Abstract
Purpose
This study evaluated the safety, toxicity, pharmacological properties and biological activity of PI-88, a heparanase endoglycosidase enzyme inhibitor, with fixed weekly docetaxel in patients with advanced solid malignancies.
Experimental design
This was a phase I study to determine the maximal-tolerated dose of escalating doses of PI-88 administered subcutaneously for 4 days per week, along with docetaxel 30 mg/m2 given on days 1, 8, 15 of a 28-day schedule.
Results
Sixteen patients received a total of 42 courses of therapy. No dose-limiting toxicities were observed despite escalation to the highest planned dose level of PI-88 (250 mg/day). Frequent minor toxicities included fatigue (38%), dysgeusia (28.5%), thrombocytopenia (12%), diarrhea (14%), nausea (12%), and emesis (10%) in the 42 courses. No significant bleeding complications were observed. One patient developed a positive anti-heparin antibody test/serotonin releasing assay with positive anti-platelet factor 4/PI-88 antibodies and grade 1 thrombocytopenia in cycle 5, and was withdrawn from the study without any sequelae. PI-88 plasma concentrations (mirrored by APTT) and urinary elimination were linear and dose-proportional. Docetaxel did not alter the pharmacokinetic (PK) profile of PI-88, nor did PI-88 affect docetaxel PK. No significant relationship was determined between plasma or urine FGF-2, or plasma VEGF levels and PI-88 dose/response. Although no objective responses were observed; 9 of the 15 evaluable patients had stable disease for greater than two cycles of therapy.
Conclusion
PI-88 administered at 250 mg/day for 4 days each week for 3 weeks with docetaxel 30 mg/m2 on days 1, 8 and 15, every 28 days, was determined to be the recommended dose level for phase II evaluation. This combination was well tolerated without severe toxicities or PK interactions.
Keywords: PI-88, Docetaxel, Heparanase inhibitor, Angiogenesis, Clinical trial, Advanced malignancies
Introduction
Anti-angiogenic approaches, either alone or in combination with chemotherapy, are active in treating advanced malignancies [39, 41, 52]. Targeting vascular endothelial growth factor (VEGF) and its receptors, platelet derived growth factor (PDGF) and basic fibroblast growth factor (FGF-2) via antibody and receptor tyrosine kinase techniques have proven efficacy; however, many other angiogenic targets have yet to be fully explored [39, 41, 52]. Heparanase is a endoglycosidase enzyme which degrades heparan sulfate glycosaminoglycan, the principal component of the basement membrane, resulting in the loss of basement membrane integrity, and release of heparan sulfate bound angiogenic and growth-promoting factors [54], which subsequently stimulate tumor blood vessel growth, cellular invasion, migration, adhesion, metastasis, differentiation and proliferation [15, 29, 53]. Furthermore, heparanase induces endothelial cell migration via activation of the protein kinase B/Akt signal pathway, independent of its endoglycosidase activity [51]. Heparanase mRNA is over-expressed in a wide variety of tumor types [30, 31, 45], with notably high over-expression in head and neck [46], pancreatic [25], and hepatocellular carcinomas [16].
PI-88 is a highly reproducible sulfonated oligosaccharide mixture derived from chemical sulfation of the oligosaccharide phosphate fraction of phosphomannan produced by yeast Pichia (Hansenula) holstii NRRLY-2448 (ATCC 13689). PI-88 inhibits heparanase and cleavage of heparan sulfate (HS), and competes with HS binding of peptide FGF, and VEGF to produce the potent anti-angiogenic and anti-metastatic effects observed preclinically [2, 34–36]. The activated partial thromboplastin time (APTT) is prolonged by PI-88 due to activation of endogenous heparin cofactor II, without affecting prothrombin time, anti-thrombin III-mediated inhibition of factor Xa or factor IIa (thrombin) [34].
PI-88 has been studied as a continuous intravenous (IV) infusion or subcutaneously (SC) in healthy male volunteers and patients [5, 36, 42]. Phase I intravenous studies in advanced cancer patients did not demonstrate tolerability. Dose-limiting toxicities (DLTs) of immune-related thrombocytopenia with formation of anti-heparin platelet factor 4 (AHPF4) complex antibodies (at 2.28 mg/kg/day for 14 days) were observed in 2 out of 14 patients in one study, [1, 36, 42], and a DLT of serum transaminitis (at 4.56 mg/kg/day for 4 days) was observed in another study. Moreover, there was minimal APTT prolongation, biologic or clinical activity at these doses [1, 36, 42]. Consequently, IV studies were terminated early, and the SC formulation was further developed for its improved bioavailability and decreased incidence of immune-mediated thrombocytopenia [36, 42]. In a phase I study of 42 patients receiving PI-88 alone (80–315 mg/day), the MTD of 250 mg/day SC daily for 4 days on both bimonthly and weekly schedules was established with linear pharmacokinetics (PK) and minimal toxicity. Grades 2–3 thrombocytopenia were observed in three patients with only one patient developing positive AHPF4 antibodies. Furthermore, this SC formulation demonstrated biologic and clinical activity. Patients demonstrated APTT prolongation correlating with AUC and Cmax as a pharmacodynamic (PD) marker, and preliminary anti-tumor activity was observed: one metastatic melanoma patient treated at 80 mg/day had a partial response (PR) maintained for >70 months and 9 patients treated at PI-88 doses between 140 and 250 mg/day maintained stable disease (SD) >6 months [5].
Docetaxel, a semi-synthetic taxane, has established broad-spectrum anti-tumor activity in breast, lung, gastric, prostate and ovarian cancers at doses of 60–100 mg/m2 IV administered every 3 weeks [7, 21, 22]. The high incidence of acute severe neutropenia, alopecia, asthenia, dermatological reactions, fluid retention, hypersensitivity reactions and stomatitis are reduced when dosing is changed to fixed low doses of 30–40 mg/m2 given weekly [3, 8]. Frequent low docetaxel doses maintain similar efficacy with mild myelosuppression, and predominant toxicities of minor nail changes, excessive lacrimation, and dose-limiting fatigue and asthenia [19, 26, 28, 47].
Anti-angiogenic drugs increase the anti-tumor efficacy, response rates and progression-free survival of patients when combined with chemotherapy, without a high incidence of hemorrhage [4, 18, 33, 55]. PI-88 shows additive activity in combination with cytotoxic agents in-vivo [36], and improved clinical efficacy is seen when docetaxel is combined with anti-angiogenic agents [6, 12, 27, 37, 38]. Therefore, PI-88 and with low dose weekly docetaxel could potentially be a well-tolerated and efficacious combination, with broad anti-tumor activity.
The goals of this phase I study were to determine the maximum-tolerated dose (MTD) or the recommended phase II dose (RPTD), safety, tolerability and PK profile of PI-88 when administered SC in combination with weekly IV docetaxel in patients with advanced malignancies. The biological activity of this combination was determined by analysis of relevant biomarkers of angiogenesis, and early anti-tumor activity was assessed.
Patients and methods
Patient selection
Eligibility criteria were as follows: patients to have histological or cytopathological confirmed advanced malignancies refractory to or without standard therapy, age ≥18 years, Eastern Cooperative Oncology Group (ECOG) performance status <2, life expectancy >3 months, and adequate laboratory parameters such as neutrophil counts >1.5 × 109/L, platelet counts >100 × 109/L, prothrombin time <1.5 times the upper limit of normal (×ULN), normal APTT, calculated creatinine clearance >60 ml/min (Cock-croft-Gault formula) [9, 40], bilirubin < ULN and liver enzyme levels <2.5 × ULN.
