Abstract
Background
Depressive symptoms are a well-known predictor of mortality in patients with heart failure (HF). Positive spousal support is associated with improved outcomes in HF patients. However, the impact on survival of having a spouse in the context of depressive symptoms is unknown.
Objective
To determine the impact of marital status on event-free survival in patients with HF with and without depressive symptoms.
Methods
Depressive symptoms were assessed using the Beck Depression Inventory-II (BDI-II) in HF patients who were followed for 4 years to collect data on mortality and hospitalizations. Patients were grouped into two groups based on the presence and absence of depressive symptom using the standard cut-point score of 14 on the BDI-II. Kaplan-Meier and Cox regression analyses were used to compare event-free survival for married and non-married patients who were stratified by presence or absence of depressive symptoms.
Results
Of a total of 166 patients, 56% were married and 33% had depressive symptoms. Levels of depressive symptoms were similar between married and non-married patients (10.9 vs. 12.1, p=0.39). Married patients experienced longer event-free survival than non-married patients (p <0.008). Even with stratification by presence or absence of depressive symptoms, married patients experienced longer event-free survival than non-married patients (p=0.012).
Conclusions
Patients with a spouse had longer event-free survival than patients even in the context of depressive symptoms. Interventions aimed at improving clinical outcomes should identify and reinforce alternative social support networks for non-married patients.
Keywords: Marital status, Depressive symptoms, Heart failure, Mortality, Hospitalization
Background
More than 5 million Americans currently suffer from heart failure (HF).1 Hospitalization rates have increased 174% during the last two decades.1 According to latest data from the Framingham study, the one-year age adjusted mortality rates for men and women with HF are 28% and 24 %, and the five-year mortality rates are 59% and 45%.2 Accumulating evidence suggests that depressive symptoms are an important independent risk factor for hospital readmission and mortality in patients with HF.3–5 It is estimated that one patient in every five with HF suffers from clinical depression.5 In one study, approximately 60% of HF patients with major depressive symptoms were readmitted to the hospital within one year of discharge for an exacerbation of HF.3 HF patients with depressive symptoms had three times greater risk of readmission and two times greater risk of death within one year compared to those without depressive symptoms.3
Social support is another important predictor of survival among individuals with coronary heart disease (CHD).6–8 Positive social support is associated with improved quality of life9, 10 while poor or absent social support is associated with increased readmission and mortality in patients with HF.11–13 Having a spouse often is an indication of the highest available level of social support because spousal caregivers typically live with patients and provide long-term commitment with continuous face-to-face contact. Most studies of social support have focused on subjectively perceived social support or the availability of social support 10, 14, 15 and relatively few studies have examined the effects of single marital status, which is often an indicator of poor or absent spousal support.16 Chin and Goldman followed 257 patients hospitalized with HF and found that single patients were at 2.1 times higher risk for readmission or death within 60 days compared to married patients.16 Although social support decreases risk of readmission and mortality among patients with HF, it is unknown whether having a spouse has a positive effect on survival in patients with depressive symptoms.
There are two possible ways that social support or marital status might exert an effect on outcomes in depressed patients: 1) a buffering effect in which social support or being married buffers the distress of depression and improves outcomes, and 2) a main-effect model in which there is a direct effect of social support or marital status on depression and/or outcomes. In the buffering model, social support or marital status protects individuals from the potentially pathogenic influences of depression.17, 18 In the main-effect model, social support or marital status is beneficial in improving outcomes in spite of the stress of depression; there are no statistical interaction effects between social support and depression in the main-effect model.19 In two recent studies, a potential buffering effect of perceived social support on cardiac mortality after acute myocardial infarction (AMI) in patients without depressive symptoms was noted.7, 8 However, it is not possible to generalize this finding to patients with HF. Based on our previous work, we hypothesize that marital status plays a direct role and thus supports that main-effect model.
Therefore, the purpose of this study was to determine the impact of marital status on event-free survival in patients with HF with and without depressive symptoms. The specific aims were (1) to examine whether depressive symptoms and marital status are independent predictors of event-free survival, (2) to examine whether there is an interaction effect between depressive symptoms and marital status on event free survival, (3) to compare the impact of marital status on event-free survival between patients with depressive symptoms and patients without depressive symptoms, and (4) to determine whether marital status is an independent predictor of event-free survival after controlling for depressive symptoms.
Methods
This was a prospective, longitudinal study in which patients with HF were followed for up to four years after their depressive symptoms were assessed to collect data on death and hospitalization. We included patients who had a confirmed diagnosis of chronic heart failure, no history of AMI within 3 months, and who were on stable doses of HF medications. We excluded patients who had HF from valvular or peripartum etiology, were referred for heart transplantation, had terminal illness such as cancer, or had poorly-controlled diabetes or end-stage liver or renal disease. We recruited patients from outpatient clinics including an academic medical center in central Kentucky.
