dependent on identification of empty beds. However, a study by Advisory Board of member clients showed that identification of empty beds can be delayed by as much as 2.4 hours7. For purposes of this paper we define a bed trigger as any tool that accelerates identification of empty beds.
In this paper, we describe a study that was designed to measure the effectiveness of using RFID technology on a small scale to accelerate identification of empty beds1. For our study, we made a small alteration in the discharge process to associate an RFID tag with the patient and created an RFIDbased software system that automatically determined the discharge time for the patient. For each patient in the study, we determined the discharge times for the current, manual discharge system and the RFID-based discharge system and then evaluated the difference between the two. Our objective was to provide the information needed to make a decision on whether to adopt this technology and automate the bed trigger component of the patient discharge process.
Background
Mount Sinai Medical Center is a tertiary academic center with 1171 hospital beds and approximately 51,000 discharges a year. Prior to our study, identifying empty beds was a manual process. Empty beds were previously identified by observations of or reports to the business associate (BA) (i.e., ward clerk) that the patient had been discharged and left the floor. The BA entered this time into the ADT (Admission Discharge Transfer system) and notified housekeeping. In other words, the BA was the bed trigger.
Before we began the study, there was a perception among the Study Hospital staff that there was, on occasion, a significant time interval between the discharged patient leaving the unit and the recording of the event in the clinical information system. Multiple explanations for this delay were thought possible such as the BA was too busy to note the discharged patient leaving. To perform some duties, the BA must leave the nurses’ station. Even while at the nurses’ station, the BA sometimes becomes consumed in tasks and is unable to make observations for periods of time. Other explanations for delay include shift changes, patients awaiting personal transportation, and delays in discharge process itself.
Method
The study requirements fell into three broad categories: hospital operational requirements, patient confidentiality/privacy, and study requirements to conduct evaluation.
Hospital Operational Requirements:
Being a time-limited research study, the project could not be permitted to significantly disrupt existing patient care nor could it involve extensive training of staff and education of patients. The next section describes existing and study process.
Existing Process: During the discharge process in the hospital, the patient is identified as a discharge possibility during the morning nursing rounds. The Provider enters Discharge Order in the Computerized Physician Order Entry (CPOE) system and the nurse retrieves a blank Discharge Instruction Form and fills out the details. The nurse also educates the patient regarding the discharge instructions and gives them a copy of the form. The patient leaves floor and hospital, possibly (but not always) in wheelchair. The BA, who sits in the nursing station near the unit exit, observes the patient leaving, records the time on a manual log sheet, enters the discharge in the ADT system, and informs housekeeping. Housekeeping cleans the room and uses an interactive voice response (IVR) system to indicate that the room/bed is now clean and available.
Study Process: The manual discharge process remains the same. However, we introduced an RFID-based discharge process that ran simultaneously as follows:
When the nurse fills out the Discharge Instructions form; he/she selects an envelope containing an RFID tag and records the unique tag number from the envelope on the top of the Discharge Instruction form. At the time that the nurse educates the patient regarding discharge instructions, he/she gives them the Discharge instructions form with the associated envelope containing the RFID tag and directs them to drop off the envelope at the security desk when they leave the hospital. A label on each envelope explained that the envelope was part of a hospital study to measure ways of improving the efficiency of the hospital. Upon exiting the floor, the RFID reader recorded the RFID tag number and the patient departure time.
A number of RFID Tags were prepared each morning by the DPPL (Discharge Project Process Leader), one of the authors. The DPPL was a member of the research team who was authorized as part of her job to handle hospital documents and access various clinical applications A single active RFID tag was placed in an envelope and the tag number was written on the outside of the envelope. At the nurses’ station, each discharged patient was identified, and the envelope with RFID tag was clipped to the patient’s discharge form in the patient folder.
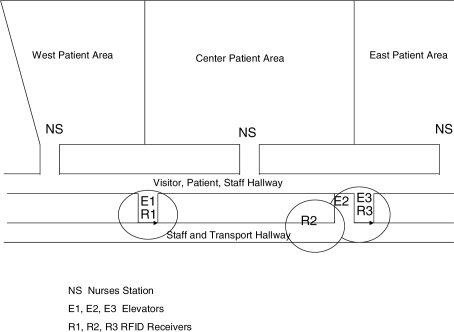
The RFID receivers on each floor had to be placed so that the patient’s RFID tag was not detected while the patient is in the hospital unit, but was detected as the patient exited the unit. The patient must pass the nurses station to exit the patient wing. Elevators are the non-emergency exits on the upper floors of the building. There is a hallway approximately 10 feet long that leads to the main Visitor/Patient hallway. There are two elevator bays, each with four elevators, on this hallway. There is a Staff/Transport hallway that is parallel to the Visitor/Patient hallway that is used to transport patients in gurneys. The patient wings involved in the case Study were the east and west hospital units on the same floor (see figure 1).