Patients were excluded if they had myocardial infarction, stroke or congestive heart failure within the past 3 months, investigational or hormonal therapy, major surgery or uncontrolled infection within the past 4 weeks, or palliative radiotherapy within 7 days of study initiation. Criteria also excluded: radiotherapy to >30% of the bone marrow, symptomatic central nervous system involvement, meningeal metastases, any history of bleeding, abnormal bleeding tendency, heparin-induced thrombocytopenia, immune-mediated thrombocytopenia, thrombotic thrombocytopenic purpura, platelet disease, or allergy and/or hypersensitivity to anti-coagulants, thrombolytic agents, heparin or polysorbate 80. Concomitant aspirin, non-steroidal anti-inflammatory drugs (except selective COX-2 inhibitors), heparin, low molecular weight heparin or coumadin (>1 mg) were not allowed, nor was heparin/low molecular weight heparin use <2 weeks prior to study initiation. Patients could not be on any cytochrome CYP3A enzyme inducers or inhibitors during/within 1 week of study treatment. Pregnant or breast-feeding women were excluded and female patients of childbearing age were required to have a negative pregnancy test. Written informed consent was obtained from all patients in compliance with federal and institutional guidelines.
Drug administration
PI-88 supplied by Progen Pharmaceuticals Limited (Toowong, QLD, Australia) as a sterile lyophilized powder (400 mg/vial) was reconstituted in 0.9% sodium chloride to form a sterile solution (320 mg/mL) administered SC for four consecutive days per week, (immediately before docetaxel infusion on day 1), for three out of 4 weeks. Commercially available docetaxel was obtained from Aventis Pharmaceutical Products Inc. (TAXOTERE® 20 and 80 mg), prepared as per manufacturer’s instructions and administered once weekly for 3 weeks of every 4-week cycle. Dexamethasone 8 mg IV was given prior to docetaxel to prevent hypersensitivity reactions, skin toxicity and peripheral edema [47].
PI-88 dosing was initiated at 106 mg/day (based on findings from a prior study of PI-88 alone) [5] and escalated by 33% between cohorts (106, 140, 190 and 250 mg/day), while maintaining a fixed docetaxel dose, until the MTD was determined or the maximum dose level of 250 mg/day of PI-88 was reached, as shown in Table 1. Although preclinically PI-88 did not affect docetaxel metabolism or excretion (PI-88 did not affect P450 enzymes in human hepatic microsome studies and was excreted unchanged in the urine without hepatic metabolism in animal studies) [36], fixed doses of 30 mg/m2 of docetaxel, lower than clinically established 35–40 mg/m2 monotherapy doses, were chosen for safety as PI-88 had not been examined in combination at the time of study design [47]. A standard 3 + 3 phase I design was implemented, and three assessable patients were enrolled to each dose level [24]. If one-third patients developed DLT, three additional patients were enrolled to the same dose level. If ≥2 patients at a dose level developed DLT, enrollment would stop, and the immediately preceding dose level would be defined the MTD. If the MTD were not determined in lower dose levels, PI-88 would be escalated to a maximum dose of 250 mg/day with enrollment of six total patients. DLT was defined as any grade ≥3 non-hematological toxicity (excluding alopecia, and nausea/vomiting in the absence of adequate anti-emetic therapy), grade 4 thrombocytopenia, grade 4 granulocytopenia >5 days, or febrile neutropenia (fever ≥ 38.3°C). DLT included the inability to administer >75% of planned PI-88 doses in a cycle due to toxicity, inability to begin the next course of treatment <2 weeks of last PI-88 dose due to unresolved toxicity, APTT >3 ×ULN for >2 h post PI-88 dosing days 1, 8 and 15, or Grade 3 injection site reaction.
Table 1.
PI-88 dose-escalation scheme
| Cohort | PI-88 (mg) administered subcutaneously for 4 days weekly |
Docetaxel (mg/m2) administered intravenously weekly for three out of four weeks |
Number of patients |
Number of cycles of therapy |
|---|---|---|---|---|
| 1 | 106 | 30 | 3 | 6 |
| 2 | 140 | 30 | 3 | 5 |
| 3 | 190 | 30 | 3 | 8a |
| 4 | 250 | 30 | 7c | 23b |
| Total | 16 | 42 |
One patient in this cohort received PI-88 alone for cycle 2 day 15. Docetaxel was withheld due to grade 1 hyperbilirubinemia possibly related to treatment
One patient in this cohort continued with stable disease after the end of cycle 6 and was transferred to the continuation protocol alone for two further cycles (included in the total number of cycles above)
One patient developed rapid progression of disease with new brain metastases after cycle 1 day 5; therefore, this patient was not included for assessment of response and was replaced and not included in the assessment of number of cycles in this table; however, this patient was included for assessment of toxicity
Pretreatment and follow-up studies
Medical histories, symptom reviews, physical examinations, medication profiles, performance status assessments, routine laboratory studies and coagulation profiles (PT, APTT, fibrinogen, and D-Dimer) were performed before study initiation and weekly during treatment. Pretreatment studies included urinalysis, a serum pregnancy test (as appropriate), an electrocardiogram, radiographic studies to evaluate measurable and assessable sites of disease, and relevant tumor markers. During cycle 1, APTT levels were monitored on day 1, then assessed pre- and 2 h post PI-88 dose on days 2, 3, 4, 8, 9, 10, 11, 15 and 28. PI-88 injection sites were monitored. Radiographic evaluations for disease status were repeated after every other course using Response Evaluation Criteria in Solid Tumors (RECIST) [49, 50], and patients continued treatment until progression or withdrawal criteria were met.
Measurement of antibodies to PF4, PI-88 or heparin
Antibodies to PI-88 or platelet factor 4 (PF4) were measured in patients prior to initial study treatment and at the end of each cycle. Anti-PI-88/PF4 antibody production was measured with an enzyme-linked immunoassay (EIA) described by Amiral et al. [1], in addition to a functional serotonin release assay (SRA) for heparin-induced thrombocytopenia previously described by Sheridan et al. [44]
Pharmacokinetic assessments
PI-88, docetaxel and APTT blood samples were collected prior to PI-88 dosing, at 0.5, 1, 1.5, 2, 3, 4, 6 and 8 h after PI-88 dosing on day 1, immediately before PI-88 on days 2, 3, 4, 8, 9, 10, 11, 15 and 28, and on day 5 (24 h post PI-88). PI-88 plasma levels were determined using a developed and validated fluorescence-quenching assay, as outlined by Basche et al. [5].
PK analysis of weekly docetaxel in human plasma, in the presence of PI-88 administration, was done by a tandem LCMS method developed and previously established by Gustafson et al. [20]. Docetaxel concentrations in plasma were calculated based on a standard curve of docetaxel in blanked pooled human plasma with internal standard docetaxel.
The PK profile of PI-88 was analyzed using compartmental methods with data fit to the compartmental module. Docetaxel PK parameters were calculated from concentration versus time data using a three-compartment model with intravenous infusion and by non-compartmental analysis. The compartmental and non-compartmental modeling and determination of PK parameters for both PI-88 and docetaxel were determined using WinNonlin software version 4.1 (Pharsight Corporation, Mountain View, CA, USA) with 1/γ2 weighting and calculation of PK parameters using Microsoft Excel and standard equations for compartmental, non-compartmental and system analysis. PK variables were calculated in a model-dependent manner.