Three major prospective studies were conducted simultaneously with the same inclusion and exclusion criteria as part of the research profile of the Research and Intervention for Cardiopulmonary Health (RICH) Heart Program at the College of Nursing, University of Kentucky. At this time, trained research nurse screened medical charts for all three studies. After review of the 1472 medical charts between January 2004 to December 2006, 671 patients (45.6%) were found not to be eligible. Of the 801 eligible patients, 274 patients (34%) immediately refused to participate and 240 patients considered participation but ultimately did not agree. Therefore, 259 patients (32.3%) participated in one of the three studies in the RICH Heart Program. In the current study, 166 unique patients were included as we excluded patients who participated in more than one study during the study period. This participation rate is similar to that of other studies of patients with HF, especially when older patients are recruited.20
Measures
Depressive symptoms were assessed using the Beck Depression Inventory-II (BDI-II). The BDI-II is a well-established instrument for the measurement of depressive symptoms that has a total of 21 items rated on a scale from 0 to 3.21–24 The total score can range from 0 to 63. Patients who score 14 or above are considered to have depressive symptoms.22 A higher total score indicates more severe depressive symptoms. The BDIII is a valid and reliable instrument, and it has been used to predict mortality and hospitalizations in CHD patients and patients with HF.4, 7, 25, 26 Reliability of this instrument was acceptable as Cronbach's alpha was .88 in this study.
Marital status was assessed from patient interview. Marital status was initially collected in five categories including married, single, widowed, divorced, and cohabitated. This variable was dichotomized into married and non-married groups. The unmarried group consisted of single, widow, and divorced patients. The married group included married and cohabitating patients.
The outcome variable in this study was event-free survival. We used a combined end-point of mortality or all cause hospitalization defined as the duration in days from baseline assessment to the first hospitalization or death from any cause. We collected date and reasons for hospitalization and death by reviewing hospital records, making monthly follow-up phone calls, and by obtaining death certificates.
Demographic (i.e., gender, age, ethnicity, marital status, education, income) and clinical characteristics (i.e., left ventricular ejection fraction, medication, co-morbidity, New York Heart Association class) of patients were collected by reviewing medical charts using a structured questionnaire. Education levels were categorized into two groups (i.e., less than or a high school diploma received vs. greater than high school). Financial status was assessed using one item that asked financially how well the household lives on the income available and rated on 3-point Likert scale (1 =having more than enough to make ends meet, 2 = having enough to make ends meet, or 3 =having not enough to make ends meet).
Procedure
After approval of the Institutional Review Board, trained nurse researchers from the RICH Heart Program, confirmed the eligibility of patients who were referred to the study by doctors or nurse practitioners by screening medical charts with approval of waiver for the Health Insurance Portability and Accountability Act. Eligible patients were contacted at their clinic visit or by telephone. Trained nurse researchers explained the studies to eligible participants and obtained signed informed consent and compliance with the Health Insurance Portability and Accountability Act was achieved. Participating eligible patients were assisted to complete all study questionnaires; the questionnaire was read to patients who had difficulty reading. The patients were carefully questioned by a trained research nurse to determine their New York Heart Association (NYHA) functional classification. Demographic and clinical characteristics were collected by patient interview and by reviewing patients' medical charts using a structured questionnaire. After completion of questionnaires, patients were asked to record their hospitalization history in a log book. They were also informed that they would be followed by monthly phone calls for one year. We collected re-hospitalization history by monthly phone follow-up with patients for one year but chart reviews were continued to obtain data on hospitalization for up to four years. A trained research nurse identified and validated all cause of admission and death using hospital records, healthcare provider and family interviews, death certificates and review of count death records.
Data analysis
Patients were grouped into presence (n = 55) and absence (n = 111) of depressive symptom groups and into groups of married (n = 93) and non-married (n = 73). The Kaplan-Meier survival analysis with a log rank test was used to compare overall survival time to the combined endpoint of mortality or hospitalization between presence and absence of depressive symptoms groups, between married and non-married groups, and between married and non-married groups who were stratified by presence or absence of depressive symptoms. Cox proportional hazard regression modeling was used to examine the interaction effect of depressive symptoms and marital status while controlling for age, gender, education, and financial status. The Cox proportional hazard regression was also used to predict outcomes based on having a spouse while controlling for age, gender, education, financial status, NYHA class, ejection fraction, and depressive symptoms. All analyses were conducted using SPSS, version 15.0 (Chicago, IL).