Figure 1.
Layout of patient wards with areas and placement of RFID receivers.
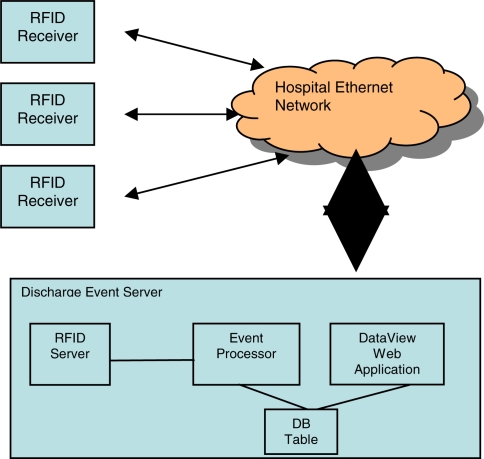
We placed three RFID receivers to detect patients as they exited the floor, from either the East or West patient wings. One RFID receiver was placed in each of the elevator areas off of the main Visitor/Patient hallway. Another RFID receiver was placed in the hallway adjacent to the transport elevator off of the Staff/Transport hallway. The read field of each RFID receiver was adjusted to limit RFID reads to the immediate vicinity of the RFID receiver. Tag detection was limited to about 30 feet. The three RFID receivers were connected to the hospital’s Ethernet LAN by Power over Ethernet connections. RFID tags send a signal that contains the identity of the tag; when the RFID receiver receives this signal, it sends an IP packet to the server software. The server software filters the incoming stream and stores the resultant stream in a temporary database table. Server applications poll this temporary database table for unprocessed events. The Event Processor component uses an internal server software API to poll the temporary database table and to store the event data in a database, the EventDB, table maintained by our application logic. The DataView application polls the EventDB table to determine those events which represent a patient discharge detection event. The RFID Server software handled the interface to the RFID receivers, including the communications protocol, configuration, and management for the receivers. The term server is used in the strictest sense, as a laptop housed the server software.
We worked to minimize the costs associated with this study, including no development of interfaces or networking of devices. The biggest decisions affecting cost was which RFID technology, active or passive11. We initially explored using passive RFID tags and associated receivers. This technology was very appealing to the hospital because of the low cost of the tags and the ease with which the passive tags could be printed and attached to the discharge instructions, something every patient takes home from the hospital. However, we reached the conclusion that this technology is not suitable for tracking people or assets. It is difficult to read a passive RFID tag that is held close to the human body. In order to guarantee a high tag-read rate, patients would have to hold the tags out from their bodies as they move through the receiver. It is unrealistic to require such cooperation from patients and would have disrupted workflow significantly to instruct each patient to do so. In addition, the physical dimensions of the passive RFID receivers to be deployed at the patient wing doorways would create a safety hazard because they would preclude two gurneys from passing through the doorway simultaneously. This issue turned out to be insurmountable with existing passive RFID technology so we moved our focus to active tags.
Once it was decided to use active RFID technology, the main issue became the cost of the tags. Typical active RFID tags cost upwards of $25, making the solution too expensive. Since the tags most likely cannot be sterilized, the tag cost becomes the main per-patient expense. We found an RFID vendor that offered a single-use tag with limited battery life of about two months for an economical cost of $10. The RFID tag was placed in an envelope to eliminate the possibility of the patient touching the tag. In this way, we could reuse tags if necessary.
We needed to modify the software to minimize cost. We were given access to an internal API of the vendors RFID server software; we needed the general RFID read hit data and not the applications bundled on the server. The general RFID read hit consists of a triple: RFID tag ID, RFID receiver ID, and a time value corresponding to the time of the RFID read hit. The RFID server software also performed some intelligent filtering of the RFID read hits. For example, if a patient stood in the same physical spot for several minutes, we would receive a number of RFID read hits with the same RFID tag ID and RFID receiver ID. It is unnecessary to process all of these RFID read hits: only the first one in each series of duplicate read hits are needed. The general RFID read hits are passed to the Event Processor component. The Event Processor stores all hits into a relational database and executes an algorithm to determine which read hit should be classified as a discharge event. A read hit classified as a discharge event is marked as such in the database. The last component is a web application that allows a person to view all RFID read hits and discharge events by date. The data can be viewed using a web browser from any computer that has network access to the Discharge Event Server.