Sterile midstream urine samples for PK determination were collected at the same intervals as the blood samples above and PI-88 levels were determined by a high performance liquid chromatography (HPLC) method validated for PI-88 by Progen Pharmaceuticals Ltd. PI-88 extraction was performed using a Waters Oasis QAX® SPE column (Milford, MA, USA) with 0.1 ammonium acetate, water and methanol, then eluted with 1% ammonia. The eluant (100 µL/replicate) was analyzed by size exclusion HPLC (Shodex OHpak 6 µ) with refractive index detection at 35°C, using a mobile phase of 0.1 ammonium acetate. PI-88 concentration was determined by comparison to a standard curve (10–150 µg/mL PI-88) prepared by adding known concentrations of PI-88 to urine from healthy volunteers and processing them the same way as patient samples. The assay had a linear range of 10–300 µg/mL PI-88.
Measurement of systemic and urinary angiogenic growth factor levels
Whole blood and urine samples were collected on prior to PI-88 administration on days 1 and 15, on day 28 and at study end. Analysis of VEGF and FGF-2 plasma levels, and of urinary FGF-2 were performed using a validated ELISA based antibody immunoassay, Quantikine® (R&D Systems, Minneapolis, MN, USA). Quality control samples containing known amounts of the substrate were run in parallel with other samples to determine the inter-day coefficient of variation. Only assays exhibiting coefficient of variation <20% were considered valid.
Results
General
Sixteen patients (median age 54 years, 69% females) received a total of 42 courses of therapy. Most patients (62.5%) were ECOG ≤1 and a wide variety of tumor types were represented with a predominance of melanoma, breast and ovarian cancers. All patients had prior systemic therapy and/or radiotherapy, with the exception of one melanoma patient. These descriptive characteristics are summarized in Table 2.
Table 2.
Patient demographics and characteristics
| Characteristic | Number |
|---|---|
| Number of patients | 16 |
| Total number of courses | 42 |
| Number of courses per patient | |
| Median | 3 |
| Range | 1–8 |
| Patients receiving ≥2 cycles of therapy | 9 |
| Sex | |
| Male | 5 |
| Female | 11 |
| Age | |
| Median (in years) | 54 |
| Range (in years) | 41–67 |
| ECOG performance status | |
| 0 | 4 |
| 1 | 11 |
| 2 | 1 |
| Previous treatment | |
| Mean prior chemotherapy regimens | 2 |
| Range of prior chemotherapy regimens | 0–6 |
| Fewer than three prior chemotherapy regimens | 8 |
| Three or greater prior chemotherapy regimens | 3 |
| Prior investigational/ targeted therapy/clinical triala | 6 |
| Prior immunotherapy | 3 |
| No prior chemotherapy or radiation therapy | 1 |
| Prior radiotherapy | 9 |
| Tumor type | |
| Melanoma | 5 |
| Ovarian | 3 |
| Breast cancer | 3 |
| Otherb | 6 |
Abbreviation: ECOG Eastern Cooperative Oncology Group
Includes interferon, IL-2 and vaccines, autologous stem cell transplantation, isolated hepatic perfusion and clinical trials with novel agents
Other tumor types include one of each including of cystic adenocarcinoma of the tongue, colon cancer, thymoma, gastric cancer, fallopian tube adenocarcinoma, and squamous cell carcinoma of the head and neck
Toxicity
PI-88 and docetaxel therapy was well tolerated in the 16 patients; 98% of all toxicities were mild to moderate in severity. Of all the adverse events (AEs) experienced, 56% were attributable to study drug, and out of these, 78% were mild. As observed in Table 3, the most frequently observed non-hematological AEs attributable to study drugs were fatigue (12 events in 10 patients, with an incidence of 33% in the 42 courses of therapy), followed by dysgeusia (28.5%), diarrhea (14%), nausea (12%), emesis (10%) and dyspepsia (10%). No patients required PI-88 dose modification. Docetaxel doses were not reduced due to toxicity. Docetaxel administration was held for one dose in a patient in cohort 3 (cycle 2 day 15) due to transient grade 1 hyperbilirubinemia, he received PI-88 alone (190 mg/day) and the hyperbilirubinemia resolved; nevertheless, the patient developed disease progression (PD) and was withdrawn from study after cycle 2. One patient in the 250 mg/day cohort was delayed 1 week from treatment with both agents due to grade 3 fatigue. No other delays were required and no hospitalizations occurred as a result of toxicity.
Table 3.
Non-hematological toxicities of PI-88 and docetaxel
| PI-88 (mg/day) |
Docetaxel (mg/m2) |
No courses (patients) |
Fatigue incidence (number of courses) |
Dysgeusia incidence (number of courses) |
Diarrhea incidence (number of courses) |
Nausea incidence (number of courses) |
Emesis incidence (number of courses) |
Dyspepsia incidence (number of courses) |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| G1 | G2 | G3 | G1 | G2 | G1 | G2 | G1 | G2 | G1 | G2 | G1 | G2 | |||
| 106 | 30 | 3 (6) | 1 | 1 | 0 | 1 | 0 | 2 | 0 | 2 | 0 | 0 | 0 | 1 | 0 |
| 140 | 30 | 3 (5) | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 |
| 190 | 30 | 3 (8) | 2 | 3 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 2 | 0 | 0 |
| 250 | 30 | 7 (23) | 6 | 1 | 1 | 1 | 10 | 1 | 0 | 2 | 0 | 2 | 0 | 2 | 0 |
| Total | 16 (42) | 16 (38%) | 12 (28.5%) | 6 (14%) | 5 (12%) | 4 (10%) | 4 (10%) | ||||||||
G1–G3 represent National Cancer Institute CTC grades 1–3 (version 2.0). The number of cycles in which each toxicity was observed is indicated in the body of the table
As shown in Table 4, there were minimal hematologic toxicities: thrombocytopenia was observed in five courses (12%), and grade 2 anemia at the 190 and 250 mg PI-88 doses was described in 4 of the 42 courses (10%). Only one incidence of severe grade 3 thrombocytopenia (<2%) occurred in a patient at the highest PI-88 dose (250 mg/day) during cycle 6, without any bleeding complications and the AHPF4 result was negative. After being taken off study for PD, the patient recovered fully without additional treatments. One patient in the 190-mg/day cohort, at the beginning of cycle 5 developed presence of a positive SRA result and anti PF4/PI-88 antibodies with transient grade 1 thrombocytopenia. Despite the lack of clinically significant bleeding or clotting complications, this patient was discontinued from study without any sequelae. No other patients developed anti-PI-88/PF4 antibodies.
Table 4.
Hematological Toxicities Attributed to PI-88 and Docetaxel
| PI-88 (mg/day) |
Docetaxel (mg/m2) |
No. patients (No. of courses) |
Bruising at injection site incidence |
Thrombocytopenia incidence |
Anemia incidence |
||||
|---|---|---|---|---|---|---|---|---|---|
| G1 | G2 | G1 | G2 | G3 | G1 | G2 | |||
| 106 | 30 | 3 (6) | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 140 | 30 | 3 (5) | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| 190 | 30 | 3 (8) | 3 | 0 | 4 | 0 | 0 | 0 | 2 |
| 250 | 30 | 7 (23) | 1 | 0 | 0 | 0 | 1 | 0 | 2 |
| Total | 16 (42) | 5 (12%) | 5 (12%) | 4 (10%) | |||||
G1–G3 represent National Cancer Institute CTC grades 1–3 (version 2.0). The number of cycles in which each toxicity was observed is indicated in the body of the table
Severe grade 3 toxicities were observed late in therapy and were infrequent. No DLTs were observed. As there were no DLTs to establish the MTD after escalation to highest predetermined dose level of PI-88, PI-88 at 250 mg/day SC daily for four consecutive days per week with fixed dose docetaxel at 30 mg/m2 IV on days 1, 8, 15 q 28 days was determined to be the RPTD.