A power analysis was conducted prior to data collection. With a significance level of 0.05 and at least 90 subjects in each depressive symptom and no depressive symptoms groups, the power of the log rank test to detect a significant difference in the combined endpoint distribution between the two subgroups was at least 74% if the no depressive symptom group had a 25% reduction in the combined endpoint relative to the depressive symptom group. With the addition of covariates in the Cox proportional hazards model, the power of the regression to detect significant group difference was greater than the power for the corresponding log-rank test given above. Power estimates were obtained using NQuery Advisor.27
Results
Patient characteristics
A total of 166 patients with HF participated in this study. The mean age of patients was 61 years old (SD = 11.4) and 69% were male. Most patients (86%) were white. Mean ejection fraction was 35% (SD =14.9) and 62% of patients were classified as NYHA class III or IV.
A total of 33% of patients had depressive symptoms (BDI score > 13). Patients who had depressive symptoms were more likely to be younger, less educated, less comfortable given their finances and more likely to take antidepressants than those without depressive symptoms (Table 1). Patients with depressive symptoms also had worse functional status than patients without depressive symptoms (NYHA class III–IV 83.3% vs. 50.5%, p < 0.001).
Table 1.
Characteristics of patients by depressive symptoms and marital status
| Characteristics | Depressed (n = 55) | Non-depressed (n = 111) | p-value | Married (n = 93) | Non-married (n = 73) | p-value |
|---|---|---|---|---|---|---|
| Age, years (M ± SD) | 57.8 ± 10.0 | 62.4 ± 11.7 | 0.012 | 61.1 ± 11.3 | 60.6 ± 11.6 | 0.792 |
| Male, gender (%) | 67.3 | 69.4 | 0.459 | 81.7 | 52.1 | < 0.001 |
| Education ≤ High school (%) | 44.5% | 63.6% | 0.032 | 48.9% | 53.4% | 0.675 |
| Finance – Having more enough | 9.4% | 33.3% | < 0.001 | 32.6% | 16.7% | 0.021 |
| Having enough | 54.7% | 52.3% | 52.2% | 54.2% | ||
| Having not enough | 35.8% | 14.4% | 15.2% | 29.2% | ||
| Married (%) | 54.5 | 56.8 | 0.458 | - | - | - |
| Depressive symptoms (M ± SD) | 21.8 ± 7.5 | 6.4 ± 3.7 | < 0.001 | 10.9 ± 8.4 | 12.2 ± 9.6 | 0.391 |
| Ischemic etiology (%) | 51.9 | 60.6 | 0.312 | 41.8 | 42.9 | 1.00 |
| Prior bypass surgery (%) | 30.2 | 34.2 | 0.370 | 39.6 | 24.7 | 0.470 |
| DM (%) | 42.6 | 46.4 | 0.648 | 42.9 | 47.9 | 0.532 |
| COPD (%) | 25.9 | 10.9 | 0.014 | 14.3 | 17.8 | 0.668 |
| Prior MI (%) | 61.5 | 52.7 | 0.188 | 56.7 | 54.2 | 0.437 |
| Ejection Fraction, % (M ± SD) | 36.9 ± 16.1 | 34.1 ± 14.3 | 0.261 | 33.7 ± 13.3 | 36.9 ± 16.6 | 0.182 |
| NYHA Class III or IV (%) | 83.3 | 50.5 | < 0.001 | 58.2 | 65.7 | 0.414 |
| Antidepressant use (%) | 37.0 | 19.1 | 0.020 | 19.8 | 31.5 | 0.103 |
| ICD (%) | 49.1 | 37.6 | 0.165 | 48.4 | 32.4 | 0.054 |
| Body mass index | 31.8 ± 8.1 | 31.7 ± 7.3 | 0.923 | 32.3 ± 7.6 | 30.9 ± 7.5 | 0.229 |
| Death (%) | 10.9 | 9.0 | 0.781 | 7.5 | 12.3 | 0.428 |
| Cardiac hospitalization (%) | 41.8 | 16.5 | < 0.001 | 19.8 | 31.5 | 0.085 |
| All cause hospitalization (%) | 60.0 | 29.1 | < 0.001 | 30.4 | 50.7 | 0.013 |
M= Mean; SD =Standard deviation; DM = Diabetes Mellitus; COPD = Chronic Obstructive Pulmonary Disease; MI=Myocardial Infarction; NYHA- New York Heart Association; ICD= Implantable Cardioverter Defibrillator.
Approximately half of the patients (56%) were married. Married patients were more likely to be male and more comfortable with their finances than non-married patients (Table 1). Levels of depressive symptoms were similar between married and non-married patients (10.9 vs. 12.1, p = 0.39).
There was no difference in the prevalence of depressive symptoms between married and non-married patients (32.3% vs. 34.2%, p = 0.087). Clinical characteristics (i.e., ischemic etiology, ejection fraction, and co-morbidities) of married patients were also similar to non-married patients (Table 1).