Study Requirements:
The metric used to evaluate the efficacy of RFID as a bed trigger was to compare the manually recorded discharge time in ADT vs. the discharge time detected by the RFID-based system. Our only restriction was that we had enough budget to conduct the study on 2 of 30 hospital units. The criteria for selecting the 2 units were: number of discharges per day, timing of discharges, number of ambulatory discharges, and number of ama (against medical advice) discharges/elopement. We heuristically determined that 240 discharges over 2 months were required to detect differences between manually recorded and RFID discharge times. There was no formal calculation of sample size. Discharges had to be predominantly ambulatory as transportation for bed-bound patients through ambulettes is a noticeable event with well-recorded times. A minimum number of ama/elopments was needed to ensure enough patients for observation as ama/elopements bypass the official discharge process and would therefore never be given RFID tags. Timing of discharges was only important in that the DPPL had to be present to make observations during the study.
The data used for this decision was internal data the DPPL had been collecting for her overall discharge project. Based on the experience of a hospital staff member very familiar with the operations of the chosen patient units, the selected units were considered to be well run.
Confidentiality Requirements:
Linking information between the ADT system and the RFID scanner without interfaces (see minimal cost) and addressing patient confidentiality and human subject concerns provided some unique challenges. Patients were unaware of the study and not to be contacted.
Yet, the patient identifier was critical to being able to compare the BA recorded discharge time in the ADT system to the RFID time stamp. The patient identifier allowed the DPPL to examine the housekeeping database to catch those patients who were not given a tag or whose tag was not detected leaving the floor. The DPPL recorded the association between the hospital patient identifier and the RFID tag number. The DPPL was serving the function of interfaces and software in a finished product.
The patient identifier was neither stored on the RFID tags nor on the scanner for reasons of patient confidentiality and human subject concerns. The alternative would have required a lengthy consent process that would have significantly disrupted patient flow. Patient identifiers were not shared with any other member of the research team and were permanently deleted at the end of each day.
Results
The total study cost was approximately $12,000. The Study took place over a 16 day period on one hospital unit and a 7 day period on the other unit and not the planned 2 months. Data was collected for a total of 86 patients. Five of the 86 RFID tags given to patients were never read. None of the 5 tags were found left in the room by patients. Due to the protocol that was used, we were not able to contact those patients to investigate what might have gone wrong with those tags.
The key metric is the difference in time between 1) the discharge time recorded in the ADT using the current discharge detection method and 2) the discharge time detected by the RFID-based system. The RFID-based discharge detection system detected patient discharge an average of 25 minutes sooner than the manual system (see table 1). A paired t-test shows that the true mean difference falls between 17 and 33 minutes, with confidence level 95%.
Table 1.
Difference Between Manually-Entered ADT Time and RFID-Stamped Time
| Minimum | 0 |
| Maximum | 179 minutes |
| Mean | 25 minutes |
| Median | 9 minutes |
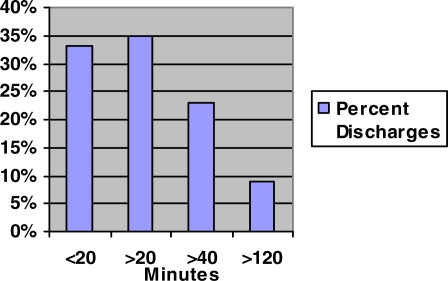
In over 67 % of the cases, the discharge time difference was 20 minutes or more. Specifically: 35% were over 20–40 minutes, 23% 40–120 minutes and over 9% were over 120 minutes (see figure 3).
Figure 3.
Delay in Minutes: ADT vs. RFID
Discussion
The aim of our study was to use a smallscale deployment of RFID with minimal investment ($12k) to assess RFID as a bed trigger to accelerate identification of empty beds. When compared to the existing manual process by the BAs in 2 (known to be) well run units, there were significant differences between RFID time stamp and the manually recorded time in ADT. There was a mean difference of 25 minutes and a median of 9 minutes with 67% greater than 20 minutes. Another RFID study showed similarly promising results in decreasing admission time from ED to ICU6.
Data collection was stopped by the research team earlier than planned because of our surprisingly positive results. Our original prediction was that differences in discharge time per patient would be infrequent as well as small. Observed differences in discharge time were very frequent and clearly significant. Since, the DPPL team member had to spend a significant amount of time on the units on data collection days; the study was stopped after collecting data on 86 patients.
None of the nurses or staff objected to the study as being intrusive. Many staff stated that they would be very happy to have anything that would make their job easier and the information more accurate. Surprisingly, there was no observer effect in which manually recorded discharge times improved because of monitoring.