Anti-tumor activity
No partial or complete responses were observed during the study period. However, at least 9 of the 15 patients evaluable for response maintained SD at completion of ≥2 cycles of therapy. The histological subtype of patients with SD ≥2 cycles included ovarian carcinoma (3), melanoma (2), adenocystic carcinoma of the head and neck (1), squamous cell carcinoma of the head and neck (1) gastric carcinoma (1), and breast carcinoma (1). Remarkably, many of these patients had been heavily pretreated with >2 prior regimens and some had failed prior taxane therapy. Most patients with prolonged SD were treated in the 190 or 250 mg/day cohorts. The patient (receiving 190 mg/day PI-88) with adenocystic carcinoma of the tongue and lung metastases maintained SD after completing four cycles, but required withdrawal from the study due to the positive AHPF4 result in cycle 5. A gastric cancer patient with extensive lymphadenopathy completed six cycles of PI-88 at 250 mg/day before developing PD. A malignant thymoma patient with involvement of pleura, pericardium, diaphragm and liver had sustained SD after six cycles of PI-88 at 250 mg/day; therefore, he was transferred to the PI-88-alone continuation protocol for two more cycles, maintaining SD for a total of eight cycles.
Pharmacokinetic studies
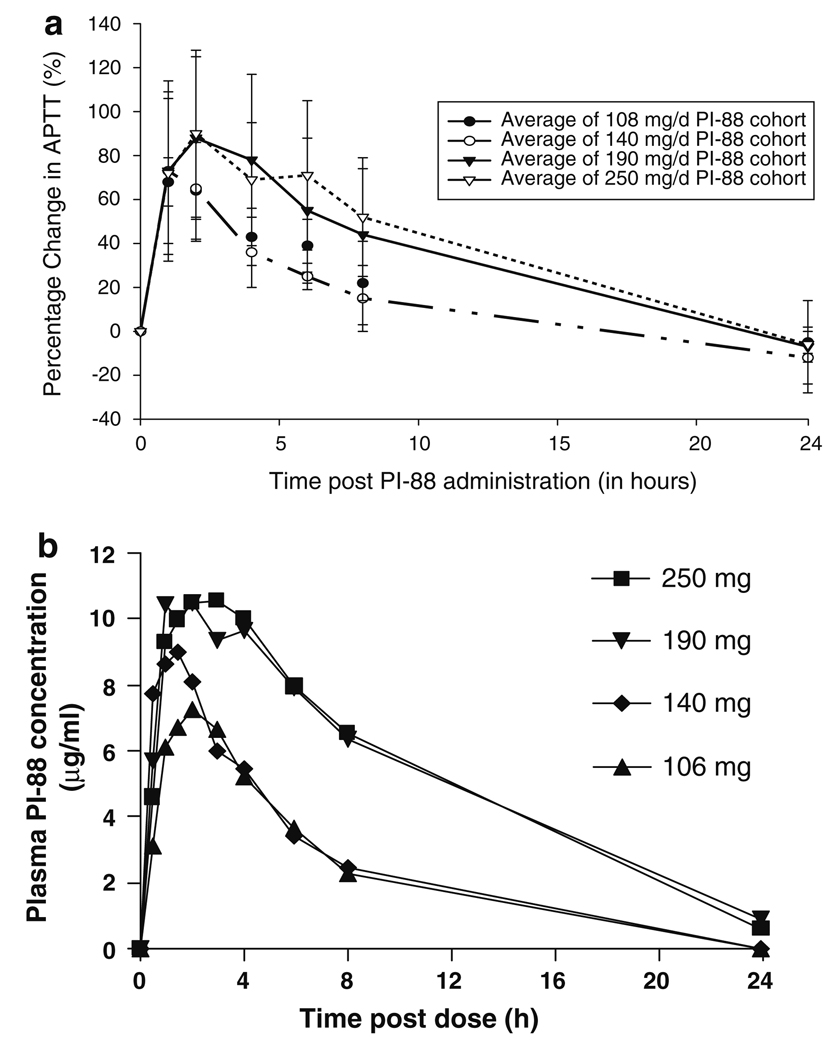
PI-88 PK profiles were assessed from 296 plasma samples from 16 patients. PI-88 plasma concentrations increased with dose (Fig. 1b) and were near linear with respect to Cmax and AUC (Table 5). The plasma PI-88 PK profile was consistent with those observed in previous studies with linear elimination evident from the time of Cmax [5, 34, 40]. The maximum pre-dose concentration reached was 1.5 µg/mL, which was consistent with the data from an earlier study of PI-88 alone [5]. There was marginal increase in the half-life (t1/2) with increasing PI-88 dose. The apparent clearance and volume of distribution did not change significantly across the doses administered with minor drug accumulation with repeat dosing.
Fig. 1.
a Percentage change in APTT (%) with respect to time post PI-88 administration (in h). b Plasma concentration of PI-88 (ug/ml) versus time post dose (h)
Table 5.
Average pharmacokinetic values for PI-88 from 106 to 250 mg subcutaneous on day 1 in the presence of Docetaxel 30 mg/m2 intravenous once weekly
| Average pharmacokinetic values for PI-88 when administered with docetaxel (30 mg/m2 IV weekly for 3 out of 4 weeks) |
PI-88 106 mg subcutaneous once daily dosing (n = 3 patients) |
PI-88 140 mg subcutaneous once daily dosing (n = 3 patients) |
PI-88 190 mg subcutaneous once daily dosing (n = 3 patients) |
PI-88 250 mg subcutaneous once daily dosing (n = 7 patients) |
|---|---|---|---|---|
| V/F (Volume of distribution/bioavailability) in mL | 8,296 ± 3,150 | 11,811 ± 1,856 | 12,855 ± 4,618 | 14,261 ± 4,338 |
| AUC (Area under the Concentration Curve) in h *ug/mL | 47 ± 10 | 55 ± 12 | 147 ± 113 | 132 ± 51 |
| T1/2 (half-life) in h | 2.5 ± 0.6 | 3.1 ± 0.3 | 7.0 ± 5.9 | 5.2 ± 2.7 |
| Tmax (time to maximal concentration) in h | 2.3 ± 0.4 | 1.1 ± 0.8 | 2.4 ± 1.2 | 3.0 ± 1.4 |
| C max (maximal concentration) in ug/mL | 6.9 ± 2.1 | 9.7 ± 3.7 | 10.7 ± 3.5 | 11.1 ± 1.3 |
| CL/F (Clearance/bioavailability) in mL/h | 2,337 ± 489 | 2,626 ± 534 | 1,783 ± 960 | 2,156 ± 828 |
PI-88 PK parameters in the presence of docetaxel demonstrated a one-compartment model with first order elimination and first-order absorption from an extravascular site with a high goodness-of-fit correlation (>0.90–0.95) in the 106 and 140 mg doses; with a lower goodness-of-fit correlation (0.88) in the 190 and 250 mg doses (Table 5) [5]. PI-88 PK parameters were not affected by the administration of docetaxel. PI-88 PK parameters in the presence of docetaxel were similar to the PK parameters of PI-88 alone in a prior study [5]. Docetaxel PK parameters demonstrated a three-compartmental model (Table 6) and were unaffected by the administration of PI-88 [20].