Follow up information
There was no attrition of study subjects during the follow-up period. There were 16 deaths (9.6%) and 41 (25%) hospital readmissions due to cardiac reason. The percentage of patients rehospitalized was higher in depressed patients than non-depressed patients (41.8% vs. 16.5%, p < 0.001) but there was no difference of death rate between depressed and non-depressed groups. Married and non-married patients had similar death rates and rates of cardiac hospitalization (Table 1).
Event-free survival
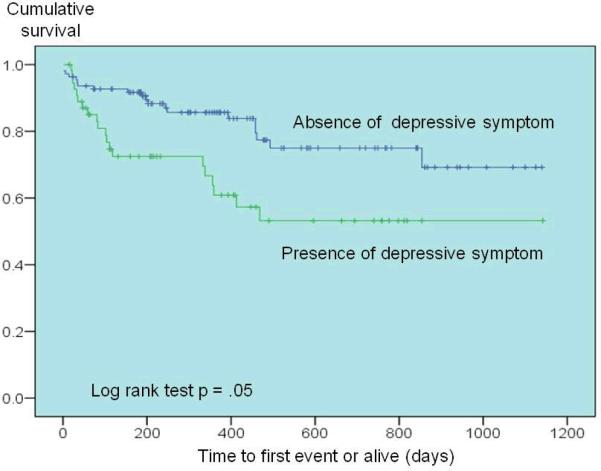
Kaplan-Meier analysis revealed that time-to-first-cardiac event (death or readmission due to cardiac reasons) was longer in patients without depressive symptoms (log rant test, p = 0.05) than patients with depressive symptoms. As indicated in Figure 1, at two years follow-up, approximately 70% of patients without depressive symptoms were event-free while only 50% of patients with depressive symptom were event-free.
Figure 1.
Event-free survival by depressive symptoms
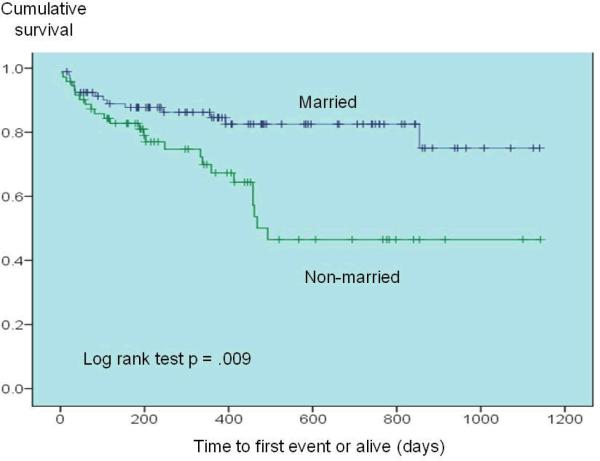
Married patients experienced longer event-free survival than non-married patients (log rank test, p = 0.009). As illustrated in Figure 2, the difference in event-free survival rate between married patients and non-married patients increased over the first year of follow-up, but increased dramatically between 12 months and 18 months. The event-free survival rate in married patients was 40% better than the event-free survival rate in unmarried patients at 18 months of follow-up.
Figure 2.
Event-free survival by marital status
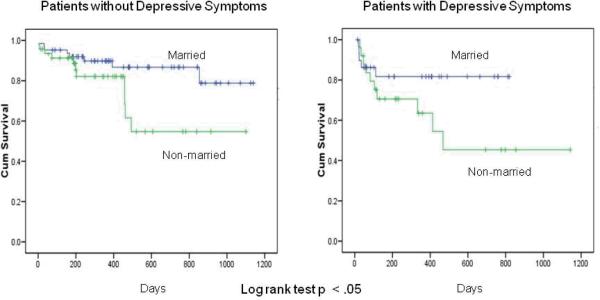
When we compared survival curves for married and non-married groups stratified by presence or absence of depressive symptoms, married patients experienced longer event-free survival than non-married patients regardless of the presence or absence of depressive symptoms (Figure 3, log rank test, p = 0.012).
Figure 3.
Event-free survival by marital Status with stratification of depressive symptoms
Kaplan-Meier analysis also showed that time to first event (death or readmission due to cardiac or non-cardiac reasons) was longer in patients without depressive symptoms (log rank test, p = 0.004) than patients with depressive symptoms as well as in married patients than non-married patients (log rank test, p = 0.001). Event –free survival was longer in married patients than non-married patients when depressive symptoms were stratified (log rank test, p = 0.001).