The study highlights many of the challenges faced in assessing a commercial technology on a small scale. As noted in methods, many limitations were overcome including how to best deploy and test a solution without purchasing it. Since half of IT functionality is frequently not used, perhaps vendors should make versions of their systems suitable for testing and evaluation.12
The study had significant limitations. The research was conducted in only 2 of 30 hospital inpatient units at one hospital during the summer months of June and July 2006. Since admission and discharge rates are subject to seasonal variation, it would have been interesting to conduct our study across multiple seasons. In the 2 multi-specialty units both housestaff and NP’s (Nurse Practioner) cared for patients. RFID tagging was not employed during the night or weekends because of DLLP availability.
Ironically one limitation was the study’s success. The original study design was meant to have phases with increasing amounts integration. For example, the second phase would have replaced the DPPL on the floor with having the BA produce the RFID tags. A later phase would include an interface to ADT to automatically record the time from the RFID scanner. However, leadership was so impressed with the initial results, the study was halted.
The hospital’s goal for bed trigger is 10 minutes after the patient leaves the floor. In our study 67% of the time the manual process was 20 minutes or more behind the actual departure time recorded by RFID., with a nearly 10% chance of a patient discharge going unobserved for over 2 hours. This situation is simply unacceptable to both the hospital and patients awaiting beds in the emergency room8, 10. A greater than 2 hour delay in identifying an empty bed exceeds reported maximum time for bed turn around7. Based on these results, hospital leadership decided to proceed with implementation planning of the RFID-based bed trigger as soon as possible. The project was subsequently approved. Space limitations prevent presentation of the project plan, cost analysis, and return on investment required.
Conclusions
We demonstrated the use of RFID as a bed trigger on a small scale with minimal investment. The challenges we faced demonstrate the hurdles to be overcome in assessing commercial technology in real world settings. The experiment was so successful that the study was stopped prematurely and leadership decided to begin planning for deployment.
Figure 2.
System Configuration
Footnotes
Acknowledgements: COO Wayne Keathley for vision and budget. VP Eric Waters for tireless assistance with hospital operations.
IBM Research provided the server, some research software, and integration of the RFID system.
References
- 1.Dempsey M. Weaving through the hopes and hype surrounding RFID. Biomed Instrum Technol 2005;Suppl:19–22. [PubMed]
- 2.Radio-frequency identification: its potential in healthcare Health Devices. 2005;34(5):149–60. [PubMed] [Google Scholar]
- 3.Wicks AM, Visich JK, Li S. Radio frequency identification applications in hospital environments. Hosp Top. 2006;84(3):3–8. doi: 10.3200/HTPS.84.3.3-9. [DOI] [PubMed] [Google Scholar]
- 4.Fry EA, Lenert LA. MASCAL: RFID Tracking of Patients, Staff and Equipment to Enhance Hospital Response to Mass Casualty Events. AMIA Annu Symp Proc 2005:261–5. [PMC free article] [PubMed]
- 5.Huang PJ. The Development of a Patient-Identification-Oriented Nursing Shift Exchange Support System Using Wireless RFID PDA Techniques. AMIA Annu Symp Proc. 2005:990. [PMC free article] [PubMed] [Google Scholar]
- 6.Chen CI, Liu CY, Li YC, Chao CC, Liu CT, Chen CF, et al. Pervasive Observation Medicine: The Application of RFID to Improve Patient Safety in Observation Unit of Hospital Emergency Department. Stud Health Technol Inform. 2005;116:311–5. [PubMed] [Google Scholar]
- 7.Advisory Board Company. Leveraging IT to Optimize Hospital Throughput . The CIO's Leadership Agenda. Washington, DC: The Advisory Board Company; 2005. 2005. pp. 14–15.pp. 20 [Google Scholar]
- 8.Richardson LD, Asplin BR, Lowe RA. Emergency department crowding as a health policy issue: past development, future directions. Ann Emerg Med. 2002;40(4):388–93. doi: 10.1067/mem.2002.128012. [DOI] [PubMed] [Google Scholar]
- 9.Schafermeyer RW, Asplin BR. Hospital and emergency department crowding in the United States. Emerg Med (Fremantle) 2003;15(1):22–7. doi: 10.1046/j.1442-2026.2003.00403.x. [DOI] [PubMed] [Google Scholar]
- 10.Simmons FM. CEU: Hospital overcrowding: An opportunity for case managers. The Case Manager. 2005;16(4):52–54. doi: 10.1016/j.casemgr.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 11.Kabachinski J. An introduction to RFID. Biomed Instrum Technol. 2005;39(2):131–4. doi: 10.2345/0899-8205(2005)39[131:AITR]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 12.Kuperman GJ, Leavitt MK, McCall CW, Patterson NL, Wilson HJ. Nashville, TN: Hanley & Belfus, Inc; 1997. Panel: Integrating Informatics into the Product: The CEO’s Perspective. In: 1997 AMIA Annual Fall Symposium; 1997. [Google Scholar]