Table 6.
Docetaxel PK in patients treated with 30 mg/m2 in the presence of PI-88 compared with PK in patients treated with docetaxel alone
| PK parameters | Docetaxel + PI-88 (n = 11) |
Docetaxel alonea (n = 8) |
|---|---|---|
| Cmax (nM) | 931 ± 347 | 933 ± 372 |
| AUC (nM h) | 1,390 ± 396 | 1,446 ± 494 |
| t1/2α (h) | 0.11 ± 0.04 | 0.08 ± 0.03 |
| t1/2β (h) | 1.24 ± 0.53 | 0.88 ± 0.49 |
| t1/2γ (h) | 33.0 ± 18.4 | 25.4 ± 20.1 |
| CL (L/h/m2) | 29.3 ± 10.7 | 29.1 ± 11.9 |
| Vss (L/m2) | 434 ± 358 | 322 ± 330 |
PK parameters calculated using a three-compartment model
Docetaxel alone data are from Gustafson et al. [20]
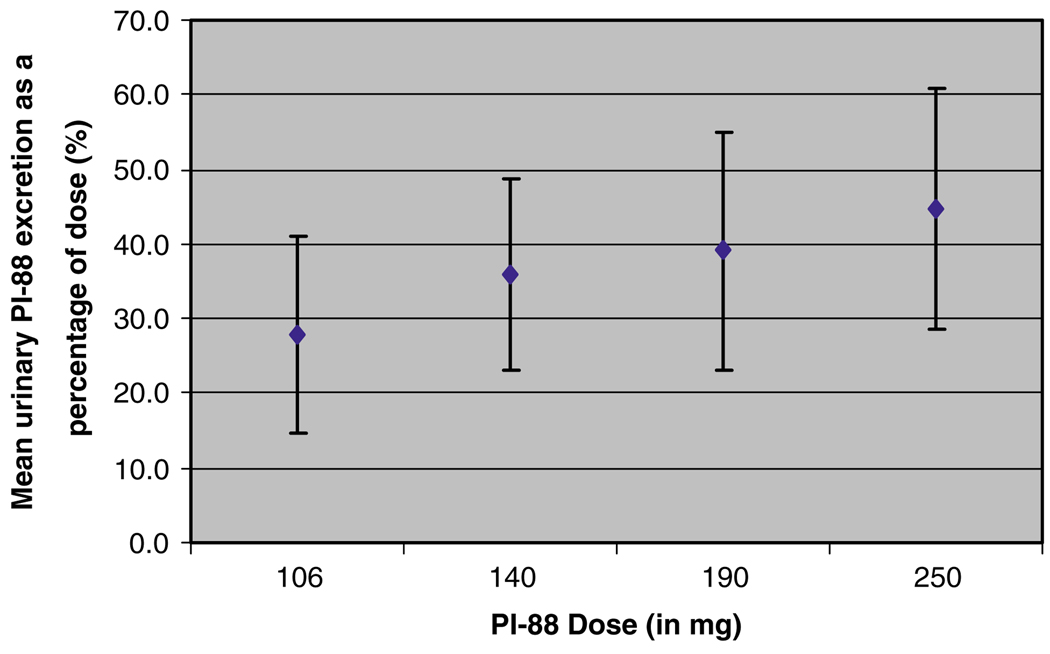
PI-88 urinary elimination as a function of dose increased linearly with increased dose (high correlation co-efficient r2 = 0.91), without obvious binding (Fig. 2).
Fig. 2.
Percentage mean urinary excretion of PI-88 with respect to PI-88 dose (mg)
Pharmacokinetic/pharmacodynamic relationships
As PI-88 has anticoagulant properties, the change in APTT served as a PI-88 PD marker: at least grade 1 APTT prolongation (>1.5 ×ULN) was evident after every dose of PI-88 as shown in Fig. 1a; however, sustained, more prominent prolongation was observed at higher doses of 190 and 250 mg/day. The change in APTT returned close to baseline after each administration, similar to PI-88, and also demonstrated a linear relationship with, respectively, Cmax and AUC. Despite low correlation, the percentage change in APTT appeared to correlate better to Cmax (goodness of fit r2 = 0.27) rather than to the AUC (goodness of fit r2 = 0.11). In the 250 mg/day cohort, 3/7 patients developed transient increases in APTT up to grade 2 (>1.5–2 ×ULN) after PI-88 dosing (at Cmax) in later cycles, without any clinical sequelae. However, one of these patients developed mild bruising at the injection site in cycles 2 and 3, and transient grade 2 hematuria concomitant with a urinary tract infection at peak APTT levels. Due to the small number of patients in this study, patient characteristics, toxicities and efficacy could not be correlated with PI-88 PK variables.
Growth factor concentrations
Levels of plasma FGF-2, VEGF and urine FGF-2 did not demonstrate any significant relationship with respect to the dose of PI-88, APTT prolongation, or cycle of therapy. These growth factor concentrations also did not appear to correlate with disease stability or progression; however, patient numbers were too low to draw conclusions.
Discussion
This study established that PI-88 could safely be given at doses up to 250 mg/day with fixed weekly docetaxel, and that this combination was well tolerated. Toxicities were mild and there were no DLTs. As PI-88 toxicity would unlikely diminish in combination with chemotherapy, doses were not escalated above 250 mg/day (the active established monotherapy MTD) [5]. Low dose weekly docetaxel was chosen due to its low incidence of severe myelosuppression (<15%), and thrombocytopenia (<5%) [7, 23, 28, 43]. The principal toxicities in this study of fatigue, dysgeusia, diarrhea, and nausea/vomiting were in keeping with the toxicity profile of docetaxel, as was transient hyperbilirubinemia in one patient [21]; whereas, injection site bruising and thrombocytopenia were observed with PI-88.
PI-88 with docetaxel was safe without significant hematologic toxicities, hemorrhage or thrombosis. Severe thrombocytopenia was observed in <2% of courses without bleeding complications. Although PI-88 inhibits thrombin-induced platelet aggregation, it does not affect collagen- or ADP-induced aggregation in vitro, and hemorrhage has not been observed in animal models [36]. As PI-88 induces the release of tissue factor pathway inhibitor without effect on anti-thrombin III-mediated inhibition of factor Xa or factor IIa (thrombin) [36], expectedly, no significant changes in PT, INR or D-Dimer were observed in this study.
The incidence of immune-mediated thrombocytopenia was very low with this SC formulation. Only one patient in this study developed immune-mediated thrombocytopenia with a positive SRA and was withdrawn from study without any sequelae. PI-88 has been associated with immune-mediated thrombocytopenia with a positive AHPF4 lab result similar to the heparin-induced thrombocytopenia syndrome, which also commonly occurs at higher heparin doses, and with the IV rather than SC formulation [10, 11, 42].