In a Cox proportional hazard regression model, when we controlled age, gender, education, financial status, ejection fraction, and NYHA class, both depressive symptoms and marital status remained independent predictors of event-free survival without demonstrating a significant interaction effect (Table 2). Patients with depressive symptoms were 3.7 times more likely to experience death or hospitalization than patients without depressive symptoms (p = 0.008). Patients who were not married were 3.86 times more likely to have such an event compared to the married patients (p = 0.001).
Table 2.
Cox regression of survival onto depressive symptoms and marital status
| Step | Predictors | Odd ratio | CI Interval (95%) | p-value |
|---|---|---|---|---|
| 1 | Age | 1.01 | 0.98 – 1.04 | 0.539 |
| Female, gender | 1.47 | 0.80 – 2.69 | 0.217 | |
| Education, ≤high school | 0.82 | 0.46 – 1.44 | 0.485 | |
| Finance, Having enough | 0.59 | 0.28 – 1.23 | 0.161 | |
| Having not enough | 0.89 | 0.38 – 2.10 | 0.805 | |
| Ejection Fraction | 0.98 | 0.97 – 1.00 | 0.064 | |
| NYHA class III | 1.17 | 0.60 – 2.26 | 0.646 | |
| IV | 0.99 | 0.43 – 2.25 | 0.971 | |
| 2 | Depressive symptoms | 3.68 | 1.40 – 9.69 | 0.008 |
| Non-married | 3.86 | 1.76 – 8.48 | 0.001 | |
| Depressive symptoms x Marital status | 0.37 | 0.12 – 1.15 | 0.086 |
Note: This is the final step of the Cox regression (full model Chi-square = 16.8, p = 0.006); CI = Confidence Interval; NYHA = New York Heart Association
Even when we controlled depressive symptoms and other covariates, marital status remained an independent predictor of event-free survival (OR = 2.48; 95% CI = 1.38 − 4.43)(Table 3).
Table 3.
Cox regression of survival onto marital status while controlling for depressive symptoms
| Step | Predictors | Odd ratio | CI Interval (95%) | p-value |
|---|---|---|---|---|
| 1 | Age | 1.01 | 0.98 – 1.04 | 0.475 |
| Female, gender | 1.40 | 0.77 – 2.55 | 0.277 | |
| Education, ≤high school | 0.90 | 0.51 – 1.58 | 0.896 | |
| Finance, Having enough | 0.60 | 0.28 – 1.28 | 0.185 | |
| Having not enough | 1.05 | 0.47 – 2.46 | 0.914 | |
| Ejection Fraction | 0.99 | 0.97 – 1.00 | 0.100 | |
| NYHA class III | 1.13 | 0.58 – 2.18 | 0.722 | |
| IV | 1.03 | 0.45 – 2.36 | 0.949 | |
| 2 | Depressive symptoms | 1.96 | 1.01 – 3.81 | 0.047 |
| 3. | Non-married | 2.48 | 1.38 – 4.43 | 0.002 |
Note: This is the final step of the Cox regression (full model Chi-square = 9.6, p = .002); CI = Confidence Interval; NYHA = New York Heart Association
Discussion
In this study, we found that depressive symptoms were an independent predictor of cardiac readmission or death. This finding is consistent with previous reports that depressive symptoms predict mortality and morbidity in patients with HF.3, 4 We also found that marital status, which reflects an aspect of social support was an independent predictor of patient's morbidity and mortality. This finding was comparable to previous research demonstrating that measures of social support predict prognosis in HF.6–8
The finding of increased risk for poor outcomes associated with depressive symptoms or low social support in CHD is not novel. However, studies examining the effect of depressive symptoms and social support simultaneously are rare in patients with CHD or HF.7, 8, 11 Two recent studies suggested that perceived social support may attenuate cardiac mortality related to depressive symptoms after AMI.7, 8 Frasure-Smith and colleagues followed 887 patients after AMI for one year and found that depressive symptoms increased the risk of cardiac mortality in patients with low levels of perceived social support, but not in patients with high levels of perceived social support.7 Moreover, they reported that perceived social support or other measures of social support alone failed to predict risk of cardiac mortality. Lett et al.8 followed 2481 AMI patients up to 4.5 years in the Enhancing Recovery in Coronary Heart Disease (ENRICHD) study and found that higher levels of perceived social support were associated with improved survival rates for patients without elevated depressive symptoms but not for patients with a high level of depressive symptoms. Neither perceived tangible support nor network support was associated with cardiac mortality in the ENRICHD trial. These two studies suggest that although perceived social support failed to predict cardiac mortality independently, perceived social support might play a buffering role in preventing cardiac mortality in AMI patients. On the other hand, social isolation was found to be an independent predictor of mortality in patients with HF. Friedmann et al.11 documented that both social isolation and depressive symptoms were independent predictors of mortality in patients with HF but did not examine the interaction between depressive symptoms and social isolation. In the current study, the most important finding was that marital status was an independent predictor of patients' mortality and morbidity outcome irrespective of whether patients had depressive symptoms. The interaction between depressive symptoms and marital status was not a significant in prediction of event-free survival in this study. Furthermore, we found that marital status was as predictive of event-free survival as were depressive symptoms when confounding variables were controlled. The results in this study indicated that marital status has a main or direct effect on outcomes, rather than a buffering effect on outcomes in patients with HF.