PK studies in rats and monkeys using 35S-PI-88 demonstrated 100% bioavailability and predominant urinary excretion of 32–57% in rats and 27% in monkeys, with no metabolites in urine, and no fecal or biliary excretion [36]. Prior clinical PI-88 SC monotherapy studies showed linear plasma concentrations with respect to dose, reflected in both AUC and Cmax, and PK following a one-compartment model with first-order elimination and first-order absorption from an extravascular site [5]—similar to the PI-88 results in this study in the presence of docetaxel. As docetaxel did not significantly interact with or change PI-88 PK, nor did PI-88 interact with or affect docetaxel PK parameters, additive toxicities due to PK interactions were unlikely.
PI-88 is similar to the polysaccharide angiogenesis inhibitor, tecogalan sodium, which inhibits binding of FGF-2 to cellular receptors and inhibits heparin cofactor II, not anti-thrombin III [14], producing anticoagulation as a PD parameter, correlating with the plasma concentration and Cmax [14]. All patients in this study had maximal APTT prolongation post PI-88 with a prolongation at of least grade 1 (>1.5 ×ULN) at Cmax, similar to the prior PI-88 monotherapy study [5]. APTT was more often sustained and more prolonged (grades 1–2) at the higher doses of 190–250 mg/day, (3/7 patients at 250 mg/day developed grade 2 APTT levels post PI-88 dosing), without any serious bleeding. More sustained anticoagulation may be associated with prolonged endothelial cell growth inhibition, improved anti-angiogenic activity and efficacy [14, 17]. Interestingly, patients with more prolonged APTT at the higher doses appeared to also have more sustained disease stability (>4 cycles in one patient at 190 mg/day, and >6 cycles in two patients at 250 mg/day). However, despite observing APTT prolongation and more SD at higher doses, no relationship was determined between PI-88 and the biologic endpoints of serum/urine FGF-2 and VEGF, consistent with previous studies [5, 36, 42]. Further validation and exploration of anti-angiogenic PD markers are necessary as angiogenic growth factor levels fluctuate quite rapidly with time due to multiple sites of production, storage and complex cross-regulation [13, 32, 48].
The study established PI-88 at 250 mg/day SC with fixed weekly 30 mg/m2 docetaxel as the RPTD. These drugs were safely administered at the above doses, without increased toxicity, DLTs or significant bleeding complications. This combination was well tolerated with evidence of disease stability in a variety of malignancies. PI-88 is promising novel therapy in a new class of anti-angiogenic anti-cancer agents, meriting further future study either alone or in combination with chemotherapy in disease-directed clinical trials.
Contributor Information
Laura Q. M. Chow, Email: laurachow@hotmail.com, lachow@ottawahospital.on.ca, University of Colorado Heath Sciences Center, Aurora, CO, USA; The Ottawa Hospital Cancer Center, 501 Smyth Road, Box 912, Ottawa, ON K1H 8L6, Canada.
Daniel L. Gustafson, University of Colorado Heath Sciences Center, Aurora, CO, USA
Cindy L. O’Bryant, University of Colorado Heath Sciences Center, Aurora, CO, USA
Lia Gore, University of Colorado Heath Sciences Center, Aurora, CO, USA.
Michele Basche, University of Colorado Heath Sciences Center, Aurora, CO, USA.
Scott N. Holden, University of Colorado Heath Sciences Center, Aurora, CO, USA
Mark C. Morrow, University of Colorado Heath Sciences Center, Aurora, CO, USA
Stacy Grolnic, University of Colorado Heath Sciences Center, Aurora, CO, USA.
Brian R. Creese, Progen Pharmaceuticals Ltd, Toowong, QLD, Australia
Kaye L. Roberts, Progen Pharmaceuticals Ltd, Toowong, QLD, Australia
Kat Davis, Progen Pharmaceuticals Ltd, Toowong, QLD, Australia.
Russell Addison, Tetra Q Integrated Preclinical Drug Development, University of Queensland, Brisbane, QLD, Australia.
S. Gail Eckhardt, University of Colorado Heath Sciences Center, Aurora, CO, USA.
References
- 1.Amiral J, Bridey F, Dreyfus M, Vissoc AM, Fressinaud E, Wolf M, Meyer D. Platelet factor 4 complexed to heparin is the target for antibodies generated in heparin-induced thrombocytopenia. Thromb Haemost. 1992;68:95–96. [PubMed] [Google Scholar]
- 2.Anderson RL, Lelekakis M, Lowen D, et al. Inhibition of lung metastasis from a breast carcinoma using PI88, a heparanase inhibitor. (abstr) Proc Metastatic Res Soc. 1998 [Google Scholar]
- 3.Baker SD, Zhao M, Lee CK, Verweij J, Zabelina Y, Brahmer JR, Wolff AC, Sparreboom A, Carducci MA. Comparative pharmacokinetics of weekly and every-three-weeks docetaxel. Clin Cancer Res. 2004;10:1976–1983. doi: 10.1158/1078-0432.ccr-0842-03. [DOI] [PubMed] [Google Scholar]
- 4.Bareschino MA, Morgillo F, Ciardiello F. Combination of standard chemotherapy and targeted agents. J Thorac Oncol. 2007;2:S19–S23. doi: 10.1097/01.JTO.0000268636.02709.b4. [DOI] [PubMed] [Google Scholar]
- 5.Basche M, Gustafson DL, Holden SN, O’Bryant CL, Gore L, Witta S, Schultz MK, Morrow M, Levin A, Creese BR, Kangas M, Roberts K, Nguyen T, Davis K, Addison RS, Moore JC, Eckhardt SG. A phase I biological and pharmacologic study of the heparanase inhibitor PI-88 in patients with advanced solid tumors. Clin Cancer Res. 2006;12:5471–5480. doi: 10.1158/1078-0432.CCR-05-2423. [DOI] [PubMed] [Google Scholar]
- 6.Belani CP. Optimizing chemotherapy for advanced nonsmall cell lung cancer: focus on docetaxel. Lung Cancer. 2005;50 Suppl 2:S3–S8. [PubMed] [Google Scholar]
- 7.Berkenblit A, Seiden MV, Matulonis UA, Penson RT, Krasner CN, Roche M, Mezzetti L, Atkinson T, Cannistra SA. A phase II trial of weekly docetaxel in patients with platinum-resistant epithelial ovarian, primary peritoneal serous cancer, or fallopian tube cancer. Gynecol Oncol. 2004;95:624–631. doi: 10.1016/j.ygyno.2004.08.028. [DOI] [PubMed] [Google Scholar]
- 8.Bruno R, Hille D, Riva A, Vivier N, ten Bokkel Huinnink WW, van Oosterom AT, Kaye SB, Verweij J, Fossella FV, Valero V, Rigas JR, Seidman AD, Chevallier B, Fumoleau P, Burris HA, Ravdin PM, Sheiner LB. Population pharmacokinetics/pharmacodynamics of docetaxel in phase II studies in patients with cancer. J Clin Oncol. 1998;16:187–196. doi: 10.1200/JCO.1998.16.1.187. [DOI] [PubMed] [Google Scholar]
- 9.Charleson HA, Bailey RR, Stewart A. Quick prediction of creatinine clearance without the necessity of urine collection. N Z Med J. 1980;92:425–426. [PubMed] [Google Scholar]
- 10.Chong BH. Heparin-induced thrombocytopenia. Br J Haematol. 1995;89:431–439. doi: 10.1111/j.1365-2141.1995.tb08346.x. [DOI] [PubMed] [Google Scholar]
- 11.Chong BH, Eisbacher M. Pathophysiology and laboratory testing of heparin-induced thrombocytopenia. Semin Hematol. 1998;35:3–8. discussion 35–36. [PubMed] [Google Scholar]
- 12.Cohn DE, Valmadre S, Resnick KE, Eaton LA, Copeland LJ, Fowler JM. Bevacizumab and weekly taxane chemotherapy demonstrates activity in refractory ovarian cancer. Gynecol Oncol. 2006;102:134–139. doi: 10.1016/j.ygyno.2006.01.030. [DOI] [PubMed] [Google Scholar]
- 13.Dvorak HF. Vascular permeability factor/vascular endothelial growth factor: a critical cytokine in tumor angiogenesis and a potential target for diagnosis and therapy. J Clin Oncol. 2002;20:4368–4380. doi: 10.1200/JCO.2002.10.088. [DOI] [PubMed] [Google Scholar]
- 14.Eckhardt SG, Burris HA, Eckardt JR, Weiss G, Rodriguez G, Rothenberg M, Rinaldi D, Barrington R, Kuhn JG, Masuo K, Sudo K, Atsumi R, Oguma T, Higashi L, Fields S, Smetzer L, Von Hoff DD. A phase I clinical and pharmacokinetic study of the angiogenesis inhibitor, tecogalan sodium. Ann Oncol. 1996;7:491–496. doi: 10.1093/oxfordjournals.annonc.a010638. [DOI] [PubMed] [Google Scholar]
- 15.Edovitsky E, Elkin M, Zcharia E, Peretz T, Vlodavsky I. Heparanase gene silencing, tumor invasiveness, angiogenesis, and metastasis. J Natl Cancer Inst. 2004;96:1219–1230. doi: 10.1093/jnci/djh230. [DOI] [PubMed] [Google Scholar]
- 16.El-Assal ON, Yamanoi A, Ono T, Kohno H, Nagasue N. The clinicopathological significance of heparanase and basic fibroblast growth factor expressions in hepatocellular carcinoma. Clin Cancer Res. 2001;7:1299–1305. [PubMed] [Google Scholar]
- 17.Folkman J. Seminars in Medicine of the Beth Israel Hospital, Boston. Clinical applications of research on angiogenesis. N Engl J Med. 1995;333:1757–1763. doi: 10.1056/NEJM199512283332608. [DOI] [PubMed] [Google Scholar]
- 18.Ganjoo K. Antiangiogenesis: a new approach to the treatment of lymphoma. Leuk Lymphoma. 2007;48:454–455. doi: 10.1080/10428190701200059. [DOI] [PubMed] [Google Scholar]
- 19.Gervais R, Ducolone A, Breton JL, Braun D, Lebeau B, Vaylet F, Debieuvre D, Pujol JL, Tredaniel J, Clouet P, Quoix E. Phase II randomised trial comparing docetaxel given every 3 weeks with weekly schedule as second-line therapy in patients with advanced non-small-cell lung cancer (NSCLC) Ann Oncol. 2005;16:90–96. doi: 10.1093/annonc/mdi018. [DOI] [PubMed] [Google Scholar]
- 20.Gustafson DL, Long ME, Zirrolli JA, Duncan MW, Holden SN, Pierson AS, Eckhardt SG. Analysis of docetaxel pharmacokinetics in humans with the inclusion of later sampling time-points afforded by the use of a sensitive tandem LCMS assay. Cancer Chemother Pharmacol. 2003;52:159–166. doi: 10.1007/s00280-003-0622-z. [DOI] [PubMed] [Google Scholar]
- 21.Hainsworth JD. Practical aspects of weekly docetaxel administration schedules. Oncologist. 2004;9:538–545. doi: 10.1634/theoncologist.9-5-538. [DOI] [PubMed] [Google Scholar]
- 22.Hainsworth JD, Burris HA, III, Yardley DA, Bradof JE, Grimaldi M, Kalman LA, Sullivan T, Baker M, Erland JB, Greco FA. Weekly docetaxel in the treatment of elderly patients with advanced breast cancer: a Minnie Pearl Cancer Research Network phase II trial. J Clin Oncol. 2001;19:3500–3505. doi: 10.1200/JCO.2001.19.15.3500. [DOI] [PubMed] [Google Scholar]
- 23.Hurria A, Fleming MT, Baker SD, Kelly WK, Cutchall K, Panageas K, Caravelli J, Yeung H, Kris MG, Gomez J, Miller VA, D’Andrea G, Scher HI, Norton L, Hudis C. Pharmacokinetics and toxicity of weekly docetaxel in older patients. Clin Cancer Res. 2006;12:6100–6105. doi: 10.1158/1078-0432.CCR-06-0200. [DOI] [PubMed] [Google Scholar]
- 24.Ji Y, Li Y, Nebiyou Bekele B. Dose-finding in phase I clinical trials based on toxicity probability intervals. Clin Trials. 2007;4:235–244. doi: 10.1177/1740774507079442. [DOI] [PubMed] [Google Scholar]
- 25.Koliopanos A, Friess H, Kleeff J, Shi X, Liao Q, Pecker I, Vlodavsky I, Zimmermann A, Buchler MW. Heparanase expression in primary and metastatic pancreatic cancer. Cancer Res. 2001;61:4655–4659. [PubMed] [Google Scholar]
- 26.Lilenbaum RC, Schwartz MA, Seigel L, Belette F, Blaustein A, Wittlin FN, Davila E. Phase II trial of weekly docetaxel in second-line therapy for nonsmall cell lung carcinoma. Cancer. 2001;92:2158–2163. doi: 10.1002/1097-0142(20011015)92:8<2158::aid-cncr1558>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 27.Lynch T, Jr, Kim E. Optimizing chemotherapy and targeted agent combinations in NSCLC. Lung Cancer. 2005;50(S2):S25–S32. [PubMed] [Google Scholar]
- 28.Mey U, Gorschluter M, Ziske C, Kleinschmidt R, Glasmacher A, Schmidt-Wolf IG. Weekly docetaxel in patients with pretreated metastatic breast cancer: a phase II trial. Anticancer Drugs. 2003;14:233–238. doi: 10.1097/00001813-200303000-00007. [DOI] [PubMed] [Google Scholar]
- 29.Miao HQ, Liu H, Navarro E, Kussie P, Zhu Z. Development of heparanase inhibitors for anti-cancer therapy. Curr Med Chem. 2006;13:2101–2111. doi: 10.2174/092986706777935230. [DOI] [PubMed] [Google Scholar]
- 30.Mikami S, Ohashi K, Katsube K, Nemoto T, Nakajima M, Okada Y. Coexpression of heparanase, basic fibroblast growth factor and vascular endothelial growth factor in human esophageal carcinomas. Pathol Int. 2004;54:556–563. doi: 10.1111/j.1440-1827.2004.01664.x. [DOI] [PubMed] [Google Scholar]