Inconsistent or discrepant evidence that social support influences outcomes in the context of depressive symptoms in previous CHD studies may be due to of use different measures of social support. Social support has been conceptualized as social networks, social relationships, and resources from different types of support. Measures of social support range from objective (e.g., counting numbers of support people) to subjective indicators (e.g., self-report on perception or experience of likelihood of receiving help from others). Social support has also been defined as a structural construct meaning living alone or not, or marital status. In this study, we attempted to capture social support in its structural aspects by defining it as having a spouse or partner who generally is the primary support system. Although we do not know the types of support (i.e. emotional support, instrumental or functional support) or quality of support provided by spouses in this study, the data suggest spouses played a pivotal role in contributing to a reduction in rehospitalization and mortality risk. Further investigations are needed to examine the effects of various types of support or social support intervention on patient's outcomes.
Although having a spouse or partner was a predictor of better outcomes in this study, the present study is limited in that the quality of the marital relationship was not investigated. Marital quality is a potential factor that may affect the buffering ability of social support. Merburg et al. found that a poor intimate network support (i.e., spousal support) was directly associated with patients' increased depressive symptoms.28 Coyne et al. also reported that HF patients with high marital quality survived longer than patients with low marital quality.29 Further examination of these relationships is needed.
The findings from this study have several implications. First, healthcare providers should assess marital status and the primary support source in the family to screen for patients at higher risk for poor outcomes. In the United States, currently more than 5 million patients have HF and most of them could benefit from the support of a spouse, family member, or significant other as they cope with living with a chronic syndrome and engage in self-management. According to a nationally representative cohort study of adults aged 65 or older,30 42% of older adults with HF received informal home care and 13% received formal care. The need for informal and formal care in adults with HF was 3 times higher than the need for those who had CHD without HF.30 However, patients with HF were less likely to have a spousal caregivers than older adults with or without CHD (47.5% vs. 56.4% vs. 55.2% respectively).30 Thus, more than half of patients with HF are likely to have an inadequate support system for self-management of HF.
Second, interventions need to be developed that address the specific needs of non-married patients particularly those with depressive symptoms. Interventions to improve depressive symptoms in CHD including pharmacotherapy and non-pharmacological interventions (i.e., cognitive behavioral therapy) have evidence of improvement of depressive symptoms.31 The ENRICHD trial is the only study designed to decrease depressive symptoms and improve social support using cognitive behavioral therapy.32 The intervention in ENRICH trial was effective in improving depressive symptoms and social isolation but it failed to reduce mortality and recurrent infarction in patients with a previous AMI. Recently, intervention programs such as peer mentor support have been developed to improve or enhance social support in patients with HF.33, 34 No intervention has been developed to improve both social support and depressive symptoms in patients with HF. Identifying and reinforcing current social support networks is helpful to improve adherence behaviors of patients who are not married. Electronic support, such as telephone and computer-based social support interventions are an alternative support resource, although using these resources successfully may depend on affordability and patients' competence in using technology.
In conclusion, this was the first study to examine the effect of marital status in the context of depressive symptoms on cardiac hospitalization and mortality of patients with HF. We demonstrated that lack of a spouse was a strong predictor of poor outcomes in patients with HF. Lack of a spouse was as strong a predictor as presence of depressive symptoms. This finding contributes to understanding of the pivotal role of spouses in improving outcomes in patients with HF particularly in the presence of depressive symptoms.
Summary of key points.
Impact of having a spouse on event-free survival in the context of depressive symptoms is unknown: page 4
Married patients experienced longer event-free survival than non-married patients even with stratification by presence or absence of depressive symptoms: page 9
Non-married patients were 2.48 times more likely to have death or hospitalization events than married patients controlling for depressive symptoms and other covariates: page 11
Acknowledgments
Grant/Financial support:
■ NIH/NINR 1K23NR010011-01 (Chung, M. L., PI)
■ NIH/NINR 3R01 NR 009280 (Lennie, T.A., PI)
■ NIH/NINR 5R01 NR 008567 (Moser, D.K., PI)
■ NIH/NINR 1P20NR010679 (Moser, DK, PI and Center Director)
■ AACN Phillips Medical Research Award (Moser, D.K., PI; Riegel, B., co-PI; Chung, M.L., co-PI)
■ University of Kentucky General Clinical Research Center (M01RR02602)
■ The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Nursing Research or the National Institutes of Health.
Because this study was funded from the NIH/NINR, I also would like to inform the American Journal of Critical Care about a new NIH Public access policy as below. “Journal acknowledges that Author retains the right to provide a copy of the final manuscript to the NIH upon acceptance for Journal publication, for public archiving in PubMed Central as soon as possible but no later than 12 months after publication by Journal.”
References
- 1.Thom T, Haase N, Rosamond W, et al. Heart disease and stroke statistics--2006 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2006;113(6):e85–151. doi: 10.1161/CIRCULATIONAHA.105.171600. [DOI] [PubMed] [Google Scholar]
- 2.Levy D, Kenchaiah S, Larson MG, et al. Long-term trends in the incidence of and survival with heart failure. N Engl J Med. 2002;347(18):1397–1402. doi: 10.1056/NEJMoa020265. [DOI] [PubMed] [Google Scholar]
- 3.Jiang W, Alexander J, Christopher E, et al. Relationship of depression to increased risk of mortality and rehospitalization in patients with congestive heart failure. Arch Intern Med. 2001;161(15):1849–1856. doi: 10.1001/archinte.161.15.1849. [DOI] [PubMed] [Google Scholar]
- 4.Jiang W, Kuchibhatla M, Clary GL, et al. Relationship between depressive symptoms and long-term mortality in patients with heart failure. Am Heart J. 2007;154(1):102–108. doi: 10.1016/j.ahj.2007.03.043. [DOI] [PubMed] [Google Scholar]
- 5.Rutledge T, Reis VA, Linke SE, et al. Depression in heart failure a meta-nalytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol. 2006;48(8):1527–1537. doi: 10.1016/j.jacc.2006.06.055. [DOI] [PubMed] [Google Scholar]
- 6.Burg MM, Barefoot J, Berkman L, et al. Low perceived social support and post-myocardial infarction prognosis in the enhancing recovery in coronary heart disease clinical trial: the effects of treatment. Psychosom Med. 2005;67(6):879–888. doi: 10.1097/01.psy.0000188480.61949.8c. [DOI] [PubMed] [Google Scholar]
- 7.Frasure-Smith N, Lesperance F, Gravel G, et al. Social support, depression, and mortality during the first year after myocardial infarction. Circulation. 2000;101(16):1919–1924. doi: 10.1161/01.cir.101.16.1919. [DOI] [PubMed] [Google Scholar]
- 8.Lett HS, Blumenthal JA, Babyak MA, et al. Social support and prognosis in patients at increased psychosocial risk recovering from myocardial infarction. Health Psychol. 2007;26(4):418–427. doi: 10.1037/0278-6133.26.4.418. [DOI] [PubMed] [Google Scholar]
- 9.Bennett SJ, Baker SL, Huster GA. Quality of life in women with heart failure. Health Care Women Int. 1998;19(3):217–229. doi: 10.1080/073993398246386. [DOI] [PubMed] [Google Scholar]
- 10.Bennett SJ, Perkins SM, Lane KA, et al. Social support and health-related quality of life in chronic heart failure patients. Qual Life Res. 2001;10(8):671–682. doi: 10.1023/a:1013815825500. [DOI] [PubMed] [Google Scholar]
- 11.Friedmann E, Thomas SA, Liu F, et al. Relationship of depression, anxiety, and social isolation to chronic heart failure outpatient mortality. Am Heart J. 2006;152(5):940, e941–948. doi: 10.1016/j.ahj.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 12.Krumholz HM, Butler J, Miller J, et al. Prognostic importance of emotional support for elderly patients hospitalized with heart failure. Circulation. 1998;97(10):958–964. doi: 10.1161/01.cir.97.10.958. [DOI] [PubMed] [Google Scholar]
- 13.Vinson JM, Rich MW, Sperry JC, et al. Early readmission of elderly patients with congestive heart failure. J Am Geriatr Soc. 1990;38(12):1290–1295. doi: 10.1111/j.1532-5415.1990.tb03450.x. [DOI] [PubMed] [Google Scholar]
- 14.Murberg TA, Bru E. Social relationships and mortality in patients with congestive heart failure. J Psychosom Res. 2001;51(3):521–527. doi: 10.1016/s0022-3999(01)00226-4. [DOI] [PubMed] [Google Scholar]
- 15.Schwarz KA, Elman CS. Identification of factors predictive of hospital readmissions for patients with heart failure. Heart Lung. 2003;32(2):88–99. doi: 10.1067/mhl.2003.15. [DOI] [PubMed] [Google Scholar]