- 31.Mikami S, Ohashi K, Usui Y, Nemoto T, Katsube K, Yanagishita M, Nakajima M, Nakamura K, Koike M. Loss of syndecan-1 and increased expression of heparanase in invasive esophageal carcinomas. Jpn J Cancer Res. 2001;92:1062–1073. doi: 10.1111/j.1349-7006.2001.tb01061.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nagy JA, Vasile E, Feng D, Sundberg C, Brown LF, Detmar MJ, Lawitts JA, Benjamin L, Tan X, Manseau EJ, Dvorak AM, Dvorak HF. Vascular permeability factor/vascular endothelial growth factor induces lymphangiogenesis as well as angiogenesis. J Exp Med. 2002;196:1497–1506. doi: 10.1084/jem.20021244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Panares RL, Garcia AA. Bevacizumab in the management of solid tumors. Expert Rev Anticancer Ther. 2007;7:433–445. doi: 10.1586/14737140.7.4.433. [DOI] [PubMed] [Google Scholar]
- 34.Parish CR, Freeman C, Brown KJ, Francis DJ, Cowden WB. Identification of sulfated oligosaccharide-based inhibitors of tumor growth and metastasis using novel in vitro assays for angiogenesis and heparanase activity. Cancer Res. 1999;59:3433–3441. [PubMed] [Google Scholar]
- 35.Pavlakis N, Parish C, Freeman C, et al. The heparanase inhibitor PI-88 reduces tumor growth in two rat mammary adenocarcinoma models, demonstrating schedule dependency and possible synergy with cisplatin (abstr) Proc Am Assoc Cancer Res. 2000 [Google Scholar]
- 36.Progen, Industries, Ltd. Progen Industries Ltd. Darra, Queensland, Australia: Progen Industries Ltd; 2004. [July 2004]. Investigator’s brochure on PI-88. (unpublished) [Google Scholar]
- 37.Ramaswamy B, Elias AD, Kelbick NT, Dodley A, Morrow M, Hauger M, Allen J, Rhoades C, Kendra K, Chen HX, Eckhardt SG, Shapiro CL. Phase II trial of bevacizumab in combination with weekly docetaxel in metastatic breast cancer patients. Clin Cancer Res. 2006;12:3124–3129. doi: 10.1158/1078-0432.CCR-05-2603. [DOI] [PubMed] [Google Scholar]
- 38.Ramaswamy B, Shapiro CL. Phase II trial of bevacizumab in combination with docetaxel in women with advanced breast cancer. Clin Breast Cancer. 2003;4:292–294. doi: 10.3816/cbc.2003.n.035. [DOI] [PubMed] [Google Scholar]
- 39.Ranieri G, Patruno R, Ruggieri E, Montemurro S, Valerio P, Ribatti D. Vascular endothelial growth factor (VEGF) as a target of bevacizumab in cancer: from the biology to the clinic. Curr Med Chem. 2006;13:1845–1857. doi: 10.2174/092986706777585059. [DOI] [PubMed] [Google Scholar]
- 40.Robertshaw M, Lai KN, Swaminathan R. Prediction of creatinine clearance from plasma creatinine: comparison of five formulae. Br J Clin Pharmacol. 1989;28:275–280. doi: 10.1111/j.1365-2125.1989.tb05427.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rosen L. Antiangiogenic strategies and agents in clinical trials. Oncologist. 2000;5 Suppl 1:20–27. doi: 10.1634/theoncologist.5-suppl_1-20. [DOI] [PubMed] [Google Scholar]
- 42.Rosenthal MA, Rischin D, McArthur G, Ribbons K, Chong B, Fareed J, Toner G, Green MD, Basser RL. Treatment with the novel anti-angiogenic agent PI-88 is associated with immune-mediated thrombocytopenia. Ann Oncol. 2002;13:770–776. doi: 10.1093/annonc/mdf117. [DOI] [PubMed] [Google Scholar]
- 43.Schuette W, Nagel S, Blankenburg T, Lautenschlaeger C, Hans K, Schmidt EW, Dittrich I, Schweisfurth H, von Weikersthal LF, Raghavachar A, Reissig A, Serke M. Phase III study of second-line chemotherapy for advanced non-small-cell lung cancer with weekly compared with 3-weekly docetaxel. J Clin Oncol. 2005;23:8389–8395. doi: 10.1200/JCO.2005.02.3739. [DOI] [PubMed] [Google Scholar]
- 44.Sheridan D, Carter C, Kelton JG. A diagnostic test for heparin-induced thrombocytopenia. Blood. 1986;67:27–30. [PubMed] [Google Scholar]
- 45.Shteper PJ, Zcharia E, Ashhab Y, Peretz T, Vlodavsky I, Ben-Yehuda D. Role of promoter methylation in regulation of the mammalian heparanase gene. Oncogene. 2003;22:7737–7749. doi: 10.1038/sj.onc.1207056. [DOI] [PubMed] [Google Scholar]
- 46.Simizu S, Ishida K, Wierzba MK, Sato TA, Osada H. Expression of heparanase in human tumor cell lines and human head and neck tumors. Cancer Lett. 2003;193:83–89. doi: 10.1016/s0304-3835(02)00719-x. [DOI] [PubMed] [Google Scholar]
- 47.Tabernero J, Climent MA, Lluch A, Albanell J, Vermorken JB, Barnadas A, Anton A, Laurent C, Mayordomo JI, Estaun N, Losa I, Guillem V, Garcia-Conde J, Tisaire JL, Baselga J. A multicentre, randomised phase II study of weekly or 3-weekly docetaxel in patients with metastatic breast cancer. Ann Oncol. 2004;15:1358–1365. doi: 10.1093/annonc/mdh349. [DOI] [PubMed] [Google Scholar]
- 48.Taipale J, Keski-Oja J. Growth factors in the extracellular matrix. Faseb J. 1997;11:51–59. doi: 10.1096/fasebj.11.1.9034166. [DOI] [PubMed] [Google Scholar]
- 49.Therasse P. Measuring the clinical response. What does it mean? Eur J Cancer. 2002;38:1817–1823. doi: 10.1016/s0959-8049(02)00182-x. [DOI] [PubMed] [Google Scholar]
- 50.Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van Oosterom AT, Christian MC, Gwyther SG. New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst. 2000;92:205–216. doi: 10.1093/jnci/92.3.205. [DOI] [PubMed] [Google Scholar]
- 51.Turnbull J, Powell A, Guimond S. Heparan sulfate: decoding a dynamic multifunctional cell regulator. Trends Cell Biol. 2001;11:75–82. doi: 10.1016/s0962-8924(00)01897-3. [DOI] [PubMed] [Google Scholar]
- 52.van Hinsbergh VW, Collen A, Koolwijk P. Angiogenesis and anti-angiogenesis: perspectives for the treatment of solid tumors. Ann Oncol. 1999;10 Suppl 4:60–63. [PubMed] [Google Scholar]
- 53.Xu X, Rao G, Quiros RM, Kim AW, Miao HQ, Brunn GJ, Platt JL, Gattuso P, Prinz RA. In vivo and in vitro degradation of heparan sulfate (HS) proteoglycans by HPR1 in pancreatic adenocarcinomas. Loss of cell surface HS suppresses fibroblast growth factor 2-mediated cell signaling and proliferation. J Biol Chem. 2007;282:2363–2373. doi: 10.1074/jbc.M604218200. [DOI] [PubMed] [Google Scholar]
- 54.Yayon A, Klagsbrun M, Esko JD, Leder P, Ornitz DM. Cell surface, heparin-like molecules are required for binding of basic fibroblast growth factor to its high affinity receptor. Cell. 1991;64:841–848. doi: 10.1016/0092-8674(91)90512-w. [DOI] [PubMed] [Google Scholar]
- 55.Zhang W, Gordon M, Lenz HJ. Novel approaches to treatment of advanced colorectal cancer with anti-EGFR monoclonal antibodies. Ann Med. 2006;38:545–551. doi: 10.1080/09546630601070812. [DOI] [PubMed] [Google Scholar]