- 16.Chin MH, Goldman L. Correlates of early hospital readmission or death in patients with congestive heart failure. Am J Cardiol. 1997;79(12):1640–1644. doi: 10.1016/s0002-9149(97)00214-2. [DOI] [PubMed] [Google Scholar]
- 17.Cohen S, MaKay G. Social support, stress and buffering hypothesis: A theoretical analysis. In: Baum A, Singer JE, Tayllor SE, editors. Handbood of psychology and health. Vol 4. Erlbaum; Hillsdale, NJ: 1984. pp. 253–267. [Google Scholar]
- 18.Lazarus RS, Folkman S. Stree, appraisal, and coping. Springer; New York: 1984. [Google Scholar]
- 19.Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98(2):310–357. [PubMed] [Google Scholar]
- 20.Pressler SJ, Subramanian U, Shaw RM, et al. Research in patients with heart failure: challenges in recruitment. Am J Crit Care. 2008;17(3):198–203. [PubMed] [Google Scholar]
- 21.Arnau RC, Meagher MW, Norris MP, et al. Psychometric evaluation of the Beck Depression Inventory-II with primary care medical patients. Health Psychol. 2001;20(2):112–119. doi: 10.1037//0278-6133.20.2.112. [DOI] [PubMed] [Google Scholar]
- 22.Beck AT, Brown G, Steer RA. Beck Depression Inventory II Manual. The Psychological Corporation; San Antonio, TX: 1996. [Google Scholar]
- 23.Steer RA, Ball R, Ranieri WF, et al. Dimensions of the Beck Depression Inventory-II in clinically depressed outpatients. J Clin Psychol. 1999;55(1):117–128. doi: 10.1002/(sici)1097-4679(199901)55:1<117::aid-jclp12>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 24.Steer RA, Clark DA, Beck AT, et al. Common and specific dimensions of self-reported anxiety and depression: the BDI-II versus the BDI-IA. Behav Res Ther. 1999;37(2):183–190. doi: 10.1016/s0005-7967(98)00087-4. [DOI] [PubMed] [Google Scholar]
- 25.Cowan MJ, Freedland KE, Burg MM, et al. Predictors of treatment response for depression and inadequate social support--the ENRICHD randomized clinical trial. Psychother Psychosom. 2008;77(1):27–37. doi: 10.1159/000110057. [DOI] [PubMed] [Google Scholar]
- 26.Frasure-Smith N, Lesperance F, Juneau M, et al. Gender, depression, and one-year prognosis after myocardial infarction. Psychosom Med. 1999;61(1):26–37. doi: 10.1097/00006842-199901000-00006. [DOI] [PubMed] [Google Scholar]
- 27.nQuery Advisor [computer program] Version Version 6.0. Statistical Solutions; Sangus, MA: 1995–2005. [Google Scholar]
- 28.Murberg TA, Bru E, Aarsland T, et al. Social support, social disability and their role as predictors of depression among patients with congestive heart failure. Scand J Soc Med. 1998;26(2):87–95. doi: 10.1177/14034948980260020701. [DOI] [PubMed] [Google Scholar]
- 29.Coyne JC, Rohrbaugh MJ, Shoham V, et al. Prognostic importance of marital quality for survival of congestive heart failure. Am J Cardiol. 2001;88(5):526–529. doi: 10.1016/s0002-9149(01)01731-3. [DOI] [PubMed] [Google Scholar]
- 30.Gure TR, Kabeto MU, Blaum CS, et al. Degree of disability and patterns of caregiving among older Americans with congestive heart failure. J Gen Intern Med. 2008;23(1):70–76. doi: 10.1007/s11606-007-0456-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Artinian NT, Artinian CG, Saunders MM. Identifying and treating depression in patients with heart failure. J Cardiovasc Nurs. 2004;19(6 Suppl):S47–56. doi: 10.1097/00005082-200411001-00007. [DOI] [PubMed] [Google Scholar]
- 32.Berkman LF, Blumenthal J, Burg M, et al. Effects of treating depression and low perceived social support on clinical events after myocardial infarction: the Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) Randomized Trial. Jama. 2003;289(23):3106–3116. doi: 10.1001/jama.289.23.3106. [DOI] [PubMed] [Google Scholar]
- 33.Daugherty J, Saarmann L, Riegel B, et al. Can we talk? Developing a social support nursing intervention for couples. Clin Nurse Spec. 2002;16(4):211–218. doi: 10.1097/00002800-200207000-00011. [DOI] [PubMed] [Google Scholar]
- 34.Riegel B, Carlson B. Is individual peer support a promising intervention for persons with heart failure? J Cardiovasc Nurs. 2004;19(3):174–183. doi: 10.1097/00005082-200405000-00006. [DOI] [PubMed] [Google Scholar]